Abstract
Our aim was to clarify the perinatal outcomes of and risk factors for hypertension that is first detected after labor onset (labor onset hypertension, LOH), which may be a risk factor for eclampsia and stroke during labor. A total of 1349 parturient women who did not exhibit preeclampsia or gestational hypertension prior to labor were examined. The patients were classified into four groups: the normotensive (n=1023) (whose systolic blood pressure (SBP) remained below 140 mm Hg throughout labor), mild LOH (n=241) (whose maximum SBP during labor ranged from 140 to 159 mm Hg), severe LOH (n=66) (whose maximum SBP during labor ranged from 160 to 179 mm Hg) and emergent LOH groups (n=19) (whose maximum SBP during labor was greater than 180 mm Hg). The perinatal outcomes and patient characteristics of the four groups were compared. Twenty-four percent of the pregnant women who remained normotensive throughout pregnancy developed hypertension during labor. One of the patients in the emergent LOH group developed eclampsia. The blood pressure at delivery and frequencies of hypotensor use, interventional delivery and low Apgar scores differed significantly among the four groups. The following risk factors for severe/emergent LOH were extracted: being over 35 years old, a body mass index at delivery of >30, an SBP at 36 weeks’ gestation of 130–134 mm Hg, an SBP at admission of 130–139 mm Hg, proteinuria (a score of 2+ on the dipstick test) and severe edema. The risk factors for severe/emergent LOH were identified in this study. In high risk cases, repeatedly measuring maternal blood pressure during delivery might help detect critical hypertension early.
Similar content being viewed by others
Introduction
Eclampsia and stroke during pregnancy are major causes of maternal and neonatal death in many countries.1, 2, 3 Women are at a greater risk of stroke during late pregnancy, delivery and the postpartum period, which highlights the importance of blood pressure management during the period around delivery.4, 5 When pregnant women are diagnosed with preeclampsia before the onset of labor, careful blood pressure management can be initiated.6 Alternatively, we have experienced cases in which pregnant women remained normotensive throughout pregnancy but then developed hypertension during labor.7, 8, 9, 10 These patients might be at risk for eclampsia or stroke during labor. Our recent study showed that 37% of eclampsia episodes and 18% of pregnancy-associated strokes occur during labor.11 In addition, hypertension was not observed before labor onset in 55% (41/75 cases) of patients who developed eclampsia and 56% (5/9 cases) of those who suffer strokes during labor (Ohno Y, 2015, manuscript in preparation). Lao et al.12 also demonstrated that hypertension was not detected before labor onset in 53% (10/19 cases) of cases of eclampsia during labor. Nevertheless, a survey we conducted in Aichi prefecture, Japan, in 2012, showed that only 53% of medical institutions measured every patient’s blood pressure during labor.11 However, the abovementioned findings suggest that clinicians should monitor blood pressure during labor in all cases. Labor onset hypertension (LOH) might have a different pathophysiology from gestational hypertension or preeclampsia that develops before labor onset.10 However, it is not currently classified as an independent condition. In addition, the limited amount of data available about LOH and the blood pressure changes that occur during labor make it difficult to establish management strategies for LOH. In the present study, we examined the changes in maternal blood pressure induced during labor and the clinical significance of LOH as well as studied the risk factors for LOH.
Methods
Subjects
To increase the amount of data available on the blood pressure changes that occur during labor, we studied 1349 Japanese pregnant women who delivered their babies at the Ohno Ladies Clinic without any complications or preeclampsia between June 2009 and December 2011. Pregnant women who developed complications, such as gestational hypertension or preeclampsia before the onset of labor, were moved to more intensive medical facilities and excluded from the present study. In addition, the subjects were restricted to women who delivered their babies at term. Patients with diabetes, chronic smokers and habitual drinkers were also excluded. During delivery and at each routine prenatal check-up, maternal blood pressure was measured in the right upper arm using an automated sphygmomanometer (HEM7300W, OMRON Healthcare, Tokyo, Japan) while the subject was in the supine position. The OMRON7300W passed both phases of the European Society of Hypertension validation protocol in tests involving women alone and both men and women.13 The OMRON7300W is used in combination with the OMRON-MIT system, which has been demonstrated to produce accurate readings in pregnant women, including those with preeclampsia.14 Blood pressure was measured at admission, every 2 h (or at shorter intervals) during labor, just after delivery, and at 1 and 2 h after delivery. If a patient’s systolic blood pressure (SBP) reached ⩾140 mm Hg, their blood pressure was measured again within 30 min. LOH was diagnosed when SBP measurements of ⩾140 mm Hg were obtained on at least two occasions after the onset of labor in a patient who was previously normotensive. We explained the study contents to all of the patients and obtained their consent, and the study protocol was approved by the institutional review board of Toyama University.
The patients were classified into four groups: the normotensive group, whose SBP remained below 140 mm Hg throughout labor; the mild LOH group, whose maximum SBP during labor ranged from 140 to 159 mm Hg; the severe LOH group, whose maximum SBP during labor ranged from 160 to 179 mm Hg; and the emergent LOH group, whose maximum SBP during labor was greater than 180 mm Hg.
The following perinatal parameters were compared among the four groups: the Apgar score, birth weight, umbilical arterial pH, delivery mode, hypotensor usage and postpartum blood pressure. An interventional delivery included emergency cesarean sections and vacuum extractions. To examine the background factors associated with the onset of LOH, the following patient characteristics were also compared among the groups: age, parity, body mass index (BMI), a family history of hypertension, prenatal blood pressure, prenatal urinary protein concentration and blood parameters, including the WBC count, hematocrit level and platelet count. The degree of proteinuria was assessed by subjecting spot urine samples to a dipstick test (Uristics, Siemens Healthcare, Tokyo, Japan).
Statistical analysis
Statistical analyses were performed using a one-way analysis of variance, chi-square test or multivariate logistic regression analysis involving a forward stepwise selection procedure. P-values of <0.05 were considered significant. All statistical analyses were performed using the SPSS software (version 21.0; IBM Japan, Tokyo, Japan).
Results
There were 1023 (76%), 241 (18%), 66 (5%) and 19 (1%) patients in the normotensive, mild LOH, severe LOH and emergent LOH groups, respectively. Alternatively, when blood pressure on admission was used to classify the patients into the same four groups, there were 1226 (91%), 111 (8%) and 12 (1%) patients in the normotensive, mild LOH and severe LOH groups, respectively. Of the 1226 patients who displayed normal blood pressure on admission, 160 (13%), 34 (3%) and 9 (1%) demonstrated mild hypertension, severe hypertension and emergent hypertension, respectively, during the period between admission and delivery.
The maternal age, pre-pregnancy BMI, BMI at delivery and frequency of a family history of hypertension differed significantly among the four groups (Table 1).
For the subjects’ antenatal findings, the SBP values recorded between 20 and 39 weeks’ gestation, WBC count at 37 weeks’ gestation, frequency of urinary protein positivity during pregnancy and frequency of severe edema during pregnancy differed significantly among the four groups (Table 2).
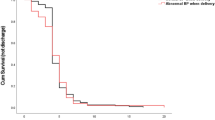
Regarding the subjects’ perinatal outcomes, the SBP at delivery, at 1 and 2 h after delivery, and during the postpartum period as well as the frequencies of hypotensor use and interventional delivery differed significantly among the four groups. The hypotensors used during delivery included oral hydralazine (in two patients with mild LOH) and i.v. nicardipine (in six patients with severe LOH and seven patients with emergent LOH). One of the patients in the emergent LOH group developed eclampsia during labor. In the emergent LOH group, seven patients delivered their babies via vacuum extraction or cesarean section because of eclampsia (one case), hypertension (seven cases), severe headache (three cases), frequent vomiting (one case) and/or a non-reassuring fetal status (three cases). The Apgar scores (at 1 min and 5 min) for the newborn babies also differed significantly among the four groups, although the inter-group differences in these parameters were not as significant as those for the abovementioned parameters. However, the birth weight and umbilical arterial blood pH did not differ significantly among the four groups (Table 3).
The multivariate analysis extracted the following parameters as risk factors for severe/emergent LOH: being 35 years or older (odds ratio (OR): 2.38, 95% confidence interval (CI): 1.19–4.77), having a BMI at delivery of ⩾30 (OR: 2.85, 95%CI: 1.04–7.79), having an SBP at 36 weeks’ gestation of 130–134 mm Hg (OR: 3.10, 95%CI: 1.27–7.53), having an SBP at admission of 130–134 mm Hg (OR: 4.00, 95%CI: 2.08–7.69), having an SBP at admission of 135–139 mm Hg (OR: 17.0, 95%CI: 9.37–31.0), having a urinary protein score of 2+ during pregnancy (OR: 4.82, 95%CI: 1.92–12.1) and having severe edema during pregnancy (OR: 1.78, 95%CI: 1.01–3.16) (Table 4). Although a family history of hypertension (OR: 2.13, 95%CI: 1.36–3.36), a pre-pregnancy BMI of <25 (OR: 6.91, 95%CI: 2.77–17.2) and an SBP at 36 weeks’ gestation of 135–139 mm Hg (OR: 4.41, 95%CI: 1.74–11.1) were extracted as risk factors for severe/emergent LOH in the univariate analysis, they were not extracted as risk factors in the multivariate analysis (Table 4).
Discussion
In the present study, 24% of the pregnant women who remained normotensive throughout pregnancy developed maternal hypertension during labor. Of these, 5% and 1% developed severe and emergent hypertension, respectively. In addition, 17% of the patients who displayed normal blood pressure upon admission developed hypertension during labor. These findings confirm the existence of LOH. Therefore, clinicians should monitor maternal blood pressure carefully during labor, even in patients who are normotensive throughout pregnancy. We classified the study subjects into four groups on the basis of their SBP rather than their diastolic blood pressure. Preeclampsia and gestational hypertension have been defined as having an SBP of >140 mm Hg or a diastolic blood pressure of >90 mm Hg.6 Recent reports have suggested that SBP is a more important determinant of future cardiovascular and cerebrovascular events than diastolic blood pressure.15, 16 In fact, Martin et al.17 suggested that a paradigm shift toward a focus on SBP instead of diastolic blood pressure might be necessary to prevent eclampsia and/or pregnancy-associated stroke. In our study, SBP at delivery and during the postpartum period as well as the frequency of hypotensor use differed significantly among the four groups. A maternal age of >35 years, a BMI of >30 at delivery, an SBP level of >130 mm Hg at 36 weeks’ gestation and at hospitalization, urinary protein positivity (a score of 2+ on a dipstick test) during pregnancy, and severe edema during pregnancy were found to be risk factors for severe and emergent LOH. Furthermore, LOH developed in 90% (19/21 cases) of the patients who displayed urinary protein scores of 2+ within the week before delivery (Table 3). Proteinuria (a score of 2+ on a dipstick test) was also found to be a significant risk factor (OR: 4.82) for LOH (Table 4). Previous studies have indicated that 8–10% of eclamptic patients exhibit proteinuria without hypertension within the week before the onset of eclampsia.1, 2 Morikawa et al.18 reported that 50% of pregnant women that develop new-onset proteinuria in the absence of hypertension progress to preeclampsia within 3 weeks. In addition, we found that the postpartum blood pressure of the LOH group was significantly higher than that of the normotensive group. These findings suggest that LOH is the dominant risk factor for postpartum hypertension.
The main strength of our study is that it is the first to investigate LOH as an independent condition in detail. The first limitation of this study is that all the subjects were Japanese. In addition, the study population was not very large and exhibited relatively good outcomes (except for the patient who developed eclampsia). Therefore, our results cannot be extrapolated to non-Japanese populations. Further studies of the impact of LOH on maternal outcomes are necessary. The second limitation of our study is that LOH includes both labor onset preeclampsia and labor onset gestational hypertension. The hypertensive disorders that occur during pregnancy have been classified into gestational hypertension, preeclampsia, chronic hypertension and superimposed preeclampsia.6, 19 The diagnostic criteria for preeclampsia include hypertension (more than 140/90 mm Hg) and proteinuria (more than 300 mg per day, a urinary protein to creatinine ratio of more than 0.3, or a score of 1+ on a dipstick test).6, 19 Preeclampsia is associated with worse perinatal outcomes than gestational hypertension.6, 19, 20 In previous studies,7, 8, 9, 10 however, all examinations were performed without the subjects first being classified into gestational hypertension and preeclampsia groups. In our study, LOH included both labor onset gestational hypertension and labor onset preeclampsia. The diagnostic criteria for labor onset preeclampsia should include a urinary protein score of 1+ on a dipstick test at admission. We did not classify our patients using this criterion because not all of the subjects underwent urinary protein tests at admission. In the future, it will be necessary to examine LOH by reclassifying it into labor onset gestational hypertension and labor onset preeclampsia according to the amount of urinary protein detected at admission.
Strokes during pregnancy are associated with extremely significant risks for both the mother and child.3, 21, 22 The incidence rate of pregnancy-related strokes is 20–25/100 000 deliveries.23, 24, 25 Maternal strokes are associated with a mortality rate of 9–38%.23, 24, 26, 27, 28 Pregnant women might have a greater risk of strokes around delivery. Ten percent of labor-associated strokes occur antenatally, 40% occur during delivery, and 50% develop during the postpartum period.4 Our previous survey, which was conducted in Japan, revealed that 37% of eclampsia episodes and 18% of pregnancy-associated strokes occur during labor.11 Hypertension is not observed before labor onset in 55% (41/75 cases) of cases of eclampsia and 56% (5/9 cases) of cases of stroke during labor (Ohno Y, 2015, manuscript in preparation). Lao et al.12 also demonstrated that hypertension is not observed before labor onset in 53% (10/19 cases) of cases of eclampsia during labor. In addition, Suzuki et al.29 reported that three out of eight eclamptic episodes occurred during labor and that two cases were derived from LOH. A Japanese nationwide survey found that approximately 27% (66/246 cases) of eclamptic episodes involved patients who displayed elevated blood pressure at delivery without any prior symptoms of hypertension or proteinuria.30 On the basis of these findings, LOH might be a risk factor for eclampsia and stroke during labor. Thus, the above studies highlight the importance of maternal blood pressure management during labor for preventing maternal deaths due to stroke. LOH is considered to be an independent condition and is treated the same way as late onset preeclampsia or gestational hypertension around the world. Patients who develop hypertension and are diagnosed with preeclampsia during the antenatal period are managed carefully. Delivery should be considered if the patient’s condition worsens. However, in patients with LOH, the onset of hypertension might be overlooked. Accurately assessing the risk of stroke is difficult. The physiological significance of LOH has not yet been established. Several studies have reported that hypertension that initially develops during labor represents a physiological change and is associated with positive outcomes.7, 8 For example, Ales and Charlson7 suggested that hypertension that is initially detected during labor exhibits a prevalence rate of 6.2% and has an excellent prognosis. However, others have indicated that hypertension that initially develops during labor represents a late manifestation of preeclampsia and displays similar outcomes to preeclampsia.9, 10 The major difference between LOH and antenatal onset preeclampsia/gestational hypertension is that LOH occurs during labor. Long et al.10 suggests that the greater fetal demand and reduced placental blood flow observed during labor might stimulate a renin-angiotensin reflex. Thus, from a clinical and pathophysiological point of view, we consider it necessary to treat LOH and antenatal onset preeclampsia/gestational hypertension as two different conditions.
The purpose of blood pressure monitoring during labor is to avoid eclampsia and stroke. In patients whose blood pressure is greater than 160/110 mm Hg, MgSO4 and hypotensors can be used to prevent eclampsia and stroke.31 It is necessary to immediately reduce the blood pressure of patients who display blood pressure levels greater than 180/120 mm Hg (hypertensive emergencies).32, 33 In our study, 7 out of the 19 patients who developed emergent LOH were administered hypotensors during labor. Hypotensors were not used in the remaining cases because delivery occurred relatively quickly. After delivery, the patients’ clinical symptoms tended to rapidly subside. However, the early postpartum stage was considered to be the time of the greatest maternal risk.9 According to our findings, LOH might be the dominant risk factor for postpartum hypertension. In our previous survey, 44% of eclampsia episodes and 54% of strokes occurred during the postpartum period.34 Moreover, Williams and Wilson35 suggested that the risk of seizures is increased for up to 1 week postpartum. Similarly, Bateman et al.36 reported that the risk of intracerebral hemorrhaging is greatest during the postpartum period. However, in our previous survey, 14% of the participating institutions allowed supporting medical staff to decide when blood pressure measurements should be taken during labor, and 23% left decisions regarding the reporting of blood pressure data to the doctors in charge of the supporting medical staff. If a patient develops hypertension during labor, it is critical that the supporting medical staff report the patient’s blood pressure to a doctor immediately and discuss the necessity of medical interventions.34
In conclusion, LOH is a risk factor for emergent hypertension and is associated with eclampsia and strokes during labor. We advocate that clinicians should pay attention to the presence of LOH. It might be possible to predict LOH using the risk factors extracted in this study. In addition, repeated blood pressure measurements might be necessary for the successful management of LOH.
References
Douglas KA, Redman CW . Eclampsia in the United Kingdom. Br Med J 1994; 309: 1395–1400.
Kullberg G, Lindeberg S, Hanson U . Eclampsia in Sweden. Hypertens Preg 2002; 21: 13–21.
Sidorov EV, Caplan LR . Stroke in pregnancy and postpartum women. Cardiac Ther 2011; 9: 1235–1247.
James AH, Bushnell CD, Jamison MG, Myers ER . Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol 2005; 106: 509–516.
Jeng JS, Tang SC, Yip PK . Incidence and etiologies of stroke during pregnancy and puerperium as evidenced in Taiwanese women. Cerebrovasc Dis 2004; 18: 290–295.
American College of Obstetricians and Gynecologists and Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013; 122: 1122–1131.
Ales KL, Charlson ME . Prognosis of hypertension first documented during labor. Am J Perinatol 1987; 4: 317–323.
Zhang J, Klebanoff MA, Robert JM . Prediction of adverse outcomes by common definitions of hypertension in pregnancy. Obstet Gynecol 2001; 97: 261–267.
Lao TT . Pregnancy outcome in women with labor onset hypertension. Gynecol Obstet Invest 1990; 29: 173–176.
Long PA, Oats JN, Beischer NA . Labour onset preeclampsia. Aust N Z J Obstet Gynecol 1981; 21: 16–19.
Ohno Y, Furuhashi M, Ishikawa K, Kaseki S, Kondo H, Kikkawa F . Results of a questionnaire survey on pregnancy-associated stroke from 2005 to 2012 in Aichi Prefecture, Japan. Hypertens Res Preg 2014; 2: 16–20.
Lao TT, Chin RK, Leung BF . Labour related eclampsia. Eur J Obstet Gynecol 1987; 26: 97–104.
Grim CE, Grim CM . The Omron elite 7300 W home blood pressure monitor passed the European Society of Hypertension International Validation Protocol for women and men. Blood Pressure Monitoring 2009; 14: 87–90.
de Greeff A, Beg Z, Gangji Z, Dorney E, Shennan AH . Accuracy of inflationary versus deflationary oscillometry in pregnancy and preeclampsia: OMRON-MIT versus OMRON-M7. Blood Press Monit 2009; 14: 37–40.
Williams B, Lindholm LH, Sever P . Systolic pressure is all that matters. Lancet 2008; 371: 2219–2221.
Sever P . Abandoning diastole. BMJ 1999; 318: 1773.
Martin JN, Thigpen BD, Moore RC, Rose CH, Cushman J, May W . Stroke and severe preeclampsia and eclampsia: A paradigm shift focusing on systolic blood pressure. Obstet Gynecol 2005; 105: 246–254.
Morikawa M, Yamada T, Yamada T, Cho K, Yamada H, Sakuragi N, Minakami H . Pregnancy outcome of women who developed proteinuria in the absence of hypertension after mid-gestation. J Pernat Med 2008; 36: 419–424.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM . The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001; 20: IX–XIV.
Redman CW . Hypertension in pregnancy: the NICE guidelines. Heart 2011; 97: 1967–1969.
DiCarlo A, Lamassa M, Consoli D, Inzitari D, Gall SL, Donnan G, Dewey H, Thrift A . Sex differences in presentation, severity, and management of stroke in a population based study. Neurology 2010; 75: 670–671.
Benedetto C, Marozio L, Tavella AM, Salton L, Grivon S, DiGiampaolo F . Coagulation disorders in pregnancy: acquired and inherited thrombophilias. Ann NY Acad Sci 2010; 1205: 106–117.
Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, Earley CJ, Macko RF, Sloan MA, Wityk RJ, Wozniak MA . Pregnancy and the risk of stroke. N Engl J Med 1996; 335: 768–774.
Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai BM . Cerebrovascular disorders complicating pregnancy−Beyond eclampsia. Am J Obstet Gynecol 1997; 176: 1139–1148.
Lanska DJ, Kryscio RJ . Risk factors for peripartum and postpartum stroke and intracranial venous thrombosis. Stroke 2000; 31: 1274–1282.
Simolke GA, Cox SM, Cunningham FG . Cerebrovascular accidents complicating pregnancy and the puerperium. Obstet Gynecol 1991; 78: 37–42.
Sharshar T, Lamy C, Mas JL . Incidence and causes of strokes associated with pregnancy and puerperium. A study in public hospitals of IIe de France. Stroke in Pregnancy Study Group. Stroke 1995; 26: 930–936.
Jaigobin C, Silver FL . Stroke and pregnancy. Stroke 2000; 31: 2948–2951.
Kojima R, Matsuura A, Yamamoto T, Watanabe K, Suzuki Y . Characteristic changes in systolic blood pressure in eclampsia. Hypertens Res Preg 2014; 2: 11–15.
Watanabe K, Suzuki Y, Yamamoto T . Incidence of eclampsia in Japanese women. Hypertens Res Preg 2013; 1: 31–34.
Minakami H, Hiramatsu Y, Koresawa M, Fujii T, Hamada H, Iitsuka Y, Ikeda T, Ishikawa H, Ishimoto H, Itoh H, Kanayama N, Kasuga Y, Kawabata M, Konishi I, Matsubara S, Ohkuchi A, Okai T, Saito S, Sakai M, Satoh S, Sekizawa A, Suzuki M, Takahashi T, Tokunaga A, Tsukahara Y, Yoshikawa H . Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology and Japan Association of Obstetricians and Gynecologists 2011 edition. J Obstet Gynecol Res 2011; 37: 1174–1197.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ . Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42: 1206–1252.
Vaughan CJ, Delanty N . Hypertensive emergencies. Lancet 2000; 356: 411–417.
Ohno Y, Ishikawa K, Kaseki S, Kikkawa F . Questionnaire-based study of cerebrovascular complications during pregnancy in Aichi Prefecture, Japan (AICHI DATA). Hypertens Res Pregnancy 2013; 1: 40–45.
Williams KP, Wilson S . Changes in cerebral perfusion pressure in puerperal women with preeclampsia. Obstet Gynecol 1998; 92: 1016–1019.
Bateman BT, Schumacher HC, Bushnell CD, Pile-Spellman J, Simpson LL, Sacco RL, Berman MF . Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology 2006; 67: 424–429.
Acknowledgements
This study was partly supported by the Japan Society for the Study of Hypertension in Pregnancy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ohno, Y., Terauchi, M., Tamakoshi, K. et al. The risk factors for labor onset hypertension. Hypertens Res 39, 260–265 (2016). https://doi.org/10.1038/hr.2015.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.112
Keywords
This article is cited by
-
Clinical characteristics and sequelae of intrapartum hypertension – a retrospective cohort study
BMC Pregnancy and Childbirth (2023)
-
Association of reproductive history with hypertension and prehypertension in Chinese postmenopausal women: a population-based cross-sectional study
Hypertension Research (2018)
-
Effect of blood pressure on reversible posterior leukoencephalopathy syndrome in pre-eclampsia or eclampsia
Hypertension Research (2018)
-
Hypertensive disorders of pregnancy: a strong risk factor for subsequent hypertension 5 years after delivery
Hypertension Research (2018)
-
Monitoring and evaluation of out-of-office blood pressure during pregnancy
Hypertension Research (2017)