Abstract
The aim of this study was to evaluate the reliability of self-reported home blood pressure (HBP) in patients with type 2 diabetes by comparing the self-reported values with HBP measurements stored in the memory of the blood pressure (BP) monitor. We also examined what factors affect the reliability of HBP measurements. A cross-sectional study was conducted in 280 patients with type 2 diabetes. Patients were requested to perform triplicate morning and evening measurements over a span of 2 weeks and to enter their HBP values into logbooks. Patients were not informed about the memory function of their BP monitoring devices. The concordance rate of HBP reporting was 78.6%. A total of 51.4% of patients (n=144) had >90% concordant data, and 15.7% of patients (n=44) had ⩽50% concordant data. In general, HBP values from the logbook were significantly lower and less variable than those from the stored memory (P<0.05). The most common type of incorrect data was selected data that were reported in the logbooks that were randomly selected from multiple readings by the HBP monitors (55.8%). The concordance rate of HBP reporting significantly correlated with hemoglobin A1c levels (β=−0.156; P=0.0149) and with smoking status (current vs. never, β=−0.165; P=0.0184). In conclusion, HBP measurements from the patients’ logbooks were lower and less variable than those from the stored memory in the BP monitors of patients with type 2 diabetes, and the reliability of HBP reporting was affected by glycemic control and smoking status. Repeated instructions regarding HBP measurement to the patients or the use of stored BP measurements is recommended to ensure accurate HBP measurements in patients with type 2 diabetes.
Similar content being viewed by others
Introduction
The prevalence of hypertension in individuals with type 2 diabetes is higher than that in the general population.1, 2, 3 In patients with type 2 diabetes, hypertension is considered an important risk factor for cardiovascular and renal disease;2, 4 therefore, it is very important for these patients to strictly control their blood pressure (BP), as well as their blood glucose levels. The intensive lowering of BP in hypertensive patients with type 2 diabetes has been associated with the reduction of cardiovascular events, as reported by the Hypertension Optimal Treatment randomized trial5 and the United Kingdom Prospective Diabetes Study.6
Home BP (HBP) monitoring has been shown to be useful for controlling BP, and some national and international guidelines also recommend HBP monitoring in certain circumstances. In addition, HBP measurement has been found to have a stronger relationship to target organ damage in several population-based studies and prospective clinical studies.7, 8 We have also shown that the average and variability of HBP correlate with albuminuria in patients with type 2 diabetes.9, 10
However, there are few studies that have assessed the precision of self-measured BP reporting,11, 12 and to our knowledge, no study has evaluated the reliability of HBP monitoring in patients with type 2 diabetes. The aim of this study was to evaluate the reliability of self-reported HBP in patients with type 2 diabetes by comparing the self-reported values with the stored HBP measurements. We also examined what factors affect the reliability of HBP.
Methods
Patients
HBP measurements were performed by patients with type 2 diabetes (regardless of hypertensive status) who had regularly visited the diabetes outpatient clinic at the Hospital of Kyoto Prefectural University of Medicine, Kyoto, Japan between May 2011 and July 2012. We recruited patients who were able to measure their BP independently. A total of 288 patients with type 2 diabetes agreed to participate in the present study. We excluded patients who did not comply with the study protocol (n=7) and who had advanced renal dysfunction (serum creatinine ⩾176.8 μmol l−1; n=1). In all, 280 patients met the criteria and comprised the study population. The diagnosis of type 2 diabetes mellitus was based on the American Diabetes Association criteria.13 The present study was approved by the local Research Ethics Committee and was conducted in accordance with the Declaration of Helsinki; informed consent was obtained from all patients, although the patients were not aware of our aim to compare the BP values in their logbooks with those stored in the memory of the device.
Study design
To assess the accuracy of the patient-reported data, we used the following criteria. The logbooks contained the data recorded by the patients after they measured their BP. The stored memory data contained all of the recordings that were retrieved from the memory of the electronic BP device. When values from the logbook matched those of the stored memory, we defined them as concordant data. We examined the rate of concordant data (concordance rate) and compared the BP levels in the logbook and those in the stored memory. For the mismatched values, we classified the data into five categories depending on the error types. First, selected data were data that were reported in the logbooks that were randomly selected from multiple readings (more than three times) by the home BP monitors. Second, fictional data refers to values entered in the logbooks that could not be retrieved from the memory of the HBP monitors. Third, shifted data were defined as the data in the logbooks that were entered into the memory of the BP device on another day but for the same time. Fourth, switched data were defined as data in the logbooks that were entered into the memory of the BP device on another day and at a different time. Fifth, omitted data were defined as data that were found in the memory of the HBP monitors but were not entered into the logbooks. We then examined the rate of these mismatched data. In addition, we classified the patients according to their most common error type and compared the BP levels and variability for the error type (as observed in the logbooks) with the BP levels and variability stored in the memory of the HBP monitor. We used s.d. of BP as an index of day-to-day variability of HBP values in the present study.
To identify the factors that affect the accuracy of HBP measurements, we examined the relationship between the concordance rate of HBP and various factors, including sex, age, duration of diabetes, body mass index, serum cholesterol concentration, hemoglobin A1c, smoking status, alcohol status, presence of microvascular complications or macrovascular complications, memory BP and the use of antihypertensive drugs and insulin.
Data collection
Blood samples for biochemical tests were collected at the hospital. Hemoglobin A1c, low-density lipoprotein cholesterol, triglycerides, high-density lipoprotein cholesterol and other biochemical data were determined using the standard laboratory assays. Information, including age, duration of diabetes, microvascular complications, macrovascular complications, smoking and alcohol drinking status, hypoglycemic medication and antihypertensive medication, were obtained at the time of the BP measurement. Alcohol drinking status (everyday, social, never) and smoking status (current, past or never smokers) were assessed by interview.
HBP measurements were performed using an automatic device (HEM-7080IC, Omron Healthcare Co. Ltd, Kyoto, Japan) that uses the cuff-oscillometric method to generate a digital display of the heart rate and the systolic/diastolic BP (SBP/DBP) values. This monitor is also capable of electronically storing BP measurements. HEM-7080IC uses the identical components and BP-determining algorithm as another device (HEM-705IT) that was previously validated and satisfies the criteria of the British Hypertension Society protocol.14
All of the patients used this oscillometer for the first time in this study. They were instructed to perform triplicate morning and evening measurements for 14 consecutive days. Morning BP measurements were made within 1 h of waking, before breakfast or taking any drugs and after the patient had been seated and rested for at least 5 min.15 Evening BP measurements were obtained in a similar manner just before bedtime. The cuff was placed directly around the non-dominant arm, and the position of the cuff was maintained at the level of the heart.
Statistical analysis
Values are expressed as the mean±s.d. for continuous variables. A paired t-test was used to assess the difference between memory and logbook BP values. Linear regression analyses, Student’s t-test and one-way analysis of variance were used to assess the relationship between the concordance rate and the factors that affect the accuracy of reporting. We chose the variables significantly related with HBP concordance rate by univariate regression analysis, Student’s t-test and one-way analysis of variance as covariates in a multivariate analysis. All statistical analyses were performed using the JMP software (JMP; SAS Institute Inc., Cary, NC, USA).
Results
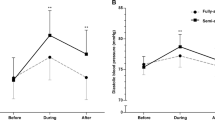
The clinical characteristics of the patients are shown in Table 1. A total of 55.4% of the patients (n=155) took antihypertensive medications during the study. We collected an average (s.d.) of 79.9±7.8 HBP measurements and 6.3±7.3 erroneous data points from each patient. The concordance rate between the BP values from the stored memory and those from the logbooks was 78.6%. A total of 23.2% of patients (n=65) had 100% concordant measurements, and 51.4% of patients (n=144) had >90% concordance. A total of 15.7% of the patients (n=44) had ⩽50% concordant measurements (Figure 1).
The mean of the morning SBP and DBP retrieved from the stored memory were 130.6±16.2 mm Hg and 72.6±9.7 mm Hg, respectively. The mean of the morning SBP and DBP from the logbooks were 129.8±15.8 mm Hg and 72.2±9.5 mm Hg, respectively (Table 2). Morning and evening BP values from the logbooks were significantly lower than those from the stored memory. The s.d. of the BP values from the logbooks was also lower than that of the BP values from the stored memory.
The most common error was selected data (55.8%), but fictional data were present for 23.3% of the patients. Shifted data, switched data and omitted data were found in 11.6%, 6.0% and 3.3% of the patients, respectively. The mean of the morning SBP and DBP measurements that were retrieved from the stored memory were not significantly different among the five error types. However, for selected and shifted data, the mean of the morning SBP and DBP values that were retrieved from the logbooks were significantly lower than those retrieved from the stored memory (Supplementary Table S1). The s.d. of the morning SBP values retrieved from the logbooks were significantly lower than those from the stored memory in selected, fictional and shifted data. The s.d. of the morning DBP measurements that were retrieved from the logbooks were also significantly lower than those from the stored memory in selected and shifted data.
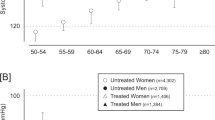
Hemoglobin A1c, high-density lipoprotein cholesterol, triglycerides, mean of the morning SBP, mean of the evening DBP and the morning SBP s.d. from the stored memory were significantly correlated with the HBP concordance rate (Table 3). In addition, the HBP concordance rate was significantly lower in current smokers than that in non-smokers (Table 4). Multivariate linear regression analysis indicated that the independent explanatory variables concerning the HBP concordance rate were hemoglobin A1c and smoking status (Table 5).
Discussion
This study revealed that the mean and the s.d. of HBP values from the logbooks were significantly lower and smaller, respectively, than those from the stored memory and that the main HBP reporting error was data selection by patients. In addition, we found that hemoglobin A1c and smoking status significantly correlated with the inaccuracy of HBP reporting. The accuracy of HBP was decreased in patients with poorly controlled glycemia and in those who smoked. Possible explanations for this decrease in accuracy are that the patients were concerned about increasing their antihypertensive medication or that their health consciousness might have been poor.
Moreover, we analyzed HBP measurement accuracy in patients who were taking or not taking antihypertensive drugs. The HBP concordance rates between the two groups was similar (76.7±23.3%, 80.9±24.8%, P=0.1852), and the mean and the s.d. of HBP values from the logbooks were significantly lower and smaller, respectively, than those from the stored memory in each group. The mean of the morning SBP from the logbooks was significantly lower than that from the stored memory from patients with (132.7±15.4 vs. 133.7±16.0 mm Hg, P=0.0002) or without (126.1±15.5 vs. 126.7±15.7 mm Hg, P=0.0031) antihypertensive drugs. The s.d. of the morning SBP from the logbooks was significantly less than that from the stored memory from patients with (8.2±3.2 vs. 10.1±3.6, P<0.0001) or without (7.4±3.2 vs. 9.4±3.3, P<0.0001) antihypertensive drugs. The HBP concordance rate was negatively correlated with the mean HBP and smoking status and was significantly lower in current smokers than in past or non-smokers taking antihypertensive drugs. This result was not observed in patients who did not take antihypertensive drugs (Supplementary Tables S2 and S3). We should pay more attention to the accuracy of HBP in patients who take antihypertensive drugs, who have poor control of their HBP or who smoke.
In this study, the HBP concordance rate between the logbooks and the stored memory was similar to previous studies in non-diabetic patients.11, 12 Our findings were also similar to the results of a study by Mazze et al.,16 who evaluated the reliability of self-reported capillary glucose measurements in logbooks (74%). Their study found that the mean blood glucose values from the logbooks were significantly lower than those from the stored memory in many cases, primarily because blood glucose measurements >13.9 mmol l−1 (250 mg dl−1) were omitted from their logbooks. Patients had a tendency to select their HBP measurements; therefore, the logbook BP values were significantly lower and less variable than memory BP values in this study. It seems that patients omitted the measurements when the measurements were higher or lower than expected in HBP reporting. Therefore, the differences in the mean BP between the stored memory and the logbooks were small in our study. However, a previous study has shown that even slight differences in SBP significantly decrease cardiovascular events;17 therefore, the findings of our study may be valuable in this regard. Moreover, we analyzed the relationship between the BP level and the difference between the BP measurements retrieved from the logbooks and from the stored memory (Supplementary Figure S1). Linear regression analysis showed that there was a significant relationship between the absolute value of the difference in the morning SBP and the mean of the morning SBP (P=0.0015). Therefore, we should consider the possibility of differences between the values in the logbooks and the actual BP in patients with poorly controlled hypertension.
HBP concordance rates were similar among the studies by Nordmann et al.11 and Johnson et al.12 and ours. However, they assessed the accuracy of HBP in patients with hypertension, and we assessed HBP in patients with type 2 diabetes, which we believe is novel. Moreover, the number of patients was larger in our study than in the other aforementioned studies. Nordmann et al.11 suggested that low education level was the only independent predictor of poor BP measurement accuracy. However, there was no relationship between the educational level and the accuracy of HBP measurement in some of the patients (n=197) in our study (P=0.9437), and there was no relationship between cognitive function (as measured by mini-cog test)18, 19 and the accuracy of HBP reporting (P=0.1949) in most of our patients (n=263). This may be because there were no patients in this study with severe cognitive dysfunction who were unable to measure their BP. Johnson et al.12 found that erroneous reporting was evident in patients with uncontrolled BP, which is in accordance with our data. In addition, there was no relationship between the accuracy of HBP measurements and the number of antihypertensive medications or the accuracy of HBP measurements and the timing of the HBP measurements. However, there was a tendency for the concordance rate for the first half of the study (days 1–7) to be higher than that of the second half (days 8–14) (80.5±25.5%; 76.8±30.6%, P=0.0013). There might be an experience effect on the accuracy of HBP measurements partly, because the patients paid less attention to HBP measurements as the study progressed.
The present study has some limitations. First, the number of patients was relatively small, because we chose patients who had never borrowed a BP monitor from us. However, this is the first study to evaluate the reliability of HBP in patients with type 2 diabetes and to identify the main errors of HBP reporting and the factors that affect the reliability of HBP reporting. Second, patients might have noticed the memory function, as mentioned on the face of the oscillometer and in the instruction manual. This knowledge might have resulted in reporting bias. However, when we provided the new logbook with the oscillometer to the patients in this study, the patients seemed to believe that we would analyze their new logbook data. Moreover, patients were not aware of our aim to compare their HBP measurements in the logbook with those recorded by the oscillometer; therefore, significantly biased reporting seems unlikely. Third, there might be weekly differences in the accuracy of HBP measurements. However, we did not account for the work day of each patient and could not assess any weekly differences by separating the HBP data into week day and weekend categories. Fourth, unfortunately, we do not have data regarding HBP monitoring experience of the patients before this study. Therefore, there is a possibility that previous experience of HBP monitoring affected the accuracy of HBP reporting.
In conclusion, patients with type 2 diabetes sometimes reported inaccurate HBP measurements and, as a result, HBP control from the logbooks appeared better than that from the stored memory. False reporting of BP may misguide physicians, resulting in inadequate medical treatment of their patients. To obtain the true HBP value, we should instruct patients to record the HBP measurement correctly. Specifically, patients with poorly controlled glycemia or who smoke may need repeated instructions. Furthermore, it may be helpful to use automatic devices that can store BP measurements for the proper assessment of BP control.
References
Iimura O . Insulin resistance and hypertension in Japanese. Hypertens Res 1996; 19 (Suppl 1): S1–S8.
Hypertension in Diabetes Study Group. HDS 1: prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardio-vascular and diabetic complications. J Hypertens 1993; 11: 309–317.
Garcia MJ, McNamara PM, Gordon T, Kannell WB . Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up. Diabetes 1974; 23: 105–111.
American Diabetes Association. Role of cardiovascular risk factors in prevention and treatment of macrovascular disease in diabetes. Diabetes Care 1989; 12: 573–579.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S . Effects of intensive blood pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet 1998; 351: 1755–1762.
UK prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998; 317: 703–713.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S . Home blood pressure measurement ha a stronger predictive power for mortality than does screening blood pressure measurement: a population- based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
Sega R, Trochino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G . Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study). Circulation 2001; 104: 1385–1392.
Ushigome E, Fukui M, Hamaguchi M, Senmaru T, Sakabe K, Tanaka M, Yamazaki M, Hasegawa G, Nakamura N . The coefficient variation of home blood pressure is a novel factor associated with macroalbuminuria in type 2 diabetes mellitus. Hypertens Res 2011; 34: 1271–1275.
Ushigome E, Fukui M, Sakabe K, Tanaka M, Inada S, Omoto A, Tanaka T, Fukuda W, Atsuta H, Ohnishi M, Mogami S, Kitagawa Y, Oda Y, Yamazaki M, Hasegawa G, Nakamura N . Uncontrolled home blood pressure in the morning is associated with nephropathy in Japanese type 2 diabetes. Heart Vessels 2011; 11: 609–615.
Nordmann A, Frach B, Walker T, Martina B, Battegay E . Reliability of patients measuring blood pressure at home: prospective observational study. BMJ 1999; 319: 1172.
Johnson KA, Partschi DJ, Rippole LL, McVey DM . Reliability of self-reported blood pressure measurements. Arch Intern Med 1999; 159: 2689–2693.
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2002; 25: S5–20.
Coleman A, Freeman P, Steel S, Shennan A . Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit 2006; 11: 27–32.
Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, Miyakawa M, Fukiyama K, Japanese Society of Hypertension. Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res 2003; 26: 771–782.
Mazze RS, Shamoon H, Pasmantier R, Lucido D, Murphy J, Hartmann K, Kuykendall V, Lopatin W . Reliability of blood glucose monitoring by subjects with diabetes mellitus. Am J Med 1984; 77: 211–217.
Staessen JA, Wang JG, Thijs L . Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens 2003; 21: 1055–1076.
Borson S, Scanlan JM, Chen P, Ganguli M . The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc 2003; 51: 1451–1454.
Borson S, Scanlan JM, Watanabe J, Tu SP, Lessig M . Simplifying detection of cognitive impairment: comparison of the Mini-Cog and Mini-Mental State Examination in a multiethnic sample. J Am Geriatr Soc 2005; 53: 871–874.
Acknowledgements
We thank Naoko Higo, Machiko Hasegawa and Terumi Kaneko for teaching the patients how to measure their blood pressure; Sayoko Tanaka, Hiroko Kawamura and Sanae Utena for their secretarial assistance; and Akane Miki for her enormous help with data handling. Each of these individuals is affiliated with Kyoto Prefectural University of Medicine, Kyoto, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Rights and permissions
About this article
Cite this article
Matsumoto, S., Fukui, M., Hamaguchi, M. et al. Is home blood pressure reporting in patients with type 2 diabetes reliable?. Hypertens Res 37, 741–745 (2014). https://doi.org/10.1038/hr.2014.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.66
Keywords
This article is cited by
-
Factors influencing home blood pressure monitor ownership in a large clinical trial
Journal of Human Hypertension (2022)
-
Methods of Blood Pressure Measurement to Predict Hypertension-Related Cardiovascular Morbidity and Mortality
Current Cardiology Reports (2022)
-
Big data and real-world data-based medicine in the management of hypertension
Hypertension Research (2021)
-
Predictive power of home blood pressure measurement for cardiovascular outcomes in patients with type 2 diabetes: KAMOGAWA-HBP study
Hypertension Research (2021)