Abstract
In non-diabetic patients with nephrotic syndrome (NS) at early stages of chronic kidney disease, it remains unclear whether the degree of proteinuria affects the nocturnal blood pressure (BP) dip. We evaluated the relationship among circadian BP rhythm, proteinuria and hypoalbuminemia in these patients. We also evaluated the autonomic nervous activity. Twenty-four-hour BP was measured in NS patients (8 men and 13 women; mean age, 58.5±14.8 years) and age- and sex-matched normal subjects (11 men and 13 women; mean age, 54.3±18.2 years) as controls. Serum albumin and urinary protein concentrations were measured. Power spectral analysis of the heart rate was performed, and the high frequency (HF) and low frequency (LF) components were calculated as indices of sympathovagal balance. There were no differences in waking BP between the NS and the control groups (131±13/78±9 vs. 130±17/76±7 mm Hg; P>0.05). However, sleeping BP was significantly higher in the NS group than in the control group (127±18/75±9 vs. 115±14/66±7 mm Hg; P<0.05). Sleeping/waking BP ratios were higher in the NS group than in the control group (P<0.01). In the NS group, these ratios correlated significantly with serum albumin level (r=−0.54, P=0.011 for systolic BP; r=−0.48, P=0.030 for diastolic BP) and urinary protein excretion (r=0.47, P=0.027 for systolic BP; r=0.60, P=0.003 for diastolic BP). Both HF components and LF/HF ratios were not significantly different between the two groups. In non-diabetic NS patients, loss of nocturnal BP reduction correlates with proteinuria and hypoalbuminemia but not with circadian autonomic nervous rhythm.
Similar content being viewed by others
Introduction
In patients with diabetic glomerulopathy, the circadian rhythm of blood pressure (BP) shows a loss of nocturnal BP reduction, which is associated with greater risks of cardiovascular complications such as left ventricular hypertrophy and cerebrovascular disease.1, 2, 3, 4 In the early stage of diabetic nephropathy, impaired diurnal autonomic nervous rhythm is closely associated with urinary albumin excretion, which has an important function in blunted nocturnal decline in BP.5 However, it is still controversial whether albuminuria causes nocturnal hypertension or is a result of it. Recently, microalbuminuria has been regarded as an indicator of organ damage6, 7, 8, 9, 10; however, albuminuria differs in many pathogenetic aspects. Especially, in non-diabetic patients with nephrotic syndrome (NS), a large quantity of urinary protein is excreted even at the early stage of renal impairment. If microalbuminuria is secondary to the loss of nocturnal BP reduction, patients with early stage of glomerulonephritis and albuminuria are supposed to show a loss of nocturnal BP decline. However, there is little evidence on the association among the circadian rhythm of BP, autonomic nervous activity and the variability of the urinary protein excretion. In this study, we evaluated the relationship among the circadian rhythm of BP, urinary protein excretion and diminished serum albumin level secondary to massive proteinuria in non-diabetic patients who showed NS without renal dysfunction, using ambulatory BP monitoring (ABPM) devices. We also analyzed the power spectrum of heart rate variability to evaluate the relations among the autonomic nervous function, ABPM and proteinuria in the same subjects.
Methods
Patients
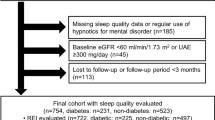
Twenty-one non-diabetic patients (8 men and 13 women; aged 18–76 years; mean age, 58.5±14.8 years), with untreated NS, were enrolled in the study before the beginning of therapy for NS. NS in the early and middle stages of chronic kidney disease (CKD) was diagnosed when patients had serum creatinine levels <1.5 mg per 100 ml, urinary protein excretion >3.5 g day−1, serum albumin <3.0 g per 100 ml, hemoglobin A1C <6.0% and fasting serum glucose <110 mg per 100 ml. Renal biopsy was performed and histologic diagnosis was confirmed in 20 patients, but biopsy was not performed in the remaining 1 patient because of her clinical background. Antihypertensive agents, when administered, were discontinued at least 1 week before the study. Diuretic agents for edema were continued if necessary. Physical and laboratory examinations were performed to exclude patients with endocrinological, hematological or hepatic disease, cerebral infarction or hemorrhage, uncontrolled hypertension, myocardial infarction occurring within 6 months before the study, unstable angina, abnormal thyroid function or other major diseases. Twenty-four age- and sex-matched healthy subjects (11 men and 13 women; aged 19–79 years; mean age, 54.3±18.2 years) were enrolled as controls. These control subjects had no proteinuria, serum creatinine <1.5 mg per 100 ml, serum albumin >3.0 g per 100 ml, hemoglobin A1C <6.0%, fasting serum glucose <110 mg per 100 ml and office BP <140/90 mm Hg. Informed consent for participation in the study was obtained from each subject.
Methods
Ambulatory 24-h BP monitoring was conducted, and urinary and blood samples were collected at approximately the same period to measure 24-h urinary excretion of protein, creatinine and sodium, as well as serum albumin level. Body mass index (BMI) was calculated as weight divided by height squared (kg m−2), and body surface area was calculated according to the DuBois and DuBois formula. In both the groups, estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) Study equation.11 All subjects were instructed to follow a diet containing approximately 6 g of salt per day.
Ambulatory BP monitoring
ABPM was performed using non-invasive multitasking BP recorders (TM2425, A&D, Tokyo, Japan). The device monitors autonomic nervous function simultaneously while measuring BP. BP was recorded at 15-min intervals from 07:00 to 21:00 and 30-min intervals from 21:00 to 07:00. The participants were asked to maintain their usual daily activities during the recording period and to relax their arms during BP measurement. The mean systolic and diastolic BP and mean heart rates were calculated for each participant. The mean BP was calculated as the sum of the diastolic BP and one third of the pulse pressure. Waking and sleeping BPs were obtained as the average values during the waking period and sleeping period, respectively. Then, sleeping/waking BP ratios were analyzed in each subject. The following readings were discarded because of technical artifacts: systolic BP >250 or <70 mm Hg, diastolic BP >130 mm Hg or <30 mm Hg, pulse pressure >160 mm Hg or <20 mm Hg, systolic differences >60 mm Hg, and diastolic differences >30 mm Hg compared with the immediately preceding or successive values. Non-dipper status was defined as a sleeping/waking ratio of mean ambulatory BP >0.9 and dipper status as 0.9 or less.
Spectral analysis of heart rate variability
The method of power spectral analysis using a multitasking recorder has been described in detail elsewhere.12, 13 Briefly, an electrocardiogram was obtained with a precordial lead to analyze the variation in RR interval length. Every 30 min, 512 RR intervals were recorded at a resolution of 7.8 milliseconds and were analyzed after Fast Fourier transformation using appropriate software (A&D). The power spectral densities of the oscillations were divided into two ranges; a low frequency (LF) component in the range of 0.05–0.15 Hz, and a high frequency (HF) component in the range of 0.15–0.4 Hz as an index of parasympathetic nervous activity. The LF/HF ratio was calculated as an index of the sympathovagal balance.
Statistical analysis
All values are expressed as mean±s.d. The differences between the NS group and the control group were analyzed by Student t test for unpaired samples. The differences in sex distribution and prevalence of non-dipper between two groups were examined by χ2 test. The correlation between sleeping/waking BP ratios and urinary protein excretion or serum albumin level was analyzed using Pearson's correlation coefficient. A P value of <0.05 was accepted as statistically significant.
Results
The background characteristics of all subjects participated in the study are summarized in Table 1. No significant differences in age, sex distribution, BMI, serum creatinine concentrations and eGFR were detected between the NS and the control groups. Serum albumin level was significantly lower (P<0.001) in the NS group than in the control group.
Ambulatory BP monitoring
Analysis of the circadian rhythm of BP showed a non-dipper pattern in 16 of 21 patients (76.1%) in the NS group compared with 9 of 24 patients (37.5%) in the control group. The rate of non-dipper status in the NS group was significantly higher (P=0.009) compared with the control group. Twenty-four-hour systolic, diastolic and mean BP were not significantly different between the NS group and the control group (Table 2). There were no significant differences in waking BP between the two groups. However, sleeping systolic, diastolic and mean BP were significantly higher in the NS group than in the control group. Consequently, sleeping/waking ratios of systolic, diastolic and mean BP were significantly higher in the NS group than in the control group. On the other hand, heart rate was significantly higher in the NS group than in the control group during sleep. Furthermore, among patients in the NS group, urinary protein excretion showed a significant positive correlation with sleeping/waking ratios of systolic BP (r=0.47; P=0.027; Figure 1) and diastolic BP (r=0.60; P=0.003; Figure 2). Serum albumin level also showed a significant reverse correlation with sleeping/waking ratios of systolic BP (r=−0.54; P=0.011; Figure 3), and diastolic BP (r=−0.48; P=0.030; Figure 4). Ten patients continued to take the diuretic agent (furosemide, 46.0±36.2 mg day−1), whereas 11 patients were not taking diuretic agents. Thus, NS patients were divided into two subgroups according to whether they were receiving diuretics or not to assess the effect of diuretics on circadian BP rhythm. Consequently, no significant difference in sleeping/waking ratios of mean BP was detected between 10 diuretic-treated patients and 11 diuretic-free patients (0.96±0.06 vs. 0.96±0.10; P=0.986). Similar results were obtained for both systolic (0.96±0.07 vs. 0.97±0.10; P=0.929) and diastolic BP (0.96±0.06 vs. 0.95±0.10; P=0.951).
Spectral analysis of heart rate variability
The power spectral densities of heart rate variability showed no significant differences in 24-h HF component and LF/HF ratio, waking HF component and LF/HF ratio, sleeping HF component and LF/HF ratio, and sleeping/waking ratios of HF component and LF/HF ratio between the NS and the control groups (Table 3).
Discussion
In this study, we evaluated both 24-h urinary protein excretion and the serum albumin level as indicators of the severity of NS. The reason is that urinary protein excretion rate is affected by various factors including the activity of NS, incorrect urine collection and variable daily protein intake. As a result, 24-h urinary protein excretion has greater day-by-day fluctuation than serum albumin level during a short-term study. Our preliminary study showed a significant negative correlation between serum albumin level and urinary protein excretion (r=−0.52; P=0.014), indicating that serum albumin level can be used as a surrogate marker of the severity of NS. This study showed that in non-diabetic patients with NS, the sleeping/waking ratios of systolic, diastolic and mean BP were significantly associated with not only urinary protein excretion but also serum albumin levels even in early and middle stages of CKD. This suggests that the more severe the NS, the more blunted is nocturnal BP reduction.
Some earlier studies in patients with non-diabetic CKD have shown that as renal function deteriorates, the nocturnal decline in BP is blunted further.14, 15, 16 However, there are very few reports on the circadian rhythm of BP during the early stage of CKD with non-diabetic NS characterized by massive proteinuria, hypoalbuminemia and edema.17 Barenbrock et al.18 showed that in non-diabetic nephrotic patients with normal serum creatinine levels, the day–night difference in BP was not different from that in the controls, suggesting that albuminuria was not related to the loss of nocturnal decline of BP. Their results contradicted with our findings. The precise reason for this discrepancy is not known, although the differences in sample size and study design probably caused the conflicting results.
Although the mechanisms responsible for nocturnal BP fall to maintain the circadian BP rhythm are not fully understood, it is well known that the withdrawal of the sympathetic nervous activity during sleeping period seems to play a crucial role in dipping mechanisms.19, 20 Patients with diabetic nephropathy show impaired circadian BP rhythm even at the early stage of CKD. Impaired autonomic nervous system is considered to induce the disturbed circadian BP rhythm.5, 21 In this study on non-diabetic patients with early and middle stages of CKD, 24-h HF components, their sleeping/waking ratios and the 24-h rhythm of LF/HF ratios did not differ significantly from those in the control group, indicating that the circadian autonomic nervous activity of these patients was not different from that in the control group. This implies that the non-dipper phenomenon recognized in NS is probably unrelated to sympathetic nervous dysfunction. However, the finding that the NS group had higher heart rate during sleep than the control group still suggests that the imbalance of the sympathovagal rhythm may play a role in the loss of nocturnal BP fall although the autonomic nervous function may not be the major cause.
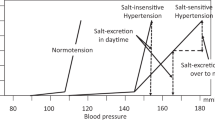
In the nephrotic state, hypoalbuminemia causes anasarca, a characteristic sign of NS. Classically, edema formation in NS was considered to be secondary to shifting of sodium and fluid from intravascular circulation to extravascular space caused by low plasma oncotic pressure.22, 23, 24 Meanwhile, in experimental animals, Chandra et al.25 and Ichikawa et al.26 showed that unilateral renal puromycin aminonucleoside infusion induced proteinuria and sodium retention in the ipsilateral kidney, whereas the contralateral non-treated kidney had normal sodium handling, suggesting that sodium retention occurs in the proteinuric kidney. This also indicates that sodium retention is not dependent on systemic factors or hypoalbuminemia, but on the nephron segments of the nephrotic kidney.27, 28, 29, 30 In clinical studies on patients with essential hypertension, Kimura and co-workers31, 32 showed that sodium retention and high sodium sensitivity cause the loss of nocturnal BP reduction, and further showed that sodium restriction and diuretics normalized BP rhythm from non-dipper to dipper patterns.33, 34 These observations suggest that when natriuresis is impaired during daytime, nocturnal BP are elevated to enhance pressure natriuresis during the night as a compensation for the diminished natriuresis during the day.32, 35
In this study, as there was no significant difference in eGFR or waking time BP between two groups, it is unlikely that the glomerular filtration capability of sodium in the NS group was more diminished than that in the control group. Meanwhile, urinary sodium excretion in patients with NS was low when they underwent ABPM. We assume that sodium retention is likely to be related to the loss of nocturnal BP reduction, and this may result in pressure natriuresis during the night. Unfortunately, we did not have the data of sodium and albumin excretion rates in fractional urine samples collected over 24 h, and consequently cannot reach a conclusion.
Our study included some patient receiving furosemide to reduce edema. However, there was little effect of diuretics on circadian BP rhythm or clinical signs. This suggests that the dosage of furosemide might not have been enough to exert its effects on renal tubules or circadian BP rhythm. Thus, there still remains a possibility that high sodium sensitivity to BP regulation and pressure natriuresis seen in essential hypertension may cause loss of nocturnal BP fall in NS.
Conclusion
In patients with non-diabetic NS in the early and middle stages of CKD, massive proteinuria causes a high proportion of non-dippers, and the sleeping/waking ratios of BP correlate significantly with urinary protein excretion and serum albumin level. To confirm the genesis for loss of the circadian rhythm of BP and evaluate the mechanisms by which proteinuria causes loss of nocturnal BP reduction, further studies are required in a large number of nephrotic patients with similar pathophysiological findings.
Conflict of interest
The authors declare no conflict of interest.
References
Covic A, Goldsmith DJA, Georgrescu GC, Ackrill P . Relationships between blood pressure variability and left ventricular parameters in haemodialysis and renal transplant patients. Nephrology 1998; 4: 87–93.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Watanabe N, Minami N, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Satoh H, Hisamichi S . Relation between nocturnal decline in blood pressure and mortality. Am J Hypertens 1997; 10: 1201–1207.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y . Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 2002; 20: 2183–2189.
Timio M, Venanzi S, Lolli S, Lippi G, Verdura C, Monarca C, Guerrini E . Non-dipper hypertensive patients and progressive renal insufficiency: a 3-year longitudinal study. Clin Nephrol 1995; 43: 382–387.
Inaba M, Negishi K, Takahashi M, Serizawa N, Maruno Y, Takahashi K, Katayama S . Increased night:day blood pressure ratio in microalbuminuric normotensive NIDDM subjects. Diabetes Res Clin PR 1998; 40: 161–166.
Bianchi S, Bigazzi R, Baldari G, Sgherri G, Campese VM . Diurnal variations of blood pressure and microalbuminuria in essential hypertension. Am J Hypertens 1994; 7: 23–29.
Gerber LM, Schwartz JE, Pickering TG . Albumin-to-creatinine ratio predicts change in ambulatory blood pressure in normotensive persons: a 7.5-year prospective study. Am J Hypertens 2006; 19: 220–226.
Lieb W, Mayer B, Stritzke J, Doering A, Hense HW, Loewel H, Erdmann J, Schunkert H . Association of low-grade urinary albumin excretion with left ventricular hypertrophy in the general population. Nephrol Dial Transplant 2006; 21: 2780–2787.
Yudkin JS, Forrest RD, Jackson CA . Microalbuminuria as predictor of vascular disease in non-diabetic subjects. Lancet 1988; 2: 530–533.
Jager A, Kostense PJ, Ruhe HG, Heine RJ, Nijpels G, Dekker JM, Bouter LM, Stehouwer CDA . Microalbuminuria and peripheral arterial disease are independent predictors of cardiovascular and all-cause mortality, especially among hypertensive subjects. Arterioscler Thromb Vasc Biol 1999; 19: 617–624.
Imai E, Horio M, Nitta K, Yamagata K, Iseki K, Hara S, Ura N, Kiyohara Y, Hirakata H, Watanabe T, Moriyama T, Ando Y, Inaguma D, Narita I, Iso H, Wakai K, Yasuda Y, Tsukamoto Y, Ito S, Makino H, Hishida A, Matsuo S . Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol 2007; 11: 41–50.
Bernardi L, Ricordi L, Lazzari P, Solda P, Calciati A, Ferrari MR, Vandea I, Finardi G, Fratino P . Impaired circadian modulation of sympathovagal activity in diabetes. Circulation 1992; 86: 1443–1452.
Pierdomenico SD, Bucci A, Costantini F, Lapenna D, Cuccurullo F, Mezzetti A . Twenty-four-hour autonomic nervous function in sustained and ‘white coat’ hypertension. Am Heart J 2000; 140: 672–677.
Portaluppi F, Montanari L, Massari M, Chiara VD, Capanna M . Loss of nocturnal decline of blood pressure in hypertension due to chronic renal failure. Am J Hypertens 1991; 4: 20–26.
Timio M, Lolli S, Verdura C, Monarca C, Merante F, Guerrini E . Circadian blood pressure changes inpatients with chronic renal insufficiency: a prospective study. Ren Fail 1993; 15: 231–237.
Middeke M, Schrader J . Nocturnal blood pressure in normotensive subjects and those with white coat, and secondary hypertension. Br Med J 1994; 308: 630–632.
Koopman MG, Koomen GCM, Van Acker BAC, Arisz L . Urinary sodium excretion in patients with nephrotic syndrome, and its circadian variation. Q J Med 1994; 87: 109–117.
Barenbrock M, Spieker C, Hausberg M, Rahn KH, Zidek W, Kisters K . Studies on diurnal blood pressure variation in kidney diseases associated with excessive salt and water retention. J Hum Hypertens 1999; 13: 269–273.
Kohara K, Nishida W, Maguchi M, Hiwada K . Autonomic nervous function in non-dipper essential hypertensive subjects. Evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808–814.
Rizzo V, Campbell SV, Maio FD, Tallarico D, Lorido A, Petretto F, Bianchi A, Carmenini G . Spectral analysis of heart rate variability in elderly non-dipper hypertensive patients. J Hum Hypertens 1999; 13: 393–398.
Farmer CKT, Goldsmith DJA, Quin JD, Dallyn P, Cox J, Kingswood JC, Sharpstone P . Progression of diabetic nephropathy—is diurnal blood pressure rhythm as important as absolute blood pressure level? Nephrol Dial Transplant 1998; 13: 635–639.
Hamm LL, Batuman V . Edema in the nephrotic syndrome: new aspect of an old enigma. J Am Soc Nephrol 2003; 14: 3288–3289.
Deschenes G, Feraille E, Doucet A . Mechanisms of oedema in nephrotic syndrome: old theories and new ideas. Nephrol Dial Transplant 2003; 18: 454–456.
Wolff HP, Bette L, Blaise H, Dusterdieck G, Jahnecke J, Kobayashi T, Kruck F, Lommer D, Schieffer H . Role of aldosterone in edema formation. Ann N Y Acad Sci 1966; 139: 285–294.
Chandra M, Hoyer JR, Lewy JE . Renal function in rats with unilateral proteinuria produced by renal perfusion with aminonucleoside. Pediatr Res 1981; 15: 340–344.
Ichikawa I, Rennke HG, Hoyer JR, Badr KF, Schor N, Troy JL, Lechene CP, Brenner BM . Role for intrarenal mechanisms in the impaired salt excretion of experimental nephrotic syndrome. J Clin Invest 1983; 71: 91–103.
Deschenes G, Wittner M, Di Stefano A, Jounier S, Doucet A . Collecting duct is a site of sodium retention in PAN nephrosis: a rationale for amiloride therapy. J Am Soc Nephrol 2001; 12: 598–601.
Feraille E, Vogt B, Rousselot M, Barlet-Bas C, Cheval L, Doucet A, Favre H . Mechanism of enhanced Na-K-ATPase activity in cortical collecting duct from rats with nephrotic syndrome. J Clin Invest 1993; 91: 1295–1300.
Valentin JP, Ying WZ, Sechi LA, Ling KT, Qiu C, Couser WG, Humphreys MH . Phosphodiesterase inhibitors correct resistance to natriuretic peptides in rats with Heymann nephritis. J Am Soc Nephrol 1996; 7: 582–593.
Rodriguez-Iturbe B, Herrera-Acosta J, Johnson RJ . Interstitial inflammation, sodium retention, and the pathogenesis of nephrotic edema: a unifying hypothesis. Kidney Int 2002; 62: 1379–1384.
Uzu T, Frida KS, Ishikawa K, Nakamura S, Inenaga T, Kimura G . High sodium sensitivity implicates nocturnal hypertension in essential hypertension. Hypertension 1996; 28: 139–142.
Fujii T, Uzu T, Nishimura M, Takeji M, Kuroda S, Nakamura S, Inenaga T, Kimura G . Circadian rhythm of natriuresis is disturbed in non-dipper type of essential hypertension. Am J Kidney Dis 1999; 33: 29–35.
Uzu T, Ichikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G . Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1997; 96: 1859–1862.
Uzu T, Kimura G . Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1999; 100: 1635–1638.
Fukuda M, Munemura M, Usami T, Nakao N, Takeuchi O, Kamiya Y, Yoshida A, Kimura G . Nocturnal blood pressure is elevated with natriuresis and proteinuria as renal function deteriorates in nephropathy. Kidney Int 2004; 65: 621–625.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andoh, D., Kobayashi, M., Yasuda, G. et al. Loss of nocturnal decline of blood pressure in non-diabetic patients with nephrotic syndrome in the early and middle stages of chronic kidney disease. Hypertens Res 32, 364–368 (2009). https://doi.org/10.1038/hr.2009.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.21
Keywords
This article is cited by
-
High frequency of nocturnal hypertension in lupus nephritis: should ABPM be implemented in usual practice?
Clinical Rheumatology (2020)
-
Preclinical cardiovascular abnormalities in patients in early stages of renal disease without nephrotic syndrome
Hypertension Research (2009)