Abstract
We recently developed novel software to measure phasic strain rate (SR) using automated one-beat real-time three-dimensional speckle tracking echocardiography (3D-STE) with high volume rates. We tested the hypothesis that left ventricular (LV) systolic function and relaxation analyzed by SR with the novel 3D-STE in hypertension (HTN) with hypertrophy may be impaired in the endocardium before there is LV systolic dysfunction. We measured LV longitudinal, radial and circumferential SR in patients with HTN (n=80, 69±7 years) and age-matched normotensive controls (n= 60, 69±10 years) using 3D-STE. HTN patients were divided into four groups according to LV geometry: normal, concentric remodeling, concentric hypertrophy and eccentric hypertrophy. We measured SR during systole as an index of systolic function, SR during isovolumic relaxation (IVR) as an index of relaxation and E/e’ as an index of filling pressure. Endocardial SR during systole in HTN with concentric and eccentric hypertrophy decreased compared with that in controls despite no reduction in ejection fraction or epicardial SR. Endocardial radial SR during IVR decreased even in normal geometry, and it was further reduced in concentric remodeling and hypertrophy despite no reduction in epicardial SR. LV phasic SR assessed by 3D-STE with high volume rates is a useful index to detect early decreases in LV systolic function and to predict subclinical LV layer dysfunction in patients with HTN.
Similar content being viewed by others
Introduction
Left ventricular (LV) pressure overload in patients with hypertension (HTN) causes hypertrophy and fibrosis, which leads to deterioration of LV function, which can lead to heart failure (HF).1 LV diastolic dysfunction in HTN directly causes left atrial remodeling associated with atrial fibrillation.2, 3 LV myocardial peak strain and strain rate (SR) during systole assessed by tissue Doppler echocardiography imaging (TDI), two-dimensional speckle tracking echocardiography (2D-STE) and three-dimensional STE (3D-STE) with low volume rates have been reported as a noninvasive and quantitative index that reflect LV contractility.4, 5, 6, 7, 8 The mitral annular tissue velocity during early diastole measured by TDI (e’) and SR during isovolumic relaxation (IVR) assessed by 2D-STE have been shown to have a good correlation with the time constant of LV pressure decline (tau).9, 10
It is well known that the subendocardium and mid-wall of the LV play important roles in ventricular function.11, 12, 13 Previous studies used sonomicrometry with crystals implanted invasively in the myocardium to evaluate subendocardial or mid-wall motion.14 Recently, MRI, TDI, 2D-STE and 3D-STE with low volume rates have been used to noninvasively evaluate myocardial layer function.5, 13, 15, 16, 17 However, MRI has the disadvantages of a low sampling rate and limited temporal resolution, and TDI has limitations of angle dependency and low reproducibility.6, 13 2D-STE is limited by out-of-plane motion5, 18, 19 and 3D-STE is so far not suitable for evaluation of phasic SR owing to low volume rates and stitched image,7, 19, 20 even though 3D-STE has high reproducibility and can measure cardiac volume and function more accurately than 2D-STE.21 We recently developed novel software to measure phasic SR by automated contouring and tracking with high volume rates of 50–80 volumes per second (v.p.s.) using one-beat real-time 3D-STE which has high sampling rate and temporal resolution and can avoid the out-of-plane motion and stitched image to obtain more accurate measurements.
There has been no study on myocardial function by global and phasic SR using 3D-STE with high volume rates. Thus, the present study had the following aims: (i) to assess the hypothesis that LV systolic function and relaxation analyzed by SR in hypertensive patients with hypertrophy may be already impaired before there is reduced LV systolic function; and (ii) to clarify the features of LV layer function according to LV geometry caused by HTN using global and phasic SR by novel 3D-STE with high volume rates.
Methods
Subjects and study protocol
The study population consisted of hypertensive patients, who were being treated with hypertensive drugs and had a systolic pressure ⩾140 mm Hg or diastolic pressure ⩾90 mm Hg prior to treatment, and 60 normotensive controls. Normotensive controls were recruited from the personnel of our hospital staff (n=15) and subjects (n=45) without cardiovascular disease who were referred to our hospital because of chest pain or discomfort and underwent electrocardiography and echocardiography. Hypertensive patients were divided into four groups according to LV geometry defined by LV mass index (LVMI) and relative wall thickness [RWT: (2 × LV posterior wall thickness at end-diastole)/LV internal diameter at end-diastole]:22 normal geometry (LVMI <95 g m−2 in females or 115 g m−2 in males and RWT ⩽0.42), concentric remodeling (LVMI is the same as above and RWT >0.42), concentric hypertrophy (LVMI⩾95 g m−2 in females or 115 g m−2 in males and RWT >0.42) and eccentric hypertrophy (LVMI is the same as above and RWT ⩽0.42). We prospectively enrolled eligible consecutive patients with HTN who underwent echocardiography until the number of patients reached 20 in each of these four groups.
Exclusion criteria in hypertensive patients were the presence of chronic atrial fibrillation, moderate to severe valvular heart disease, past history of surgery for structural heart disease, cardiomyopathy and patients with LV ejection fraction (EF) <50% and signs or symptoms of HF.
At the end of the echocardiographic examination, heart rate and blood pressure (average of three measurements by a cuff sphygmomanometer) were recorded. All participants gave written informed consent, and the research protocol was approved by the ethics committee of our institution.
Standard echo-Doppler examination
A standard echo-Doppler examination was performed using an ultrasound system (SC2000, Siemens Medical Solutions, Mountain View, CA, USA) with a 4V1c transducer (1.25–4.5 MHz) and a 3D-STE data set of the LV was obtained with the 4Z1c 3D volumetric transducer (1.5–3.5 MHz) on the SC2000 while the patient was in sinus rhythm. Echocardiographic measurements were made according to the American Society of Echocardiography criteria.22 We evaluated the following two LV systolic properties: (i) LV pumping properties that were assessed by measuring the stroke work (SW) calculated as the product of mean arterial blood pressure and stroke volume; and (ii) LV shortening parameters such as LV EF. LV EF was obtained from LV end-diastolic and end-systolic volumes according to the biplane modified Simpson’s rule.
LV mass was calculated by M-mode imaging using the Devereux and Reichek formula and indexed to body surface area. IVR time was measured as the time between the end of LV outflow and the beginning of LV inflow by Doppler echocardiography from the apical three-chamber view. The e’ of the septal mitral annulus was measured and the ratio of the transmitral peak early inflow velocity (E) to e’ (E/e’) was calculated as an estimate of LV filling pressure.
LV function assessed by automated one-beat real-time 3D-STE
A full-volume scan was acquired in a single heart beat from an apical approach using the SC2000 with a volume rate of 50–80 v.p.s. Data sets were stored digitally in raw data format and exported to a separate workstation equipped with newly developed software (VMM pre-release ver. 1/7/2013, Siemens Medical Solutions) for off-line analysis of LV volume, strain and SR. The algorism of this novel software was written by Siemens Medical Solutions, and its clinical feasibility was repeatedly tested and improved by staff of our hospital. A recent improvement in the software was applied to automatically divide the LV into all 16 segments and calculate LV strain and SR in both endocardial and epicardial layers of 16 segments. This novel software can measure both endocardial and epicardial LV phasic peak SR during the following phases: isovolumic contraction, systole, IVR, early diastole and atrial contraction (Figure 1). Among these parameters, we employed peak SR during systole as an index that reflects systolic function and IVR as an index that reflects relaxation for our analyses. LV contractility, which refers to the intrinsic property of contractile state in the entire ventricle, was assessed by peak SR of both the endocardium and epicardium (average of peak SR in 16 LV segments) during systole. LV relaxation was estimated by peak SR of both layers during IVR. Novel 3D-STE with high volume rates of 50–80 v.p.s. gave the peak SR during IVR in most patients because duration of one volume has at least 20 ms which is enough time to detect peak SR during IVR (IVR time is several times longer than 20 ms). However, in case that peak SR is not clear, we chose the inflection points or notch during IVR as a peak SR. Strain and SR are affected by stress–strain relationship. Therefore, we calculated LV systolic stress (systolic blood pressure × LV end-systolic dimension/LV systolic thickness) to correlate SR by LV systolic stress using a multivariate logistic analysis.
Full-volume acquisition and automated measurement of the left ventricle by one-beat real-time three-dimensional speckle tracking echocardiography and novel software. (a) Automatic tracing of the endocardial and epicardial borders of a four-slice display for full-volume acquisition: one apical four-chamber view and three short axis views (apical, middle and basal portions of the left ventricle). (b) Representative image of phasic left ventricular strain rate obtained using novel three-dimensional speckle tracking echocardiography and software at volume rates of 70 volumes per second. Left: left ventricular endocardial radial strain rate. Right: left ventricular epicardial radial strain rate. Blue arrow: isovolumic contraction; red arrow: systole; yellow arrow: isovolumic relaxation; orange arrow: early diastole; white arrow: atrial contraction. A full color version of this figure is available at the Hypertension Research journal online.
Volume myocardial mechanics
To take advantage of the additional information provided by volume data, a specialized volume-tracking algorithm must be utilized. Therefore, automated voxel-based speckle-tracking software (eSie Mechanics version 01 2013, Siemens Medical Solutions) was employed. This new software leverages knowledge-based technology to minimize variability of the initial contour which currently limits the clinical use of speckle tracking. An existing commercially available automatic segmentation algorithm (eSie LVA product) is used initially to contour the endocardium at the end of systole.23 An epicardial contour is then added based on the endocardial layer. The user can optimize both contours globally or regionally. A specialized voxel-based volume-tracking algorithm is then applied to the remaining volumes in the sequence.24, 25 Once completed, the user verifies the tracking based on how well it follows the endocardial and epicardial contours of the left ventricle. Valve opening and closing events are automatically defined utilizing the cycle length and estimated events. The user can verify the timing of events utilizing the volume data where the valve anatomy and function can be verified. All volume deformation quantitative data are subsequently available.
Reproducibility of LV SR by the novel 3D-STE and the novel software
We determined the interobserver variability of LV radial, longitudinal and circumferential SR of the endocardium and epicardium during systole and during IVR by comparing the raw data set obtained by two observers in randomly selected 20 subjects (age 59±9, 14 male, normotensive control: n=10, normal geometry: n=3, concentric remodeling: n=4 concentric LVH: n=3). The relation of radial, longitudinal and circumferential SR during systole and during IVR between the two observers and limits of agreement of the measurements were evaluated.
Statistical analyses
Continuous variables are expressed as the mean±s.d., and categorical variables are presented as frequency and percentage. Differences among groups for the categorical variables were assessed by the χ2 test or Fisher’s exact test, and differences among groups for the continuous variables were analyzed by analysis of variance followed by a Bonferroni test for post hoc comparisons. The relationship between measurements of SR by two observers was tested by simple linear regression analysis. Bland–Altman analysis was used to determine the limits of agreement between measurements of SR by two observers. Multivariate logistic analysis was performed to evaluate independent features of LV geometry. A P value <0.05 was considered statistically significant. All statistical analyses were performed using Stat View version 5.0 (SAS Institution, Cary, NC, USA).
Results
Reproducibility of LV SR by the novel 3D-STE and the novel software
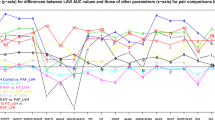
The interobserver correlation coefficient and limits of agreement of SR during systole and IVR in endocardium and epicardium were shown in Figures 2 and 3. However, it was not possible to measure circumferential SR in epicardium because epicardium was likely to move too little to detect phasic SRs in circumferential direction.
Characteristics of the study population
Patients were excluded owing to chronic atrial fibrillation (n=4), moderate to severe valvular heart disease (n=7), past history of surgery for structural heart disease (n=4), cardiomyopathy (n=5) and symptoms or signs of HF or LV EF<50% (n=7). Two patients were excluded because of poor recording due to obesity and emphysema. After exclusions, 80 hypertensive patients (69±7 years, 49 men) and 60 normotensive controls (69±10 years, 37 men) were included in the final analysis. The hypertensive patients had concomitant cardiovascular diseases such as coronary artery disease (n=17), paroxysmal atrial fibrillation (n=11) and thoracic or abdominal aortic aneurysm (n=11). The characteristics of the study population are listed in Table 1. Age, gender, body surface area and heart rate were not significantly different among the five groups, whereas systolic blood pressure was significantly higher in the hypertensive patients. Number of patients with coronary artery disease and number of patients with diabetes mellitus did not have significant difference in the four groups of HTN.
Echocardiographic parameters
LV phasic SR in three directions (longitudinal, radial and circumferential) was obtained within 3 min (150 ±12 s) using 3D-STE images obtained at high volume rate of 65±5 v.p.s. and analyzed with novel software. Data from standard and conventional echo-Doppler examinations are shown in Table 2. Hypertensive patients with concentric remodeling and hypertrophy had significantly higher LVMI and significant deterioration of diastolic parameters compared with controls. The 3D-STE assessment of LV strain and SR are summarized in Table 3.
LV longitudinal, radial and circumferential strain of the endocardium in HTN with hypertrophy was reduced compared with control. The percent reduction of longitudinal strain between the controls and HTN with normal geometry was the highest, followed by radial and circumferential strain (percent reductions: 10%, 6% and 6%, respectively). Endocardial LV peak SR in all three directions during systole and IVR was also reduced in HTN with hypertrophy, in the absence of significant reductions in LV EF and SW (Table 3). LV relaxation of the endocardium assessed by SR during IVR was impaired even in HTN with normal geometry without an elevation of E/e’.
Endocardial LV radial SRs during systole and IVR in normotensive controls were significantly greater than the corresponding epicardial SRs (by 37% and 54%, respectively). The difference in LV radial SR during systole and IVR between the endocardium and epicardium continued to diminish in association with HTN-induced changes in LV geometry. Decreasing myocardial performance from the endocardial to epicardial layer and decreasing endocardial function in association with HTN-induced changes in LV geometry are shown in Figure 4.
Left ventricular radial stain rate during isovolumic relaxation (left) and systole (right) of the endocardium and epicardium in normotensive controls and hypertensive patients. LV: left ventricle; SR: strain rate. *P<0.05 vs. control, #P<0.05 vs. normal geometry, $P<0.05 vs. concentric remodeling, +P<0.05 vs. endocardial SR. A full color version of this figure is available at the Hypertension Research journal online.
In the multivariate logistic analyses, endocardial radial SR during systole were independent features of concentric and eccentric LVH, whereas epicardial radial SRs during systole were not independent features of LV geometry (Table 4). In addition, good endocardial radial SR during systole was an independent feature of normal geometry.
Discussion
We evaluated, for the first time, LV phasic SR of the endocardium in three directions and SR of the epicardium in the radial direction using novel one-beat real-time 3D-STE with high volume rates of 65±5 v.p.s. We demonstrated that LV SR of the endocardium in three directions during systole and IVR in HTN with hypertrophy were significantly reduced compared with controls, despite no reduction in LV EF and SW. These results suggested that LV function in these hypertensive patients were already reduced because of hypertrophy before any deterioration of LV EF and SW.
In the multivariate logistic analyses, we demonstrated that LV function of the endocardial side assessed by SR during systole began to deteriorate in concentric and eccentric LVH, whereas there was no deterioration in the epicardial side. We also found that LV relaxation of endocardial side assessed by radial SR during IVR was not significantly deteriorated according to LV geometry. These results suggested that LV endocardial contractility may be impaired first by HTN-induced pressure overload.
Comparison with conventional assessment of LV contractility and relaxation
Echocardiographic estimation of LV function is routinely accomplished through visual interpretation of endocardial motion and myocardial thickening,4 and estimation of myocardial shortening and thickening reflects the radial mechanics of the LV.5 However, this approach is subjective and operator-dependent, and it is impossible to accurately evaluate LV layer function. Hare et al.26 found that there was a significant reduction in LV SR obtained by 2D-STE in patients treated with trastuzumab, a drug that is used to treat breast cancer, despite no change in LV EF. This indicates that myocardial SR is more sensitive than LV EF and seems to be suitable to detect early stages of LV dysfunction.27 Furthermore, Morris et al.28 and Ohara et al.29 reported using systolic LV strain assessed by 2D-STE that there was subtle LV systolic dysfunction in patients with HTN, even though LV EF was normal. We obtained a similar finding, as there was no difference in LV EF among the five groups, whereas not only LV strain in longitudinal and radial directions but also SR during systole in three directions assessed by novel 3D-STE even in hypertensive patients with concentric remodeling was already reduced. This discrepancy between LV EF and LV strain or SR during systole may be because LV EF is calculated as LV stroke volume divided by LV end-diastolic volume, and LV EF is affected by loading conditions and LV torsion that may be a compensatory mechanism to maintain a normal LV EF,30 whereas LV strain represented by the myocardial deformation in length or SR that reflects the intrinsic property of contractile state of myocardium may be less affected by loading conditions. Wang et al.30 reported that patients with HF with preserved LV EF had reduced longitudinal and radial strain but preserved circumferential strain which may contribute to keep LV EF within normal.
Echocardiographic assessment of LV diastolic function is routinely accomplished by Doppler echocardiography or TDI. Recently, e’ and E/e’ have been widely used to estimate LV diastolic function. However, e’ represents only regional tissue velocity and has the limitation of angle dependency. In the previous study to evaluate the effects of exercise training on systo-diastolic ventricular dysfunction in patients with HTN, strain and SR measurements demonstrated positive influence of exercise training, whereas conventional echocardiography revealed a mild degree of diastolic dysfunction without significant differences from baseline to the end of the exercise training protocol.31 This finding suggested that strain and SR may detect more subtle change in diastolic function than conventional measurements. Although regional myocardial SR in the longitudinal direction during IVR derived from 2D-STE was shown to have a strong correlation with tau and to reflect LV relaxation,10 global SR during IVR derived from previous 3D-STE has not been validated because of low volume rates. Our novel 3D-STE system with high volume rates can overcome the limitations of TDI and 2D-STE, and estimate LV function by SR during systole and IVR.
Utility of novel 3D-STE to estimate LV function
The heart is a complex mechanical organ that undergoes cyclic changes in multiple dimensions that ultimately affects a change in chamber volume.6 Thus, the complex mechanics of the heart seem to be best represented by 3D strain echocardiography. Our novel 3D-STE method with a high volume rate (65±5 v.p.s.) seems promising for several reasons: (i) all 16 segments of the LV endocardium and epicardium can be evaluated in their 3D motion and the method is able to avoid the out-of-plane phenomenon inherent to 2D imaging; (ii) non-stitched, 90 × 90 degrees full LV volume data obtained during a single beat are assessed with volumetric speckle tracking software allowing for an accurate and complete evaluation of the regional and global layer contractions and relaxations in all deformation directions; and (iii) a high volume rate allows estimation of phasic layer SR such as SR during isovolumic contraction, systole, IVR, early diastole and atrial contraction, which was not possible with previous 3D-STE system.
Peak SR during systole and IVR have been reported to be the parameters that reflect contractility and relaxation, and SR is relatively volume-independent.6, 10 Therefore, we focused on the measurement of peak SR during systole and IVR by our novel 3D-STE technique. We observed a parallel decrease of longitudinal, radial and circumferential SR during systole in HTN that depended on LV geometry. Furthermore, we found that SR during systole in all three directions in HTN with not only hypertrophy but also concentric remodeling was decreased compared with control. In contrast, LV SR during systole in patients with HTN and normal geometry was comparable with control, suggesting that LV contractility was still preserved in those patients. We also demonstrated that LV relaxation assessed by radial SR during IVR even in patients with normal geometry was already reduced compared with control. This suggested that LV relaxation may be better evaluated by SR in the radial direction and may be impaired even in the early stage of HTN.
Radial deformation imaging in endocardium may yield information about dysfunction in patients with LV hypertrophy16, 32 and radial SR was reported to be related to the contractility index even in altered loading conditions.33 We found that LV function assessed by SR in normotensive controls was better in the endocardium than epicardium. This finding is consistent with previous studies.13, 18, 34 A novel approach using phasic SR assessed by automated one-beat real-time 3D-STE with high volume rates allowing definition of deformation parameters in both endocardium and epicardium may be useful to characterize the features of early abnormalities of LV systolic function and relaxation in HTN.
Clinical implications
Some patients with concentric hypertensive hypertrophy but no symptoms or signs of chronic HF have decreased LV function.1, 35 LV relaxation is impaired at first in patients with diastolic dysfunction and even in mild HTN.36 It was reported that in patients with HTN and LVH was an important risk factor for stroke and concentric hypertrophy carried the highest risk of stroke.37 Thus, it is important to know the optimal timing to intervene with additional intensive HTN therapy to prevent not only systolic dysfunction but also the progression of diastolic dysfunction because of pressure overload hypertrophy, as there is currently no appropriate treatment for HF with preserved LV EF. Therefore, the assessment of SR by STE may allow more accurate estimation of the beginning of the decline of LV contractility and relaxation. This in turn will help shed light on when to change patient management and initiate a more intensive treatment of HTN to prevent hypertensive HF.
Study limitations
There were several limitations in this study. First, the number of patients in this study was small, so that further studies with larger patient numbers are needed to validate the present findings. Second, this study population included the patients with coronary artery disease but without myocardial infarction and the patients with diabetes mellitus. Although the number of these diseases did not have significant difference in four groups of HTN, these diseases might influence the endocardial function. Third, LV contractility is an intrinsic property of the myocardium that is difficult to measure, but SR during systole measured by TDI was reported to be related to the contractility index in experimental model.32, 38 Therefore, we assessed the SR during systole that reflects LV contractility. However, SR may depend on loading conditions for the ventricle to some extent, to regard SR as an index of contractility may be inappropriate, even though radial SR was reported to be related to the contractility index even in altered loading conditions.33 Although LV function assessed by SR using TDI and 2D-STE were validated by invasive measurement, those assessed by SR using the novel 3D-STE and software were not validated by invasive measurement. Current results and conclusions require additional validation in a larger population to verify whether the reported modifications can be offset by intervention of intensive antihypertensive therapy.
Conclusions
LV function assessed by SR was reduced in HTN with concentric and eccentric hypertrophy compared with normotensive controls despite no reduction in LV EF and SW. Furthermore, LV relaxation assessed by radial SR was reduced even in hypertensive patients with normal geometry. Endocardial function was decreased in association with HTN-induced changes in LV geometry. The assessment of LV SR by our novel 3D-STE method may be useful to detect early and subclinical LV layer dysfunction in patients with HTN.
References
Baicu CF, Zile MR, Aurigemma GP, Gaasch WH . Left ventricular systolic performance, function, and contractility in patients with diastolic heart failure. Circulation 2005; 111: 2306–2312.
Hirose T, Kawasaki M, Tanaka R, Ono K, Watanabe T, Iwama M, Noda T, Watanabe S, Takemura G, Minatoguchi S . Left atrial function assessed by speckle tracking echocardiography as a predictor of new-onset non-valvular atrial fibrillation: results from a prospective study in 580 adults. Eur Heart J Cardiovasc Imaging 2012; 13: 243–250.
Watanabe T, Kawasaki M, Tanaka R, Ono K, Nishigaki K, Takemura G, Arai M, Noda T, Watanabe S, Minatoguchi S . Association among blood pressure control in elderly patients with hypertension, left atrial structure and function and new-onset atrial fibrillation: a prospective 2-year study in 234 patients. Hypertens Res 2013; 36: 799–806.
Gorcsan J, Strum DP, Mandarino WA, Gulati VK, Pinsky MR . Quantitative assessment of alterations in regional left ventricular contractility with color-coded tissue Doppler echocardiography comparison with sonomicrometry and pressure-volume relations. Circulation 1997; 95: 2423–2433.
Hoit BD . Strain and strain rate echocardiography and coronary artery disease. Circ Cardiovasc Imaging 2011; 4: 179–190.
Abraham TP, Dimaano VL, Liang HY . Role of tissue Doppler and strain echocardiography in current clinical practice. Circulation 2007; 116: 2597–2609.
Matsumoto K, Tanaka H, Miyoshi T, Hiraishi M, Kaneko A, Fukuda Y, Tatsumi K, Kawai H, Hirata K . Dynamic left ventricular dyssynchrony assessed on 3-dimensional speckle-tracking area strain during dobutamine stress has a negative impact on cardiovascular events in patients with idiopathic dilated cardiomyopathy. Circ J 2013; 77: 1750–1759.
Cho G-Y, Marwick TH, Kim H-S, Kim M-K, Hong K-S, Oh D-J . Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol 2009; 54: 618–624.
Nagueh SF, Middleton KI, Kopelen HA, Zoghhi WA, Quinones MA . Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997; 30: 1527–1533.
Wang J, Khoury DS, Thohan V, Torre-Amione G, Nagueh SF . Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressure. Circulation 2007; 115: 1376–1383.
Zabalgoitia M, Rahman SN, Haley WE, Yarows S, Krause L, Anderson LC, Oraby MA, Amarena J . Effect of regression of left ventricular hypertrophy from systematic hypertension on systolic function assessed by midwall shortening. Am J Cardiol 2001; 88: 521–525.
Perlini S, Muiesan ML, Cuspidi C, Sampieri L, Trimarco B, Aurigemma GP, Agabiti-Rosei E, Mancia G . Midwall mechanics are improved after regression of hypertensive left ventricular hypertrophy and normalization of chamber geometry. Circulation 2001; 103: 678–683.
Hashimoto I, Li X, Hejimadi Bhat A, Jones M, Zetts AD, Sahn DJ . Myocardial strain rate is a superior method for evaluation of left ventricular subebdocardial function compared with tissure Doppler imaging. J Am Coll Cardiol 2003; 42: 1574–1583.
Lima JAC, Jeremy R, Guier W, Bouton S, Zerhouni EA, McVeigh E, Buchalter MB, Weisfeldt ML, Shapiro EP, Weiss JL . Accurate systolic wall thickening by neuclear magnetic resonance imaging with tissue tagging. Correlation with sonomicrometers in normal and ischemia myocardium. J Am Coll Cardiol 1993; 21: 1741–1751.
Altiok E, Neizel M, Tiemann S, Krass V, Kuhr K, Becker M, Zwicker C, Koos R, Lehmacher W, Kelm M, Marx N, Hoffmann R . Quantitative analysis of endocardial and epicardial left ventricular myocardial deformation - Comparison of strain-encoded cardiac magnetic resonance imaging with two-dimensional speckle-tracking echocardiography. J Am Soc Echocardiogr 2012; 25: 1179–1188.
Minoshima M, Noda A, Nishizawa T, Hara Y, Sugiura M, Iino S, Nagata K, Koike Y, Murohara T . Endocardial radial strain imaging and left ventricular relaxation abnormalities in patients with hypertrophic cardiomyopathy or hypertensive left ventricular hypertrophy. Circ J 2009; 73: 2294–2299.
Leitman M, Lysiansky M, Lysyansky P, Fredman Z, Tyomkin V, Fuchs T, Adam D, Krakover R, Vered Z . Circumferential and longitudinal strain in 3 myocardial layers in normal subjects and in patients with regional left ventricular dysfunction. J Am Soc Echocardiogr 2010; 23: 64–70.
Maffessanti F, Nesser HJ, Weinert L, Steringer-Mascherbauer R, Neil J, Gorissen W, Sugeng L, Lang RM, Mor-Avi V . Quantitative evaluation of regional left ventricular function using three-dimensional speckle tracking echocardiography in patients with and without heart disease. Am J Cardiol 2009; 104: 1775–1762.
Yodwut C, Weinert L, Klas B, Lang RM, Mor-Avi V . Effects of frame rate on three-dimensional speckle-tracking-based measurements of myocardial deformation. J Am Soc Echocardiogr 2012; 25: 978–985.
Thebault C, Donal E, Bernard A, Moreau O, Schnell F, Mabo P, Leclercq C . Real-time three-dimensional speckle tracking echocardiography: a novel technique to quantify global left ventricular mechanical dyssynchrony. Eur J Echocardiogr 2011; 12: 26–32.
Nagaya M, Kawasaki M, Tanaka R, Onishi N, Sato N, Ono K, Watanabe T, Minatoguchi S, Miwa H, Goto Y, Hirose T, Arai M, Noda T, Watanabe S, Minatoguchi S . Quantitative validation of left atrial structure and function by two-dimensional and three-dimensional speckle tracking echocardiography: A comparative study with three-dimensional computed tomography. J Cardiol 2013; 62: 188–194.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ . Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standard Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Thavendiranathan P, Liu S, Verhaert D, Calleja A, Nitinunu A, Houten TV, Michelis N, Simonetti O, Rajagopalan S, Ryan T, Vannan MA . Feasibility, accuracy, and reproducibility of real-time full-volume 3D transthoracic echocardiography to measure LV volumes and systolic function: a fully automated endocardial contouring algorithm in sinus rhythm and atrial fibrillation. J Am Coll Cardiology Img 2012; 5: 239–251.
Wang Y, Georgescu B, Houle H, Comaniciu D . Volumetric myocardial mechanics from 3D+t ultrasound data with multi-model tracking. In Camara O, Pop M, Rhode K, Sermesant M, Smith N, Young A. (eds) Statistical Atlases and Computational Models of the Heart, Lecture Notes in Computer Science. Springer: Berlin Heidelberg. 2010; 6364, pp 184–193.
Yang L, Georgescu B, Zheng Y, Meer P, Commaniciu D . 3D ultrasound tracking of the left ventricle using one-step forward prediction and data fusion of collaborative trackers. Proc IEEE Comput Soc Conf Comput Vis Pattern Recognit 23-28 June 2008. IEEE: Anchorage, AK, USA, 1–8.
Hare JL, Brown JK, Leano R, Jenkins C, Woodward N, Marwick T . Use of myocardial deformation imaging to detect preclinical myocardial dysfunction before conventional measurements in patients undergoing breast cancer treatment with trastuzumab. Am Heart J 2009; 158: 294–301.
Koshizuka R, Ishizu T, Kameda Y, Kawamura R, Seo Y, Aonuma K . Longitudinal strain impairment as a marker of the progression of heart failure with preserved ejection fraction in a rat model. J Am Soc Echocardiogr 2013; 26: 316–323.
Morris DA, Otani K, Bekfani T, Takigiku K, Izumi C, Yuda S, Sakata K, Ohte N, Tanabe K, Friedrich K, Kuhnle Y, Nakatani S, Otsuji Y, Harverkamp W, Boldt L-H, Takeuchi M . Multidirectional global left ventricular systolic function in normal subjects and patients with hypertension: multicenter evaluation. J Am Soc Echocardiol 2014; 27: 493–500.
Ohara Y, Yoshimura Y, Fukuoka Y, Yamamoto K . Impaired endocardial radial strain in hypertensive patients with electrocardiographic strain pattern on two-dimensional speckle-tracking echocardiography. J Clin Trail Cardiol 2014; 1: 1–6.
Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF . Preserved left ventricular twist and circumferential deformation, but depressed longitudinal and radial deformation in patients with diastolic heart failure. Eur Heart J 2008; 29: 1283–1289.
Leggio M, Mazza A, Cruciani G, Sgorbini L, Pugliese M, Bendini MG, Severi P, Jesi AP . Effects of exercise training on systo-diastolic ventricular dysfunction in patients with hypertension: an echocardiographic study with tissue velocity and strain imaging evaluation. Hypertens Res 2014; 37: 649–654.
Ferferieva V, Van den Bergh A, Claus P, Jasaityte R, Veulemans P, Pellens M, Gerche A, Rademakers F, Herijgers P, D’hooge J . The relative value of strain and strain rate for defining intrinsic myocardial function. Am J Physiol Heart Circ Physiol 2012; 302: 188–195.
Weidemann F, Janmal F, Sutherland GR, Claus P, Kowalski M, Hatle L, Scheerder I, Bijnens B, Radenakers FE . Myocardial function defined by strain rate and strain during alterations in inotropic states and heart rate. Am J Physiol Heart Circ Physiol 2002; 283: H792–H799.
Delfino JG, Fornwalt BK, Eisner RL, Leon AR, Oshinski JN . Determination of transmural, endocardial, and epicardial radial strain and strain rate from phase contrast MR velocity data. J Magn Reson Imaging 2008; 27: 522–528.
Aurigemma GP, Silver KH, Prrest MA, Gaasch WH . Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol 1995; 26: 195–202.
Eshoo S, Ross DL, Thomas L . Impact of mild hypertension on left atrial size and function. Circ Cardiovasc Imaging 2009; 2: 93–99.
Wang S, Xue H, Zou Y, Sun K, Fu C, Wang H, Hui R . Left ventricular hypertrophy, abnormal ventricular geometry and relative wall thickness are associated with increased risk of stroke in hypertensive patients among the Han Chinese. Hypertens Res 2014; 37: 870–874.
Greenberg NL, Firstenberg MS, Castro PL, Main M, Travaglini A, Odabashian JA, Drinko JK, Rodriguez LL, Thomas JP, Garcia MJ . Doppler-derived myocardial systolic strain rate is a strong index of left ventricular contractility. Circulation 2002; 105: 99–105.
Acknowledgements
We acknowledge the help of Mr Hidemaro Sato, Mr Ryutaro Tanaka and Ms Ritsuko Tanaka for the preparation of manuscript and the technical assistance and meaningful discussion of Ms Helene Houle.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saeki, M., Sato, N., Kawasaki, M. et al. Left ventricular layer function in hypertension assessed by myocardial strain rate using novel one-beat real-time three-dimensional speckle tracking echocardiography with high volume rates. Hypertens Res 38, 551–559 (2015). https://doi.org/10.1038/hr.2015.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.47
Keywords
This article is cited by
-
Non-invasive continuous blood pressure monitoring systems: current and proposed technology issues and challenges
Physical and Engineering Sciences in Medicine (2020)
-
The roles of mid-myocardial and epicardial cells in T-wave alternans development: a simulation study
BioMedical Engineering OnLine (2018)
-
Future Direction for Using Artificial Intelligence to Predict and Manage Hypertension
Current Hypertension Reports (2018)
-
Evaluation of systolic and diastolic properties of hypertensive heart failure using speckle-tracking echocardiography with high volume rates
Heart and Vessels (2017)
-
Impact of gender and healthy aging on pulmonary capillary wedge pressure estimated by the kinetics-tracking index using two-dimensional speckle tracking echocardiography
Hypertension Research (2016)