Abstract
The aim of this study was to examine whether the combination of abdominal obesity and high serum levels of high-sensitivity C-reactive protein (hsCRP) improves the prediction of new-onset hypertension in the general Japanese population. Participants in the Tanno–Sobetsu study, a prospective cohort study, were enrolled. Of 1516 subjects aged 30 years or older in 2002, those with hypertension or abnormal hsCRP levels were excluded, and the remaining 705 subjects were included in the present analyses. Abdominal obesity (AO) and high hsCRP levels were defined by the Japanese criteria of waist circumference and median hsCRP values, respectively. Subjects were followed up on for a maximum of 4.5 years, and the hazard ratio (HR) for new-onset hypertension was calculated using the Cox proportional hazard model. The HR for new-onset hypertension after adjustment for age, sex, fasting plasma glucose, alcohol intake, smoking, treatment for dyslipidemia and high normal blood pressure at baseline was significantly higher in the group with AO and high hsCRP (HR=1.44, 95% CI: 1.00–2.07) compared with the reference group, a group with no AO and low hsCRP; AO alone or high hsCRP alone was not associated with a significant increase in the HR. Similar trends for the increase in the HR by AO and high hsCRP were observed in separate analyses of men and women, although the differences did not reach statistical significance. Co-presence of AO and a high level of hsCRP is associated with a high risk for new-onset hypertension in the general population.
Similar content being viewed by others
Introduction
In a report by the World Health Organization, hypertension is ranked first among the important risk factors associated with mortality and fifth among the risk factors of disability-adjusted life years.1 A recent study on the risk factors for noncommunicable diseases confirmed that hypertension is a major risk factor for adult mortality, as is smoking.2 Hypertension therapy has greatly advanced in the past four decades, and the prognosis of hypertension has improved. In addition, the importance of hypertension prevention has been recognized in society and by several organizations, including the Japanese Society of Hypertension,3 which have formulated lifestyle modifications for preventing hypertension. Lifestyle modifications for hypertension prevention (that is, salt and alcohol restrictions, control of obesity, increase in physical activity, diet rich in fruits and vegetables and low fat intake) are beneficial and recommended for the general population. On the other hand, stratification of hypertension risks in normotensive subjects is important for the efficient use of social resources for education and lifestyle guidance. However, how to stratify hypertension risks in normotensive adults has not yet been established except for the fact that blood pressure at high normal blood pressure levels poses a great risk of new-onset hypertension.4
We hypothesized that the risk of hypertension in normotensives is better predicted by a combination of multiple risk factors, and we selected abdominal obesity and elevated levels of serum C-reactive protein (CRP) as indices for the combination. Obesity is an established risk factor of hypertension and cardiac diseases, and earlier studies have demonstrated a significant association of abdominal obesity (AO) with subsequent development of hypertension in various ethnic groups.5, 6, 7, 8, 9, 10 Conversely, weight reduction has been shown to reduce blood pressure in hypertensive subjects.11 Chronic low-grade inflammation has also been shown to be involved in blood pressure elevation and atherosclerosis.12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Inflammatory cytokines and upregulated production of reactive oxygen species induce endothelial dysfunction and vascular remodeling.26, 27 CRP is produced in the liver in response to interleukin-6 and interleukin-1,28 and its levels, as determined by a high-sensitivity test or high-sensitivity CRP (hsCRP), predict cardiovascular events.17, 20, 21 Although visceral obesity is associated with upregulation of inflammatory cytokines, obesity is not the only factor that promotes chronic inflammatory reactions.29 To test the present hypothesis, we used data from the Tanno–Sobetsu study, a prospective cohort study.5, 30, 31
Methods
This study was approved by the Ethical Committee of Sapporo Medical University. Written informed consent was received from all participants.
Study subjects
The Tanno and Sobetsu study is a prospective cohort study that has followed residents in two rural towns in Hokkaido, Japan, since 1977 (5,30,31). In the present study, we retrieved data for subjects who participated in annual examinations in 2002 (n= 1516) and then excluded 765 individuals with hypertension, 27 individuals with serum levels of hsCRP ⩾0.5 mg dl−1, and 19 individuals with missing data for waist circumference, hsCRP and other confounding factors. Hypertension was defined as a systolic blood pressure (SBP) ⩾140 mm Hg and/or a diastolic blood pressure (DBP) ⩾90 mm Hg or treatment with antihypertensive agents. Subjects with hsCRP ⩾0.5 mg dl−1 were excluded because of probable inflammatory diseases. Data for the remaining 705 subjects were used for the analyses.
Measurements
Study participants were examined in the morning after an overnight fast. After 5 minutes of rest, their SBP and DBP were measured twice by a well-trained doctor using a mercury sphygmomanometer with the patient in a sitting position, and the average values were used. In addition to body weight and height, waist circumference at the umbilical level was measured. Body mass index (BMI) was calculated as body weight (in kg) divided by the square of body height (in m). Information regarding past history of hypertension, diabetes, dyslipidemia, heart disease, hepatic disease, regular medication for any diseases and lifestyle habits, including smoking and alcohol intake, was collected by public health nurses on an interview form.
Venous blood was sampled to determine the levels of high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), triglycerides (TG), fasting plasma glucose (FPG) and hsCRP. The serum levels of TC, HDL-C and TG were determined by the cholesterol-oxidase-dimethoxy-aniline hydroxyl-3-sulfopropyl (DAOS) method, the dextran sulfate–magnesium hydrochloride precipitation method and the glycerol-3-phosphate-oxidase-DAOS method, respectively. The glucose oxide method and the latex aggregation and nephelometry method were used to determine plasma glucose and hsCRP levels, respectively.
Follow-up and study end point
The study end point was new onset of hypertension (SBP⩾140 mm Hg and/or DBP ⩾90 mm Hg and/or initiation of regular medication for hypertension). The study subjects were followed until the annual examination in 2007.
Statistical analysis
To assess the effect of abdominal obesity with high hsCRP levels on the development of hypertension, the participants were divided into four groups based on the cutoff levels of AO and hsCRP. The cutoff points of waist circumference for AO were ⩾85 cm for men and ⩾90 cm for women, according to the criteria for abdominal obesity by the Japan Society for the Study of Obesity.32 The cutoff values of hsCRP were the median values for men and women: 0.048 mg dl−1 and 0.034 mg dl−1, respectively. A similar analysis was conducted using the cutoff points of waist circumference for Asians (⩾90 cm for men and ⩾80 cm for women) in the international diagnostic criteria for metabolic syndrome (MS).33
Continuous variables are presented as the mean±standard deviation or median (range). The unpaired t-test, Mann–Whitney test and χ2 test were used for comparison between two groups, and Dunett’s test and Steel’s test were used for multiple comparisons among the four groups. Because hsCRP showed a skewed distribution, the Mann–Whitney test was used for comparison between men and women, and logarithmically transformed values were used to analyze the correlations. The hazard ratio (HR) for the end point was calculated for each group using the Cox proportional hazard model in which the reference group was a group without AO and with an hsCRP level below the median. As known confounding factors for high hsCRP and hypertension, age, sex, alcohol intake, smoking, FPG, medication for dyslipidemia and high normal blood pressure at baseline (SBP of 130–139 mm Hg and/or DBP of 85–89 mm Hg) were selected. IBM-SPSS ver. 17 (IBM, Tokyo, Japan) was used for the statistical analysis. The level of statistical significance was P<0.05.
Results
Table 1 shows the characteristics of the study subjects. Men were significantly older and had larger waist circumference, SBP, DBP, TG and FPG levels and smoking rates, and women had higher levels of TC and HDL-C. The hsCRP level was significantly higher in men than in women, and thus the cutoff values of hsCRP level defined as the medians were different in men and women, as described in the statistical analysis.
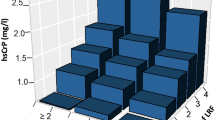
As shown in Figure 1, log-hsCRP was positively correlated with waist circumference in both men and women (men: r=0.28, P<0.001; women: r=0.42, P<0.001). When the subjects were divided into four levels of waist circumference that included both Japanese and Asian cutoff levels separately by sex, the rate of high hsCRP (that is, hsCRP above the median) was higher in the group with a larger waist circumference in both men(trend P<0.001) and women (trend P=0.001; Figure 1).
Log-hsCRP was positively correlated with waist circumference in both menand women . When subjects were divided into four levels of waist circumference, the rate of high hsCRP (that is, hsCRP above the median) was higher in a group with larger waist circumference in both menand women. In the bar plots, numbers in parentheses mean numbers of individuals with high hsCRP/numbers of all participants in each category.
Table 2 shows comparisons of abdominal obesity and hsCRP characteristics in each sex among the four groups. In men, BMI was larger, DBP and TG levels were higher and HDL-C levels were lower in groups with AO and high or low hsCRP than in the reference group (that is, the group with no AO and low hsCRP). None of the parameters was significantly different between the reference group and the group with non-AO and high hsCRP. Similarly, groups with AO in women exhibited larger BMI, higher levels of TG and lower levels of HDL-C than those in the group with non-AO and low hsCRP, but the high hsCRP groups additionally showed higher levels of SBP, DBP and TC. Moreover, the AO and high hsCRP group additionally exhibited higher levels of FPG. In contrast to the absence of differences between the reference group and the group with non-AO and high hsCRP in men, significant differences were observed between the corresponding groups in women: BMI was larger; SBP, DBP, TC and TG levels were higher; and HDL-C levels were lower in the group with non-AO and high hsCRP.
The incidence rates of HT in the four groups are shown in Table 3. The median follow-up period was three years, and the incidence of new-onset hypertension, the end point in this study, was approximately 70–85 per 1000 person-years in the groups with non-AO and low hsCRP. The incidence rate tended to be higher in the group with AO and low hsCRP, the group with non-AO and high hsCRP and the group with AO and high hsCRP in both sexes.
To quantify the impact of AO and high levels of hsCRP on the incidence of the end point, we conducted Cox’s proportional hazard model analysis. As shown in Table 4, in the analysis of all subjects with adjustments for age, sex, FPG, alcohol intake, smoking and treatment for dyslipidemia (model 1), the HR was increased by high hsCRP, but not by AO, to 1.41 (95% confidence interval (CI): 1.02–1.94), and the HR was larger in the group with both high hsCRP and AO (HR=1.67, 95% CI: 1.18–2.42). However, after additional adjustment for high normal blood pressure (model 2), the HR in the group with non-AO and high hsCRP (1.29, 95% CI: 0.93–1.79) was not significantly different from the HR in the reference group, although the increase in the HR by the presence of both AO and high hsCRP remained significant (HR=1.44, 95% CI: 1.00–2.07).
In men, the HR for the end point in model 1 was significantly higher in the group with AO and high hsCRP (HR=1.83, 95% CI: 1.07–3.13) than in the reference group, but statistical significance was lost with additional adjustment for high normal blood pressure (model 2). In women, HRs in model 1 and model 2 were not significantly different between the four groups, although the HR was largest in the group with AO and high hsCRP in model 1 and model 2.
Table 5 shows the results of the Cox’s proportional hazard analysis in groups divided based on the use of AO criteria in the international diagnostic criteria for MS. In the analysis of all subjects, inter-group differences in HRs were comparable to those in Table 4: compared with the reference group, the HR was significantly higher in the group with non-AO and high hsCRP (HR=1.51, 95% CI: 1.07–2.13) and the group with AO and high hsCRP (HR=1.72, 95% CI:1.22–2.45) in model 1, and the latter group showed only a significantly higher HR (HR= 1.55, 95% CI: 1.10–2.20) in model 2. However, the results for each gender were different from those based on the use of different AO criteria in Table 4. In men, the HR in model 1 was significantly higher in the group with non-AO and high hsCRP (HR=1.64, 95% CI: 1.02–2.65) but not in the group with AO and high hsCRP. In women, the HR was significantly higher in the group with AO and hsCRP than in the reference group in model 1 (HR= 1.73, 95% CI: 1.11–2.72) but was not significantly higher in model 2.
Discussion
In the present study, the HR for new-onset hypertension was significantly higher in the group with AO and high hsCRP at baseline than in the reference group (that is, the group with no AO and low hsCRP) after adjustment for known confounding factors for hsCRP and development of hypertension, whereas HRs in the groups with AO alone or high hsCRP alone were not significantly different from the reference HR. Similar trends for an increase in the HR based on the copresence of AO and high hsCRP were observed in separate analyses of men and women, although the presence or absence of statistical significance was dependent on AO criteria and the inclusion of high normal blood pressure as an adjustment. The findings indicate that a combination of AO and elevation of hsCRP level is a useful predictor of new-onset hypertension, although sex-specific cutoff levels of AO and hsCRP levels for prediction of hypertension remain to be further investigated. Individuals with AO and high hsCRP may be a high priority for lifestyle intervention to prevent the development of hypertension.
Earlier studies5, 34 have shown that the risk of hypertension has increased from a comparatively small waist circumference without a clear threshold level. Thus, changes in HRs by AO were considerably different depending on the criteria used for the definition of AO (that is, criteria of the Japan Society for the Study of Obesity32 vs. criteria for Asians in the international diagnostic criteria for MS33). The cutoff levels of waist circumference were lower for men and higher for women in the Japanese Society criteria than in the international criteria, and the differences are a plausible explanation for the lower HR in men and higher HR in women in the results obtained using the former criteria (Table 4) than in the results obtained using the latter criteria (Table 5). The results of this study may indicate that lower cutoff levels of waist circumference are suitable for the screening of individuals at high risk of future occurrence of hypertension, but further studies are needed to establish appropriate cutoff levels in clinical situations for primary prevention of hypertension.
Consistent with an earlier report of a relationship between the accumulation of visceral fat and chronic inflammation,35 there was a positive correlation between waist circumference and hsCRP at baseline, and the rate of a high level of hsCRP was higher in the group with a larger waist circumference. Adipose tissue remodeling is well known to be one of the underlying mechanisms of the accumulation of visceral fat and chronic inflammation. Animal experiments using a live-tissue imaging technique have shown that leukocyte and activated platelets attach to blood vessel walls in adipose tissues, modifying the functions of the vascular endothelial cells and macrophages.36 In addition, upregulation of the expression of adhesion molecules (ICAM1, P-selectin, L-selectin, PECAM), platelet activation and increased vascular permeability have been observed in adipose tissues in AO models.37, 38 Elevation of serum hsCRP appears to be an index of the complex inflammatory reactions in visceral fat.
There have been many reports on the relationship between inflammation and blood pressure elevation.13, 14, 15, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 39 Sesso et al. reported that CRP levels were associated with subsequent development of hypertension in a cohort consisting of 20 525 US female health professionals.12 In that study, even after adjustment for several confounding factors including BMI, the relative risks of quintiles divided by the baseline CRP level were 1.07, 1.17, 1.30 and 1.52 (linear trend P<0.001) compared with the lowest quintile group. In the present study, the HR for new-onset hypertension was higher in the high hsCRP groups than in the low hsCRP groups (Tables 4 and 5), confirming the findings by Sesso et al. in a different ethnic population.
Several mechanisms have been postulated for the elevation of blood pressure and atherosclerosis by chronic inflammatory reactions: CRP-mediated inhibition of nitric oxide production in endothelial cells;40, 41 endothelia damage by leukocyte adherence, platelet activation, oxidation and thrombosis;42, 43, 44 and CRP-induced upregulation of the angiotensin type-1 receptor and plasminogen activator inhibitor-1.45 Accumulation of visceral fat is not the only trigger of chronic inflammation; other environmental factors and genetic backgrounds are involved in the extent of inflammatory reactions in each individual. The present finding that the HR for hypertension was larger in the group with both AO and high hsCRP than in the group with AO alone or high hsCRP alone suggests that inflammatory reactions unrelated to AO also contribute to blood pressure elevation.
As another reason for the HR of the AO and hsCRP group being the highest among the four groups, the combination of AO and high hsCRP may improve the accuracy of prediction of a high-risk condition of obesity with adipose tissue remodeling. Abdominal obesity assessed by waist circumference may not discriminate visceral fat-type obesity at high risk for developing atherosclerosis from subcutaneous fat-type obesity at low risk for atherosclerosis. A high hsCRP level may also not discriminate disorders of adipocytokines or potential atherosclerosis from various inflammatory diseases, such as infectious disease, collagen disease, malignancy and other inflammatory diseases. The combination of AO and high hsCRP, however, may reflect visceral fat-type obesity with disorders of various adipocytokines, including hsCRP and chronic inflammation in the early stages of atherosclerosis.
One of the clinical implications of this study is that the use of the combination of AO and hsCRP for identifying and intervening in individuals at high risk for the development of hypertension may be a useful ‘high-risk’ strategy for the primary prevention of hypertension. In Japan, specific health checkups and specific counseling guidance that focus on MS have been performed since 2008. In this system, public nurses or nutritionists intervene with individuals who satisfy the criteria for MS or pre-MS (those with AO and 1 risk factor) to prevent future occurrence of lifestyle-related diseases. Thus, lifestyle interventions may be initiated for individuals with AO and high normal blood pressure level but not for obese individuals without high normal blood pressure level. The results of this study may be useful for screening of normotensive patients with AO who are at high risk for hypertension because the combination of AO and high hsCRP was related to new-onset hypertension after adjustment for high normal blood pressure level. Identification of those at high risk for new onset of hypertension among obese individuals, who have been increasing with the aging of the population, may be important because of limited social resources. However, further studies are needed to evaluate the cost-effectiveness of routinely measuring hsCRP in this system.
There were several limitations of this study. First, we excluded individuals with hsCRP⩾0.5 mg dl−1 to eliminate the effects of co-existing inflammatory diseases such as infectious diseases and connective tissue disease. However, we could not exclude low-grade inflammatory disorders because we did not conduct complete screening for these disorders. Second, we did not incorporate changes in AO and hsCRP levels during the follow-up period regarding their impact on the development of hypertension. Third, the number of study subjects was insufficient for clarifying gender differences in the predictive values of AO and high hsCRP for new-onset hypertension. Because high normal blood pressure is the strongest predictor of the development of hypertension,4 incorporating high normal blood pressure into the model would make it difficult for relatively small samples to show the contribution of other factors to hypertension. However, the trend for an increase in the HR by the co-presence of AO and high hsCRP was clear in both men and women after adjustment, including high normal blood pressure (Tables 4 and 5).
In conclusion, the presence of both AO and a high serum level of hsCRP indicates a high risk of new-onset hypertension in the general population, and individuals with these two risk factors should be advised regarding lifestyle modification for prevention of hypertension. Cutoff levels for AO and hsCRP for risk stratification of hypertension warrant further investigation.
References
Global Health Risks Mortality and burden of disease attributable to selected major risks World Health Organization 2009. Available at http://www.who.int/healthinfo/global_burden_disease/global_health_risks/en/.
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, Noda M, Mizoue T, Imano H, Saito E, Katanoda K, Sobue T, Tsugane S, Naghavi M, Ezzati M, Shibuya K . Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med 2012; 9: 1001160.
Guidelines for the management of hypertension JSH2009. The Japanese Society of Hypertension. Hypertens Res 2009; 32: 3–107.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D . Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001; 358: 1682–1686.
Ohnishi H, Saitoh S, Akasaka H, Mitsumata K, Chiba M, Furugen M, Furukawa T, Mori M, Shimamoto K . Incidence of hypertension in individuals with abdominal obesity in a rural Japanese population: the Tanno and Sobetsu study. Hypertens Res 2008; 31: 1385–1390.
Sakurai M, Miura K, Takamura T, Ota T, Ishizaki M, Morikawa Y, Kido T, Naruse Y, Nakagawa H . Gender differences in the association between anthropometric indices of obesity and blood pressure in Japanese. Hypertens Res 2006; 29: 75–80.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS . Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003; 289: 76–79.
Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, Colditz G A . Body weight, weight change, and risk for hypertension in women. Ann Intern Med 1998; 128: 81–88.
Nakamura K, Okamura T, Hayakawa T, Hozawa A, Kadowaki T, Murakami Y, Kita Y, Okayama A, Ueshima H . The proportion of individuals with obesity-induced hypertension among total hypertensives in a general Japanese population: NIPPON DATA80, 90. Eur J Epidemiol 2007; 22: 691–298.
Landsberg L, Aronne LJ, Beilin LJ, Burke V, Igel LI, Lloyd-Jones D, Sowers J . Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment - a position paper of The Obesity Society and The American Society of Hypertension. J Clin Hypertens 2013; 15: 14–33.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM . Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 2003; 42: 878–884.
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM . C-reactive protein and the risk of developing hypertension. JAMA 2003; 290: 2945–2951.
Shafi Dar M, Pandith AA, Sameer AS, Sultan M, Yousuf A, Mudassar S . hs-CRP: A potential marker for hypertension in Kashmiri population. Indian. J Clin Biochem 2010; 25: 208–212.
Davey Smith G, Lawlor DA, Harbord R, Timpson N, Rumley A, Lowe GD, Day IN, Ebrahim S . Association of C-reactive protein with blood pressure and hypertension: life course confounding and mendelian randomization tests of causality. Arterioscler Thromb Vasc Biol 2005; 25: 1051–1056.
Mattace-Raso FU, Verwoert GC, Hofman A, Witteman JC . Inflammation and incident-isolated systolic hypertension in older adults: the Rotterdam study. J Hypertens 2010; 28: 892–895.
Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW . C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 1999; 19: 972–978.
Wilson PW, Pencina M, Jacques P, Selhub J, D'Agostino R Sr ., O'Donnell CJ . C-reactive protein and reclassification of cardiovascular risk in the Framingham Heart Study. Circulation 2008; 1: 92–97.
Buckley DI, Fu R, Freeman M, Rogers K, Helfand M . C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Ann Intern Med 2009; 151: 483–495.
Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, Carr JJ, Goff DC, Greenland P, Herrington DM . Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012; 308: 788–795.
Arima H, Kubo M, Yonemoto K, Doi Y, Ninomiya T, Tanizaki Y, Hata J, Matsumura K, Iida M, Kiyohara Y . High-sensitivity C-reactive protein and coronary heart disease in a general population of Japanese: the Hisayama study. Arterioscler Thromb Vasc Biol 2008; 28: 1385–1391.
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V . Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 2000; 148: 209–214.
Hwang JJ, Li HY, Shieh GJ, Chien YF, Hua CH, Lin JW . Illustrating the roles of C-reactive protein in the development of the metabolic syndrome in women—a cross-racial validation. Nutr Metab Cardiovasc Dis 2008; 18: 671–677.
Rabkin SW, Langer A, Ur E, Calciu CD, Leiter LA . Inflammatory biomarkers CRP, MCP-1, serum amyloid alpha and interleukin-18 in patients with HTN and dyslipidemia: impact of diabetes mellitus on metabolic syndrome and the effect of statin therapy. Hypertens Res 2013; 36: 550–558.
Kong H, Qian YS, Tang XF, Zhang J, Gao PJ, Zhang Y, Zhu DL . C-reactive protein (CRP) gene polymorphisms, CRP levels and risk of incident essential hypertension: findings from an observational cohort of Han Chinese. Hypertens Res 2012; 35: 1019–1023.
Li H, Zhu X, Wang A, Wang G, Zhang Y . Co-effect of insulin resistance and biomarkers of inflammation and endothelial dysfunction on hypertension. Hypertens Res 2012; 35: 513–517.
Ross R . Atherosclerosis is an inflammatory disease. Am Heart J 1999; 138: S419–S420.
Todd ME . Hypertensive structural changes in blood vessels: do endothelial cells hold the key? Can J Physiol Pharmacol 1992; 70: 536–551.
Black S, Kushner I, Samols D . C-reactive Protein. J Biol Chem 2004; 279: 48487–48490.
Henson J, Yates T, Edwardson CL, Khunti K, Talbot D, Gray LJ, Leigh TM, Carter P, Davies MJ . Sedentary time and markers of chronic low-grade inflammation in a high risk population. PLoS med 2013; 8: 0078350.
Mitsumata K, Saitoh S, Ohnishi H, Akasaka H, Miura T . Effects of parental hypertension on longitudinal trends in blood pressure and plasma metabolic profile: mixed-effects model analysis. Hypertension 2012; 60: 1124–1130.
Yoshihara M, Akasaka H, Ohnishi H, Miki T, Furukawa T, Yuda S, Saitoh S, Miura T . Glucagon-like peptide-1 secretory function as an independent determinant of blood pressure: analysis in the Tanno-Sobetsu study. PLoS med 2013; 8: 0067578.
New criteria for 'obesity disease' for Japanese in 2011. Journal of Japan Society for the Study of Obesity; Extra edition 2011.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr . Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, VasanR S, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB Sr ., O'Donnell CJ . Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007; 116: 39–48.
Pitsavos C, Chrysohoou C, Panagiotakos DB, Lentzas Y, Stefanadis C . Abdominal obesity and inflammation predicts hypertension among prehypertensive men and women: the ATTICA Study. Heart Vessels 2008; 23: 96–103.
Hotamisligil GS . Inflammation and metabolic disorders. Nature 2006; 444: 860–867.
Nishimura S, Manabe I, Nagasaki M, Seo K, Yamashita H, Hosoya Y, Ohsugi M, Tobe K, Kadowaki T, Nagai R, Sugiura S . In vivo imaging in mice reveals local cell dynamics and inflammation in obese adipose tissue. J Clin Invest 2008; 118: 710–721.
Nishimura S, Nagasaki M . [In vivo imaging reveals chronic inflammation and abnormal local immunity in obese adipose tissue]. Seikagaku. J Jpn Biochem Soc 2010; 82: 832–836.
Niskanen L, Laaksonen DE, Nyyssonen K, Punnonen K, Valkonen VP, Fuentes R, Tuomainen TP, Salonen R, Salonen JT . Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension 2004; 44: 859–865.
Verma S, Wang CH, Li SH, Dumont AS, Fedak PW, Badiwala MV, Dhillon B, Weisel RD, Li RK, Mickle DA, Stewart DJ . A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation 2002; 106: 913–919.
Venugopal SK, Devaraj S, Yuhanna I, Shaul P, Jialal I . Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation 2002; 106: 1439–1441.
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle D A . Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation 2002; 105: 1890–1896.
Devaraj S, Xu DY, Jialal I . C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: implications for the metabolic syndrome and atherothrombosis. Circulation 2003; 107: 398–404.
Wang TJ, Wollert KC, Larson MG, Coglianese E, McCabe EL, Cheng S, Ho JE, Fradley MG, Ghorbani A, Xanthakis V, Kempf T, Benjamin EJ, Levy D, Vasan RS, Januzzi JL . Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham Heart Study. Circulation 2012; 126: 1596–1604.
Verma S, Anderson TJ . The ten most commonly asked questions about endothelial function in cardiology. Cardiol Rev 2001; 9: 250–252.
Acknowledgements
We thank the public health nurses and staff at the Tanno and Sobetsu Town Offices for their help in the recruitment of study participants and data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fujii, M., Ohnishi, H., Saitoh, S. et al. The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno–Sobetsu study. Hypertens Res 38, 426–432 (2015). https://doi.org/10.1038/hr.2015.27
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.27
Keywords
This article is cited by
-
White blood cell and platelet distribution widths are associated with hypertension: data mining approaches
Hypertension Research (2024)
-
Combined effect of obesity and low physical performance on the incidence of hypertension in Chinese community-dwelling older population
Journal of Human Hypertension (2021)
-
The association between high-sensitivity C-reactive protein and blood pressure in Yi people
BMC Public Health (2019)
-
High blood pressure and its relationship to adiposity in a school-aged population: body mass index vs waist circumference
Hypertension Research (2018)
-
Feeling the pressure: (patho) physiological mechanisms of weight gain and weight loss in humans
Hypertension Research (2017)