Abstract
Long-term blood pressure variability (BPV) has been associated with cardiovascular events but the prognostic significance of short-term BPV remains uncertain, including its influence on the presence of target-organ damage, specifically left-ventricular hypertrophy. A meta-analysis exploring the correlation between short-term BPV and left-ventricular mass index was performed. Studies were identified by systematic searches in Pubmed and EMBASE. Any summary measure of short-term BPV obtained from ambulatory blood pressure monitoring was included. Twelve studies were included. Average real variability (ARV), s.d., weighted s.d. and coefficient of variation across 24 h/day/night periods were identified as measures of variability. Meta-analysis showed the pooled subgroup correlation coefficients of LVMI with 24 h systolic blood pressure (SBP) s.d., day SBP s.d., weighted s.d. SBP and 24 h ARV SBP were 0.22 (95% confidence interval (CI): 0.12–0.31), 0.19 (95% CI: 0.15–0.25), 0.23 (95% CI: 0.13–0.33), 0.37 (95% CI: 0.01–0.65), respectively. This meta-analysis suggests there is a weak positive correlation, between BPV and LVMI.
Similar content being viewed by others
Introduction
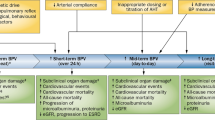
Hypertension is a well-established risk factor for cardiovascular disease.1, 2 To date guidelines on the management of hypertension have focused on reducing mean blood pressure (BP), which is clearly important, but do not mention BP variability (BPV),3 for which there is increasing evidence of prognostic value. Evidence from meta-analyses suggest that although different anti-hypertensive-drug classes have similar effects in terms of reducing BP levels, pronounced differences in their ability to reduce BPV are observed.4, 5 These differences in addition are accounted for effects on stroke risk independent of mean BP. Studies have also shown that systolic BP (SBP) variation from one visit to the next may be associated with a poor cardiovascular prognosis. In treated hypertensive patients enrolled in ASCOT-BPLA (Anglo-Scandinavian Cardiac Outcomes Trial–Blood Pressure Lowering Arm), higher visit-to-visit variability in SBP was associated with stroke and coronary events independent of mean BP.6 In a population-based observational study, higher visit-to-visit variability in SBP was associated with increased mortality risk over a 14-year follow-up.7 Importantly visit-to-visit BPV predicted all-cause mortality among those with normal BP, suggesting it may be a prognostic marker before hypertension develops.
Short-term BPV refers to fluctuations of BP across minutes or hours usually taken over a 24-h period and can be obtained through the use of ambulatory BP monitoring (ABPM).8 The predictive value of short-term BPV is less well established than that of visit-to-visit variability. Hansen et al.9 using a large population cohort (8938 subjects) explored the relationship between BPV recorded at base line with cardiovascular events over a median period of 11.3 years and determined that although short-term reading-to-reading BPV was an independent predictor, it did not contribute significantly to risk stratification over and beyond 24-h BP. Evidence from the ASCOT-BPLA trial which included both long and short-term variability suggests that although not as strong a predictor as visit-to-visit BPV, short-term BPV measured by the coefficient of variation still predicted risk of vascular events independently of average daytime mean SBP.6
The occurrence of major cardiovascular events is usually the result of long-term exposure to hypertension and other risk factors and is often preceded by the development of asymptomatic functional and structural abnormalities known as target-organ damage (TOD).10 Little is known about the influence of short-term BPV on the presence of TOD, specifically left-ventricular hypertrophy (LVH). LVH can be determined by ECG or quantified more accurately by measuring left-ventricular mass by echocardiography and indexing this to body surface area to give the left-ventricular mass index (LVMI).11 In their seminal paper, Parati et al.12 demonstrated that higher diurnal BPV measured as 24 h s.d. was associated with an increased risk of LVH (determined by ECG) in 108 mild-to-severe essentially hypertensive patients. They also showed that for nearly any level of 24 h mean BP, subjects in whom the 24 h BPV was low had a lower prevalence and severity of TOD those in whom BPV was high, indicating an independent association. However as highlighted evidence since suggests the predictive value of short-term BPV remains unclear and may not contribute much more than mean levels alone.9 To advance our knowledge of short-term variability, this review attempts to assess and quantify the correlation between BPV and LVMI. A meta-analysis on the various correlation coefficients will be performed.
Methods
Types of studies
Cohort, cross-sectional or case–control studies that explored the relationship between 24-h BPV and LVMI.
Study populations
Participants recruited to observational studies that underwent 24-h non-invasive ABPM and an assessment of LVMI. Studies of pregnant women and children were excluded.
Predictor variables
Any summary measure of short-term BPV, where short-term refers to variations across minutes or hours taken over a 24-h period obtained by non-invasive ABPM.
Outcomes
LVMI determined with echocardiography.
Search methods for identification of studies
Studies were identified by systematic searches in Pubmed and EMBASE (up to June 2015). The following search terms were used as keywords and/or MESH terms: (('ambulatory blood pressure' or 'blood pressure' or 'ambulatory blood pressure monitoring') or (short-term blood pressure) or (24 h blood pressure)) and (variability) and ('left ventricular hypertrophy' or 'left ventricular mass index') or ('end' or 'target' organ ('damage' or 'disease')). The full search strategy can be seen in the Supplementary Information, Appendix which includes different spellings and combinations of words.
Potentially relevant articles were identified and duplicates were removed. Only original research articles were included. We supplemented our electronic search by crosschecking the reference lists of all identified studies. There were no date or language restrictions. Non-English papers were translated with an online translation programme. The full texts of relevant articles were obtained and an independent reviewer reviewed selected papers against the inclusion criteria and assessed their quality using the guidelines recommended by Hayden et al.13 for quality appraisal in systematic reviews of prognostic studies. Our systematic review and meta-analysis was conducted according to the checklist of Meta-analysis of Observational Studies in Epidemiology (MOOSE), and the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA), see Supplementary Information, Appendix.
Data extraction
The study characteristics extracted included sampling approach, study design, sample size, mean age, BPV index and value, mean LVMI, correlation coefficients and relative information, such as P-values and if it was indicated that they were statistically significant or not. The data was extracted independently by two researchers (JMM and AMOF).
Statistical analysis
For the meta-analysis, correlation coefficients were converted into Fisher’s z-scores and s.e.m., which in turn were used to calculate 95% confidence intervals. The overall effect size was the weighted inverse variance of the adjusted individual effect sizes (z-scores). The overall effect sizes from the meta-analyses were then back transformed which corresponded to the overall correlation coefficients. Data from the various studies were pooled using the random-effects model. Heterogeneity between studies was assessed using the I2 statistic. The Begg’s test and Egger’s test were used to assess the extent of publication bias. All analysis was performed using Stata software.14
Results
Basic characteristics of studies
After removal of 218 duplicates, a total of 440 articles were identified during the search, of which 416 were excluded based on their titles and abstracts alone; Figure 1. After reviewing the remaining 24 full-text articles, 12 were eligible for inclusion in the review; Table 1. Reasons for exclusion included articles did not calculate LVMI as an outcome, summary measures of variability were not calculated and no effect size was reported. Out of the 12 studies, 11 were cross-sectional and one had a case–control design. The population sample sizes ranged from 33 to 1822. The various indexes used in the studies along with their definitions are presented in Table 2. The s.d. of either 24 h/day/night BP readings were used as indexes of BPV in all studies with the exception of two: one which only reported coefficient of variation (CV);15 and another study16 only reported average real variability (ARV). In addition to s.d., two studies also included CV17, 18 and a further two included weighted s.d. (wSD).19, 20 Leoncini et al. 20 also explored ARV. The average value of 24 SBP s.d., day s.d., night s.d. had range 13.0–19.7, 10.9–19 and 11.5–13.6 mm Hg, respectively. As there were so few studies exploring the other indices, we have not reported their range here but can be found in Table 3. The correlation between 24 SBP s.d., day s.d., night s.d. and LVMI had range 0.05–0.52, 0.13–0.21 and 0.04–0.21, respectively. These correlations were all statistically significant with the exception of day s.d. (r=0.19),21 24 h SBP s.d. (r=0.05) and night s.d. (r=0.04).19 In the three studies in which it was explored, wSD had a significant correlation of r= 0.15, 0.26 and 0.31.19, 20, 22 Similarly in the two studies which examined 24-h SBP ARV, a significant correlation of 0.53 and 0.19 with LVMI was observed.16, 20
Of the studies that adjusted for covariates (including mean BP), findings were mixed. Schillaci et al.23 who considered 1822 untreated subjects with essential hypertension, reported a weak univarite correlation between daytime-and night-time s.d. and LVMI but the association did not persist after adjustment for various confounders. Similar findings were found by Roman et al.18 who found daytime- and night-time s.d. were univariately associated with LVMI but the association did not persist after adjustment for confounders including average BP. Pascual et al.24 also found similar results after adjustment for age, sex and mean BP.
In contrast, Tatasciore et al.22 in a study examining 180 untreated hypertensive patients, found daytime s.d. and wSD to be significantly associated with LVMI even after adjustment for other covariates, including mean BP. Similarly Bilo et al.19 found wSD was significantly related to LVMI in a study which investigated 339 hypertensive patients. Zhang et al.16 also found 24 h ARV to be significantly related to LVMI after adjustment.
Using the guidelines recommended by Hayden et al.,13 the quality appraisal of each paper was assessed and is presented in Table 4.
Meta-analysis
Figure 2 presents converted correlation coefficients (z-scores) with subgroup meta-analysis reported for each BPV index. An overall z-score for all studies was omitted as combining different indexes would not be appropriate. After conversion from z-scores the pooled subgroup correlation coefficients of LVMI with 24 h SBP s.d., day SBP s.d., wSD SBP and 24 h ARV SBP were 0.22 (95% CI: 0.12–0.31), 0.19 (95% CI: 0.15–0.25), 0.23 (95% CI: 0.13–0.33) and 0.37 (95% CI: 0.01–0.65), respectively. All but one index (wSD) showed heterogeneity (P<0.05) across the studies and as a result random-effects models were used to combine coefficients. Begg’s and Egger’s tests indicated no evidence of publication bias within each variability index.
Discussion
Overall our review suggests that there is a weak positive correlation, between BPV and LVMI. We carried out a separate analysis for each measure of variability, resulting in reduced power in the meta-analysis. Our review highlights the lack of good epidemiological studies exploring the relationship between BPV and LVMI. As 11 out of the 12 studies were cross-sectional, we cannot assess cause–effect relationships. Although all studies reported univariate coefficients, we found just over half of the studies did any further analysis or appropriate adjustment for covariates. Despite these limitations, the results are still worth exploring and the review raised some important issues in relation to BPV in general and also specifically to LVMI.
Veerman et al.21 reported a non-significant correlation with day s.d. We cited the small sample size (n=33) as a potential reason for the discrepancy between day s.d. compared with the other studies. Bilo et al.19 also reported a non-significant correlation of LVMI with 24 h s.d., but interestingly in the same study found both day s.d. and wSD were significantly correlated with LVMI even after adjustment. This finding highlights that results are sensitive to the index chosen and leads to the issue of variability measurement.
Most studies have used s.d. as a measure of BPV and the appropriateness of such an index has been disputed because it only reflects the dispersion of measurements around a single value (mean) not accounting for the order, in which BP measurements were obtained.25, 26 The discrepancies between day and 24 h s.d. in the study by Bilo et al.19 may be explained by the fall of BP at night (dip). A large dip which is known to be associated with healthier individuals will lead to a larger 24 h s.d. The wSD attempts to remove the effect of the dip and was found to be significantly correlated unlike the 24 h s.d. This suggests that perhaps s.d., at least over 24 h may not be a good measure of BPV. Mena et al.25 first explored, and later Pierdomenico et al.,26 ARV in relation to BP which is the average absolute difference between successive readings, and is thought to give a true reflection of real variability. In both studies high ARV was found to be an independent predictor of cardiovascular risk in hypertension patients while high s.d. was not. The two studies that included ARV in this review both found a significant correlation with LVMI.16, 20 In one study association remained significant after adjustment,16 while the other study found it to be an independent predictor of multiple TOD where the majority of these had LVH.20 As ARV is thought to give a true reflection of real variability it may be the most appropriate marker of short-term BPV over other indexes and could potentially be used to predict outcome in patients even before BP becomes elevated and ultimately provide a means of identifying at risk patients before they develop hypertension.
Other studies exploring the relationship between BPV and TOD have found varied results. As mentioned, Parati et al.12 found an association between 24 h BPV and severity of TOD (a score based on presence of LVH, chest X-ray abnormalities, abnormalities of the fundus plus a clinical event and/or a renal abnormality). The same group conducted another follow-up study with a follow-up period of 7 years to assess the prognostic relevance of short-term BPV on 73 hypertensive patients.27 They found an independent association between 24 h BPV at baseline and TOD at follow-up. Similarly, in another study of over 700 hypertensive and normotensive patients, daytime systolic s.d. was found to be associated with degree of TOD. However in the same study, after adjustment for mean BP no strong association was found between BPV and LVH.28 Hansen et al.9 explored the relationship between BPV and cardiovascular events. ARV predicted all fatal and nonfatal outcomes even after adjustment for mean BP but found that it added only 0.1% to the explained risk of an event occuring. They concluded that the main risk factor remained mean BP.
As the studies are cross-sectional in nature we are not able to determine whether higher BPV initiates increases in LVMI or do increases in LVMI represent a risk factor for increased BPV rather than being a consequence of it. It is however argued that vascular hypertrophy induced by exaggerated and large BPV may lead to an impaired arterial distensibility of the large arteries, resulting in increased cardiac afterload and as a result increases LVMI.29 Clinical trials have recently shown that some classes of anti-hypertensive drugs significantly outperform others in terms of lowing BPV, and that this reduction in short-term and long-term BPV contributes to the prevention of cardiovascular events in hypertensive patients.6, 30 Results indicate that calcium channel blockers and to a lesser extent thiazide diuretics are superior to other drugs in reducing BPV and preventing stroke and other vascular events compared with the older β-blocker atenolol which increases BPV.4, 31 Similar findings were reported in a more recent observational study assessing the efficacy of mono and combination therapy on short-term BPV of 2780 hypertensive patients.32 Again calcium channel blockers, followed by diuretics were correlated with lower short-term BPV compared with angiotensin-2-receptor blockers, angiotensin converting enzyme inhibitors and β blockers. In addition, combination of calcium channel blockers’s and diuretics resulted in the lowest BPV compared with others. In those with marked BPV, the prescribing of these drugs may offer a better alternative and could help reduce the risk of LVH especially in individuals where hypertension has not yet developed.
The major limitation of this review is that we have pooled together studies in a meta-analysis in regard to their correlation coefficients which are a very weak marker of association. As a result of using correlation coefficients there is an implicit assumption that the association between BPV and LVMI is linear which in reality may not be the case. The strength of this review is its focus on short-term BPV, which has recently been receiving growing attention. It is also the first review to our knowledge that quantifies the correlation between BPV and LVMI. The review identifies a research gap where stronger epidemiological studies are needed to explore the relationship further and understand the prognostic value, if any, of short-term BPV.
References
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–2260.
Warlow C, Sudlow C, Dennis M, Wardlaw J, Sandercock P, Stroke. . Lancet 2003; 362: 1211–1224.
National Clinical Guideline C National Institute for Health and Clinical Excellence: Guidance Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34. Royal College of Physicians (UK) National Clinical Guideline Centre: London. 2011.
Webb AJ, Fischer U, Mehta Z, Rothwell PM . Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010; 375: 906–915.
Webb AJ, Fischer U, Rothwell PM . Effects of beta-blocker selectivity on blood pressure variability and stroke: a systematic review. Neurology 2011; 77: 731–737.
Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlof B, Sever PS, Poulter NR . Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010; 375: 895–905.
Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S . The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: findings from NHANES III, 1988 to 1994. Hypertension 2011; 57: 160–166.
Parati G, Schumacher H . Blood pressure variability over 24 h: prognostic implications and treatment perspectives. An assessment using the smoothness index with telmisartan-amlodipine monotherapy and combination. Hypertens Res 2014; 37: 187–193.
Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O'Brien E, Staessen JA . Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 2010; 55: 1049–1057.
Devereux RB, Alderman MH . Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation 1993; 88: 1444–1455.
Sibiya MJ, Norton GR, Hodson B, Redelinghuys M, Maseko MJ, Majane OH, Libhaber E, Woodiwiss AJ . Gender-specific contribution of aortic augmentation index to variations in left ventricular mass index in a community sample of African ancestry. Hypertens Res 2014; 37: 1021–1027.
Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G . Relationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertension. J Hypertens 1987; 5: 93–98.
Hayden JA, Cote P, Bombardier C . Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med 2006; 144: 427–437.
StataCorp. Stata Statistical Software: Release 12. StataCorp LP: College Station, TX. 2011.
Ajayi OE, Ajayi EA, Akintomide OA, Adebayo RA, Ogunyemi SA, Oyedeji AT, Balogun MO . Ambulatory blood pressure profile and left ventricular geometry in Nigerian hypertensives. J Cardiovasc Dis Res 2011; 2: 164–171.
Zhang QQ, Zhang XJ, Chang BB, Qiu BY, Zhang Y, Li J, Zeng Z . Blood pressure variability correlates with target-organ damage in elderly patients with hypertension. Sichuan Da Xue Xue Bao Yi Xue Ban 2011; 42: 252–255.
Kristensen KS, Hoegholm A, Bang LE, Gustavsen PH, Poulsen CB . No impact of blood pressure variability on microalbuminuria and left ventricular geometry: Analysis of daytime variation, diurnal variation and 'white coat' effect. Blood Press Monit 2001; 6: 125–131.
Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB . Relation of blood pressure variability to carotid atherosclerosis and carotid artery and left ventricular hypertrophy. Arterioscler Thromb Vasc Biol 2001; 21: 1507–1511.
Bilo G, Giglio A, Styczkiewicz K, Caldara G, Maronati A, Kawecka-Jaszcz K, Mancia G, Parati G . A new method for assessing 24-h blood pressure variability after excluding the contribution of nocturnal blood pressure fall. J Hypertens 2007; 25: 2058–2066.
Leoncini G, Viazzi F, Storace G, Deferrari G, Pontremoli R . Blood pressure variability and multiple organ damage in primary hypertension. J Hum Hypertens 2013; 27: 663–670.
Veerman DP, de Blok K, van Montfrans A . Relationship of steady state and ambulatory blood pressure variability to left ventricular mass and urinary albumin excretion in essential hypertension. Am J Hypertens 1996; 9: 455–460.
Tatasciore A, Renda G, Zimarino M, Soccio M, Bilo G, Parati G, Schillaci G, De Caterina R . Awake systolic blood pressure variability correlates with target-organ damage in hypertensive subjects. Hypertension 2007; 50: 325–332.
Schillaci G, Verdecchia P, Borgioni C, Ciucci A, Porcellati C . Lack of association between blood pressure variability and left ventricular mass in essential hypertension. Am J Hypertens 1998; 11: 515–522.
Pascual JM, Baldo E, Bertolin V, Rovira E, Gonzalvo F, Gonzalez C, Redon J . Ambulatory arterial pressure and left ventricular hypertrophy in untreated hypertensive patients. Med Clin 1999; 112: 166–170.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T . A reliable index for the prognostic significance of blood pressure variability. J Hypertens 2005; 23: 505–511.
Pierdomenico SD, Di Nicola M, Esposito AL, Di Mascio R, Ballone E, Lapenna D, Cuccurullo F . Prognostic value of different indices of blood pressure variability in hypertensive patients. Am J Hypertens 2009; 22: 842–847.
Frattola A, Parati G, Cuspidi C, Albini F, Mancia G . Prognostic value of 24-hour blood pressure variability. J Hypertens 1993; 11: 1133–1137.
Palatini P, Penzo M, Racioppa A, Zugno E, Guzzardi G, Anaclerio M, Pessina AC . Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Arch Intern Med 1992; 152: 1855–1860.
London GM . Role of arterial wall properties in the pathogenesis of systolic hypertension. Am J Hypertens 2005; 18: 19s–22s.
Hocht C, Bertera FM, Taira CA . Importance of blood pressure variability in the assessment of cardiovascular risk and benefits of antihypertensive therapy. Expert Rev Clin Pharmacol 2010; 3: 617–621.
Dolan E, O'Brien E . Blood pressure variability: clarity for clinical practice. Hypertension 2010; 56: 179–181.
Levi-Marpillat N, MacQuin-Mavier I, Tropeano AI, Parati G, Maison P . Antihypertensive drug classes have different effects on short-term blood pressure variability in essential hypertension. Hypertens Res 2014; 37: 585–590.
Colivicchi F, Guerrera C, Melina G, Bevilacqua E . Ambulatory blood pressure and cardiac rhythm disturbances in elderly hypertensives: relation to left ventricular mass and filling pattern. Age and ageing. Age Ageing 1996; 25: 155–158.
Polónia J, Amado P, Barbosa L, Nazaré J, Silva JA, Bertoquini S, Martins L, Carmona J . Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage. A cross-sectional study in 743 subjects. Rev Port Cardiol 2005; 24: 65–78.
Acknowledgements
We acknowledge Professor John Browne of the Department of Epidemiology and Public Health in University College Cork for his postgraduate module course PG7016 ‘Systematic Reviews for the Health Sciences’. This module was completed by both JMM and AMOF. This research was funded by the Health Research Board PhD/2007/16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JMM is currently receiving funding from the Health Research Board Ireland: PhD Scholars programme. AMOF is currently receiving funding from a Health Research Board Ireland research training fellowship for healthcare professionals and has received the John Feely research bursary from the Irish Heart Foundation to support this work. She has also received payment unrelated to the submitted work through her institution for the development of the European Society of Cardiology e-learning platform. APF has no conflicts of interest to declare. PMK has received grants from the Health Research Board Ireland and the European Union FP7 for activities outside of the submitted work.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Madden, J., O'Flynn, A., Fitzgerald, A. et al. Correlation between short-term blood pressure variability and left-ventricular mass index: a meta-analysis. Hypertens Res 39, 171–177 (2016). https://doi.org/10.1038/hr.2015.126
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.126
Keywords
This article is cited by
-
Very short-term beat-by-beat blood pressure variability in the supine position at rest correlates well with the nocturnal blood pressure variability assessed by ambulatory blood pressure monitoring
Hypertension Research (2022)
-
Association of home and ambulatory blood pressure variability with left ventricular mass index in chronic kidney disease patients
Hypertension Research (2021)
-
Blood pressure variability: its relevance for cardiovascular homeostasis and cardiovascular diseases
Hypertension Research (2020)
-
Differences in visit-to-visit blood pressure variability between normotensive and hypertensive pregnant women
Hypertension Research (2019)
-
Baroreflex failure and beat-to-beat blood pressure variation
Hypertension Research (2018)




