Abstract
HIV infected subjects present an unfavorable cardiovascular (CV) risk profile that is determined by the infection itself, highly active anti-retroviral therapy (HAART) and other factors, such as chronic kidney disease (CKD). Information is scant and contradictory on whether these factors are associated with arterial stiffness and blood pressure (BP) alteration. Our study aimed to evaluate those parameters in HIV-positive subjects both with and without HAART and with and without CKD, which was defined as the presence of microalbuminuria with a normal glomerular filtration rate. We enrolled 94 HIV-infected subjects without known CV risk factors and compared them with 37 control subjects. We recorded brachial and central BP (pulse wave analysis) and pulse wave velocity ( SphygmoCor). HIV-positive subjects of similar ages and with similar BP values showed central pulse pressure values that were significantly greater than those of controls; this was also the case for the Aix value. Central systolic and pulse pressure values and Aix were significantly greater in HIV-positive subjects with HAART and CKD than in the other HIV-positive subgroups and control subjects. PWV was also superimposable between groups when the data were analyzed relative to the presence of HAART and CKD. Our study shows that the unfavorable CV risk profile associated with HIV infection includes an increase in both central BP and Aix. The central BP increase seems to be favored by renal damage, which apparently has a role in the early stages of the disease.
Similar content being viewed by others
Introduction
Highly active anti-retroviral therapy (HAART) has strikingly reduced the incidence of death in HIV positive subjects. Concomitantly, it has markedly altered the incidence of comorbidities and the causes of death associated with HIV infection, which now result primarily from non-HIV-related diseases, many of which are of a cardiovascular (CV) nature.1, 2, 3, 4, 5, 6, 7 Because of the extended survival of patients, classic CV risk factors can now exert their harmful effects over a longer time span.8 However, some evidence suggests that HIV infection itself promotes or accelerates the progression of atherosclerosis via direct (molecular viral products) or indirect (chronic inflammation) mechanisms.9, 10, 11 Furthermore, HAART is also believed to contribute, by aggravating dyslipidemias and diabetes.12, 13, 14, 15, 16, 17, 18, 19
Although the association of HIV infection and HAART with metabolic CV risk factors has been studied extensively, limited information is available on the association of this condition with central blood pressure (BP) alterations, which are more important than peripheral BP alterations.20, 21, 22, 23, 24, 25 Furthermore, information is scant and contradictory on whether HIV infection and HAART are associated with a reduction in large artery distensibility,26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 which is an alteration of paramount importance as both a predictor of systolic hypertension and a determinant of systolic BP levels in individuals with an isolated systolic BP elevation.40, 41, 42, 43, 44, 45
Our study aimed to add information on these issues in a relatively large group of HIV-positive subjects. BP was measured not only in the brachial artery but also as central BP, and large artery stiffness was measured using the gold standard method of aortic pulse wave velocity (PWV). Data were collected from HIV-positive subjects with and without HAART and in patients with and without chronic kidney disease (CKD). The latter is of particular interest because the prevalence of CKD in HIV infections has markedly increased over the past few years.46
Methods
Study population
A total of 94 HIV-positive patients followed by the Infectious Disease Department of San Gerardo Hospital were studied, and their data were compared with those for 37 HIV-negative control subjects, who were selected from the hospital’s blood donor list. The HIV-positive patients had serologically confirmed presence of HIV infection, and the control subjects were serologically excluded. For both groups, the exclusion criteria were as follows: age less than 18 years; pregnancy; a history of CV disease (myocardial infarction, angina pectoris, heart failure, stroke, transient ischemic attacks or claudication); use of antiaggregants, anticoagulants or any other CV drugs except antihypertensive agents; diabetes mellitus (defined as a fasting plasma glucose >126 mg dl−1 on two occasions or the use of antidiabetic drugs); uncontrolled hypertension (defined as a systolic BP ⩾140 mm Hg and a diastolic BP ⩾90 mm Hg under treatment); and dyslipidemia (defined as LDL cholesterol ⩾160 mg dl−1, serum triglycerides ⩾400 mg dl−1 or the use of lipid-lowering drugs). In HIV-positive subjects, the information collected included the status of the infection, the degree of disease progression and the use of current HAART.
In all subjects, we measured height and body weight, which allowed calculation of body mass index (BMI, kg m−2), serum creatinine, glucose, triglycerides and total and fractionated cholesterol. Additionally, in the HIV-positive subjects, CD4 cell count and HIV RNA level were measured. Proteinuria was measured by dipstick on the morning urine and considered positive if ⩾1+. In the case of a positive dipstick, proteinuria was quantified over the next 24 h, and the subjects were included in the HAART CKD subgroup (see below) if a value higher than 30 mg per 24 h was confirmed. Control subjects with proteinuria were excluded.
Glomerular filtration rate was estimated (eGFR) by using the modification of diet in renal disease equation.47
CKD was defined as the presence of structural (proteinuria) and/or functional (eGFR lower than 60 ml min−1 per 1.73 m2) renal alteration.
Subjects agreed to participate in the study after being informed of its nature and purpose. The study protocol complies with the Declaration of Helsinki (as revised in 2004)48 and was approved by the ethics committee of the institutions involved.
Protocol
Subjects were asked to come to the outpatient clinic of the San Gerardo Hospital in the afternoon. After 10 min of rest in a quiet room, in which the temperature was maintained at 22 °C, brachial BP was measured three times in the right arm, using an oscillometric device (Omron Healthcare Europe, Hoofddorp, The Netherlands). With the subject remaining in the supine position, the brachial BP measurements were followed by central BP assessment via pulse wave analysis (PWA) and PWV (see below).
Pulse wave velocity
Aortic (carotid-to-femoral) PWV was obtained using an automatic applanation tonometry-based device, the SphygmoCor Vx system (AtCor Medical, Sydney, NSW, Australia). ECG-gated pulse waveforms were obtained sequentially over the common carotid and femoral arteries, and PWV was automatically provided as the ratio (meters per second) of the delay between the feet of the pressure wave at the second vs the first point to the distance between the vessels measured on the surface of the body with a rigid ruler and corrected by 0.8.49, 50 Each instance of data acquisition included at least ten consecutive cardiac beats so that the information would include a complete respiratory cycle. The mean of two acquisitions was used for the analysis.
In our laboratory, the intra-session within- and between-operator variability of PWV had a mean coefficient of variation value of 2 and 4%, respectively, and the corresponding value for the inter-session between-operator variability was 4%.
Pulse wave analysis
PWA is used to determine central BP via a Millar piezoresistive pressure transducer connected to a device (SphygmoCor)51, 52 that allows measurement of the arterial waveform from the applanation of the radial artery at the site of its maximum pulsation. The central systolic, diastolic and pulse pressures are then calculated using a validated transfer function53 that is based on a previous software calibration performed using values obtained sphygmomanometricaly at the brachial artery site. The collected data included the augmentation index (AIx), which is the supplementary increase in systolic BP as determined by the reflected pressure waves, according to the following formula:

where AP is the pressure difference between the shoulder of the wave and the peak systolic pressure and PP is the pulse pressure. Because of their dependence on heart rate, the data are automatically normalized to 75 b.p.m. (called AIx @ HR75).50, 54
In our laboratory, the intra-session within- and between-operator variability of the Aix values (coefficient of variation of the mean) was 3 and 5%, respectively, and the inter-session within-operator variability was 4%.
Statistical analysis
The data obtained for each subject were averaged, and the individual data were summed and expressed as the means (±s.d.) separately for the HIV-positive and control groups.
The subgroup analysis involved HIV patients with and without HAART and with and without CKD. Between-group differences were assessed by Student’s t-test with Bonferroni correction, Wilcoxon and χ2-tests (or Fisher exact test when needed) for normally distributed, non-normally distributed and categorical variables, respectively. One-way analysis of variance was used for multiple comparisons, and Pearson’s or Spearman’s correlation coefficients were used, as appropriate, to test the association between variables. We performed linear regression by using the additive model and adjusting for covariates as determined by stepwise regression. The covariates used for multivariate adjustments were age, sex and BMI.
Sample size was calculated for the central BP to demonstrate a significant difference of 4 mm Hg with an SD of 5 mm Hg, a type 1 error of 0.05 and a power of 0.80; thus, a minimum number of 47 cases was needed.
SPSS 13.0 (SPSS, IBM, Armonk, NY, USA) was used for the statistical analyses, and a P-value <0.05 was taken as the level of statistical significance.
Results
Population characteristics
As shown in Table 1, the mean age was similar in the control and HIV-positive groups, which showed a slight and non-significant prevalence of females. The BMI, brachial BP, blood glucose, serum creatinine and eGFR values were all within the normal range and were similar between groups. Compared with the control group, HIV-positive subjects showed a greater prevalence of smokers (current and former) as well as higher serum triglycerides and lower serum total cholesterol, LDL-cholesterol and HDL-cholesterol values. A small percentage of HIV-positive subjects were hypertensive (eight patients, all on treatment); no hypertension was observed in the control group.
Table 2 shows the demographic and clinical data for HIV-positive patients with and without HAART, and the corresponding data for HIV-positive patients without and with CKD are shown in Table 3. Compared with HIV-positive patients with HAART, the only significant difference exhibited by those without HAART was a much lower serum triglyceride value. As expected, HAART patients with CKD showed a higher serum creatinine and a lower eGFR compared with the HAART patients without CKD although in both groups the mean values were still in the normal range. HAART patients also showed a slightly higher serum triglyceride value than that in patients with HIV infection and no anti-retroviral therapy.
The patients’ immunological, virological and detailed HAART data are shown in Table 4. No difference was observed in the CD4+ cell count and HIV RNA level between the HAART-treated patients with CKD, the HAART-treated patients without CKD and the non-HAART-treated HIV-positive patients. HAART-treated patients with CKD were given nephrotoxic drugs (tenofovir, nevirapin and efavirenz) less frequently and were given protease inhibitors more frequently compared with HAART-treated patients without CKD.
Pulse wave velocity, pulse wave analysis and central blood pressure
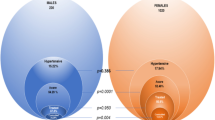
Figure 1 shows that PWV was not significantly different between control and HIV-positive patients and that no difference was observed when the data were analyzed relative to the presence of HAART with or without CKD vs the absence of any treatment (Figure 2).
Brachial BP (a), central BP (b), Aix (c) and PWV (d) of HIV+ patients (when divided by the presence of HAART and CKD) and controls. Aix, augmentation index; CKD, chronic kidney disease; DBP, diastolic blood pressure; HAART, highly active anti-retroviral therapy; PP, pulse pressure; PWV, pulse wave velocity; SBP, systolic blood pressure.
Despite similar augmentation pressure and Aix values, standardizing the latter at a heart rate of 75 b.p.m. (Aix@HR75) resulted in higher values in the HIV-positive subjects than in the controls (Figure 1). However, this difference disappeared when the subgroup analysis was performed and multiple comparison methods were used (Figure 2). In all HIV-positive subjects, the central systolic and diastolic BP values were similar to those in the control group, whereas the central pulse pressure values were significantly greater (Figure 1). Both the central systolic and pulse pressure values were significantly greater in HIV-positive subjects with HAART and CKD than in the other HIV-positive subgroups and control subjects. This was also the case when the statistical analyses were corrected using Bonferroni’s method (Figure 2).
Discussion
In our HIV-positive patients, the brachial artery systolic and diastolic BP values were similar to those exhibited by age-matched controls. This was also the case for brachial pulse pressure. By contrast, central systolic BP was greater in HIV-positive patients than in controls, and the difference was statistically significant for the central pulse pressure value (11.7% higher in HIV-positive patients than in controls). This was also the case for the Aix value, which was 43% higher in HIV-positive patients than in controls. Based on these observations, we can conclude that the unfavorable CV risk profile known to be associated with HIV infection includes an increase in BP. This increase may not be detected when BP is measured peripherally, but it appears to be significant and quantitatively non-marginal when BP is obtained at the central site.
Our study provides an additional piece of information, that is, the extent of BP alterations in treated or untreated HIV-positive patients and in HIV-positive patients with or without renal damage. The central pulse pressure values were superimposable in patients under HAART and in those without HIV treatment but were significantly greater (and extended not only to pulse but also to systolic BP) in patients under HAART who showed evidence of renal damage because of increased urinary protein excretion. These data suggest that HIV treatment does not contribute to the central BP increase observed in HIV infection. Instead, the increase seems to be favored by renal damage. The ‘renal factor’ apparently plays a role at an early stage because in our patients the increased urinary protein excretion was associated with a renal filtration level that was still within the normal limits. The role played by this renal factor in the central BP alteration is in line with the conclusions of several studies of HIV patients showing that renal damage was the precipitating factor for CV disease.55, 56, 57, 58, 59 Additionally, the reverse causality—that hypertension can determine microalbuminuria instead of the hypothesis that renal damage can determine augmented central BP—may be true. Only a small proportion of our population had hypertension; it was treated and well controlled in all cases, with all patients presenting with BP levels lower than 140/90 mm Hg. As such, no clinically relevant BP acted on the kidney and could influence its function, thus favoring our hypothesis that renal damage determines an increase in central BP. However, more studies are needed to disentangle this difficult argument.
In our patients, arterial stiffness as assessed by PWV was not significantly different between the HIV-positive patients and controls. Furthermore, arterial stiffness did not show any noticeable difference when the comparison was made between HAART and untreated patients or individuals with or without renal disease. This observation is not in line with the results of some previous studies, which have reported an increase in PWV, and thus a reduction of large artery distensibility, in HIV-infected patients.20, 21, 22, 23 It may also appear to be in opposition to the finding that, in general, there is arterial stiffening in individuals with kidney disease.60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70 However, in our patients renal damage was probably in its incipient phase (as shown by the normality of their eGFR value), which allows us to suggest that in HIV-positive patients this alteration becomes evident in a somewhat more established phase of renal involvement. This is not inconsistent with an earlier increase in central BP because central BP has been shown to have only a limited relationship to the ability of large arteries to distend in response to intravascular pressure.50 Therefore, the major determinant of its increase is probably a reflected wave phenomenon that allows forward and background waves to coalesce at the large artery level.50
Our study has some limitations. First, it was cross-sectional, which means that it does not provide evidence pertaining to the progression of the abnormalities of central BP and arterial stiffening with the duration of the HIV disease. Furthermore, we used eGFR instead of directly measured glomerular filtration rate, and we assessed both proteinuria and eGFR only once. Thus, there was no possibility of addressing the natural variability of these measures. Additionally, we did not obtain a comprehensive assessment of CV risk profile and therefore could not identify the relationship between alterations of central BP and large artery stiffness with CV risk factors. Third, the HIV patient group had a higher proportion of smokers compared with the controls; this might have influenced the final results in terms of accurately reflecting the true epidemiology of HIV subjects regarding their smoking habits. Fourth, a second control group with CKD but without HIV would surely add important information to our results. Finally, because of the limited number of our HIV-infected patients, some of the subgroups were small, limiting the power to detect some associations or changes, particularly regarding anti-retroviral drugs.
However, our study also had strengths. First, the careful CV selection and the absence of between-group differences regarding the principal confounders allowed us to draw clear conclusions, at least concerning the impact of CKD on central blood pressure. Second, the central blood pressure and PWV were measured using a state-of-the-art technique. Finally, our controls were blood donors who were free from any CV or metabolic overt disease and thus represented an excellent control population for the comparisons.
In conclusion, the determinants of the unfavorable CV risk profile associated with HIV infection are actually not fully understood, and HIV infection itself, HAART and other factors have been advocated. Our study found that in HIV-infected patients an increase in central BP can be part of this risk profile. Moreover, another factor known to have an impact on arterial vessels in the general population was identified, that is, renal damage, which seems to have an important role, even at an early stage.
References
Aberg JA . Cardiovascular complications in HIV management: past, present, and future. J Acquir Immune Defic Syndr 2009; 50: 54–64.
Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD . Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 1998; 338: 853–860.
Rasmussen LD, Engsig FN, Christensen H, Gerstoft J, Kronborg G, Pedersen C, Obel N . Risk of cerebrovascular events in persons with and without HIV: a Danish nationwide population-based cohort study. AIDS 2011; 25: 1637–1646.
Cammarosano C e, Lewis W . Cardiac lesion in acquired immune deficiency sindrome (AIDS). JACC 1985; 5: 703–706.
D:A:D Study Group, Sabin CA, Worm SW, Weber R, Reiss P, El-Sadr W, Dabis F, De Wit S, Law M, D'Arminio Monforte A, Friis-Møller N, Kirk O, Pradier C, Weller I, Phillips AN, Lundgren JD . Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet 2008; 371: 1417–1426.
Worm SW, Sabin C, Weber R, Reiss P, El-Sadr W, Dabis F, De Wit S, Law M, Monforte AD, Friis-Møller N, Kirk O, Fontas E, Weller I, Phillips A, Lundgren J . Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) Study. J Infect Dis 2010; 201: 318–330.
Strategies for Management of Anti-Retroviral Therapy/INSIGHT DAD Study Groups. Use of nucleoside reverse trasncriptase inhibitors and risk of myocardial infarction in HIV-infected patients. AIDS 2008; 22: F17–F24.
Savès M, Chêne G, Ducimetière P, Leport C, Le Moal G, Amouyel P, Arveiler D, Ruidavets JB, Reynes J, Bingham A, Raffi F, French WHO MONICA Project and the APROCO (ANRS EP11) Study Group. Risk factors for coronary heart disease in patients treated for human immunodeficiency compared with the general population. Clin Infect Dis 2003; 37: 292–298.
Oliviero U, Bonadies G, Apuzzi V, Foggia M, Bosso G, Nappa S, Valvano A, Leonardi E, Borgia G, Castello G, Napoli R, Saccà L . Human immunodeficiency virus per se exerts atherogenic effects. Atherosclerosis 2009; 204: 586–589.
Phillips AN, Carr A, Neuhaus J, Visnegarwala F, Prineas R, Burman WJ, Williams I, Drummond F, Duprez D, Belloso WH, Goebel FD, Grund B, Hatzakis A, Vera J, Lundgren JD . Interruption of ART and risk of cardiovascular disease in persons with HIV-1 infection: exploratory analyses from the SMART trial. Antivir Ther 2008; 13: 177–187.
Jiang J, Fu W, Wang X, Lin PH, Yao Q, Chen C . HIV gp120 induces endothelial dysfunction in tumour necrosis factor-a activated porcine and human endothelial cells. Cariovasc Res 2010; 87: 366–374.
Hurlimann D, Weber R, Enseleit F, Lüscher TF . HIV infection, antiretroviral therapy, and endothelium. Herz 2005; 30: 472–480.
Shafran SD, Mashinter LD, Roberts SE . The effect of low-dose ritonavir monotherapy on fasting serum lipid concentrations. HIV Med 2005; 6: 421–425.
Mulligan K, Grunfeld C, Tai VW, Algren H, Pang M, Chernoff DN, Lo JC, Schambelan M . Hyperlipidemia and insulin resistance are induced by protease inhibitors independent of changes in body composition in patients with HIV infection. J Acquir Immune Defic Syndr 2000; 23: 35–43.
Gallant JE, Staszewski S, Pozniak AL, DeJesus E, Suleiman JM, Miller MD, Coakley DF, Lu B, Toole JJ, Cheng AK, 903 Study Group. Efficacy and safety of tenofovir DF vs stavudine in combination therapy in antiretroviral-naive patients: a 3-year randomized trial. JAMA 2004; 292: 191–201.
Lee Grace A, Rao M, Mulligan K, Lo JC, Aweeka F, Schwarz JM, Schambelan M, Grunfeld C . Effects of ritonavir and amprenavir on insulin sensitivity in healthy volunteers. AIDS 2007; 21: 2183–2190.
De Wit S, Sabin CA, Weber R, Worm SW, Reiss P, Cazanave C, El-Sadr W, Monforte Ad, Fontas E, Law MG, Friis-Møller N, Phillips A, Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Incidence and risk factors for new-onset diabetes in HIV-infected patients: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Diabetes Care 2008; 31: 1224–1229.
Crane HM, Van Rompaey SE, Kitahata MM . Antiretroviral medication associated with elevated blood pressare among patients receiving highly active antiretroviral therapy. AIDS 2006; 20: 1019–1026.
Podzamczer D, Ferrer E, Sanchez P, Gatell JM, Crespo M, Fisac C, Lonca M, Sanz J, Niubo J, Veloso S, Llibre JM, Barrufet P, Ribas MA, Merino E, Ribera E, Martínez-Lacasa J, Alonso C, Aranda M, Pulido F, Berenguer J, Delegido A, Pedreira JD, Lérida A, Rubio R, del Río L, ABCDE (Abacavir vs. d4T (stavudine) plus efavirenz) Study Team. Less lipoatrophy and better lipid profile with abacavir as compared to stavudine: 96-week results of a randomized study. J Acquir Immune Defic Syndr 2007; 44: 139–147.
Safar ME, Blacher J, Pannier B, Guerin AP, Marchais SJ, Guyonvarc'h PM, London GM . Central pulse pressure and mortality in end-stage renal disease. Hypertension 2002; 39: 735–738.
Rosenwasser RF, Shah NK, Smith SM, Wen X, Gong Y, Gums JG, Nichols WW, Chapman AB, Boerwinkle E, Johnson J, Epstein B . Baseline predictors of central aortic blood pressure: A PEAR substudy. J Am Soc Hypertens 2014; 8: 152–158.
Pini R, Cavallini MC, Palmieri V, Marchionni N, Di Bari M, Devereux RB, Masotti G, Roman MJ . Central but not brachial blood pressure predicts cardiovascular events in an unselected geriatric population: the ICARe Dicomano Study. J Am Coll Cardiol 2008; 51: 2432–2439.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 2010; 31: 1865–1871.
Tomiyama H, O'rourke MF, Hashimoto H, Matsumoto C, Odaira M, Yoshida M, Shiina K, Nagata M, Yamashina A . Central blood pressure: a powerful predictor of the development of hypertension. Hypertens Res 2013; 36: 19–24.
Katsuda S, Miyashita H, Shimada K, Miyawaki Y, Kojima I, Shiogai Y, Hazama A . Subservient relationship of the peripheral second systolic pressure peak to the central hemodynamic parameters is preserved, irrespective of atherosclerosis progression in hypercholesterolemic rabbits. Hypertens Res 2014; 37: 19–25.
Papiţa AM, Albu A, Fodor D, Bondor C, Itu C, Cârstina D . Markers of preclinical vascular disease and left ventricular diastolic dysfunction in patients with HIV infection. Med Ultrason 2012; 14: 10–18.
Schillaci G, De Socio GV, Pucci G, Mannarino MR, Helou J, Pirro M, Mannarino E . Aortic stiffness in untreated adult patients with human immunodeficiency virus infection. Hypertension 2008; 52: 308–313.
Schillaci G, De Socio GV, Pirro M, Savarese G, Mannarino MR, Baldelli F, Stagni G, Mannarino E . Impact of treatment with protease inhibitors on aortic stiffness in adult patients with human immunodeficiency virus infection. Arterioscler Thromb Vasc Biol 2005; 25: 2381–2385.
Lekakis J, Ikonomidis I, Palios J, Tsiodras S, Karatzis E, Poulakou G, Rallidis L, Antoniadou A, Panagopoulos P, Papadopoulos A, Triantafyllidi H, Giamarellou H, Kremastinos DT . Association of highly active antiretroviral therapy with increased arterial stiffness in patients infected with human immunodeficiency virus. Am J Hypertens 2009; 22: 828–834.
Echeverría P, Bonjoch A, Moltó J, Jou A, Puig J, Ornelas A, Pérez-Álvarez N, Clotet B, Negredo E . Pulse wave velocity as index of arterial stiffness in HIV-infected patients compared with a healthy population. J Acquir Immune Defic Syndr 2014; 65: 50–56.
Ngatchou W, Lemogoum D, Ndobo P, Yiagnigni E, Tiogou E, Nga E, Kouanfack C, Nde F, Degaute JP, van de Borne P, Leeman M . Effects of antiretroviral therapy on arterial stiffness in Cameroonian HIV-infected patients. Blood Press Monit 2013; 18: 247–251.
Rose H, Low H, Dewar E, Bukrinsky M, Hoy J, Dart A, Sviridov D . The effect of HIV infection on atherosclerosis and lipoprotein metabolism: a one year prospective study. Atherosclerosis 2013; 229: 206–211.
Monteiro P, Miranda-Filho DB, Bandeira F, Lacerda HR, Chaves H, Albuquerque MF, Montarroyos UR, Ximenes RA . Is arterial stiffness in HIV-infected individuals associated with HIV-related factors? Braz J Med Biol Res 2012; 45: 818–826.
Charakida M, Loukogeorgakis SP, Okorie MI, Masi S, Halcox JP, Deanfield JE, Klein NJ . Increased arterial stiffness in HIV-infected children: risk factors and antiretroviral therapy. Antivir Ther 2009; 14: 1075–1079.
Van Vonderen MG, Smulders YM, Stehouwer CD, Danner SA, Gundy CM, Vos F, Reiss P, Agtmael MA . Carotid intima-media thickness and arterial stiffness in HIV-infected patients: the role of HIV, antiretroviral therapy, and lipodystrophy. J Acquir Immune Defic Syndr 2009; 50: 153–161.
Lazar JM, Wu X, Shi Q, Kagame A, Cohen M, Binagwaho A, Munyakazi L, Salciccioli L, Shi D, Anastos K . Arterial wave reflection in HIV-infected and HIV-uninfected Rwandan women. AIDS Res Hum Retroviruses 2009; 25: 877–882.
Ho JE, Deeks SG, Hecht FM, Xie Y, Schnell A, Martin JN, Ganz P, Hsue PY . Initiation of antiretroviral therapy at higher nadir CD4+ T-cell counts is associated with reduced arterial stiffness in HIV-infected individuals. AIDS 2010; 24: 1897–1905.
Maloberti A, Giannattasio C, Dozio D, Betelli M, Villa P, Nava S, Cesana F, Facchetti R, Giupponi L, Castagna F, Sabbatini F, Bandera A, Gori A, Grassi G, Mancia G . Metabolic syndrome in human immunodeficiency virus-positive subjects: prevalence, phenotype, and related alterations in arterial structure and function. Metab Syndr Relat Disord 2013; 11: 403–411.
Giannattasio C, Failla M, Squillace N, Dolara A, Cesana F, Sabbatini F, Bandera A, Facchetti R, Dozio D, Gori A, Mancia G . Ultrasonographic backscatter of the carotid artery wall in patients with HIV infection: a pilot study. Blood Press 2010; 19: 344–350.
Stella ML, Failla M, Mangoni AA, Carugo S, Giannattasio C, Mancia G . Effects of isolated systolic hypertension and essential hypertension on large and middle-sized artery compliance. Blood Press 1998; 7: 96–102.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 55: 1318–1327.
Giannattasio C, Failla M, Capra A, Scanziani E, Amigoni M, Boffi L, Whistock C, Gamba P, Paleari F, Mancia G . Increased arterial stiffness in normoglycemic normotensive offspring of type 2 diabetic parents. Hypertension 2008; 51: 182–187.
Ostlund E, Al-Nashi M, Hamad RR, Larsson A, Eriksson M, Bremme K, Kahan T . Normalized endothelial function but sustained cardiovascular risk profile 11 years following a pregnancy complicated by preeclampsia. Hypertens Res 2013; 36: 1081–1087.
Hanaoka Y, Soejima H, Yasuda O, Nakayama H, Nagata M, Matsuo K, Shinohara M, Izumi Y, Ogawa H . Level of serum antibody against a periodontal pathogen is associated with atherosclerosis and hypertension. Hypertens Res 2013; 36: 829–833.
Eggers PW, Kimmel PL . Is there an epidemic of HIV Infection in the US ESRD program? J Am Soc Nephrol 2004; 15: 2477–2485.
Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW, Van Lente F . Chronic Kidney Disease Epidemiology Collaboration. Modification of diet in renal disease - expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem 2007; 53: 766–772.
Word Medical Association Declaration of Helsinki, Ethical principles for Medical Research Involving Human Subjects. http://www.wma.net/e/policy/b3.htm.
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace-Raso FU, Protogerou AD, Schillaci G, Segers P, Vermeersch S, Weber T, Artery Society European Society of Hypertension Working Group on Vascular Structure and Function European Network for Noninvasive Investigation of Large Arteries. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens 2012; 30: 445–448.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H, European Network for Non-invasive Investigation of Large Arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
O'Rourke MF, Pauca A, Jiang XJ . Pulse wave analysis. Br J Clin Pharmacology 2001; 51: 507–522.
Salvi P, Lio G, Labat C, Ricci E, Pannier B, Benetos A . Validation of a new non-invasive portable tonometer for determining arterial pressure wave and pulse wave velocity: the PulsePen device. J Hypertens 2004; 22: 2285–2293.
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL, Kass DA . Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation 1997; 95: 1827–1836.
Wilkinson IB, Mohammad NH, Tyrrell S, Hall IR, Webb DJ, Paul VE, Levy T, Cockcroft JR . Heart rate dependency of pulse pressure amplification and arterial stiffness. J Hypertens 2002; 15: 24–30.
Szczech LA, Hoover DR, Feldman JG, Cohen MH, Gange SJ, Goozé L, Rubin NR, Young MA, Cai X, Shi Q, Gao W, Anastos K . Association between renal disease and outcomes among HIV-infected women receiving or not receiving antiretroviral therapy. Clin Infect Dis 2004; 39: 1199–1206.
George E, Lucas GM, Nadkarni GN, Fine DM, Moore R, Atta MG . Kidney function and the risk of cardiovascular events in HIV-1-infected patients. AIDS 2010; 24: 387–394.
Choi AI, Li Y, Deeks SG, Grunfeld C, Volberding PA, Shlipak MG . Association between kidney function and albuminuria with cardiovascular events in HIV-infected persons. Circulation 2010; 121: 651–658.
Serrano-Villar S, Estrada V, Gomez-Garre D, Avila M, Fuentes-Ferrer M, Sanchez-Parra C, Sainz T, Patino R, Fernandez-Cruz A . Incipient Renal Impairment as a Predictor of Subclinical Atherosclerosis in HIV-Infected Patients. JAIDS 2012; 59: 141–148.
Jotwani V, Scherzer R, Choi A, Szczech L, Polak JF, Kronmal RA, Grunfeld C, Shlipak M . Reduced kidney function and preclinical atherosclerosis in HIV-infected individuals: the study of fat redistribution and metabolic change in HIV infection (FRAM). Am J Nephrol 2011; 33: 453–460.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW, American Heart Association Councils on Kidney in Cardiovascular Disease High Blood Pressure Research Clinical Cardiology, and Epidemiology and Prevention. Kidney disease as a risk factor fors development of cardiovascular disease. Circulation 2003; 108: 2154–2169.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY . Chronic kidney disease and the risk of death, cardiovascular events and hospitalization. NEJM 2004; 351: 1296–1305.
Pannier B, Guérin AP, Marchais SJ, Safar ME, London GM . Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension 2005; 45: 592–596.
Blacher J, Safar ME, Guerin AP, Safar ME, London GM . Aortic pulse wave velocity index and mortality in end-stage renal disease. Kidney Int 2003; 63: 1852–1860.
Blacher J, Guerin A, Pannier B, Marchais SJ, Safar ME, London GM . Impact of aortic stiffness on survival in end-stage renal failure. Circulation 1999; 99: 2434–2439.
Mulè G, Cottone S, Cusimano P, Palermo A, Geraci C, Nardi E, Castiglia A, Costanzo M, Cerasola G . Unfavourable interaction of microalbuminuria and mildly reduced creatinine clearance on aortic stiffness in essential hypertension. Int J Cardiol 2010; 145: 372–375.
Safar ME, Blacher J, Pannier B, Guerin AP, Marchais SJ, Guyonvarc’h PM, London GM . Central pulse pressure and mortality in end-stage renal disease. Hypertension 2002; 39: 735–738.
Taal MW, Sigrist MK, Fakis A, Fluck RJ, McIntyre CW . Markers of arterial stiffness are risk factors for progression to end-stage renal disease among patients with chronic kidney disease stages 4 and 5. Nephron Clin Pract 2007; 107: 177–181.
Weber T, Ammer M, Gündüz D, Bruckenberger P, Eber B, Wallner M . Association of increased arterial wave reflections with decline in renal function in chronic kidney disease stages 3 and 4. Am J Hypertens 2011; 24: 762–769.
Gordin D, Wadén J, Forsblom C, Thorn LM, Rosengård-Bärlund M, Heikkilä O, Saraheimo M, Tolonen N, Hietala K, Soro-Paavonen A, Salovaara L, Mäkinen VP, Peltola T, Bernardi L, Groop PH, FinnDiane Study Group. Arterial stiffness and vascular complications in patients with type 1 diabetes: The Finnish Diabetic Nephropathy (FinnDiane) Study. Ann Med 2012; 44: 196–204.
Prince CT, Secrest AM, Mackey RH, Arena VC, Kingsley LA, Orchard TJ . Augmentation pressure and subendocardial viability ratio are associated with microalbuminuria and with poor renal function in type 1 diabetes. Vasc Dis Res 2010; 7: 216–224.
Acknowledgements
We thank the participating patients, nurses (Poli Anna, Marzia Fiorino) and research coordinators (Elena Cappelletti and Valeria Pastore).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Maloberti, A., Dozio, D., Betelli, M. et al. Brachial and central blood pressure in HIV-infected subjects. Hypertens Res 38, 405–412 (2015). https://doi.org/10.1038/hr.2015.25
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.25
Keywords
This article is cited by
-
Vascular dysfunction and body mass index in African adults with HIV
BMC Cardiovascular Disorders (2023)
-
Aortic stiffness and central hemodynamics in treatment-naïve HIV infection: a cross-sectional study
BMC Cardiovascular Disorders (2020)
-
Arterial stiffness and decline of renal function in a primary care population
Hypertension Research (2017)
-
Renal abnormalities in a cohort of HIV-infected children and adolescents
Pediatric Nephrology (2016)