Abstract
Pneumonia is one of the most frequent complications in elderly patients with acute ischemic stroke. Although severe hypertension is often observed in the early phase of acute stroke, there are few studies of acute hypertension as a factor influencing the incidence of stroke-associated pneumonia (SAP) in elderly subjects with acute ischemic stroke. To assess the association of acute phase blood-pressure elevation with the incidence of SAP, we compared 10 elderly patients with acute ischemic stroke complicated with severe hypertension (⩾200/120 mm Hg) with 43 patients with moderate hypertension (160–199/100–119 mm Hg), as well as with 65 control normotensive or mildly hypertensive (<160/100 mm Hg) controls on admission. Data were collected on known risk factors, type of ischemic stroke and underlying chronic conditions. The significance of differences in risk factors was analyzed using univariate and multivariate comparisons of 38 SAP cases and others, 8 SAP death cases and others, and 28 patients with poor outcome associated with in-hospital death or artificial feeding at discharge and others. After adjustment for potential confounding factors, the relative risk estimates for SAP, SAP death and poor outcome were 2.83 (95% confidence interval 1.14–7.05), 5.20 (1.01–26.8) and 6.84 (1.32–35.4), respectively, for severe hypertension relative to normotensive or mildly hypertensive controls. We conclude that severe hypertension on admission is an independent predictive factor for SAP in elderly patients with acute ischemic stroke.
Similar content being viewed by others
Introduction
Stroke-associated pneumonia (SAP) is among the leading complications of stroke,1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 and is an important cause of death after cerebrovascular events.1, 3, 4 SAP is most likely to develop in patients who are seriously ill and those with dysphagia. There are various data available on independent predictors of SAP in treated acute stroke patients. In those studies, a number of risk factors have been reported, such as lower baseline Glasgow Coma Scale score,4, 5, 6 dysphagia,7, 8, 9 male sex,3, 7, 9, 10 stroke subtype,8, 9 diabetes,10 ischemic heart disease9 and chronic congestive heart failure.11 SAP is known to occur more frequently in elderly patients,2, 3, 9, 10, 11 although conflicting results are also reported.4 Besides SAP, severe arterial hypertension is another frequent medical complication observed in patients with acute ischemic stroke within the first week after admission.12, 13, 14, 15, 16 This increased blood pressure (BP) falls spontaneously within the first week, without specific antihypertensive therapy.17 Severe hypertension in the early phase of acute ischemic stroke is another sign associated with poor functional outcome and higher mortality.18, 19, 20 As yet, however, there are only limited data on the association of SAP with severe arterial hypertension in patients with acute stroke. We here present a study of SAP in elderly patients admitted to our hospital with acute ischemic stroke associated with severe hypertension with systolic BP (SBP) ⩾200 mm Hg and/or diastolic BP (DBP) ⩾120 mm Hg on admission.21 The results were compared with those in elderly patients with acute ischemic stroke with moderate hypertension with SBP 160–199 mm Hg and/or DBP 100–119 mm Hg, who may develop signs of encephalopathy,22 and with normotensive and/or mildly hypertensive controls with SBP <160 mm Hg and DBP <100 mm Hg.
Methods
Subjects
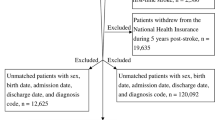
Consecutive patients admitted to the Geriatric Emergency Ward of Kanazawa Medical University Hospital, a major urban hospital in Ishikawa Prefecture, Japan, with a diagnosis of ischemic stroke during 2002–2010 were recruited into the study. Patients participating in this study were 70 years of age or older, and had both clinical and neuroimaging evidence of ischemic cerebral infarction. Only patients with symptom onset within 24 h of admission were included in this study. All subjects were systematically evaluated. Neurovascular evaluation, including assessment of underlying chronic conditions, serial neurological examinations including Glasgow Coma Scale, 12-lead electrocardiograms, chest X-ray examination and transthoracic echocardiograms, in addition to routine hematologic and chemistry tests were completed in all subjects. The presence of dysphagia was screened in all the study subjects. For this, clinical examination and a water swallowing test with pulse oximetry were performed, and a drop in arterial oxygen saturation of >2% within 2 min after swallowing was considered clinically significant to detect dysphagia with silent aspiration or cough.23 Dysphagia with impaired voice or complete dysphagia without swallowing was also considered to indicate the presence of dysphagia. During this period, vital signs, including noninvasive cuff BP, pulse rate and body temperature, were measured at least every 2 h during the first 24 h and continued every 2–8 h up to 72 h. Antihypertensive medication was given at the discretion of physicians not involved in the study, who in general followed the recommendations of the Guidelines for the Management of Hypertension published in 2009 by the Japanese Society of Hypertension Committee (JSH 2009)24 for BP of 220/120 mm Hg and higher. The patients were divided into three groups according to the record of the highest mean SBP and/or DBP of two measurements every 2 h during the first 24 h after admission; control patients with normotension to mild hypertension (SBP <160 mm Hg and DBP <100 mm Hg), patients with moderate hypertension (SBP 160–199 mm Hg and/or DBP 100–119 mm Hg) and those with severe hypertension (SBP ⩾200 mm Hg and/or DBP ⩾120 mm Hg).
Assessment of brain lesions
All patients underwent brain magnetic resonance imaging and magnetic resonance angiography on the first day of admission. Imaging was performed using a 1.5-T MRI (Model: MAGNETOM Avanto, Siemens Medical Solution, Erlangen, Germany). Acute ischemic lesions were assessed by diffusion-weighted imaging with apparent diffusion coefficient. Ischemic lesions on diffusion-weighted imaging were classified as single lesions (corticosubcortical lesion, cortical lesion, subcortical lesion with diameter >15 mm or subcortical lesion with diameter <15 mm), scattered lesions in one vascular territory (small (<15 mm) scattered lesions or confluent (>15 mm) lesions with an additional lesion) and multiple lesions in multiple vascular territories (in the unilateral anterior circulation, posterior circulation, bilateral anterior circulation or anterior and posterior circulation). Stroke subtype classification was performed according to a previous report.25 Patients with diffusion-weighted imaging imaging findings of a corticosubcortical single lesion and those with multiple lesions in both the anterior and posterior circulation were classified as having cardiac embolism if they had atrial fibrillation and/or another cardioembolic source. Those with subcortical small lesion(s) (<15 mm) were classified as having small-vessel occlusion. Those with subcortical lesion(s) (<20 mm) were also classified as having small-vessel occlusion according to the recommendations in the report.25 Other patients with atrial fibrillation and/or another cardioembolic sources were classified as having cardiac embolism. Patients without a cardioembolic source were classified as having large-artery atherosclerosis. Patients with transient ischemia with no visible lesion on diffusion-weighted imaging were excluded from this study.
Underlying chronic conditions
We observed the clinical features of the enrolled patients, including past history of stroke, ischemic heart disease, chronic congestive heart failure, chronic kidney disease, diabetes mellitus and hypertension under treatment with an antihypertensive agents. Operational definitions of each preexisting chronic condition were established prior to data collection, including past history of stroke (evidence of chronic phase of stroke on magnetic resonance imaging), ischemic heart disease (evidence on electrocardiography or echocardiography), chronic congestive heart failure (left ventricular ejection fraction ⩽40%), chronic kidney disease (estimated glomerular filtration rate with coefficients modified for Japanese patients:26 194 × Cr−1.094 × age−0.287 ( × 0.739 if female) <60 ml min−1 1.73 m−2), diabetes mellitus (use of hypoglycemic agents and/or insulin) and hypertension (use of antihypertensive agents).
Definitions of SAP and poor outcome
Patients with (without) SAP are referred to as SAP+ (SAP−) patients. The definition of SAP includes either the clinical finding of rales or dullness to percussion and one of the following: purulent sputum, isolation of the organism, chest radiograph showing evidence of an infiltrate/consolidation/cavitation or pleural effusion, and one of the following: purulent sputum, isolation of the agent or antibody evidence of an agent.7 Definition of SAP death was defined as death in SAP patients during in-hospital treatment. The definition of poor outcome was either in-hospital death or artificial feeding at discharge. Patients who had a prior history of dysphagia before the index stroke and those who required mechanical ventilation during the hospital stay were excluded. Patients who had another identifiable source of infection before the development of pneumonia and those who had fever before stroke onset were also excluded.
Statistical methods
For comparing cases and controls, we used univariate analyses including χ2 test (Fisher's exact test when needed) for comparing categorical variables and nonparametric Mann–Whitney U statistics for comparing the distributions of ordinal variables. Continuous variables were compared among the three hypertensive states by one-way ANOVA, with Tukey's test for post-hoc comparisons. The distribution of serum C-reactive protein level was positively skewed, and was therefore log transformed before statistical comparison. Results were then expressed in natural units for ease of interpretation. Discrete variables were reported as percentages and compared by χ2 analysis. Logistic regression analysis was used to identify factors independently associated with SAP after adjustment for confounding variables. Common pitfalls associated with multivariate regression were avoided as described by Cibcati et al.27 The odds ratio (OR) for severe hypertension associated with various conditions was calculated by logistic regression analysis, adjusting for age, sex and all associated variables selected according to their univariate analysis P-value (P<0.10). Estimates for OR and corresponding two-sided 95% confidence interval (CI) demonstrating statistical significance were derived from the regression model. Data were analyzed using SPSS (v. 16.0, Chicago, IL, USA). A probability of P<0.05 was taken as statistically significant.
Results
Study population
A total of 118 patients (mean age 84 6±5.4 years, range 72–96 years; 58 men, 85.0±5.1 years; 60 women, 84.2±5.7 years) with complete ischemic stroke were included. The mean duration of treatment was 25.7±7.2 days (range 1–109 days). Hemispheric infarction was documented in 104 (88%) patients, with more than one hemispheric territory affected in 14 of them. According to the results of magnetic resonance imaging, 62 patients were classified as having large-artery atherosclerosis, 22 small-vessel occlusion and 34 cardiac embolism.
Characteristics of SAP
SAP occurred in 38 (30.5%) out of 118 patients, with a mean latency from admission of 1.8±2.7 days (range 0–12 days). These 38 SAP+ patients were compared with 80 SAP− patients (Table 1). SAP+ patients had higher mean SBP compared with SAP− patients (166±31 vs. 150±28 mm Hg, P=0.006), higher mean pulse BP (80±22 vs. 69±20 mm Hg, P=0.018), lower Glasgow Coma Scale score (11.8±3.4 vs. 13.6±2.6, P=0.001), higher WBC count (8.13±2.55 vs. 6.08±1.42 × 1012 l−1, P<0.001), higher serum C-reactive protein (7.9 with s.d. range 1.5–40.9 vs. 3.8 with s.d. range 1.0–6.0, P<0.001) and higher incidence of dysphagia (44.7% vs. 15.0%, P=0.001) on admission. However, there was no significant difference in age, sex, type of ischemic stroke or underlying chronic conditions including prior use of antihypertensive agents (Table 1).
Clinical predictors of SAP
The Glasgow Coma Scale score was significantly higher in both the moderate hypertensive group and severe hypertensive group than in the control group. WBC count was also significantly higher in the severe hypertensive group, and the incidence of dysphagia was significantly higher in the moderately hypertensive group than in the control group. The clinical background, frequency of underlying chronic conditions and previous use of antihypertensive medication were similar in the three hypertensive states, although previous use of antihypertensive medication in moderately hypertensives was significantly higher than that in normotensive/mildly hypertensive controls (Table 2).
Logistic regression analysis using age, sex, Glasgow Coma Scale score, WBC count, log(serum C-reactive protein), dysphagia and hypertensive state as confounding factors revealed that log(serum C-reactive protein) (OR: 1.89, 95% CI: 1.26–2.85, P=0.002), WBC count (OR: 1.47, 95% CI: 1.11–1.95, P=0.008) and hypertensive state (OR: 2.27, 95% CI: 1.04–4.97, P=0.040) were independently and significantly associated with an increased risk of SAP. Conditional logistic regression analysis revealed a significantly higher risk of SAP in those with severe hypertension, with adjusted OR estimate of 2.83 and CI 1.14–7.05, with control BP level as the reference group (Table 3). Even when the previous use of antihypertensive medication was added as another confounding factor to those above, hypertensive state was still independently and significantly associated with an increased risk of SAP (OR: 2.26, 95% CI: 1.03–4.94, P=0.041) by logistic regression analysis, and a significant increase in the risk of SAP in those with severe hypertension (OR: 2.85, 95% CI: 1.13–7.16, P=0.026) was still revealed with control BP level as the reference group by conditional logistic regression analysis.
SAP death and poor outcome
On the other hand, out of the eight patients with SAP death, three patients showed severe hypertension, three moderate hypertension and two control BP levels. Logistic regression analysis using age, sex, Glasgow Coma Scale score, WBC count, log(serum C-reactive protein), dysphagia and hypertensive state as confounding factors revealed that male sex (OR: 23.0, 95% CI: 1.66–319, P=0.019) and hypertensive state (OR: 5.69, 95% CI: 1.24–26.1, P=0.025) were independently and significantly associated with an increased risk of SAP death. Conditional logistic regression analysis adjusted by the same confounding factors revealed a significant increase in the risk of SAP death in those with severe hypertension on admission, with an adjusted OR estimate of 5.20 and CI 1.01–26.8, with control BP level as the reference group (Table 4). Even when the previous use of antihypertensive medication was added as another confounding factor to the above, hypertensive state was still independently and significantly associated with an increase risk of SAP death (OR: 5.92, 95% CI: 1.25–28.1, P=0.025) by logistic regression analysis, although a tendency for increased risk of SAP death in those with severe hypertension (OR: 6.11, 95% CI: 0.84–44.6, P=0.074) was still revealed with control BP level as the reference group by conditional logistic regression analysis.
Besides the 8 patients with SAP death, 3 patients died from other causes in hospital and 17 patients were receiving artificial feeding at discharge. Logistic regression analysis using the same confounding factors revealed that dysphagia (OR: 65.2, 95% CI: 9.74–437, P<0.001) and hypertensive state (OR: 5.66, 95% CI: 1.32–24.3, P=0.020) were independently and significantly associated with an increased risk of poor outcome associated with in-hospital mortality and artificial feeding at discharge. Conditional logistic regression analysis adjusted by the same confounding factors revealed a significant increase in the risk of poor outcome in those with severe hypertension on admission, with adjusted OR estimate of 6.84 and CI 1.32–35.4, with control BP level as the reference group (Table 5). Even when the previous use of antihypertensive medication was added as another confounding factor to those above, hypertensive state was still independently and significantly associated with an increased risk of poor outcome (OR: 7.43, 95% CI: 1.24–44.6, P=0.028) by logistic regression analysis, and a significant increase in the risk of poor outcome in those with severe hypertension (OR: 9.78, 95% CI: 1.24–77.4, P=0.031) was still revealed with control BP level as the reference group by conditional logistic regression analysis.
Discussion
In this study, we attempted to compare SAP+ patients with SAP− patients in the acute phase of ischemic stroke and obtain evidence of predictors of SAP in elderly patients with a mean age of 84.6 years. Because older age is one of the risk factors for SAP,2, 3, 9, 10, 11 our study was carried out in one of the most susceptible groups for SAP. Besides age, we adopted known risk factors for SAP as possible confounding factors in the present study, such as sex3, 7, 9, 10), Glasgow Coma Scale score,4, 5, 6 dysphagia,7, 8, 9 stroke subtype,8, 9 diabetes,10 ischemic heart disease9 and chronic congestive heart failure.11 We also adopted chronic kidney disease as a factor, because the risk of hospitalization due to pneumonia is also greater in these patients.28 Indeed, univariate analysis revealed that elderly SAP+ patients had a significantly lower mean Glasgow Coma Scale score and a higher incidence of dysphagia, as well as higher WBC count and log(serum C-reactive protein) on admission, compared with SAP− patients.
In the present study, however, the most notable finding was the significant association of severe hypertension, defined as 200/120 mm Hg or higher, on admission with the occurrence of SAP. Univariate analysis revealed that elderly SAP+ patients had significantly higher SBP and pulse pressure on admission compared with SAP− patients (Table 1). There were significant differences in Glasgow Coma Scale score, WBC count and incidence of dysphagia among the three BP groups (Table 2). However, even after adjustment for these known confounding factors, severe hypertension on admission was significantly and independently associated with SAP, with OR 2.83 and CI 1.14–7.05, with control BP level as the reference group (Table 3).
The precise mechanism of this association is not known. SAP is most likely to develop in patients who are seriously ill, and aspiration due to dysphagia may be one of the most important causes of this complication. Hypertension in the elderly is a well-known risk factor for silent cerebral infarction, which is a predictor of not only overt stroke29 but also aspiration pneumonia due to dysphagia.29, 30 On the other hand, known hypertension before stroke was significantly associated with elevated post-stroke BP.15 In the present study, the incidence of both dysphagia and known hypertension under treatment with antihypertensive agents was significantly higher in patients with moderate hypertension on admission compared with normotensive and/or mildly hypertensive controls (Table 2). Although patients with a prior history of dysphagia before the index stroke were excluded in the present study, these observations may indicate that known hypertension would influence subclinical swallowing dysfunction through hypertension-induced brain damage such as silent cerebral infarction before overt ischemic stroke. However, there was no significant difference in the incidence of dysphagia and known hypertension between patients with severe hypertension on admission and patients with control BP. Moreover, conditional logistic regression analysis revealed a significant increase in the risk of SAP in those with severe hypertension compared with control BP patients, even after adjustment for dysphagia (Table 3) and known hypertension under antihypertensive treatment as confounding factors.
Another potential confounder may be drug therapy. ACEI may decrease the prevalence of aspiration pneumonia in elderly subjects, probably due to stimulation of the cough reflex.31, 32 Moreover, several other antihypertensive agents are reported to modify the risk of community-acquired pneumonia.33 In the present study, the rate of antihypertensive treatment prior to ischemic stroke was significantly higher in the moderate hypertension group than in the control group. However, there was no significant difference in the rate of single or combination use of particular antihypertensive agents between the severe hypertensive group and either the control group or moderate hypertensive group. Moreover, there was no significant difference in the rate of single or combined use of particular antihypertensive agents between SAP+ and SAP− patients. These results indicate that the effect(s) of any antihypertensive treatment prior to ischemic stroke on SAP is minimal.
Another possible explanation may be overactivation of the sympathetic nervous system. Acute severe hypertension in the early phase of acute ischemic stroke is related to stroke-induced changes in sympathoadrenergic activity.12, 15, 34 Dysphagia and subsequent aspiration are considered to account for the high incidence of bacterial pneumonia after stroke. However, aspiration alone cannot explain the high incidence of SAP,35 because aspiration occurs in healthy adults during sleep without inducing pneumonia.36 The high incidence of pneumonia in patients with acute ischemic stroke may be due to stroke-induced immunodeficiency primarily caused by overactivation of the sympathetic nervous system, which was described in mouse models of cerebral ischemia.37, 38 In these animal models, experimental stroke propagated bacterial aspiration ranging from harmless intranasal colonization to harmful pneumonia, which was exacerbated by immunodepression due to sympathetic hyperactivity. Moreover, immediately after admission, chest X-ray infiltrate was noted only in 4 normotensive and/or mildly hypertensive control subjects, but not in the 7 subjects with severe hypertension on admission, out of the 38 SAP patients in the present study (data not shown). This evidence may suggest that severe hypertension preceded SAP, at least in the seven patients, in our study. Although we did not determine sympathetic activity including circulating levels of catecolamines in the present study, overactivation of the sympathetic nervous system could induce both severe hypertension and immunodepression, resulting in SAP in our elderly ischemic stroke patients. Further, studies are required to elucidate the precise mechanism of the association of severe hypertension with SAP.
In the present study, severe hypertension on admission was an independent predictor not only of SAP but also of SAP death (Table 4), and of poor outcome associated with in-hospital mortality and artificial feeding at discharge (Table 5). Severe hypertension in the early phase of acute ischemic stroke is a predictor of a poor outcome, with higher mortality and a poor functional outcome.18, 19, 20 Because SAP is an important cause of death1, 3, 4 and a worse long-term clinical outcome,4 the association of severe hypertension with poor outcome would, at least in part, be explained by higher SAP death and poor functional outcome in those with severe hypertension revealed in the present study. However, in view of the small sample size, care must be taken when these results are interpreted and further evaluation in larger trials is needed. Moreover, four patients suffered from SAP already on admission, but remaining 34 patients with SAP were diagnosed as nosocomial, hospital-acquired pneumonia occurring during hospitalization. Microbiological examination of tracheal specimens and/or blood cultures did not detected atypical pathogens, such as Chlamydia pneumoniae, Mycoplasma pneumoniae or Legionella pneumophila (data not shown), suggesting aspiration pneumonia as predominant type in these 38 SAP patients. However, we previously reported association between human metapneumovirus seroprevalence and hypertension in elderly subjects.39 Further, studies including examination of pathogen(s) are also needed to elucidate precise mechanism for the association of severe hypertension and SAP.
References
Henon H, Godefroy O, Leys D, Mounier-Vehier F, Lucas C, Rondepierre P, Duhamel A, Pruvo JP . Early predictors of death and disability after acute cerebral ischemic event. Stroke 1995; 26: 392–398.
Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, Dick F, Taylor GS, Murray G . Medical complications after stroke: a multicenter study. Stroke 2000; 31: 1223–1229.
Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW . The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 2003; 60: 620–625.
Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, Heiss WD . Nosocomial pneumonia after acute stroke: Implication for neurological intensive care medicine. Stroke 2003; 34: 975–981.
Hamidon BB, Raymond AA, Norlinah MI, Jefferelli SB . The predictors of early infection after an acute ischaemic stroke. Singapore Med J 2003; 44: 344–346.
Upadya A, Thorevska N, Sena KN, Manthous C, Amoateng-Adjepong Y . Predictors and consequences of pneumonia in critically ill patients with stroke. J Crit Care 2004; 19: 16–22.
Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S . Formal dysphagia screening protocols prevent pneumonia. Stroke 2005; 36: 1972–1976.
Walter U, Knoblich R, Steinhagen V, Donat M, Benecke R, Kloth A . Predictors of pneumonia in acute stroke patients admitted to a neurological intensive care unit. J Neurol 2007; 254: 1323–1329.
Finlayson O, Kapral M, Hall R, Asllani E, Selchen D, Saposnik G . Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology 2011; 77: 1338–1345.
Aslanyan S, Weir CJ, Diener HC, Kaste M, Lees KR . Pneumonia and urinary tract infection after acute ischaemic stroke: a tertiary analysis of the GAIN International trial. Eur J Neurol 2004; 11: 49–53.
Ovbiagele B, Hills NK, Saver JL, Johnston SC . Frequency and determinants of pneumonia and urinary tract infection during stroke hospitalization. J Stroke Cerebrovasc Dis 2006; 15: 209–213.
Meyer J, Stoica E, Pascu I, Shimazu K, Hartmann A . Catecholamine concentrations in CSF and plasma of patients with cerebral infarction and haemorrhage. Brain 1973; 96: 277–288.
Wallace JD, Levy LL . Blood pressure after stroke. JAMA 1981; 246: 2177–2180.
Morfis L, Schwartz RS, Poulos R, Howes LG . Blood pressure changes in acute cerebral infarction and hemorrhage. Stroke 1997; 28: 1401–1405.
Boreas AM, Lodder J, Kessels F, de Leeuw PW, Troost J . Predictors of poststroke blood pressure level and course. J Stroke Cerebrovasc Dis 2001; 10: 85–91.
Weimar C, Roth MP, Zillessen G, Glahn J, Wimmer ML, Busse O, Haberl RL, Diener HC . Complications following acute ischemic stroke. Eur Neurol 2002; 48: 133–140.
Britton M, Carlsson A, de Faire U . Blood pressure course stroke and matched controls. Stroke 1986; 17: 861–864.
Chamorro A, Vila N, Asasco C, Elices E, Schonewille W, Blanc R . Blood pressure and functional recovery in acute ischemic stroke. Stroke 1998; 29: 1850–1853.
Ahmed N . High initial blood pressure after stroke is associated with poor functional outcome. J Intern Med 2001; 249: 467–473.
Ogata T, Yasaka M, Wakugawa Y, Ibayashi S, Okada Y . Predisposing factors for acute deterioration of minor ischemic stroke. J Neurol Sci 2009; 287: 147–150.
Bath P, Chalmers J, Powers W, Beilin L, Davis S, Lenfant C, Mancia G, Neal B, Whitworth J, Zanchetti A . International Society of Hypertension (ISH): statement on the management of blood pressure in acute stroke. J Hypertens 2003; 21: 665–672.
Vaughan CJ, Delanty N . Hypertensive emergencies. Lancet 2000; 356: 411–417.
Collins MJ, Bakheit AM . Does pulse oximetry reliably detect aspiration in dysphagic stroke patients? Stroke 1997; 28: 1773–1775.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Kang DW, Chalela JA, Ezzeddine MA, Warach S . Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 2003; 60: 1730–1734.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A . Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
Cibcati J, Feinstein AR, Holford TRE . The risk of determining risk with multivariable models. Ann Intern Med 1993; 118: 201–210.
James MT, Quan H, Tonelli M, Manns BJ, Faris P, Laupland KB, Hemmelgarn BR . CKD and risk of hospitalization and death with pneumonia. Am J Kidney Dis 2009; 54: 24–32.
Lim JS, Kwon HM . Risk of ‘silent stroke’ in patients older than 60 years: risk assessment and clinical perspectives. Clin Interv Aging 2010; 5: 239–251.
Nakagawa T, Sekizawa K, Nakajoh K, Tanji H, Arai H, Sasaki H . Silent cerebral infarction: a potential risk for pneumonia in the elderly. J Intern Med 2000; 247: 255–259.
Arai T, Yasuda Y, Toshima S, Yoshimi N, Kashiki Y . ACE inhibitors and pneumonia in elderly people. Lancet 1998; 352: 1937–1938.
Okaishi K, Morimoto S, Fukuo K, Niinobu T, Hata S, Onishi T, Ogihara T . Reduction of risk of pneumonia associated with use of angiotensin I converting enzyme inhibitors in elderly inpatients. Am J Hypertens 1999; 12: 778–783.
Mukamal KJ, Ghimire S, Pandey R, O'Meara ES, Gautam S . Antihypertensive medications and risk of community-acquired pneumonia. J Hypertens 2010; 28: 401–405.
Jansen PAF, Themn TH, Gribnau FWJ, Schulte BP, Willemsen JJ, Lamers KJ, Poels EF . Blood pressure and both venous and urinary cathecholamines after cerebral infarction. Clin Neurol Neurosurg 1988; 90: 41–45.
Perry L, Love CP . Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia 2001; 16: 7–18.
Marik PE . Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001; 344: 665–671.
Prass K, Meisel C, Hoeflich C, Braun J, Halle E, Wolf T, Ruscher K, Victorov IV, Priller J, Dirnagl U, Volk H-D, Meisel A . Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by post-stroke T helper cell type 1-like immunostimulation. J Exp Med 2003; 198: 725–736.
Prass K, Braun JS, Dirnagl U, Meisel C, Meisel A . Stroke propagates bacterial aspiration to pneumonia in a model of cerebral ischemia. Stroke 2006; 37: 2607–2612.
Zeng L, Chen R, Ishigami K, Atsumi M, Koiszumi Y, Sato K, Iritani O, Okuro M, Morimoto S . Association between human metapneumovirus seroprevalence and hypertension in elderly subjects in a long-term care facility. Hypertens Res 2011; 34: 474–478.
Acknowledgements
This work was supported by Research Funding for Longevity Sciences (20A-02) from the National Center for Geriatrics and Gerontology (NCGG) Japan, Comprehensive Research on Aging and Health, the Ministry of Health, Labour and Welfare, and grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Ishigami, K., Okuro, M., Koizumi, Y. et al. Association of severe hypertension with pneumonia in elderly patients with acute ischemic stroke. Hypertens Res 35, 648–653 (2012). https://doi.org/10.1038/hr.2012.7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.7
Keywords
This article is cited by
-
Predictors of post-stroke fever and infections: a systematic review and meta-analysis
BMC Neurology (2018)
-
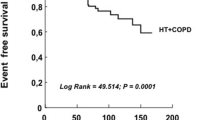
Impact of pneumonia and lung cancer on mortality of women with hypertension
Scientific Reports (2016)