Abstract
Seasonal variation of blood pressure (BP) has been reported in small populations or by BP levels captured at only a few points in a year, for example, summer and winter. We aimed to investigate the multiyear seasonal variation in self-measured home BP among hypertensive patients receiving antihypertensive medications. We selected 1649 eligible patients receiving antihypertensive drug treatment, and weekly averaged home BPs were analyzed throughout the follow-up period. Systolic and diastolic home BPs were fitted with the cosine function: ‘Variation+Other Effects+Intercept’, in which the ‘Variation’ was expressed by a cosine curve with three parameters representing: (1) maximum–minimum difference of home BP in one cycle of the cosine curve; (2) time required for one cycle of the cosine curve for home BP variation; and (3) time at which home BP reached the maximum point. Maximum–minimum differences in home BP were 6.7/2.9 mm Hg, and the highest home BPs were observed in mid-to-late January. In the multivariable-adjusted model, a large maximum–minimum difference in home BP was associated with lower body mass index and older age, and larger differences were observed in men compared with women. Summer–winter difference in home BP was essentially similar every year, though it was marginally reduced by 0.14/0.04 mm Hg per year, under long-term antihypertensive treatment. Records of daily home BP measurements enable us to capture long-term factors such as seasonal variation. Home BP should therefore be carefully monitored, particularly in patients with increased BP in winter, to mitigate cardiovascular risk.
Similar content being viewed by others
Introduction
Blood pressure (BP) is generally higher in winter and lower in summer.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 A consistent trend for such seasonal variation has been reported regardless of BP level.5 Seasonal change of BP is associated with seasonal change in incidence of and mortality from cardiovascular disease.15, 16
Compared with conventional office BP, home BP is a useful tool17, 18, 19, 20, 21 that is highly reproducible22 and reliable for predicting cardiovascular complications23, 24, 25 and renal function.26 Continuous self-measurement of home BP is supposed to enable the capture of a large amount of BP information on long-term changes, such as seasonal variation in BP. However, most studies on seasonal variation with home BP to date have either analyzed small populations to clarify differences in BP between summer and winter,2, 3, 4, 9, 10, 11, 14 had follow-up for a single year only2, 3, 4, 10 or the same patients were not followed-up.5 Furthermore, it is unclear whether summer–winter difference in BP is modified over time under antihypertensive treatment.
We conducted the multicenter Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) trial,27 in which eligible patients measured home BP daily during the follow-up period. Along with accurate information on antihypertensive drug medication, we investigated multiyear seasonal variation in home BP among treated hypertensive patients using a model-based mathematical approach.
Methods
HOMED-BP trial
The present study was part of the multicenter HOMED-BP controlled trial (2001–2010) that aimed to establish the long-term benefits of clinical practice based on self-measured home BP.27 In the HOMED-BP, participants with mild-to-moderate hypertension with a minimum age of 40 years were recruited throughout Japan. Participants were treatment-naive patients and previously treated patients for whom antihypertensive treatment would be discontinued for ⩾2 weeks. Off treatment, participants had to maintain a self-measured home BP of 135–179 mm Hg systolic BP or 85–119 mm Hg diastolic BP. In a 2 × 3 factorial design, 3518 eligible patients were randomized to tight (n=1759; targeting <125/<80 mm Hg) or usual (n=1759; targeting 125–134/80–84 mm Hg) control of home BP and to the initiation of antihypertensive drug treatment with angiotensin-converting enzyme inhibitors (ACEIs; n=1172), angiotensin receptor blockers (ARBs; n=1175) or calcium channel blockers (CCBs; n=1171). Antihypertensive drug medications were titrated based on home BP level.
The HOMED-BP protocol complies with the Helsinki Declaration for Investigation of Human patients28 and is registered with the UMIN Clinical Trial Registry (#C000000137; http://www.umin.ac.jp/ctr). The institutional review board of the Tohoku University Graduate School of Medicine approved the study protocol, and all study participants provided written informed consent before the treatment designated in the protocol.
Selection of eligible patients
Of the 3518 HOMED-BP patients, 1649 hypertensive patients with morning home BP data for ⩾52 weeks after the first year, that is, a total of ≈2 years or more since randomization, were investigated in the present study. Home BP data within the first year after randomization were excluded to minimize the influence of frequent titration of the initial antihypertensive treatment.
Home BP measurement and evaluation
In HOMED-BP, all patients were asked to measure BP and heart rate after ⩾2 min rest in a sitting position every morning throughout the study. These measurements were required to be obtained within 1 h of waking, before breakfast and before taking antihypertensive medications, in accordance with Japanese guideline for home BP monitoring.21 Validated oscillometric OMRON HEM-747IC-N monitors (Omron Healthcare, Kyoto, Japan),29 which store up to 350 readings in memory, were supplied to patients for self-measurement of BP at home. At each clinic visit, the recorded home BP values with the information of antihypertensive drugs were uploaded by physicians via a local computer to the HOMED-BP data server. Home BP was averaged on a weekly basis to reduce the effect of day of the week on BP, and averaged home BP values calculated from <5 measurements in a week were treated as missing values. Representing 1 year as 52 weeks, we included December 31 and February 29 (when applicable) in week 52 and week 9 of each year, respectively, with those weeks thus covering 8 days.
Statistical analyses with mathematical modeling methods
Weekly averaged systolic and diastolic home BPs were fitted to the following cosine function, applying PROC NLMIXED procedure as a nonlinear mixed effect model (Figure 1) using SAS version 9.3 software (SAS Institute, Cary, NC, USA):
The concept of fitting analysis in the basic seasonal variation model. BPvar is the maximum–minimum difference in home blood pressure (BP) in one cycle (mm Hg); Tfreq is the time (weeks) required for one cycle of home BP variation; Tmax is the time (weeks) at which home BP reached the first maximum point after 1 January; and BPref is a reference point for variation (mm Hg). This figure shows an ideal curve assuming BPvar=10 mm Hg, Tfreq=52 weeks, Tmax=10 weeks and BPref=140 mm Hg. Home BP data in the first year after randomization were excluded, and data for the present study were provided from week 53 onwards. When Tfreq is exactly 52 weeks, the curve illustrates complete seasonal variation.

where BPvar is the maximum–minimum difference of home BP in one cycle of the cosine curve (mm Hg), Tfreq is the time required for one cycle of home BP variation (weeks) and Tmax is the time at which home BP reached the first maximum point from 1 January (weeks). ‘W’ denotes the time (weeks) and ‘W’ of ‘1–52’ indicates ‘1 January to 31 December’ in the year in which each patient was randomized. Other effects consisted of the effects of the defined daily dose (DDD),30 KDDD (mm Hg per unit) and the elapsed time from randomization in the HOMED-BP study, KTime (mm Hg per year), to adjust for the effects of BP change induced by participation in the study, including antihypertensive drug titration. The intercept is BPref, a reference point for home BP variation. To detect between-patient variability, random effects were assumed for the maximum–minimum difference (BPvar) and the intercept (BPref). A cosine curve was incorporated for the model because it expressed a cyclic and symmetric curve.
Pearson’s correlation coefficients between individual weekly averaged home BP and estimated home BP by the assumed models (empirical Bayes estimates) were computed to confirm whether systolic and diastolic models appropriately predicted actual observed home BP. We further assumed a fully adjusted model on seasonal variation to explore independent factors associated with seasonal variation in home BP within the following covariates: body mass index (BMI); age; sex; diabetes mellitus; hypercholesterolemia; previous cardiovascular disease; current smoking; current habitual drinking; the region of the outpatient clinic where enrolled patients were followed-up (Northern Japan: Hokkaido and Tohoku regions, n=678; Southern Japan: Kanto, Chubu, Kansai, Chugoku, Shikoku, and Kyushu-Okinawa regions, n=971); the elapsed years from randomization in the HOMED-BP study; and 2 × 3 randomized groups (tight or usual control and initial therapy with ACEIs, ARBs or CCBs). Values of P⩽0.05 were considered significant throughout the analysis.
Analyses for evening home BP
Patients enrolled in HOMED-BP were optionally instructed to perform evening home BP measurement just before going to bed (n=1284). Evening home BP was analyzed in the same manner as morning home BP described above for further investigation.
Results
Characteristics of eligible patients
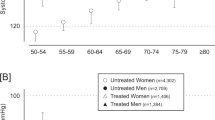
Baseline characteristics among 1649 eligible patients are shown in Table 1. At baseline, the mean age was 61.5 years and pretreatment home systolic/diastolic BP was 151.7/89.1 mm Hg. Median follow-up from randomization to the last measurement of home BP was 5.7 years (interquartile range, 4.2–7.2 years), and the median number of weeks for which home BP data were available per patient was 178 weeks. The time course of home BP per week is shown in Figure 2a; the number of provided weekly averaged home BPs increased until 104 weeks, that is, 2 years after 1 January of the randomization year as the initiation day varied and we enrolled home BP data from 1 year after the randomization. Measurement points regularly dipped three times per year matching the major vacation periods in early May (consecutive holidays), mid-August (traditional summer vacation) and late December to early January (New Year’s holiday) in Japan. In total, 309 081 weekly averaged points for morning home BP were evaluated. In general, study doctors adjusted antihypertensive drugs along with the seasons (Figure 2b), and the intension of treatment, represented as DDD, gradually increased through the study period (P<0.0001), although the magnitude of the increase was small (∼0.2 units).
(a) Number of provided weekly averaged morning home blood pressure (BP) data for the morning recording group. The number of points increased during weeks 53–104 because the week of randomization in HOMED-BP (Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure) study differed among enrolled patients. (b) The defined daily dose of antihypertensive medications for the morning recording group. Medication was adjusted along with seasons and defined daily dose was gradually increased.
Seasonal variation models
Basic seasonal variation models converged in all parameters (P<0.0001), and estimated means in each parameter are shown in Table 2. Seasonal variation was confirmed by a 52.1-week cycle, Tfreq, that indicates that a 1-year cycle can be defined in the current analysis. The maximum–minimum difference in systolic/diastolic home BP, BPvar, was 6.7/2.9 mm Hg (95% confidence intervals: 6.4–6.9/2.8–3.1 mm Hg). The corresponding s.d. for the maximum–minimum difference was 5.8/3.2 mm Hg. The highest home BPs in systolic and diastolic values were both observed on 19 January that is, 2.6 weeks from 1 January as denoted by Tmax. Home systolic and diastolic BP decreased along with the DDD (KDDD: −1.37/−0.81 mm Hg per unit, P<0.0001) and elapsed time from randomization (KTime: −0.37/−0.58 mm Hg per year, P<0.0001). Figure 3 illustrates the long-term seasonal trend in home BP among study patients. Estimated weekly averaged home BP by the basic models correlated significantly with observed home BP levels (r=0.76/0.87 in systolic/diastolic home BP, P<0.0001).
In fully adjusted seasonal variation models that included clinical characteristics at baseline (Table 3), maximum–minimum differences in home BP showed an increasing trend along with lower BMI and older age, and significantly larger differences were observed in men (vs. women, 0.57 mm Hg in systolic and 0.22 mm Hg in diastolic, P<0.0001), in patients with diabetes (vs. without diabetes, 1.05 mm Hg in systolic and 0.32 mm Hg in diastolic, P<0.0001) and in patients living in Southern Japan (vs. in Northern Japan, 1.48 mm Hg in systolic and 0.99 mm Hg in diastolic, P<0.0001). The amplitude of seasonal variation in home BP gradually decreased as time elapsed from randomization in the study (0.14/0.04 mm Hg per year, P⩽0.0002). Larger amplitude of seasonal variation in systolic BP was observed in the ACEI group compared with other treatment groups (vs. ARBs: 0.23 mm Hg, P=0.0100; vs. CCBs: 0.18 mm Hg, P=0.0466), whereas larger variation in diastolic BP was observed in the ARB group compared with other treatment groups (vs. ACEIs: 0.13 mm Hg, P=0.0109; vs. CCBs: 0.13 mm Hg, P=0.0104). Statistically significant differences were not observed in other comparisons between treatment groups (ARBs vs. CCBs in systolic and ACEIs vs. CCBs in diastolic, P⩾0.55). Larger seasonal variation in diastolic BP was observed in the usual control group (vs. tight control group: 0.13 mm Hg, P=0.0013).
Analyses for evening home BP
Baseline characteristics, parameters in the basic seasonal variation model and long-term seasonal trend among 1284 patients with evening home BP were generally consistent with the aforementioned 1649 patients with morning home BP, as shown in Supplementary Tables S1 and S2 and Supplementary Figure S1, respectively. Estimated weekly averaged home BP captured in the evening correlated significantly with observed home BP levels (r=0.81/0.86 in systolic/diastolic home BP, P<0.0001). In the fully adjusted seasonal variation models (Supplementary Table S3), individual characteristics were similarly associated with maximum–minimum differences in evening home BP. Meanwhile, differences in evening BP were larger in those who currently drink (vs. those who do not currently drink, 0.82 mm Hg in systolic and 0.64 mm Hg in diastolic, P<0.0001) and the difference in evening diastolic BP was small in patients with diabetes compared with patients with normal glucose metabolism (0.22 mm Hg, P=0.0013). In addition, a smaller amplitude of seasonal variation in systolic and diastolic BP was observed in the CCB group (vs. ACEIs: −0.31 mm Hg, P=0.0025; vs. ARBs: −0.37 mm Hg, P=0.0004 in systolic and vs. ACEIs: −0.20 mm Hg, P=0.0011; vs. ARBs: −0.21 mm Hg, P=0.0005 in diastolic). A larger seasonal variation in systolic BP was observed in the usual control group (vs. tight control group: 0.29 mm Hg, P=0.0005).
Discussion
The present study is the first report to investigate the long-term seasonal trend of home BPs derived from weekly averaged BP levels. Regarding the basic and fully adjusted seasonal variation models, we found that: (1) the cycle of the cosine curve significantly represented seasonal variation in this population; (2) home BP was maximal in mid-to-late January and minimal in mid-to-late July, and differences were 6.7/2.9 mm Hg in the morning and 5.5/2.7 mm Hg in the evening; (3) men, elderly and underweight patients showed large maximum–minimum seasonal differences, whereas drinking habits significantly strengthened differences in evening home BP, but not in morning home BP, between summer and winter; and (4) the amplitude of seasonal variation in BP changed significantly, but only ⩽0.14 mm Hg per year, under antihypertensive treatment.
We assumed the cosine function model (basic model) and further constructed the multivariable-adjusted model (fully adjusted model) for seasonal variation. The basic model clearly illustrated seasonal variation in home BP given the parameter for the time required for 1 cycle of home BP variation (Tfreq) was 52.1 weeks, and the estimated weekly averaged home BP strongly correlated with the observed home BP levels (r⩾0.76). The cosine function model therefore enables us to express the yearly seasonal variation in home BP among patients under monotherapy or combination therapy with antihypertensive drug treatment. Effects of confounders were appropriately observed in the fully adjusted models.
Within the seasonal variation, the highest home BP was observed in mid-to-late January whereas the lowest home BP was observed in mid-to-late July. This timing was essentially similar regardless of morning (Figure 3) or evening (Supplementary Figure S1) home BP measurements. The overall seasonal trend, for example, higher BP in winter and lower BP in summer, was similarly observed in previous studies using office BP5, 6, 8, 13 and 24 h ambulatory BP.3, 5, 12, 14 Fedecostante et al.,12 however, reported that nighttime ambulatory systolic BP measured from 2200 to 0600 h was significantly higher in summer (2.3 mm Hg, P=0.005). This divergence from our findings may indicate different features between awake evening home BP and sleeping ambulatory BP. Sleep quality may be related to nighttime ambulatory BP, particularly in regions without common use of air conditioners, as investigated by Fedecostante et al.12 Conversely, significantly higher BP in winter than summer was reported for daytime BP measured from 0600 to 2200 h (2.4 mm Hg in systolic and 2.2 mm Hg in diastolic, P⩽0.001),12 consistent with our findings for home BP.
The estimated maximum–minimum BP difference in systolic/diastolic (BPvar) was 6.7/2.9 mm Hg with between-patient variability (σ1, 5.8/3.2 mm Hg as the s.d.). These findings are compatible with studies conducted in the same climate region, that is, the temperate zone.2, 3, 5 In contrast, summer–winter office BP differences were 17.0/9.0 mm Hg in Iraq8 and 2.1/1.1 mm Hg in Norway.13 Hozawa et al.11 reported that the increase in BP along with lowering outside temperature was attenuated below 10 °C. The distinguishing difference in duration of low outside temperature ⩽10 °C among Iraq, Norway and Japan31 may explain these inconsistent results; elevated BP during winter is expected to be diminished in subarctic regions such as Norway because of the long duration with a low temperature ⩽10 °C. This attenuation of BP increase in winter might be explained by room temperatures modified by heating systems.11 In contrast, populations in comparatively hot areas closer to the Equator showed larger seasonal variations in BP.32 In the present study, this effect of latitude for BP variability was observed even within Japan; larger seasonal variation in systolic and diastolic BP, by 1.48/0.99 mm Hg, was observed in Southern Japan. The wide difference in climates around the world would contribute to differences in seasonal variations in BP.
The present findings regarding summer–winter difference in morning home BP are supported by previous reports in relation to increasing age,33 men33 and positive smoking status.34 Meanwhile, associations between BMI and seasonal variation remain controversial.33, 35, 36 Some studies33, 35 have found no relationship between BMI and summer–winter difference in BP, whereas Kristal-Boneh et al.36 reported an inverse correlation between BMI and mean summer–winter change in systolic BP captured in the clinical setting. The presence of diabetes mellitus was associated with seasonal variation in morning home BP, and drinking habits associated with evening home BP in the present study. However, these effects of diabetes mellitus and drinking habits on seasonal variation in BP have not been reported previously, and the clinical significance of such confounders on seasonal BP variation needs to be investigated. Predefined 2 × 3 randomized groups in the HOMED-BP study were also statistically associated with seasonal variation. However, the differences between the groups were small (⩽0.37 mm Hg in systolic and ⩽0.21 mm Hg in diastolic) and inconsistent between systolic and diastolic BP or between morning and evening measurements, suggesting that these differences were clinically less meaningful.
The complex models with home BP in the present analyses had several advantages. The models can minimize the inevitable effect of possible outliers that exaggerate the maximal–minimal differences. Furthermore, the nonlinear mixed model can include patients with insufficient amounts of data that resulted in maintaining the population size in the analysis and in finding out the primary characteristics of seasonal variation from numerous data. These features enabled us to precisely estimate the amplitude of seasonal variation and timing of maximum and minimum BP with the cosine curve.
The present study has some potential limitations. First, the HOMED-BP trial was not designed specifically to investigate the seasonal variation in BP. Although models with large numbers of home BP measurements converged (P<0.0001) and appear to have appropriately illustrated the seasonal variation in BP, the lack of detailed meteorological parameters related to individual patients might have biased the present results; in particular, records of indoor temperatures were not available, and a thermometer was not installed into the sphygmomanometer we used in the present study. Furthermore, enrolled patients lived throughout Japan, and their precise locations were not available, although a rough estimation of location, that is, northern and southern part of Japan, was applied according to the clinic address. Second, antihypertensive drug medication was titrated based on home BP level during the study period that might have affected the seasonal variation in home BP. However, detailed information on prescribed medications was included in the models, allowing us to show the precise home BP variation. We standardized the varied antihypertensive drug effect using DDD as adjusted in the model. DDD should be used as the sole standard dose unit in all pharmacoepidemiologic studies as no other proposed standards, namely, the minimum marketed dose, the equipotential dose, the average daily dose and the nonstandard prescribed daily dose, appeared to offer any advantage over DDD.37 Nevertheless, even adjustment by DDD is not perfect to completely eliminate the effect of change in antihypertensive medications in this post hoc analysis. Home BP significantly decreased throughout the follow-up period, suggesting that steady titration of antihypertensive drug medication and improvement of lifestyle might have contributed to lowering home BP. Third, we focused on the hypertensive population and not on individual patients; therefore, the diversity of seasonal variation in BP was not sufficiently investigated. However, our findings would be useful for population strategy in the long-term management of hypertension. Fourth, the amplitude of seasonal variation in home BP was statistically reduced during the follow-up period under antihypertensive treatment. Although it reached 0.70 mm Hg during at most 5 years and this effect was appropriately adjusted for in the model, the long-term seasonal trend in home BP under antihypertensive drug medication, for example, ⩾10 years, remains unclear. Finally, because the present models consisted of a simple trigonometric function, the duration between time points for maximum–minimum home BP was inevitably half of the time required for 1 cycle of home BP variation, that is, 26 weeks. The lowest and highest temperatures in Japan are generally observed in January and August, respectively,31 whereas the present study showed the highest BP in January and the lowest BP in July, mainly because of the cosine model. However, this discrepancy can be further explained based on the following: (1) BP is affected by measurement conditions such as room temperature38 and weather;39 and (2) seasonal variation in BP is related to hours of daylight40 and the availability of air conditioning or heating.41 Seasonal variation in BP is thus attributable to numerous complex factors. A more complex function, for example, a sum of multiple trigonometric functions and trigonometric series, might also express the seasonal variation in BP, although such functions may obfuscate clinical meanings of the analysis.
In conclusion, we observed the highest and lowest home BPs in mid-to-late January and mid-to-late July, respectively, among hypertensive patients on antihypertensive pharmacotherapy who were followed-up for a median of 5.7 years. The cosine curve model appropriately predicted multiyear week-to-week seasonal home BP variation. Age, BMI, sex, diabetes mellitus and drinking habits may influence the maximum–minimum difference in seasonal home BP variation. Summer–winter difference in home BP was essentially the same every year, though marginally reduced, throughout the study period under antihypertensive treatment. Although the impact of this study has not been fully elucidated in clinical practice, we emphasize that daily home BP measurements enable us to capture long-term conditions, such as seasonal variation, in patients. Home BP should therefore be carefully monitored, particularly in patients with increased BP in winter, to mitigate cardiovascular risk. Ultimately, seasonal variation should be studied in a large population of untreated hypertensive patients or normotensive individuals, and we should clarify whether seasonal variation in BP predicts prognosis and whether it can be controlled by intervention.
References
Rose G . Seasonal variation in blood pressure in man. Nature 1961; 21: 189–235.
Imai Y, Munakata M, Tsuji I, Ohkubo T, Satoh H, Yoshino H, Watanabe N, Nishiyama A, Onodera N, Kato J, Sekino M, Aihara A, Kasai Y, Abe K . Seasonal variation in blood pressure in normotensive women studied by home measurements. Clin Sci (Lond) 1996; 90: 55–60.
Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S . Seasonal variations in office, home and 24 h ambulatory blood pressure in patients with essential hypertension. J Hypertens 1996; 4: 1421–1425.
Minami J, Ishimitsu T, Kawano Y, Matsuoka H . Seasonal variations in office and home blood pressures in hypertensive patients treated with antihypertensive drugs. Blood Press Monit 1998; 3: 101–106.
Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, Mancia G . Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens 1998; 16: 1585–1592.
Thomas C, Wood GC, Langer RD, Stewart WF . Elevated blood pressure in primary care varies in relation to circadian and seasonal changes. J Hum Hypertens 2008; 22: 755–760.
Metoki H, Ohkubo T, Watanabe Y, Nishimura M, Sato Y, Kawaguchi M, Hara A, Hirose T, Obara T, Asayama K, Kikuya M, Yagihashi K, Matsubara Y, Okamura K, Mori S, Suzuki M, Imai Y BOSHI Study Group. Seasonal trends of blood pressure during pregnancy in Japan: the babies and their parents' longitudinal observation in Suzuki Memorial Hospital in Intrauterine Period study. J Hypertens 2008; 26: 2406–2413.
Al-Tamer YY, Al-Hayali JM, Al-Ramadhan EA . Seasonality of hypertension. J Clin Hypertens (Greenwich) 2008; 10: 125–129.
Kimura T, Senda S, Masugata H, Yamagami A, Okuyama H, Kohno T, Hirao T, Fukunaga M, Okada H, Goda F . Seasonal blood pressure variation and its relationship to environmental temperature in healthy elderly Japanese studied by home measurements. Clin Exp Hypertens 2010; 32: 8–12.
Takenaka T, Kojima E, Sueyoshi K, Sato T, Uchida K, Arai J, Hoshi H, Kato N, Takane H, Suzuki H . Seasonal variations of daily changes in blood pressure among hypertensive patients with end-stage renal diseases. Clin Exp Hypertens 2010; 32: 227–233.
Hozawa A, Kuriyama S, Shimazu T, Ohmori-Matsuda K, Tsuji I . Seasonal variation in home blood pressure measurements and relation to outside temperature in Japan. Clin Exp Hypertens 2011; 33: 153–158.
Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessì-Fulgheri P, Sarzani R . Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J Hypertens 2012; 30: 1392–1398.
Hopstock LA, Barnett AG, Bønaa KH, Mannsverk J, Njølstad I, Wilsgaard T . Seasonal variation in cardiovascular disease risk factors in a subarctic population: the Tromsø Study 1979–2008. J Epidemiol Community Health 2013; 67: 113–118.
Stergiou GS, Myrsilidi A, Kollias A, Destounis A, Roussias L, Kalogeropoulos P . Seasonal variation in meteorological parameters and office, ambulatory and home blood pressure: predicting factors and clinical implications. Hypertens Res 2015; 38: 869–875.
The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet 1997; 349: 1341–1346.
Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, Collins R, Peto R, Liu Y, Yang R, Zhang Y, Li G, Liu S, Chen Z China Kadoorie Biobank Study Collaboration. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J 2015; 36: 1178–1185.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O'Brien E, Ohkubo T, Padfield P, Palatini P, Pickering T, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens 2008; 26: 1505–1526.
Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, Tsuchihashi T, Ohkubo T, Kuwajima I, Miyakawa M Japanese Society of Hypertension Committee for Guidelines for Self-monitoring of Blood Pressure at Home. The Japanese Society of Hypertension Guidelines for Self-monitoring of Blood Pressure at Home (Second Edition). Hypertens Res 2012; 35: 777–795.
Stergiou GS, Baibas NM, Gantzarou AP, Skeva II, Kalkana CB, Roussias LG, Mountokalakis TD . Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens 2002; 15: 101–104.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S . Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G . Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation 2005; 111: 1777–1783.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y Ohasama Study. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens 2004; 22: 1099–1104.
Ishikura K, Obara T, Kikuya M, Satoh M, Hosaka M, Metoki H, Nishigori H, Mano N, Nakayama M, Imai Y, Ohkubo T J-HOME-Morning Study Group. Home blood pressure level and decline in renal function among treated hypertensive patients: the J-HOME-Morning Study. Hypertens Res 2016; 39: 107–112.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP). Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35: 1102–1110.
World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997; 277: 925–926.
Chonan K, Kikuya M, Araki T, Fujiwara T, Suzuki M, Michimata M, Hashimoto J, Ohkubo T, Hozawa A, Yamamoto N, Miyawaki Y, Matsubara M, Imai Y . Device for the self-measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit 2001; 6: 203–205.
World Health Organization. World Health Organization Collaborating Centre for drug statistics methodology system of defined daily doses. http://www.whocc.no/atc_ddd_index. Accessed 1 December 2015.
World Weather Onlinehttp://www.worldweatheronline.com/. Accessed 1 December 2015.
Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ WHO MONICA Project. The effect of temperature on systolic blood pressure. Blood Press Monit 2007; 12: 195–203.
Tu YK, Chien KL, Chiu YW, Ellison GT . Seasonal variation in blood pressure is modulated by gender and age but not by BMI in a large Taiwanese population, 1996-2006. J Am Soc Hypertens 2013; 7: 216–228.
Kristal-Boneh E, Harari G, Green MS . Seasonal change in 24-hour blood pressure and heart rate is greater among smokers than nonsmokers. Hypertension 1997; 30: 436–441.
Nakajima J, Kawamura M, Fujiwara T, Hiramori K . Body height is a determinant of seasonal blood pressure variation in patients with essential hypertension. Hypertens Res 2000; 23: 587–592.
Kristal-Boneh E, Harari G, Green MS, Ribak J . Body mass index is associated with differential seasonal change in ambulatory blood pressure levels. Am J Hypertens 1996; 9: 1179–1185.
Merlo J, Wessling A, Melander A . Comparison of dose standard units for drug utilisation studies. Eur J Clin Pharmacol 1996; 50: 27–30.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, Kurumatani N . Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens 2014; 32: 1582–1589.
Morabito M, Crisci A, Orlandini S, Maracchi G, Gensini GF, Modesti PA . A synoptic approach to weather conditions discloses a relationship with ambulatory blood pressure in hypertensives. Am J Hypertens 2008; 21: 748–752.
Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, Gensini GF, Parati G . Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension 2013; 61: 908–914.
Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, Whitlock G, Yang L, Collins R, Chen J, Wu X, Wang S, Hu Y, Jiang L, Yang L, Lacey B, Peto R, Chen Z China Kadoorie Biobank study collaboration. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012; 30: 1383–1391.
Acknowledgements
We are grateful to all HOMED-BP study collaborators as listed previously27 for their valuable contribution. The Japanese Society of Hypertension endorsed the HOMED-BP trial. This study was funded by grants from the Japan Cardiovascular Research Foundation, the Japan Arteriosclerosis Prevention Fund and Tohoku University. Fujitsu Systems East (Tokyo, Japan) and Omron Healthcare (Kyoto, Japan) developed and maintained the internet-based infrastructure for the measurement of blood pressure at home and the management of patients. Part of this work was presented at the 25th European Meeting on Hypertension and Cardiovascular Protection (Milan, Italy, 2015).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
TH is a full-time employee of GlaxoSmithKline. TH is also a graduate student at Tohoku University and has contributed to this study independently of GlaxoSmithKline. Omron Healthcare provided research support to YI and HM. The other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Hanazawa, T., Asayama, K., Watabe, D. et al. Seasonal variation in self-measured home blood pressure among patients on antihypertensive medications: HOMED-BP study. Hypertens Res 40, 284–290 (2017). https://doi.org/10.1038/hr.2016.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.133
Keywords
This article is cited by
-
Seasonal variation in the effect of antihypertensive treatment with the irbesartan/hydrochlorothiazide combination
Hypertension Research (2023)
-
Gender-specific effect of outdoor temperature and seasonal variation on blood pressure components: a cross-sectional study on Iranian adults from 2015 to 2018
Environmental Science and Pollution Research (2023)
-
Novel insights into the association between seasonal variations, blood pressure, and blood pressure variability in patients with new-onset essential hypertension
BMC Cardiovascular Disorders (2022)
-
Temperature, cardiovascular mortality, and the role of hypertension and renin–angiotensin–aldosterone axis in seasonal adversity: a narrative review
Journal of Human Hypertension (2022)
-
Update on Hypertension Research in 2021
Hypertension Research (2022)