Abstract
Few studies have focused on the effect of organ damage on achievement of long-term home blood pressure (BP) control. Based on the nationwide home BP-based trial data, we aimed to investigate the factors associated with home BP control, in particular, left ventricular hypertrophy (LVH) using the electrocardiogram in patients who started antihypertensive drug treatment. According to the trial protocol, we defined BP as controlled when systolic home BP reached specified targets (125–134 mm Hg in usual control (UC), n=1261; <125 mm Hg in tight control (TC), n=1288). At baseline, before drug treatment started, the mean Sokolow–Lyon voltage was 2.57±0.87 mV, and the mean Cornell product was 1573±705 mm·ms. The numbers of patients who achieved the target BP level in the UC and TC groups were 892 (70.7%) and 576 (44.7%), respectively. In both the UC and TC groups, systolic home BP at baseline was significantly lower in patients who achieved target levels than in those who did not achieve target levels (P<0.0001). Sokolow–Lyon voltage was significantly lower in patients who achieved target levels than in those who did not (P⩽0.0055). The Cornell product levels in each group were similar (P⩾0.12), although significantly different between patients who did or did not achieve the target level when the UC and TC groups were combined for analysis (P=0.031). Sokolow–Lyon voltage was significantly associated with achievement of home BP control in the multivariable-adjusted model (odds ratio, 1.13; 95% confidence intervals, 1.02–1.26; P=0.015), but Cornell product was not (P=0.13). These results indicate the difficulty of sufficient antihypertensive treatment when untreated patients had target organ damage, that is, LVH diagnosed by Sokolow–Lyon voltage.
Similar content being viewed by others
Introduction
Left ventricular hypertrophy (LVH) is one of the major types of target organ damage caused by hypertension.1 Electrocardiography is usually the first test performed to assess LVH in clinical practice because electrocardiography is easy to perform, widely available and inexpensive.2 Sokolow–Lyon voltage, which represents abnormally high voltage of the QRS complex, has been most commonly used for diagnosing LVH by electrocardiography.3 Recently, the Cornell product, which is based on correlation with left ventricular mass index, has also been commonly used.4, 5 However, the utility of electrocardiography for the diagnosis of LVH is unclear.6, 7 Electrocardiography shows similar specificity but lower sensitivity for the diagnosis of LVH compared with echocardiography.8 To identify the current conditions and prognoses of patients accurately, we need to further establish the potential of LVH diagnosis based on electrocardiograms.
The causes of uncontrolled hypertension in clinic blood pressure (BP) include: older age,9 higher baseline systolic BP,10 the presence of LVH and obesity (body mass index >30 kg m−2).11 Although self-measured home BP has higher predictive power than conventional clinic BP measurements,12, 13 few studies have focused on factors for achievement of long-term home BP control.14 Izzo et al.15 reported that initial left ventricular mass is a significant predictor of uncontrolled clinic BP. However, the association between LVH and long-term home BP control is not clear. Based on the multicenter Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) trial,13, 16, 17 we aimed to investigate determinant factors for achievement of target home BP, and in particular the impact of LVH, determined by electrocardiography, as well as other organ damage in patients with mild-to-moderate hypertension who started antihypertensive treatment.
Methods
Study population
The HOMED-BP study was a multicenter clinical trial with PROBE (prospective, randomized, open-label, blinded end point evaluation)18 design. The HOMED-BP protocol complies with the Helsinki declaration for the investigation of human subjects19 and is registered with the UMIN Clinical Trial Registry, number C000000137 (http://www.umin.ac.jp/ctr). The institutional review board of the Tohoku University Graduate School of Medicine approved the study protocol, and all study participants gave written informed consent.
In the HOMED-BP study,13, 16 patients with mild-to-moderate hypertension with a minimum age of 40 years were recruited from 457 general practices throughout Japan. Treatment-naive patients as well as previously treated patients whose antihypertensive drug treatment could be discontinued for ⩾2 weeks qualified for enrollment. Off treatment, eligible patients had a home BP of 135–179 mm Hg systolic or 85–119 mm Hg diastolic. Randomization was based on a computerized random number function with a minimization algorithm running on a central server at Tohoku University (Sendai, Japan), considering sex, age and systolic and diastolic home BP. In a 2 × 3 design, eligible patients were randomized to usual control (UC; ranging from 125 to 134 mm Hg systolic and from 80 to 84 mm Hg diastolic) vs. tight control (TC; <125 mm Hg systolic and 80 mm Hg diastolic) of home BP and to the initiation of antihypertensive drug treatment with calcium channel blocker (CCB), angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blockade. The first patient was randomized on 6 June 2001, and the last patient on 7 October 2009. Moreover, the HOMED-BP Management Committee decided to continue the operation of the HOMED-BP system until the end of 2012; therefore, we collected BP data and ascertained outcomes until 31 December 2012.13, 17
From the 3518 randomized patients, 969 were excluded from analysis because home BP at follow-up was not available (n=371) or because information on Sokolow–Lyon voltage or Cornell product was missing (n=628). Therefore, the number of patients statistically analyzed totaled 2549 (1261 in UC and 1288 in TC). The clinical characteristics of the 969 excluded patients are shown in Supplementary Table S1. In the present analysis, we defined achievement of BP control as systolic BP that reached the target range (125–134 mm Hg in UC, <125 mm Hg in TC) because systolic pressure is an overriding risk factor in middle-aged and older people.20, 21
Data collection
At each visit, after the patients had rested in the sitting position for ⩾2 min, practitioners obtained two consecutive measurements of BP and heart rate using the validated22 oscillometric OMRON HEM-907IT device (Omron Healthcare, Kyoto, Japan). The clinic BP was the average of these two readings. Patients received spoken and written instructions on BP self-measurement and the utilization of the validated23 oscillometric HEM-747IC-N monitors (Omron Healthcare). The monitor stores up to 350 BP and heart rate readings in its memory. The home BP used for determining eligibility and treatment adjustments at each visit was the average of the morning readings available over 5 days immediately preceding the visit. Patients were asked to measure BP once every morning after ⩾2 min of rest in the sitting position during the whole study period. They had to obtain these measurements within 1 h of awakening, before breakfast and before taking antihypertensive medication.
At each visit, the central server received the home and clinic BP data from local practices and immediately displayed them on the screen of the local computer along with advice for treatment adjustment based on a computerized algorithm, as described elsewhere.13, 16 Doctors were allowed to modify the treatment advice throughout the follow-up period according to the condition of the patients, drug adoption in each clinic or their judgement.
According to the study protocol,16 we obtained information, including physical measurements, medical records, electrocardiogram measurements and laboratory test data from each practice.
Definitions
Body mass index was defined as body weight in kilograms divided by height in meters squared. We calculated the Sokolow–Lyon voltage (RV5+SV1; mV) 3 and Cornell product ((RaVL+SV3) × QRS duration in men; (RaVL+SV3+6) × QRS duration in women; mm·ms)4, 5 as electrocardiographic diagnostic criteria (Figure 1).24 Estimated glomerular filtration rate (eGFR) was calculated with the Japanese Equation25: Estimated glomerular filtration rate (ml min−1 1.73 m−2)=194 × serum creatinine−1.094 × age−0.287 (× 0.739, for women). We used the defined daily dose index to standardize the hypertensive drug uses.26 The defined daily dose is defined by the World Health Organization Collaborating Centre for Drug Statistics Methodology and is the assumed average maintenance dose per day for a drug used for its main indication in adults.26
Criteria of left ventricular hypertrophy (LVH) based on the electrocardiogram. LVH was defined as follows: Sokolow–Lyon voltage ⩾3.50 mV, Cornell product ⩾2440 mm·ms.24
Statistical analysis
For database management and statistical analysis, we used the SAS software, version 9.4 (SAS Institute, Cary, NC, USA). Statistical significance was defined as an alpha level <0.05 in two-sided tests. All data are expressed as the mean±s.d. unless otherwise stated.
Categorical variables were compared using the χ2 test, and Student’s t-tests or Wilcoxon tests were applied to continuous variables appropriately according to its distribution normality. As electrocardiographic diagnostic criteria, we compared Sokolow–Lyon voltage vs. Cornell product with systolic home BP in relation to the correlation coefficients. Logistic regression models were then used to estimate the multivariate adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for the association between electrocardiographic indices and management of hypertension. The models were adjusted for baseline home BP, sex, age, smoking, drinking, previous cardiovascular disease, duration of the state of hypertension, defined daily dose and the following laboratory tests that can represent each organ relevant to its cardiovascular risks: hemoglobin concentration, white blood cell counts, platelet counts, serum γ-glutamyltransferase level, estimated glomerular filtration rate, total cholesterol level, plasma glucose level, and proteinuria. Target home BP, UC vs. TC, was further adjusted among all patients. Missing values were complemented by Multiple Imputation using a Markov single-chain Monte Carlo method.27 The imputation model included all covariables entered in the logistic regression model. Sensitivity analyses were conducted to ascertain that imputations did not weaken or inflate the reported associations.
Based on Sokolow–Lyon voltage, we also divided patients according to the quartile points of the population (<1.93, 1.93–2.50, 2.50–3.09 and ⩾3.09 mV) as well as the electrocardiographic diagnostic criteria of LVH (⩾3.50 mV) and computed ORs and CIs of achievement of home BP level in a higher category. Furthermore, we analyzed logistic regression models dividing patients between UC and TC. ORs and CIs of patients’ achieving hypertension management with the threshold of 135 mm Hg in systolic pressure, which has been widely accepted as definition of hypertension for home BP,28, 29 were also analyzed. In the sensitivity analysis, diabetes mellitus was defined by fasting plasma glucose ⩾7.0 mmol l−1 (⩾126 mg dl−1), hemoglobin A1c ⩾6.5% or treatment with antidiabetic agents.13, 17 Finally, we calculated the ORs of clinic BP instead of home BP and analyzed the association between Sokolow–Lyon voltage and the management of hypertension based on clinic BP.
Results
The baseline characteristics of the study population are shown in Table 1. The mean age was 60.0±9.9 years, and 1302 (51.2%) patients were women. The numbers of patients who achieved the target BP in UC and TC were 892 (70.7%) and 576 (44.7%), respectively. In both the UC and TC groups, systolic home BP at baseline was significantly lower in patients who achieved target BP than in those who did not (Table 2; 150.3±12.5 mm Hg vs. 155.1±12.5 mm Hg in UC, P>0.0001; 149.4±12.0 vs. 153.5±12.4 mm Hg in TC, P>0.0001), whereas diastolic home BPs did not differ (P⩾0.074). Clinic BP values at baseline were similar regardless of the achievement of home BP control (P>0.13), except for diastolic clinic BP among TC (P=0.0012).
The Sokolow–Lyon voltage at baseline averaged 2.57±0.87 mV, and the Cornell product was 1573±705 mm·ms. Both LVH indexes were significantly correlated with each other (r=0.16, P>0.0001), and 532 patients (20.8%) had LVH based on Sokolow–Lyon criteria and/or Cornell product. However, the number of patients with LVH diagnosed by electrocardiogram was 353 (13.9%) when based on Sokolow–Lyon voltage and 251 (9.9%) when based on Cornell product, and only 72 patients fulfilled both diagnostic criteria (2.8%; κ=0.14).
The Sokolow–Lyon voltage was significantly higher in patients without achievement of the target BP than those whose BP did not (Table 1; P⩽0.0055). This difference was also observed when the UC and TC groups were combined (2.65±0.89 vs. 2.51±0.84 mV, P=0.0001). Although the Cornell product level was significantly different when both groups were combined (1608±721 vs. 1547±691 mm•ms, P=0.031), statistical significance was not observed in either the UC or the TC group (P⩾0.12). The correlation between systolic home BP and Sokolow–Lyon voltage was also significant (r=0.16, P>0.0001) and tended to be stronger than that between systolic home BP and Cornell product (r=0.11, P>0.0001).
Based on the aforementioned results, we used Sokolow–Lyon voltage as the representative index of LVH. The multivariable-adjusted ORs of failure to achieve target BP when Sokolow–Lyon voltage was treated as the continuous variable are shown in Table 3. After the adjustment of baseline systolic home BP, which was significantly associated with the achievement of target BP (OR, 1.26; 95% CI, 1.17–1.36; P<0.0001), a 1-mV increment of Sokolow–Lyon voltage resulted in a 13% increase in patients who did not achieve target BP (P=0.015). The ORs of failure to achieve target BP were similar, 1.14 (95% CI, 0.98–1.33; P=0.089) and 1.13 (95% CI, 0.98–1.30; P=0.084), when patients were divided into UC and TC, respectively. When we set the same criteria of hypertension in home systolic BP, 135 mm Hg to TC as well as UC, the risk of being hypertensive during the follow-up period was marginal among all patients (OR per 1-mV increment, 1.10; 95% CI, 0.99–1.22; P=0.083).
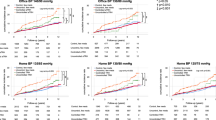
Figure 2 shows the multivariate ORs when we set four different Sokolow–Lyon voltage criteria, such as 3.50 mV (as the LVH definition), 3.09 mV (upper quartile of patients), 2.50 mV (median) and 1.93 mV (lower quartile). None of the thresholds had a significant impact on achievement of target BP regardless of total, UC and TC (P⩾0.063), except in patients with Sokolow–Lyon voltage ⩾2.50 mV (Figure 2; P=0.043).
Odds ratios (ORs) of Sokolow–Lyon voltages for patients who fail to achieve target blood pressure (vs. patients who do achieve target) among (a) total, (b) usual control and (c) tight control groups when systolic home blood pressure was included in the models. Values are shown as ORs (95% confidence intervals). The models were adjusted for sex, age, smoking, alcohol consumption, previous cardiovascular disease, duration of state of hypertension, defined daily dose and the following laboratory test information: hemoglobin concentration, white blood cell counts, platelet counts, serum γ-glutamyltransferase level, eGFR, total cholesterol level, plasma glucose level, and proteinuria. Target home blood pressure, UC vs. TC, was further adjusted among all patients. None of the thresholds had a significant impact on the achievement of target blood pressure regardless of total, UC and TC (P⩾0.063) except in patients with Sokolow–Lyon voltage ⩾2.50 mV (P=0.043). Mark indicates significance of ORs: *P<0.05.
When we calculated ORs of the diabetes mellitus variable (based on plasma glucose level), diabetes mellitus was not found to be significantly associated with home BP control as shown in Supplementary Table S2 (OR, 1.06; 95% CI, 0.83–1.36).
Clinic BP was not significantly associated with the achievement of home BP control (P=0.56), whereas Sokolow–Lyon voltage was still a significant predictor of successful home BP control (OR, 1.19; 95% CI, 1.08–1.32; P=0.0005) (Supplementary Table S3). The multivariate-adjusted ORs when UC and TC patient groups were separately analyzed were 1.19 among UC (95% CI 1.03–1.38; P=0.022) and 1.19 among TC (95% CI 1.04–1.37; P=0.013). In the dichotomous analysis, when systolic clinic BP was included in the models, patients with Sokolow–Lyon voltage ⩾3.09, ⩾2.50 and ⩾1.93 mV did not achieve home BP control level significantly more often than the other corresponding patients (Supplementary Figure S1; P<0.006). When we focused on the achievement of clinic systolic BP control level (<140 mm Hg systolic), Sokolow–Lyon voltage was not significantly associated with clinic BP control (P=0.94), whereas high plasma glucose was a significant predictor for worse control of clinic BP (P=0.0078; Supplementary Table S4). Cornell product was significantly but marginally associated with achievement of home BP control when systolic clinic BP was adjusted in the multiple regression model (OR, 1.14; 95% CI, 1.01–1.29; P=0.035), although it was not significant when systolic home BP was used for the adjustment (P=0.13). Further sensitivity analysis based on 2343 selected patients who had full baseline information, without applying multiple imputation, provided confirmatory results.
Discussion
In the multivariable-adjusted model including baseline home BP, we found that (1) Sokolow–Lyon voltage was significantly higher in patients with a failure to achieve control group regardless of UC or TC grouping (P⩽0.0055), whereas the Cornell product was not (P⩾0.12), and (2) the achievement rate of BP control level among patients with antihypertensive treatment was 13% lower for each 1-mV increment of Sokolow–Lyon voltage at baseline. To our knowledge, this is the first study to indicate the difficulty of determining sufficient antihypertensive treatment based on self-measured home BP when untreated patients had target organ damage, that is, LVH diagnosed by Sokolow–Lyon voltage in electrocardiography.
The discrepancy between Sokolow–Lyon voltage and Cornell product on the achievement of BP control can be explained by the different measuring targets of each method (Figure 1). Sokolow–Lyon voltage represents the electric potential in the horizontal plane, which mainly reflects left ventricle wall thickness.3, 30 Additionally, a previous study demonstrated that concentric hypertrophy was the most common type of left ventricular disorder in patients with resistant hypertension.31 Pressure overloaded left ventricle resulting in concentric hypertrophy is indicated by the increased ratio of left ventricle wall thickness to internal radius.32 The Cornell product is associated with volume overload,4, 5 as the product of wave voltages and QRS duration can identify the left ventricular mass index more accurately than each component alone.5 In contrast to pressure overload, such volume-overloaded ventricles showed eccentric hypertrophy with an increased diameter but a normal ratio of left ventricle wall thickness to internal radius.32 The ratio of left ventricle wall thickness to internal radius was normal in patients with left ventricle volume overload but was increased in patients with pressure overload.33 These findings suggest that pressure overload leads to thickening of the left ventricular wall in patients with hypertension. Sokolow–Lyon voltage at baseline may therefore reflect the difficulty of BP control by antihypertensive drug treatment. Sokolow–Lyon voltage and Cornell product are strongly associated with pressure overload and volume overload, respectively; therefore, Sokolow–Lyon voltage is a better method for identifying LVH caused by hypertension.
Non-invasive electrocardiography is commonly used to screen for cardiac dysfunction because the test can be conducted more safely, at lower cost and with shorter duration than echocardiography.34, 35 However, the sensitivity of the electrocardiogram for predicting cardiovascular events was too low to be practical as a screening tool.6 Sensitivity and specificity for diagnosing LVH by echocardiography vs. electrocardiography are 93% and 95% vs. 21% and 95%, respectively.8 False-positive tests are likely to lead to harm through unnecessary invasive procedures, overtreatment and misdiagnosis.7 Our findings explore the novel usefulness of electrocardiography to predict achievement of antihypertensive drug management, which may be one step toward avoiding target organ damage in patients with hypertension.
Hemoglobin concentration and white blood cell counts were also significant predictors of uncontrolled home BP. Shankar et al.36 reported that white blood cell count was related to incident hypertension, and this can explain the effect of elevated white blood cell count on hypertension, which involves chronic low-grade inflammation.37 However, few studies demonstrated the positive association between BP control and white blood cell counts as well as hemoglobin concentration. Although C-reactive protein information was unavailable, our study would be the first to indicate that high white blood cell counts or hemoglobin are related to uncontrolled BP.
Plasma glucose level and diabetes mellitus were not associated with home BP control, which was different from the results of a previous study by Izzo et al.15 In the present study, glucose level was associated with worse clinic BP control during treatment (Supplementary Table S4); however, we emphasize that the HOMED-BP study was designed with the aim to home BP control. Clinic BP was treated as additional information, and the central server did not use the clinic BP for decision-making on antihypertensive medication. The difference in the prevalence of diabetes (15% in the present study vs. 5% in the study by Izzo et al.15) might also contribute to this discrepancy between studies.
The present findings must be interpreted with potential limitations. First, the current population consisted of patients with mild-to-moderate essential hypertension with comparably low risk, and generalizability of the current findings is not guaranteed. Second, although the prevalence of LVH in this study population was reported to be 16–34%,24, 38 the kappa coefficient of diagnosing LVH by Sokolow–Lyon voltage and Cornell product was only 0.14. However, similar to the case in the present study, in the Japanese nationwide surveillance study, 15.5% of 747 patients had LVH diagnosed by electrocardiogram, while 10.8% were diagnosed using Sokolow–Lyon voltage and 5.4% by Cornell productwith little overlap.24 Third, we failed to determine the threshold of LVH indices by the logistic regression model with home BP as covariate. Although the continuous trend for Sokolow–Lyon voltage was significant, we cannot apply our findings directly to establish a threshold for suggesting resistant hypertension in the screening process. Finally, we could not assess the drug differences among groups receiving calcium channel blockers, angiotensin-converting enzyme inhibitors and angiotensin receptor blockades because the number of patients was too small to compare the drug contribution to LVH for home BP control during follow-up. We adjusted the drug potency, represented by the defined daily dose, and the final on-treatment home BP level was similar among three drug classes in the HOMED-BP patients13; however, regressive effects of renin–angiotensin system inhibitors on LVH might affect home BP control.
In conclusion, the present study demonstrated that elevated Sokolow–Lyon voltage was an independent predictor for BP control failure even when systolic home BP was included in the multivariable-adjusted model. Although we failed to determine the threshold of LVH indices for adequate BP control, the importance of electrocardiographic measurement for patients with mild-to-moderate hypertension was demonstrated. Accurate electrocardiographic measurement in conjunction with home BP measurement is useful for long-term home BP control by antihypertensive drug treatment.
References
Devereux RB, Pickering TG, Harshfield GA, Kleinert HD, Denby L, Clark L, Pregibon D, Jason M, Kleiner B, Borer JS, Laragh JH . Left ventricular hypertrophy in patients with hypertension: importance of blood pressure response to regularly recurring stress. Circulation 1983; 68: 470–476.
Alfakih K, Reid S, Hall A, Sivananthan MU . The assessment of left ventricular hypertrophy in hypertension. J Hypertens 2006; 24: 1223–1230.
Sokolow M, Lyon TP . The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 1949; 37: 161–186.
Casale PN, Devereux RB, Kligfield P, Eisenberg RR, Miller DH, Chaudhary BS, Phillips MC . Electrocardiographic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol 1985; 6: 572–580.
Molloy TJ, Okin PM, Devereux RB, Kligfield P . Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol 1992; 20: 1180–1186.
Ashley EA, Raxwal V, Froelicher V . An evidence-based review of the resting electrocardiogram as a screening technique for heart disease. Prog Cardiovasc Dis 2001; 44: 55–67.
Brown M . AAFP participates in campaign to cut unnecessary medical interventions. Ann Fam Med 2012; 10: 373–374.
Reichek N, Devereux RB . Left ventricular hypertrophy: relationship of anatomic, echocardiographic and electrocardiographic findings. Circulation 1981; 63: 1391–1398.
Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D . Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension 2000; 36: 594–599.
Lloyd-Jones DM, Evans JC, Larson MG, Levy D . Treatment and control of hypertension in the community: a prospective analysis. Hypertension 2002; 40: 640–646.
Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, Black HR, Hamilton BP, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright JT Jr, Alderman MH, Weiss RJ, Piller L, Bettencourt J, Walsh SM . Allhat Collaborative Research Group. Success and predictors of blood pressure control in diverse North American settings: the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial (ALLHAT). J Clin Hypertens 2002; 4: 393–404.
Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, Aparicio LS, Hara A, Johansson JK, Ohkubo T, Tzourio C, Stergiou GS, Sandoya E, Tsuji I, Jula AM, Imai Y, Staessen JA . International Database of Home Blood Pressure in Relation to Cardiovascular Outcome Investigators. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med 2014; 11: e1001591.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y . Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35: 1102–1110.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S . Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
Izzo R, de Simone G, Devereux RB, Giudice R, De Marco M, Cimmino CS, Vasta A, De Luca N, Trimarco B . Initial left-ventricular mass predicts probability of uncontrolled blood pressure in arterial hypertension. J Hypertens 2011; 29: 803–808.
Fujiwara T, Nishimura T, Ohkuko T, Imai Y . HOMED-BP Study Group. Rationale and design of HOMED-BP Study: hypertension objective treatment based on measurement by electrical devices of blood pressure study. Blood Press Monit 2002; 7: 77–82.
Asayama K, Ohkubo T, Hanazawa T, Watabe D, Hosaka M, Satoh M, Yasui D, Staessen JA, Imai Y . Hypertensive Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure Study Investigators. Does antihypertensive drug class affect day-to-day variability of self-measured home blood pressure? The HOMED-BP Study. J Am Heart Assoc 2016; 4: e002995.
Hansson L, Hedner T, Dahlof B . Prospective randomized open blinded end-point (PROBE) study. A novel design for intervention trials. Prospective randomized open blinded end-point. Blood Press 1992; 1: 113–119.
World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997; 277: 925–926.
Kannel WB . Elevated systolic blood pressure as a cardiovascular risk factor. Am J Cardiol 2000; 85: 251–255.
Staessen J, Amery A, Fagard R . Isolated systolic hypertension in the elderly. J Hypertens 1990; 8: 393–405.
White WB, Anwar YA . Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit 2001; 6: 107–110.
Chonan K, Kikuya M, Araki T, Fujiwara T, Suzuki M, Michimata M, Hashimoto J, Ohkubo T, Hozawa A, Yamamoto N, Miyawaki Y, Matsubara M, Imai Y . Device for the self-measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit 2001; 6: 203–205.
Shibamiya T, Obara T, Ohkubo T, Shinki T, Ishikura K, Yoshida M, Satoh M, Hashimoto T, Hara A, Metoki H, Inoue R, Asayama K, Kikuya M, Imai Y . J-HOME-Elderly study group. Electrocardiographic abnormalities and home blood pressure in treated elderly hypertensive patients: Japan home vs. office blood pressure measurement evaluation in the elderly (J-HOME-Elderly) study. Hypertens Res 2010; 33: 670–677.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A . Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
World Health Organization World Health Organization Collaborating Centre for Drug Statistics Methodology System of Defined Daily Doses 2011. http://www.whocc.no/atc_ddd_index/. Accessed 23 August 2011.
Rubin DB . Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons: Hoboken, New Jersey, USA. 2008.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S . Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Tomita S, Ueno H, Takata M, Yasumoto K, Tomoda F, Inoue H . Relationship between electrocardiographic voltage and geometric patterns of left ventricular hypertrophy in patients with essential hypertension. Hypertens Res 1998; 21: 259–266.
Dobrowolski P, Prejbisz A, Klisiewicz A, Florczak E, Rybicka J, Januszewicz A, Hoffman P . Determinants of concentric left ventricular hypertrophy in patients with resistant hypertension: RESIST-POL study. Hypertens Res 2015; 38: 545–550.
Grossman W, Jones D, McLaurin LP . Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest 1975; 56: 56–64.
Gaasch WH, Zile MR . Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 2011; 58: 1733–1740.
Corrado D, Pelliccia A, Bjornstad HH, Vanhees L, Biffi A, Borjesson M, Panhuyzen-Goedkoop N, Deligiannis A, Solberg E, Dugmore D, Mellwig KP, Assanelli D, Delise P, van-Buuren F, Anastasakis A, Heidbuchel H, Hoffmann E, Fagard R, Priori SG, Basso C, Arbustini E, Blomstrom-Lundqvist C, McKenna WJ, Thiene G . Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology, the Working Group of Myocardial Pericardial Diseases of the European Society of Cardiology. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2005; 26: 516–524.
Maron BJ, Friedman RA, Kligfield P, Levine BD, Viskin S, Chaitman BR, Okin PM, Saul JP, Salberg L, Van Hare GF, Soliman EZ, Chen J, Matherne GP, Bolling SF, Mitten MJ, Caplan A, Balady GJ, Thompson PD . American Heart Association Council on Clinical Cardiology, Advocacy Coordinating Committee, Council on Cardiovascular Disease in the Young, Council on Cardiovascular Surgery and Anesthesia, Council on Epidemiology and Prevention, Council on Functional Genomics and Translational Biology, Council on Quality of Care and Outcomes Research, American College of Cardiology. Assessment of the 12-lead electrocardiogram as a screening test for detection of cardiovascular disease in healthy general populations of young people (12–25 years of age): a scientific statement from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol 2014; 64: 1479–1514.
Shankar A, Klein BE, Klein R . Relationship between white blood cell count and incident hypertension. Am J Hypertens 2004; 17: 233–239.
Bautista LE . Inflammation, endothelial dysfunction, and the risk of high blood pressure: epidemiologic and biological evidence. J Hum Hypertens 2003; 17: 223–230.
Park JB, Schiffrin EL . Small artery remodeling is the most prevalent (earliest?) form of target organ damage in mild essential hypertension. J Hypertens 2001; 19: 921–930.
Acknowledgements
We are grateful to all the HOMED-BP study collaborators as listed previously13 for their valuable contribution. We thank the staff of Tohoku University and Teikyo University for their valuable help. This work was supported by the Japan Cardiovascular Research Foundation; the Japan Arteriosclerosis Prevention Fund; Tohoku University 21st Center of Excellence Program ‘Comprehensive Research and Education Center for Planning of Drug Development and Clinical Evaluation’; Grant-in-Aid for Scientific Research (23390171, 25253059, 26860093, 16K15359) from the Ministry of Education, Culture, Sports, Science and Technology, Japan; and Grant-in-Aid for Japan Society for the Promotion of Science (JSPS) fellows (25*7756 and 25*9328).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
T Hanazawa is a full-time employee of GlaxoSmithKline. T Hanazawa is also a graduate student at Tohoku University and has contributed to this study independently of GlaxoSmithKline. Omron Healthcare gave research support to Y Imai. The other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Tanabe, A., Asayama, K., Hanazawa, T. et al. Left ventricular hypertrophy by electrocardiogram as a predictor of success in home blood pressure control: HOMED-BP study. Hypertens Res 40, 504–510 (2017). https://doi.org/10.1038/hr.2016.176
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.176
Keywords
This article is cited by
-
Home blood pressure monitoring: a position statement from the Korean Society of Hypertension Home Blood Pressure Forum
Clinical Hypertension (2022)
-
Electrocardiography and left ventricular function: looking beyond hypertrophy
Hypertension Research (2019)