Abstract
Heart failure is a serious disease induced by several conditions, including hypertrophic cardiomyopathy. Although many reports suggest that there is an association between periodontal disease and cardiovascular disease, the mechanisms have yet to be elucidated. The purpose of this study was to clarify the relationship between periodontal disease and heart disease, especially in cardiac hypertrophy. We used C57BL/6J mice and implanted two types of subcutaneous chambers. First, we subcutaneously implanted a coil-shaped chamber into the back of a mouse. Porphyromonas gingivalis (P.g.), a major periodontal pathogen, was injected into the chamber. Then, an osmotic pump was implanted to infuse isoproterenol. Four weeks after the ISO infusion, we performed echocardiography and harvested the heart and blood. We measured the serum level of anti-P.g.-IgG using ELISA. The mRNA levels of several factors were measured using PCR. We found stronger cardiomyocyte hypertrophy in the ISO(+)/P.g.(+) mice compared with the ISO(+)/P.g.(−) mice. The total square of randomly selected cardiomyocytes was 23% larger in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice. We detected a higher level of mRNA expression in Toll-like receptor 2 and NADPH oxidase 4 in the ISO(+)/P.g.(−) mice compared with the control group. We revealed that a periodontal pathogen affected ISO-induced cardiac hypertrophy via oxidative stress.
Similar content being viewed by others
Introduction
Heart failure is a serious disease induced by several conditions, including cardiomyopathy. Cardiac dysfunction is pathologically caused by tissue degeneration, for example, cell apoptosis or necrosis and interstitial fibrosis. Prior to degeneration, the heart undergoes cardiac remodeling. The β-adrenergic pathway is known to stimulate this process. It was reported that mice with chronic β-adrenergic stimulation showed myocardial remodeling.1
Cardiac hypertrophy is characterized by a chronic physiological increase in cardiac muscle mass and is often caused by some mechanical stress. Cardiac hypertrophy could lead to fatal diseases such as hypertrophic cardiomyopathy (HCM) and heart failure. Isoproterenol (ISO)-induced cardiac hypertrophy is a widespread model that mimics sustained adrenergic stimulation. This model also represents an important hallmark of the pathogenesis of maladaptive cardiac hypertrophy.2
Periodontal disease is characterized by the progressive destruction of the periodontal tissues that support the teeth.3 This disease is well known for its contribution to systemic inflammation.4, 5 Many papers have reported the association between heart disease and periodontal disease.6 It has been reported that Porphyromonas gingivalis (P.g.), a periodontal pathogen, has a role in cardiovascular disease.7, 8 We also reported that a periodontopathic pathogen deteriorated trans-aortic constriction (TAC)-induced myocardial hypertrophy.9 Although both TAC and ISO could induce cardiac hypertrophy, their pathological mechanisms are significantly different. TAC causes a pressure overload (mechanical stress), whereas ISO stimulates cardiac β1-and β2-receptors (pharmacological stress). Therefore, it is important to reveal the pathophysiological effects of periodontopathogens on myocardial hypertrophy induced by TAC and ISO. From these previous reports, we assumed that there was a relationship between periodontopathic bacterial infection and ISO-induced myocardial hypertrophy.
Therefore, the purpose of this study was to reveal the relationship between periodontopathic bacterial infection and ISO-induced myocardial hypertrophy.
Materials and methods
Animal models
We used a subcutaneous chamber model as previously described.10 Male wild-type C57BL/6J mice (7 weeks old) were used to observe the influence of P.g. on heart remodeling. The mice were housed in a temperature-controlled (22 ºC) facility with a 12-hour light/dark cycle and were given free access to food and water. Coil-shaped chambers made from 0.5 mm stainless steel wire were subcutaneously implanted into the backs of the mice. This investigation conformed to the Guide for the Care and Use of Laboratory Animals of the Tokyo Medical and Dental University.
Bacterial growth and immunization
P.g. is a gram-negative facultative anaerobic species that is often present in chronic periodontitis. In this study, we used the P.g. strain A7A1-28, which was cultivated on blood agar plates in an anaerobic chamber with 85% N2, 5% H2, 10% CO2 and subsequent incubation. Incubation was conducted at 37 °C for 2–3 days. The bacterial cells were then inoculated into a peptone yeast extract and incubated for another week. The bacterial concentration was standardized to 108 colony-forming units per ml.
Bacteria injection into the coil-shaped chamber
Test group (ISO(+)/P.g.(+) mice, n=9) mice were injected with live P.g. (0.1 ml) into the coil-shaped chamber 2 weeks after chamber implantation. P.g. was injected every 7 days for 21 days after the initial injection on day 0. The level of anti-P.g.-specific IgG in the serum was determined by an enzyme-linked immunosorbent assay (ELISA). Serum from each mouse was obtained prior to killing. Control group (ISO(+)/P.g.(−), n=7) mice and sham group (ISO(−)/P.g.(−), n=4) mice were injected with phosphate buffered saline instead of P.g. at the same time point as the P.g. injection.
ISO administration
Micro-osmotic pumps (Model 1004; Alzet, Cupertino,Palo Alto, CA, USA), which gradually released ISO (30 mg per kg body weight) dissolved in hosphate buffered saline, were implanted subcutaneously 2 weeks after the implantation of a coil-shaped chamber. The procedure was conducted under anesthesia with 3.6% chloral hydrate (10 mg per 100 mg body weight). Mice were studied for 28 days after the surgery and then killed.
Hemodynamic measurements and echocardiogram
Heart rate and blood pressure (BP) were measured using a tail-cuff system (BP-98 A, Softron Co., Tokyo, Japan) on day 28. An echocardiograph with a 14 MHz transducer (Toshiba, Tokyo, Japan) was conducted to record the function of the heart. A 2D-targeted M-mode echocardiogram was conducted over 3 consecutive cardiac cycles according to the American Society for Echocardiography leading edge method. We averaged the measurements of 3 consecutive cardiac cycles.
Histopathology
Hearts were extracted immediately after killing on day 28. Harvested hearts were sliced transversely into three sections (Apex, mid and basal level slices) for histological examination. The mid-level slice from each mouse was stained with hematoxylin-eosin (HE) and the silver impregnation method. The silver impregnation staining was used for the measurement of the myocyte cross-sectional area. To assess hypertrophy, we measured each cell area in 100 randomly selected cardiomyocytes in the left ventricle cross-section. We traced the cross-sectional area of the cardiomyocytes and calculated the extent of hypertrophy.11
RT–PCR
To assess the influence of P.g. on gene expression at its transcriptional level, reverse transcriptase-polymerase chain reaction (RT–PCR) was performed. We harvested the heart and extracted RNA from the whole tissue in the following manner. TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA, USA) was used to isolate total RNA according to the manufacturer's protocol. Complementary deoxyribonucleic acid was prepared with an RT–PCR kit (Affymetrix, Santa Clara, CA, USA). We used 18 s-rRNA as the control. One cell cycle was 20 s at 94 °C followed by 30 s at 60 °C. This cycle was repeated 40 times. The following sequences of primers were purchased from Applied Biosystems (Waltham, MA, USA): atrial natriuretic peptide (ANP) (Mm01255747_g1), myosin heavy chain (MyHC7) (Mm01319006_g1), TLR2 (Toll-like receptor 2) (Mm00442346-m1), TLR4 (Toll-like receptor 4) (Mm00445273_m1), Nox4 (NADPH oxidase 4) (Mm00479246_m1), Nox2 (Mm01287743-m1), interleukin (IL)-6 (Mm00446190_m1) and IL-1b (Mm00434228_m1).
Statistical analysis
The data are presented as the mean±SE. Three groups were compared with ANOVA followed by Tukey-Kramer test. A value of P<0.05 was considered statistically significant.
Results
Anti-P.g. antibody level in serum
To confirm the influence of P.g., we measured the level of serum anti-P.g. IgG using ELISA. In the ISO(+)/P.g.(+) mice, the anti-P.g. IgG level was statistically higher than in the ISO(+)/P.g.(−) mice (data not shown).
Physiological measurement
We measured cardiac function using the devices mentioned previously. The heart rate and BP showed a trend among the groups; however, there was no significant difference. There was no significant difference in the left ventricle fractional shortening, heart weight and heart weight per body weight ratio among the groups (Table 1 and Figure 1).
Histopathology
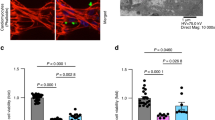
To determine the effect of P.g. on cardiac hypertrophy, heart sections were made. In the low-power field, there was no difference among the groups (Figure 2). In the high-power field, cardiomyocyte hypertrophy was observed in the ISO(+)/P.g.(−) and the ISO(+)/P.g.(+) groups (Figure 3). For assessment of the cardiomyocyte hypertrophy, the total area of 100 randomly chosen cardiomyocytes was measured using Image-Pro Express software (Media Cybernetics, Rockville, MD, USA). The cardiomyocytes were significantly larger in the ISO(+)/P.g.(+) group than in the ISO(+)/P.g.(−) group. There was also a significant difference in the size between the ISO(−)/P.g.(−) mice and the ISO(+)/P.g.(+) mice (Figure 4).
Low-power microscopic fields. Panels a, b and c show the heart sections of the representative figures, microscopic photos of low-power fields from ISO(−)/P.g.(−) mice, ISO(+)/P.g.(−) mice and ISO(+)/P.g.(+) mice, respectively. There was no apparent difference between the groups. A full color version of this figure is available at the Hypertension Research journal online.
High-power microscopic fields. Panels a, b and c show the heart sections of the representative microscopic photos of high-power fields from ISO(−)/P.g.(−), ISO(+)/P.g.(−) mice and ISO(+)/P.g.(+) mice, respectively. The bars indicate 100 μm. A full color version of this figure is available at the Hypertension Research journal online.
Cardiomyocytes hypertrophy. The graph shows the quantitative data of cardiomyocyte hypertrophy. The cardiomyocytes in the ISO(+)/P.g.(+) mice were significantly larger than those in the ISO(+)/P.g.(−) mice. There was also a significant difference in the cardiomyocyte size between the ISO(−)/P.g.(−) mice and the ISO(+)/P.g.(+) mice.
RT-PCR
To determine the mechanisms of cardiomyocyte hypertrophy observed in the present study, we measured the mRNA levels using real-time PCR. First, we measured the mRNA level of TLR2 and TLR4 to show the influence of P.g. on the innate immunity in cardiac hypertrophy. The mRNA level of TLR2 in the ISO(+)/P.g.(+) mice was significantly higher than that of the ISO(+)/P.g.(−) mice. The mRNA level of TLR4 tended to be higher in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice, although there was no significant difference (Figure 5).
Expression of TLR2 and TLR4. Panels a and b show the mRNA levels of TLR2 (a) and TLR4 (b), respectively. We found significantly higher expression of TLR2 mRNA in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice. TLR4 mRNA tended to be higher in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice. However, the difference was not significant.
To confirm the influence of P.g. on oxidative stress, we measured the mRNA level of Nox4 and Nox2. The mRNA level of Nox4 in the ISO(+)/P.g.(+) mice was significantly higher than in the ISO(+)/P.g.(−) mice on day 28. There was no significant difference in Nox2 among the groups (Figure 6).
Expression of NADPH oxygenase 2 and 4 (Nox2 and 4). Panels a and b show the mRNA levels of Nox4 (a) and Nox2 (b), respectively. Significantly higher expression of Nox4 mRNA was found in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice on day 28. There was no significant difference in the expression of Nox2-mRNA among the groups.
To assess the influence of P.g. on cardiac hypertrophy, we measured the mRNA levels of ANP and MyHC7. Both of these levels tended to be higher in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice. However, there was no significant difference between the two groups (Figure 7).
To assess the influence of P.g. on the production of pro-inflammatory cytokines in the ventricle, we measured the mRNA levels of IL-1β and IL-6. There was no significant difference between the ISO(+)/P.g.(−) and ISO(+)/P.g.(+) mice (Figure 8).
Discussion
In this study, we assessed cardiac hypertrophy in mice stimulated with a β-adrenergic stimulator and a periodontopathic pathogen. We found that the left ventricle cardiomyocytes were significantly larger in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice. We revealed that the mRNA levels of TLR2 and Nox4 were significantly higher in the ISO(+)/P.g.(+) mice than in the ISO(+)/P.g.(−) mice.
Recently, cardiovascular disease is known as a disease that might be promoted by chronic inflammation, which is regulated by several inflammatory factors such as angiotensin receptors and cytokines.12 Takeshita et al.13 demonstrated that adipose tissue inflammation is also crucial in cardiac damage in a rat model of metabolic syndrome. Accumulating evidence supports that innate immunity has a critical role in myocardial ischemia and in the development of heart failure.14 Nakashima and colleagues15 showed that TLRs are critical in vascular remodeling. Some reports suggested a role of TLRs in cardiomyocyte hypertrophy and apoptosis.16, 17 Another paper showed that bacterial infection directly or indirectly induced the development of cardiac hypertrophy via the Na+–Ca2+ exchanger.18 Systemic chronic inflammation has an important role in cardiac hypertrophy through the production of ROS. Recently, an association between Nox4 and cardiac hypertrophy has been reported.19
The role of TLR2 in cardiomyocyte hypertrophy
It was reported that P.g. enhanced the expression of TLR2 in various types of cells, including human gingival epithelial cells,20 human monocytes21 and periodontal ligament fibroblasts.22 In this study, we detected a higher expression of TLR2 in P.g.-injected mice. This result suggests that P.g. could enhance the expression of TLR2 in the heart. With respect to cardiac hypertrophy, a study using the TAC model in mice reported that cardiac hypertrophy was suppressed in TLR2-deficient mice. Two weeks after the TAC operation, TLR2-deficient mice showed reduced cardiac hypertrophy compared with wild-type mice.23 In our study, we detected cardiomyocyte hypertrophy and a higher expression of TLR2 on day 28 in the P.g.-injected mice. This result suggests that TLR2 might have a critical role in cardiomyocyte hypertrophy induced by periodontopathic pathogens.
Nox4 in the cardiac hypertrophy
It was also reported that P.g. enhanced the expression of Nox4 in some cells, for example, periodontal ligament fibroblasts.24 In this study, we found that P.g. enhanced the Nox4 expression in the heart of P.g.-injected mice. This finding suggested that infection of P.g. promoted Nox4 expression in this model. Nox4 has an important role in cardiomyocyte hypertrophy. Upregulation of Nox4 in the myocardium causes cardiac remodeling through activating the Akt-mTOR and NF-κB signaling pathways. The inhibition of Nox4 has therapeutic potential to treat cardiac remodeling.19 These points suggest that Nox4 was enhanced by P.g. infection and possibly promoted cardiomyocyte hypertrophy.
In this study, we detected the possible roles TLR2 and Nox4 have in the progression of cardiac hypertrophy. We could not elucidate the mechanisms in detail; however, we revealed that both TLR2 and Nox4 were induced by P.g. infection. This finding may elucidate the mechanisms by which periodontal disease affects systemic diseases. In our preliminary observation, pathological remodeling of the hearts was comparable between the ISO(-)/P.g.(−) group and the ISO(−)/P.g.(+) group. Therefore, we estimate that P.g. infection might accelerate ISO-induced myocardial hypertrophy, but it might not trigger the pathological changes. Our previous observation in the myocardial infarction model also demonstrated that a periodontal pathogen exacerbated ischemia-induced myocardial remodeling, although the infection itself did not trigger the pathological tissue degeneration.25 Therefore, the effect of periodontal pathogen infection on a diseased myocardium was limited.
We reported for the first time that a periodontal pathogen affected ISO-induced cardiac hypertrophy. In the near future, this finding might be useful to prevent and/or treat periodontopathic bacteria accelerated CVD, which is strongly associated with cardiac hypertrophy.
References
Song S, Si LY . Klotho ameliorated isoproterenol-induced pathological changes in cardiomyocytes via the regulation of oxidative stress. Life Sci. 2015; 135: 118–123.
Frank D, Kuhn C, Brors B, Hanselmann C, Lüdde M, Katus HA, Frey N . Gene expression pattern in biomechanically stretched cardiomyocytes: evidence for a stretch-specific gene program. Hypertension 2008; 51: 309–318.
Levine RS . Obesity, diabetes and periodontitis – a triangular relationship? Br Dent J 2013; 215: 35–39.
Moutsopoulos NM, Madianos PN . Low-grade inflammation in chronic infectious diseases: paradigm of periodontal infections. Ann N Y Acad Sci. 2006; 1088: 251–264.
Pihlstrom BL, Michalowicz BS, Johnson NW . Periodontal diseases. Lancet 2005; 366: 1809–1820.
Beck JD, Offenbacher S . Systemic effects of periodontitis: epidemiology of periodontal disease and cardiovascular disease. J Periodontol. 2005; 76: 2089–2100.
Kobayashi N, Suzuki J, Ogawa M, Aoyama N, Komuro I, Izumi Y,? Isobe M . Porphyromonas gingivalis promotes neointimal formation after arterial injury through toll-like receptor 2 signaling. Heart Vessels. 2014; 29: 542–549.
Ashigaki N, Suzuki J, Ogawa M, Watanabe R, Aoyama N, Kobayashi N, Hanatani T, Sekinishi A, Zempo H, Tada Y, Takamura C, Wakayama K, Hirata Y, Nagai R, Izumi Y, Isobe M . Periodontal bacteria aggravate experimental autoimmune myocarditis in mice. Am J Physiol Heart Circ Physiol 2013; 304: H740–H748.
Sekinishi A, Suzuki J, Aoyama N, Ogawa M, Watanabe R, Kobayashi N, Hanatani T, Ashigaki N, Hirata Y, Nagai R, Izumi Y, Isobe M . Periodontal pathogen Aggregatibacter actinomycetemcomitans deteriorates pressure overload-induced myocardial hypertrophy in mice. Int Heart J. 2012; 53: 324–330.
Reina S, Ganzinelli S, Sterin-Borda L, Borda E . Pro-apoptotic effect of anti-beta1-adrenergic receptor antibodies in periodontitis patients. Int Immunopharma 2012; 14: 710–721.
Chatterjee A, Mir SA, Dutta D, Mitra A, Pathak K, Sarkar S . Analysis of p53 and NF-κB signaling in modulating the cardiomyocyte fate during hypertrophy. J Cell Physiol. 2011; 226: 2543–2554.
Dhande I, Ma W, Hussain T . Angiotensin AT2 receptor stimulation is anti-inflammatory in lipopolysaccharide-activated THP-1 macrophages via increased interleukin-10 production. Hypertens Res. 2015; 38: 21–29.
Takeshita Y, Watanabe S, Hattori T, Nagasawa K, Matsuura N, Takahashi K, Murohara T, Nagata K . Blockade of glucocorticoid receptors with RU486 attenuates cardiac damage and adipose tissue inflammation in a rat model of metabolic syndrome. Hypertens Res. 2015; 38: 741–750.
Lin L, Knowlton AA . Innate immunity and cardiomyocytes in ischemic ?heart disease. Life Sci. 2014; 100: 1–8.
Nakashima T, Umemoto S, Yoshimura K, Matsuda S, Itoh S, Murata T, Fukai T, Matsuzaki M . TLR4 is a critical regulator of angiotensin II-induced vascular remodeling: the roles of extracellular SOD and NADPH oxidase. Hypertens Res. 2015; 38: 649–655.
Tzeng HP, Fan J, Vallejo JG, Dong JW, Chen X, Houser SR, Mann DL . Negative inotropic effects of high-mobility group box 1 protein in isolated contracting cardiac myocytes. Am J Physiol Heart Circ Physiol 2008; 294: H1490–H1496.
Su FF, Shi MQ, Guo WG, Liu XT, Wang HT, Lu ZF, Zheng QS . High-mobility group box 1 induces calcineurin-mediated cell hypertrophy in neonatal rat ventricular myocytes. Mediators Inflamm. 2012; 2012: 805149.
Magi S, Nasti AA, Gratteri S, Castaldo P, Bompadre S, Amoroso S, Lariccia V . Gram-negative endotoxin lipopolysaccharide induces cardiac hypertrophy: detrimental role of Na(+)-Ca(2+) exchanger. Eur J Pharmacol. 2015; 746: 31–40.
Zhao QD, Viswanadhapalli S, Williams P, Shi Q, Tan C, Yi X, Bhandari B, Abboud HE . NADPH oxidase 4 induces cardiac fibrosis and hypertrophy through activating Akt/mTOR and NF-κB signaling pathways. Circulation 2015; 131: 643–655.
Savitri IJ, Ouhara K, Fujita T, Kajiya M, Miyagawa T, Kittaka M, Yamakawa M, Shiba H, Kurihara H . Irsogladine maleate inhibits Porphyromonas gingivalis-mediated expression of toll-like receptor 2 and interleukin-8 in human gingival epithelial cells. J Periodontal Res 2015; 50: 486–493.
Eskan MA, Hajishengallis G, Kinane DF . Differential activation of human gingval epithelial cells and monocytes by Porphyromonas gingivalis fimbriae. Infect Immun. 2007; 75: 892–898.
Wara-aswapati N, Chayasadom A, Surarit R, Pitiphat W, Boch JA, Nagasawa T, Ishikawa I, Izumi Y . Induction of Toll-like receptor expression by Porphyromonas gingivalis. J Periodontol. 2013; 84: 1010–1018.
Higashikuni Y, Tanaka K, Kato M, Nureki O, Hirata Y, Nagai R, Komuro I, Sata M . Toll-like receptor-2 mediates adaptive cardiac hypertrophy in response to pressure overload through interleukin-1b upregulation via nuclear factor κB activation. J Am Heart Assoc 2013; 2: e000267.
Gölz L, Memmert S, Rath-Deschner B, Jäger A, Appel T, Baumgarten G, Götz W, Frede S . LPS from P. gingivalis and hypoxia increases oxidative stress in periodontal ligament fibroblasts and contributes to periodontitis. Meditors Inflamm 2014; 2014: 986264.
Hanatani T, Suzuki J, Ogawa M, Aoyama N, Kobayashi N, Hirata Y, Nagai R, Izumi Y, Isobe M . The periodontal pathogen Aggregatibacter actinomycetemcomitans deteriorates ventricular remodeling after myocardial infarction in mice. Int Heart J 2012; 53: 253–256.
Acknowledgements
This work was supported by grants from the Mitsui Life Insurance Research Foundation, the Mitsui Sumitomo Marine Welfare Research Foundation, the Geriatric Dental Research Foundation, the Human Health Future Research Foundation, St. Luke’s Hospital Research Foundation, the Health Management Foundation, the Taiyo Life Insurance Research Foundation, the 8020 Promotion Foundation, the Terumo Science Foundation, the Pfizer Health Research Foundation, the General Health Promotion Foundation, the Suzuken Memorial Foundation, the Health Science Center Foundation, the Kobayashi International Scholarship Foundation, JSPS (ID: 15K20616) and the Hakujikai Institute of Gerontology Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sato, H., Suzuki, Ji., Aoyama, N. et al. A Periodontal pathogen Porphyromonas gingivalis deteriorates Isoproterenol-Induced myocardial remodeling in mice. Hypertens Res 40, 35–40 (2017). https://doi.org/10.1038/hr.2016.114
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.114
Keywords
This article is cited by
-
Cardiovascular and Autonomic Dysfunction in Murine Ligature-Induced Periodontitis
Scientific Reports (2020)
-
Periodontitis and myocardial hypertrophy
Hypertension Research (2017)