Abstract
Several modifiable risk factors have been shown to lower blood pressure, but little is known about their combined risk in Chinese individuals. In this prospective cohort study, we followed 2751 subjects aged 18–60 years in the China Health and Nutrition Survey who were free of diagnosed hypertension, cardiovascular disease, diabetes or cancer at baseline in 2000. The associations between each of the risk factors and the risk of developing incident hypertension were analyzed by gender. The three low-risk factors for hypertension were a body mass index (BMI) between 18.5 and 24, a moderate or heavy physical activity level ⩾0.5 h per day and a high score on the Dietary Approaches to Stop Hypertension (DASH) diet. Low-risk factors were combined to assess their effects on the risk of hypertension. During the 11-year follow-up, we documented 1147 cases of hypertension. Three risk factors were independently associated with the risk of hypertension even after adjustment for age, alcohol intake and smoking status. Adopting all three low-risk lifestyle factors (normal BMI, DASH-style diet and physical activity) could prevent 38% (95% confidence interval (CI), 19–53%) of new hypertension cases among women and 43% (95% CI, 25–57%) of new hypertension cases among men. Adherence to a healthy lifestyle and a DASH-style diet was associated with a lower risk of hypertension.
Similar content being viewed by others
Introduction
Hypertension is one of the most important risk factors for cardiovascular disease, accounting for nearly 45% of cardiovascular disease morbidity and mortality globally.1 In China, the prevalence of hypertension in adults has increased from 14.5% to 21.4% from 1991 to 2009, respectively.2 Given this epidemic of hypertension in China, only 22.8% of individuals with hypertension were treated; only 6.1% of those had their blood pressure (BP) controlled in 2009.2 Many modifiable risk factors for hypertension have been studied independently, including being obese,3 not participating in physical inactivity4 and having an unhealthy diet.5 The effects of interventions that modify one or several of these factors have been documented.6, 7 Compared with the costly pharmacologic management of hypertension, lifestyle and dietary interventions that focus on a combination of modifiable risk factors can prevent hypertension in a cost-effective way. Although a body of evidence on the combined effects of lifestyle risk factors on hypertension has been reported in Western populations,8 data for a Chinese population are still limited. We, therefore, investigated the relationship between combinations of low-risk lifestyle factors and the risk of developing hypertension using data from an ongoing prospective cohort study in China, the China Health and Nutrition Survey (CHNS).
Methods
Study design and subjects
The CHNS is a large-scale, longitudinal survey that was designed to explore how the health and nutritional status of the Chinese population has been affected by social and economic changes.9 A multistage, random cluster process was used to draw the sample surveyed in each of the following provinces from northeast to southwest: Heilongjiang, Liaoning, Jiangsu, Shandong, Henan, Hubei, Hunan, Guizhou and Guangxi. Information on age, gender, region, body mass index (BMI) and BP measurements was collected. The sampling design has been fully described elsewhere.9
The CHNS surveys were conducted in 1989, 1991, 1993, 1997, 2000, 2004, 2006, 2009 and 2011. Because of the high quality of data from 2000, it was defined as the baseline year. A total of 11 972 subjects participated in the CHNS in 2000. Of these subjects, 5742 were excluded for the following exclusive reasons at baseline in 2000: (1) the subject was younger than 18 or older than 60 years(n=4167); (2) the subject had missing average systolic blood pressure (SBP) or diastolic blood pressure data (if a subject had two or three measurements, we used the average of the measurements, and if a subject had only one measurement, then we used that measurement) (n=631); (3) the subject was identified to have hypertension in the baseline survey (n=2055); (4) the subject took antihypertensive medications (n=455); or (5) the subject had an existing diagnosis of diabetes (n=129), myocardial infarction (n=49) or apoplexy (n=66). Of the remaining 6230 subjects, 44.2% participated in all five successive follow-up surveys (2000–2011) with valid data, leading to a study population of 2751 subjects aged 18–60 years at baseline. Compared with the subjects (n=2751), those who did not complete the study (n=3479) were, on average, younger (36 vs. 42 years), were more often men (49.0% vs. 42.3%), had a slightly lower BMI (22.4 vs. 22.7 kg m−2) and performed moderate or heavy physical activity time less often (3.4 vs. 3.8 h per day) (P<0.05 for all comparisons), while there were no significant differences in average BP (112.5/73.9 vs. 113.0/74.0 mm Hg) and Dietary Approaches to Stop Hypertension (DASH) score (20.4 vs. 20.5) between non-completers and completers (P>0.05). Moreover, according to the methodology described by Hildrum et al.10, we tested for the effect modifications of sex and age by incorporating interaction terms into the models.10, 11 However, we found no interaction between age or sex and the association between DASH-style diet/BMI/physical activity and hypertension (P>0.10 for all interactions) (data not shown). Therefore, we did not expect non-completers to bias our findings.11 We defined hypertension as having an average SBP⩾140 mm Hg, an average diastolic blood pressure ⩾90 mm Hg, currently undergoing treatment with an antihypertensive medication, or having received a previous diagnosis by a physician.
Dietary data collection and definition
Diet data were collected at the household level using weighing methods and at the individual level using three consecutive 24-h dietary recalls12, 13 on the same three consecutive days. All the foods and condiments that were in the home inventory, purchased from markets and picked from gardens were carefully recorded and measured at the start of the first 24-h dietary recall and at the end of the last 24-h dietary recall in the survey. The days of the 24-h dietary recall were selected randomly from Monday to Sunday in each community. Dietary intake (for example, vegetables and meat) at the individual level was surveyed by 24-h recalls by asking the individuals to report all food consumed each day while they were away from home and at-home. On the same three consecutive days, we directly and accurately weighed intakes of condiments (that is, salt, soy sauce and monosodium glutamate) at the household level, estimated salt intake based on the consumption of condiments according to the Chinese food composition table (FCT)14 and allocated a proportion of salt consumed at the household level to each individual based on their meal consumption frequency.
To evaluate the overall dietary quality,15 a DASH score was calculated based on the dietary data. The details of this score can be found elsewhere.16 In brief, the DASH score recommends a high intake of five food components: fruits, vegetables, nuts and legumes, low-fat dairy products and whole grains; it also recommends a low intake of three food components: sodium, sweetened beverages, and red and processed meats.
Each subject’s dietary data were collected at baseline in 2000, and then the dietary data were updated with every survey during the period from 2000 to 2011. To obtain the best estimate of long-term dietary intake, we used the cumulative-update method,17 which takes the average of all previous dietary data. For each of the components, men and women were separately classified into quintiles according to their cumulative mean intake. A point from 1 to 5 was given according to the subject’s sex-specific quintile ranking for the eight food components, making the total score range from 8 to 40. Of the 2751 subjects in our final sample, 88.6% did not consume low-fat dairy products, 75.3% did not consume nuts and 58.6% did not consume fruits (those who did not consume the component were assigned 1 point, the lowest quarter was assigned 2 points and the fourth quarter was assigned 5 points). The component scores for vegetables and whole grains were assigned according to the participant’s quintile ranking (that is, quintile 1 was assigned 1 point and quintile 5 was assigned 5 points). For salt, red and processed meats, and sweetened beverages, a low intake was desired (the lowest quintile was assigned a score of 5 points and the highest quintile was assigned a score of 1 point, except for sweetened beverages). Of the subjects, 79.5% did not consume sweetened beverages (those who did not consume the component were assigned 5 points, the lowest quarter was assigned 4 points and the fourth quarter was assigned 1 point).
Non-dietary data collection
Physical activity was defined as the combination of occupational activities, home activities and leisure-time physical activities. On the basis of the model proposed by Pate et al.18 that classifies the metabolic equivalent intensity of physical activities, moderate physical activity was activity performed at an intensity from 3 to 6 metabolic equivalents (vigorous physical activity, >6 metabolic equivalents). We collected the amount of time that each subject spent doing moderate or vigorous physical activities (⩾3 metabolic equivalents), including carrying small children, mopping, running and performing other aerobic activities.19
The data on demographics (age, sex and living area), BP, BMI (calculated as weight in kilograms divided by height in meters squared), lifestyle (ever smoking, alcohol intake) and the use of medications were collected by trained and certified health professionals through interviews and physical examinations. For smoking, the subjects were divided into four groups according to their smoking status (non-, ex-, current smoking, heavy smoking (those who smoked ⩾15 cigarettes per day)). For drinking, the subjects were divided into five categories according to their alcohol consumption (non-drinker, ex-drinker, 0.1~10, 10.1~25.0, >25 g per day).
After at least a 10-min rest, arterial BP was measured on the right arm (~25 mm above the elbow) in a sitting position using a mercury sphygmomanometer with the cuff maintained at the heart level. Blood pressure was measured three times during one visit, and the average of three reading was used in the analysis.
Definition of low-risk groups
The DASH diet has been shown in randomized controlled trails to lower BP,20 and in our study, the subjects whose DASH scores were in the top quintile (quintile 5) had a significantly lower hazard ratio (HR) for incident hypertension than subjects in the reference group. Consistent with this result, the subjects with high DASH scores were in quintile 5 and were classified as having a low-risk diet.
Initially, we considered defining the low-risk group according to five modifiable risk factors: (DASH-style) diet, BMI, physical activity, smoking and alcohol. However, smoking and drinking were not chosen for the present analysis because smoking was not associated with hypertension and light-to-moderate drinking increased the risk of hypertension in men based on the results of this study as shown in Table 1. Although light-to-moderate alcohol consumption decreased hypertension risk in women based on the results shown in Table 1, previous observational studies have demonstrated that modest alcohol use was associated with a lower risk of hypertension in women.21 However, the estimates in our study were somewhat imprecise because few women were in the light-to-moderate alcohol categories.
On the basis of the weight criteria for adults in China,22 a BMI<24 but >18.5 is defined as a normal weight, a BMI>24 is defined as overweight and a BMI>28 is defined as obese. In this study, normal weight was selected as the low-risk category for BMI.
Physical activity lowers BP and decreases hypertension risk,23 and in our study, performing moderate or heavy physical activities (metabolic equivalent ⩾3) for at least 0.5 h per day was defined as the low-risk physical activity.
Statistical analysis
The person-time for each subject was calculated from 2000 to either the date that hypertension was first diagnosed or 2011, whichever came first. For those who developed hypertension, the date of hypertension onset was assumed to be the day that hypertension was diagnosed.
Separate analyses were performed for women and men. The associations between each of the five modifiable risk factors and the risk of developing incident hypertension were analyzed by gender. A Cox proportional hazards regression was used to estimate the HR of incident hypertension and its 95% confidence interval (CI) for each risk factor. The multivariable models simultaneously adjusted for all these modifiable risk factors as well as for the potential confounders, including age, income, employment status, education, province and urban or rural region. We calculated the cumulative means for the time spent performing physical activities and for the dietary data. For all other risk variables and covariates apart from diet and physical activity, we used the most recent information.17
Then, we divided these factors into low- and high-risk categories according to the aforementioned methodology (‘Definition of Low-risk Groups’ section): DASH score (highest quintile vs. lower 4 quintiles); BMI (from 18.5 to 24 kg m−2 vs. other levels of BMI); and moderate or heavy physical activity (⩾0.5 h per day vs. <0.5 h per day). Separate analyses were performed for women and men. The associations between the combinations of low-risk factors and incident hypertension were analyzed using Cox proportional hazards regression. Subjects with a high DASH score were compared with all other subjects after adjusting for age, income, employment status, education, province, urban or rural region, smoking, alcohol intake, BMI and moderate or heavy physical activity time. Then, subjects with a combination of two low-risk factors, including DASH score and BMI, were analyzed. Finally, subjects with a combination of three low-risk factors, including DASH score, BMI and moderate or heavy physical activity time, were compared with all other subjects. The hypothetical population attributable risk (PAR) was calculated for each of these analyses under the assumption that the observed associations were causal with the following standard equation:

where Pe is the exposed proportion.8
To obtain the best estimate of PAR, we calculated the PAR by using the observed HR (calculated from 2751 subjects) with a more representative population of those aged 18–60 years (N=6230) at baseline.
Finally, we combined the sex-specific results to analyze the associations between combinations of risk factors and multivariable HR for hypertension among all subjects.
All statistical tests were performed using SAS statistical software version 9.1 (SAS Institute, Cary, NC, USA). All P-values were 2-tailed; P<0.05 was considered statistically significant.
Results
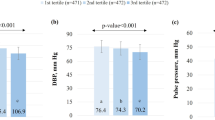
Table 2 shows the baseline characteristics of the participants. At baseline, in 2000, the mean (s.d.) age of the population was 42 (9.3) years old, and the mean (s.d.) BMI was 22.7 (2.9) kg m−2. During the 25 647 person-year follow-up, we documented 1147 cases of hypertension, and the incidence rate was 4.5 cases per 100 person-years. Subjects with a higher baseline SBP were more likely to be those with a higher baseline BMI, those who were older, or those who performed less physical activity per day.
To address whether a low-risk lifestyle was similarly associated with a lower hypertension risk between men and women, we stratified our analysis by gender. The multivariable adjusted associations between the five individual modifiable risk factors and incident hypertension are independently shown in Table 1 for men and women. Smoking was not significantly associated with incident hypertension in both men and women. However, after multivariable adjustment, the other four modifiable risk factors were associated with incident hypertension. Those who had a higher DASH score, who spent more time performing moderate or heavy physical activities per day and who had a normal BMI had a lower HR for incident hypertension regardless of gender. There was a dose–response relationship between the DASH score and the HR for incident hypertension; subjects with scores in the highest quintiles had a significantly lower HR than those with scores in the remaining quintiles for both men (0.62 (95% CI, 0.45–0.85)) and women (0.71 (95% CI, 0.53–0.94)). Men who performed 2 h per day of moderate or heavy physical activity had a HR for incident hypertension of 0.36 (95% CI, 0.27–0.47) relative to men who performed <0.5 h per day of moderate or heavy physical activity. Obese men had a HR for incident hypertension of 2.15 (95% CI, 1.55–2.98) relative to men who had a BMI<24 kg m−2 but >18.5 kg m−2. The association between alcohol intake and the risk of developing hypertension differed in men and women. We found that men in the highest level of alcohol intake (>25 g per day) had a HR for incident hypertension of 1.42 (95% CI, 1.05–1.93) relative to men who did not consume alcohol, with no evidence of benefit for those who consumed a light–moderate amount of alcohol (P>0.05). However, women who consumed a light–moderate amount of alcohol (10–25 g per day) had a HR for incident hypertension of 0.39 (95% CI, 0.15–0.96). For women who drank 25 g or more alcohol per day, there was a small but not significant increase in incident hypertension compared with non-drinkers.
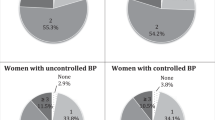
The associations between the combinations of risk factors and hypertension were stratified by gender (Table 3). Specifically, among men, the hypothetical PARs ranged from 16% (95% CI, 0–30%) for one low-risk factor to 43% (95% CI, 25–57%) for three low-risk factors. Among women, the hypothetical PARs ranged from 14% (95% CI, −2–28%) for one low-risk factor to 38% (95% CI, 19–53%) for three low-risk factors.
Table 4 shows the associations between the combinations of risk factors and the multivariable HR for hypertension among all subjects. Subjects with a DASH-style diet (in the highest quintile of DASH score) had a HR for incident hypertension of 0.85 (95% CI, 0.73–0.98). The hypothetical PAR was 12% (95% CI, 2–23%), suggesting that 12% of new-onset hypertension cases in this population could potentially be prevented if all subjects adopted this one low-risk factor of a DASH-style diet. The hypothetical PAR was 31% (95% CI, 18–43%) if the low-risk group further adopted a normal BMI (18.5–24 kg m−2) and rose to 40% (95% CI, 27–50%) if the low-risk group further adopted a daily moderate or heavy physical activity (three low-risk factors total).
Discussion
In this population-based prospective cohort study of an adult Chinese population, we found that Chinese adults with low-risk combinations of modifiable lifestyle factors were associated with dramatic reduction in the incidence of hypertension during follow-up. Moreover, based on the gender-stratified model (Table 3), we found that the association between a low-risk lifestyle and lower hypertension was similar among men and women. Among women, having three low-risk factors (a DASH-type diet, normal BMI and daily moderate or heavy physical activity) was associated with a HR for incident hypertension of 0.60 (95% CI, 0.45–0.80); the corresponding hypothetical PAR was 38% (95% CI, 19–53%), which was similar to previous findings.8
BMI, physical activity, a DASH-type diet and alcohol consumption have been shown to be independently associated with a risk of incident hypertension or changes in BP in various studies. A higher BMI has been shown to be associated with a higher risk of incident hypertension.24, 25 Compared with those who lowered their BMI, males and females who gained ⩾2.4 kg m−2 had a 1.68 or 1.42 times higher odds of becoming hypertensive, respectively.24 Daniels et al.26reported the following predicted increases in SBP per unit increase in BMI (mm Hg per kg m−2): 0.65±0.04 mm Hg per kg m−2 in whites and 0.52±0.04 mm Hg per kg m−2 in blacks (P<0.001). Higher physical activity levels also have been shown to be associated with a lower risk of incident hypertension. Subjects with low physical activity had a 1.27 times higher risk relative to subjects with high physical activity.27 Hallal et al.28 found that those who exceeded the 300-min moderate-to-vigorous physical activity threshold per week had a 2.6 mm Hg lower mean increase in diastolic blood pressure from 11 to 14 years old than those below the threshold. DASH-type diets, which are rich in fruits and vegetables but low in sweets, salt and high-fat protein sources, have been proven to lower BP. The longitudinal Chicago Western Electric Study found that men who consumed 0.5–1.5 cups per day compared with those who consumed <0.5 cups per day of fruits and vegetables were estimated to had a lower rise in SBP over 7 years (P<0.05).29 One study demonstrated that mean SBP significantly decreased by 4.5±7.5 mm Hg in response to decreased salt intake during the night.30 Modest alcohol consumption was associated with a lower risk of hypertension and heavy alcohol consumption was associated with an increased risk of hypertension in women.31 However, for men, a linear dose–response relationship was observed such that those consuming 50 g pure alcohol per day had a 1.57 higher risk and those consuming 100 g pure alcohol per day had a 2.47 higher risk than non-drinkers.32 These findings support our results.
In our study, although we found that multiple low-risk factors were significantly associated with a low risk of hypertension, the subjects may not benefit from DASH-type diets unless they strongly adhere to the diet recommendations. Health benefits could also be gained from physical activity. Subjects who performed 30 min of moderate or heavy physical activity per day could benefit, and those who spent more time performing moderate-intensity physical activities were also likely to derive more health benefits. Smoking is a strong risk factor for cardiovascular disease, but our data did not clearly present evidence of a direct relationship between smoking and hypertension. Our data indicated that light alcohol consumption could significantly reduce the risk of hypertension in women, and this finding was consistent with the finding from an earlier study31 that showed light-to-moderate alcohol consumption decreased hypertension risk in women and increased the risk in men. However, the estimates of our study were somewhat imprecise because there were only a few women in the light-to-moderate alcohol categories (Table 1). Thus, limiting alcohol intake should be advised for both men and women.
The limitations of the present study should be acknowledged. First, we did not have information about the subject’s family history of hypertension and other residual confounders; thus, the adjustment might be not perfectly comprehensive. Second, it is possible that the diet data that were gathered using weighing methods in combination with three consecutive 24-h dietary recalls does not represent the real diet data throughout the year, and some subjects may have had their DASH scores misclassified. Third, we categorized lifestyle factors into low-risk and high-risk groups to simplify the analysis, but the associations between these factors and hypertension risk are continuous. However, increasing the number of categories for each of the three risk factors would exponentially increase the number of possible low-risk factors, thereby making the calculation and presentation of the data overly complex and underpowered. Finally, the rate of follow-up in the study was limited; however, we do not expect non-completers to bias the associations that we have observed.
Conclusions
Although pharmacologic treatment of hypertension has been proven effective, our study supports that adherence to a low-risk diet and healthy lifestyle factors could prevent a substantial majority of incident hypertension cases in Chinese individuals. A decrease in SBP of 2 mm Hg would lower the risk of stroke mortality by ~10% and lower the risk of mortality from ischemic heart disease or other vascular causes by ~7% in middle age.33 The prevention of hypertension would have major public health benefits.
References
Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, Rodgers A, Murray CJ . Rethinking the ‘diseases of affluence’ paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med 2005; 2: 0404–0412.
Xi B, Liang Y, Reilly KH, Wang Q, Hu Y, Tang W . Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol 2012; 158: 326–329.
Niu J, Seo DC . Central obesity and hypertension in Chinese adults: a 12-year longitudinal examination. Prev Med 2014; 62: 113–118.
Ng SW, Norton EC, Popkin BM . Why have physical activity levels declined among Chinese adults? Findings from the 1991-2006 China Health and Nutrition Surveys. Soc Sci Med 2009; 68: 1305–1314.
Dauchet L, Kesse-Guyot E, Czernichow S, Bertrais S, Estaquio C, Péneau S, Vergnaud AC, Chat-Yung S, Castetbon K, Deschamps V, Brindel P, Hercberg S . Dietary patterns and blood pressure change over 5-y follow-up in the SU.VI.MAX cohort. Am J Clin Nutr 2007; 85: 1650–1656.
Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER Clinical Trial. JAMA 2003; 289: 2083–2093.
Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, Lin PH, Champagne C, Harsha DW, Svetkey LP, Ard J, Brantley PJ, Proschan MA, Erlinger TP, Appel LJ PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med 2006; 144: 485–495.
Forman JP, Stampfer MJ, Curhan GC . Diet and lifestyle risk factors associated with incident hypertension in women. JAMA 2009; 302: 401–411.
Popkin BM, Du S, Zhai F, Zhang B . Cohort profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol 2010; 39: 1435–1440.
Hildrum B, Mykletun A, Stordal E, Bjelland I, Dahl AA, Holmen J . Association of low blood pressure with anxiety and depression: the Nord-Trondelag Health Study. J Epidemiol Community Health 2007; 61: 53–58.
Hildrum B, Romild U, Holmen J . Anxiety and depression lowers blood pressure: 22-year follow-up of the population based HUNT study, Norway. BMC Public Health 2011; 11: 601.
Zhai F, Guo X, Popkin BM, Ma L, Wang Q, Yu W, Jin S, Ge K . Evaluation of the 24-hour individual recall method in China. Food Nutr Bull 1996; 17: 154–161.
Du S, Mroz TA, Zhai F, Popkin BM . Rapid income growth adversely affects diet quality in China-particularly for the poor!. Soc Sci Med 2004; 59: 1505–1515.
Yang Y, Wang G, Pan X . China Food Composition. Beijing, China: Peking University Medical Press. 2002.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N . A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997; 336: 1117–1124.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB . Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 2008; 168: 713–720.
Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC . Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med 2000; 343: 16–22.
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Health GW, King AC, Kriska A, Leon AS, Marcus BH, Morris J, Paffenbarger RS, Patrick K, Pollock ML, Rippe JM, Sallis J, Wilmore JH . Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995; 273: 402–407.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS . Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32 (9 Suppl): S498–S504.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N, Lin PH DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) Diet. N Engl J Med 2001; 344: 3–10.
Briasoulis A, Agarwal V, Messerli FH . Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012; 14: 792–798.
The People's Republic of China National Health and Family Planning Comimision Criteria of Weight for Adults [M]. Beijing, China: Standards Press of China. 2013.
Pereira MA, Folsom AR, McGovern PG, Carpenter M, Arnett DK, Liao D, Szklo M, Hutchinson RG . Physical activity and incident hypertension in black and white adults: the Atherosclerosis Risk in Communities Study. Prev Med 1999; 28: 304–312.
Williams PT . Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity 2008; 16: 2541–2548.
Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, Colditz GA . Body weight, weight change, and risk for hypertension in women. Ann Intern Med 1998; 128: 81–88.
Daniels SR, McMahon RP, Obarzanek E, Waclawiw MA, Similo SL, Biro FM, Schreiber GB, Kimm SY, Morrison JA, Barton BA . Longitudinal correlates of change in blood pressure in adolescent girls. Hypertension 1998; 31: 97–103.
Gu D, Wildman RP, Wu X, Reynolds K, Huang J, Chen CS, He J . Incidence and predictors of hypertension over 8 years among Chinese men and women. J Hypertens 2007; 25: 517–523.
Hallal PC, Dumith SC, Reichert FF, Menezes AM, Araújo CL, Wells JC, Ekelund U, Victora CG . Cross-sectional and longitudinal associations between physical activity and blood pressure in adolescence: birth cohort study. J Phys Act Health 2011; 8: 468–474.
Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H . Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric Study. Am J Epidemiol 2004; 159: 572–580.
Yasutake K, Horita N, Murata Y, Koyama S, Enjoji M, Tsuchihashi T . Estimated urinary salt excretion by a self-monitoring device is applicable to education of salt restriction. Hypertens Res 2015; 38: 143–148.
Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM . Alcohol consumption and the risk of hypertension in women and men. Hypertension 2008; 51: 1080–1087.
Taylor B, Irving HM, Baliunas D, Roerecke M, Patra J, Mohapatra S, Rehm J . Alcohol and hypertension: gender differences in dose–response relationships determined through systematic review and meta-analysis. Addiction 2009; 104: 1981–1990.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
Acknowledgements
This research uses data from the China Health and Nutrition Survey. We thank the National Institute of Nutrition and Food Safety, the Chinese Center for Disease Control and Prevention, the Carolina Population Center, the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350 and R01-HD38700), and the Fogarty International Center of the NIH for financial support and all the persons involved in the China Health and Nutrition Survey. We also thank Dong Wang, PhD, for his help and technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bai, G., Zhang, J., Zhao, C. et al. Adherence to a healthy lifestyle and a DASH-style diet and risk of hypertension in Chinese individuals. Hypertens Res 40, 196–202 (2017). https://doi.org/10.1038/hr.2016.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.119
Keywords
This article is cited by
-
The association of ideal cardiovascular health metrics and incident hypertension among an urban population of Iran: a decade follow-up in Tehran Lipid and Glucose Study
Journal of Human Hypertension (2023)
-
The Mediterranean, DASH, and MIND diets and the incident of hypertension over a median follow-up of 7.4 years in the Tehran Lipid and Glucose Study
BMC Public Health (2022)
-
Effectiveness of a patient-centered medical home model of primary care versus standard care on blood pressure outcomes among hypertensive patients
Hypertension Research (2020)
-
Hyperuricemia predicts the risk for developing hypertension independent of alcohol drinking status in men and women: the Saku study
Hypertension Research (2020)
-
Combined use of a healthy lifestyle smartphone application and usual primary care counseling to improve arterial stiffness, blood pressure and wave reflections: a Randomized Controlled Trial (EVIDENT II Study)
Hypertension Research (2019)