Abstract
To test the hypothesis that a mobilization of endothelial progenitor cells (EPCs) occurs after acute cerebrovascular diseases, we evaluated the number of EPCs in the process of acute stroke. A total of 203 individuals were examined, including 100 patients with ischemic strokes, 36 patients with hemorrhagic strokes and 67 healthy controls. Ninety-eight patients were observed at days 1, 7, 14 and 28 after acute stroke. Circulating EPCs were defined by the surface markers CD133/KDR and analyzed by flow cytometry. Serum high sensitivity C-reactive protein (hs-CRP) concentrations were determined by particle-enhanced immunonephelometry using the N high sensitivity CRP Reagent. Patients with acute stroke had lower numbers of EPCs (0.037±0.001/100 peripheral blood mononuclear cells (PMNCs) vs. 0.06±0.002/100 PMNCs, P<0.05) and higher levels of serum hs-CRP (1.99 vs. 0.03 mg per 100 ml, P<0.05) than control subjects after adjusting for age, sex, body mass index (BMI) and blood pressure. There were no differences in EPCs counts or serum hs-CRP levels between patients with ischemic and hemorrhagic stroke. In univariate analyses, BMI, age, systolic blood pressure (SBP), diastolic blood pressure, low-density lipoprotein (LDL), total cholesterol (T-cho), blood glucose and hs-CRP (P<0.001) were inversely correlated with EPCs counts. Multivariate analyses showed SBP and total cholesterol as independent predictors of EPCs levels. The number of EPCs gradually increased at day 7 after acute onset, remained elevated at day 14; and returned to baseline by day 28. Our results suggest a possible contribution of circulating EPCs in acute stroke. SBP and total cholesterol are independent factors of reduced EPCs numbers. A transient early increment of EPCs may result from the mobilization of EPCs in response to stroke stress.
Similar content being viewed by others
Introduction
Endothelial progenitor cells (EPCs) play a critical role in the pathophysiology of different forms of cardiovascular diseases, including hypertension, coronary artery disease, chronic heart failure, peripheral artery diseases, diabetes and chronic renal failure. However, as the structural and functional integrity of the endothelial monolayer becomes detached after vascular injury, turnover and repair of endothelial cells are thought to be maintained at a low basal replication rate. EPCs from peripheral blood were first isolated and characterized in 1997.1 Further studies suggested that peripheral blood-derived EPCs had the potential to differentiate into endothelial cells and to contribute to vascular repair and neovascularization after ischemic tissue injury.2, 3 At the same time, clinical studies demonstrated that patients with cardiovascular risk factors and one of several cardiovascular diseases had a low level of circulating EPCs.4, 5 Acute coronary syndromes and acute myocardial infarction are correlated with elevated numbers of EPCs, indicating that EPCs could mobilize in response to vascular trauma or tissue ischemia.6 Therefore, it may be speculated that conventional risk factors not only participate in endothelial injury but also play a role in the impairment of EPCs, thereby advancing the process of atherosclerosis.
Stroke, a growing pandemic, is a major cause of mortality and disability worldwide. Coronary and cerebrovascular diseases, which share the majority of the causal etiologies that result in endothelial cell damage and arteriosclerosis, comprise the arterial obstructive syndromes. Although EPCs have been extensively studied as a surrogate marker of vascular function, few data are available regarding the relationship of EPCs with cerebrovascular diseases. EPCs have also been shown to promote neovascularization in the ischemic brain after experimentally induced stroke.7
Thus, the severity and pathogenesis of cerebrovascular diseases can be estimated by measuring circulating numbers of EPCs. Precise measurement of circulating EPCs provides a marker for cerebrovascular function in the setting of stress. The established method of quantifying circulating EPCs is by flow cytometry, using antibodies against CD133 and KDR.8
In this study, we evaluated the number of EPCs during the process of acute stroke to test our hypothesis that the mobilization of EPCs occurs after acute cerebrovascular stroke and is associated with recovery of the repair process.
Methods
Study subjects
All studies were IRB approved and patients gave informed consent. All patients who suffered a stroke between October 2004 and March 2006 and visited the Emergency Department of Ruijin Hospital Shanghai were enrolled in an ongoing prospective registry that included clinical attributes and blood samples. A total of 136 patients with clinically suspected acute ischemic or hemorrhagic stroke confirmed with CT or MRI scan after admission were included. The following individuals were excluded from the study to reduce potentially confusing influences on EPCs or high sensitivity C-reactive protein (hs-CRP): pre-menstrual women, patients who had received a blood transfusion or surgery, patients with bleeding, inflammation, ulcer, trauma, operation, malignant tumors, peripheral vascular diseases, acute coronary syndrome, myocardial infarction, proliferative retinopathy within 2 months, or recurrent acute stroke within 3 months. None of the patients included in the study had been treated with statins or erythropoietin in the preceding 2 months. Thirty patients were excluded and eight patients died during follow-up; therefore, data from a total of 98 patients were analyzed. Sixty-seven age- and gender-matched healthy volunteers were also studied. The experimental protocol was approved by the ethics committee of Shanghai Jiaotong University and informed consent was given by patients or their relatives.
Clinical variables
All patients were admitted to the acute stroke unit and underwent general supportive care and treatment of acute complications in accordance with the Guidelines of the Cerebrovascular Diseases, by the same stroke team.9, 10 The patients’ characteristics were obtained from medical records with regard to the history of hypertension, hypercholesterolemia, diabetes, alcohol consumption and smoking. Participants underwent physical examination and blood tests to assess cerebrovascular risk factors including age, gender, BMI, blood pressure, blood glucose and total serum cholesterol.
Neurological assessment
Evaluation of physical function and neurological impairment of the stroke patients was based on the Chinese Stroke Scale11 and the Modified Barthel Score at days 1, 7, 14 and 28 after the onset of stroke.12
Determination of the volume of an intracerebral hemorrhage or intracerebral ischemia
The gold standard for approximating the volume of an intracerebral hemorrhage or intracerebral ischemia is direct volumetric measurement with imaging software using CT scanner. The formula is V=4/3π(A/2)(B/2)(C/2). For π=3, the formula becomes V=ABC/2, where A, B and C are the three diameters.13, 14, 15 Subsequently, the window level and width were chosen so as to obtain the best contrast between the lesion and the normal surrounding tissue; each volume was calculated three times and the mean value was taken as definitive. All neuroimaging evaluations were made by a neuroradiologist who was blinded to the patients’ clinical and laboratory results.
Laboratory assessment
In addition to a full clinical assessment, ancillary examinations at days 1 and 14 after stroke were performed, including a complete blood count, hepatic and renal function tests, blood glucose, total serum cholesterol, uric acid, electrocardiogram, brain CT scan and brain MRI, if necessary.
Determination of the serum concentrations of high sensitivity C-reactive protein
To determine the serum hs-CRP concentration, peripheral blood was quantified once (interval 6±2 h) at 06:00 hours on days 1, 7, 14 and 28 after the onset of stroke. Serum concentrations of hs-CRP were determined by particle-enhanced immunonephelometry using N high sensitivity CRP reagent (Dade Behring, Inc., Marburg, Germany).
Assessment of circulating EPCs level by flow cytometry
To determine the number of EPCs, peripheral blood was quantified once (interval 6±2 h) at 0600 hours on days 1, and 7, 14 and 28 after the onset of stroke. One hundred fifty microliters of whole blood treated with heparin as an anticoagulant was incubated for 30 min in the dark with APC-labeled monoclonal antibody against human KDR (R&D, Minneapolis, MN, USA) and monoclonal antibody against human CD133 (MACS, Bergisch Gladbach, Germany). Isotype-identical antibodies IgG1-PE and IgG1-APC (Becton Dickinson, Franklin Lakes, NJ, USA) served as the controls. The analysis was performed using a FACSCalibur flow cytometer with CellQuest software (BD Pharmingen, San Diego, CA, USA). The viable lymphocyte population was analyzed and each analysis included 60 000 events. KDR was determined by flow kilometric analysis using laser excitation of 620–650 nm and emitted fluorescence was monitored with a detector optimized to collect peak emissions at 660–670 nm. CD133 was determined using 488/575 nm excitation/emission wavelengths. All assessments were performed by an investigator who was blinded to the patients’ clinical and laboratory results.
Statistical Analysis
SPSS software was used for data analysis. Results were expressed as means±s.d. The independent samples T test was used to compare the mean values of variables clinical characteristic of two groups, whereas χ2 was used to compare proportions. We used a logarithmic transformation of hs-CRP to meet the demands of a normal frequency distribution, with a 95% confidence interval for the mean. The comparison of EPCs and hs-CRP levels between stroke patients and healthy controls was carried out using univariate analysis. The interaction between the number of EPCs and various risk factors, as well as the volume of an intracerebral hemorrhage or ischemia, was examined by bivariate correlation. Multivariate stepwise regression analysis was used to test the relationship between various risk factors and the number of EPCs. One-way ANOVA was used to compare the mean values of the dynamic change in EPCs number. P<0.05 indicated statistical significance.
Results
Clinical characteristics of the study subjects
The 67 healthy controls had a mean age of 68 years and comprised almost equal numbers of males (49%) and females (51%). A total of 136 patients with acute stroke were enrolled; 76 (56%) were male. Patients presented with the following: 100 with acute ischemic stroke, 36 with hemorrhagic stroke with a history of hypertension (average 13 years), 16 with alcohol consumption, 21 cases with smoking, 26 cases with diabetes, 21 cases with coronary heart disease and 42 cases with hypertensive cardiopathy. The baseline characteristics of all 203 subjects are summarized in Table 1. As expected, the stroke patients displayed significantly higher risk factors; BMI, blood pressure, glucose, total cholesterol, low-density lipoprotein cholesterol and triglyceride were all higher in stroke patients than in controls (P<0.05).
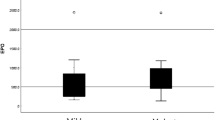
Comparison of circulating EPCs and hs-CRP levels between stroke patients and healthy controls
Univariate analyses, adjusted for age, gender, BMI and blood pressure, were performed to compare the number of circulating EPCs and hs-CRP. The control subjects had significantly higher levels of EPCs and lower levels of hs-CRP compared with stroke patients (P<0.05, Table 2). We further analyzed EPCs and CRP levels between cases of hemorrhagic and ischemic stroke. We found that the number of EPCs was lower in both hemorrhagic and ischemic stroke patients compared with controls, but no significant difference was found between the hemorrhagic and ischemic stroke groups.
No significant difference in the hs-CRP count was noted between hemorrhagic and ischemic stroke groups (Table 2).
Correlation between cerebrovascular risk factors and EPCs
Using bivariate analysis for the entire cohort, the classic risk factors of age, BMI, blood pressure, heart rate, blood glucose, total cholesterol, low-density lipoprotein and hs-CRP were shown to be inversely correlated with the number of circulating EPCs (Table 3). However, multivariate analysis revealed that systolic blood pressure (SBP), total cholesterol, triglyceride and age remained significant independent predictors of a reduced number of EPCs (P<0.05, Table 4). Discriminate function coefficients indicated that BMI, hypertension history, SBP, total cholesterol, EPCs and hs-CRP are multivariate predictors of the presence of stroke (Table 5).
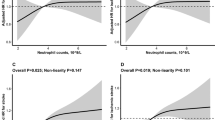
The dynamic change in circulating EPCs in patients with stroke
To investigate whether the number of EPCs would change after stroke, we observed the changes in circulating EPCs levels during the course of stroke progression by detecting the number of EPCs every week for 4 weeks. Interestingly, we found a transient increment of EPCs on day 7 following stroke, and subsequently the number of EPCs was slowly reduced through day 28 (Figure 1).
Relationships between the number of EPCs and modified stroke scale on days 1, 7, 14 and 28 after acute stroke
There was no statistical difference in the number of EPCs among stroke patients when using either the Chinese Stroke scale or the Barthel Score on days 1, 7, 14 or 28 after acute stroke (data not shown). The relationship between the patients’ levels of EPCs and the volume of an intracerebral hemorrhage or ischemia is shown in Table 6.
Discussion
This study of the number of circulating EPCs in patients after acute stroke produced several clinically striking results. In our study, we used a simple and precise method to quantify the number of circulating EPCs during the process of acute stroke and evaluate the relationship of this number to several risk factors. We demonstrated that the level of circulating EPCs was significantly lower in patients with acute stroke than in control subjects; in particular, the number of circulating EPCs changed following a time course after the occurrence of stroke. Multivariate analyses revealed that SBP and total cholesterol are independent predictors of EPCs levels.
Our previous study suggested that the number of circulating EPCs was significantly reduced in patients with coronary artery disease compared with control subjects.16 In this study, we showed that the number of circulating EPCs was lower in patients with cerebrovascular disease 24 hours after acute stroke than in control subjects. Our findings are consistent with previous reports and further support the idea that the number of EPCs is usually decreased in patients with cerebrovascular disease.17
Our study is the first to show that the levels of circulating EPCs are correlated with cerebral hemorrhage in a clinical setting, although more compelling evidence indicates that EPCs numbers are decreased in patients with cerebral infarction.17 Interestingly, despite the different pathogenesis of cerebral hemorrhage and infarction, there were no differences in EPCs counts between patients experiencing ischemic or hemorrhagic stroke. Recent studies provide evidence that the number of EPCs is a surrogate marker of vascular injury because it decreases in subjects with cardiovascular risks, such as hypercholesterolemia, hypertension and diabetes.4, 5 The same result was observed with serum hs-CRP, which has been suggested as an inflammatory parameter in patients with a cerebrovascular attack.18, 19, 20
Because EPCs mobilization from bone marrow may occur following acute stroke, we hypothesized that the number of EPCs would change during the course of stroke. We therefore monitored circulating EPCs levels during the course of stroke progression. Interestingly, we found that the number of EPCs gradually increased through day 7 after acute onset, remained significantly higher until day 14 and returned to baseline by day 28. Although an earlier study that included only a small group of patients had findings similar to the present study,21 the authors did not investigate the dynamic change in circulating EPCs in patients with hemorrhagic stroke. Therefore, our findings are the first to suggest that EPCs are mobilized to the peripheral blood in response to vascular trauma and may enhance the repair of damaged vessels.2, 3
Another important finding of this study was that the classic cerebrovascular risk factors of BMI, age, blood pressure, blood glucose, total cholesterol, low-density lipoprotein and hs-CRP were inversely correlated with the number of circulating EPCs. Particularly, a significant correlation between the hs-CRP concentration and the number of EPCs in stroke patients has not been reported in a clinical study; this lack of correlation suggests that inflammation may potentially correlate with the level of EPCs. An in vitro experiment showed that CRP significantly reduced the number of EPC cells.22 Inhibition of the expression of endothelial cell-specific markers significantly increases EPCs apoptosis and impairs EPC-induced angiogenesis.22 Furthermore, multiple logistic regression analysis showed that SBP and total cholesterol were independent predictors of EPC number. The mechanisms by which risk factors reduce EPC numbers remain to be determined. Many risk factors, including hypertension and hypercholesterolemia, could impair the functional integrity of the endothelial monolayer, which could lead to an eventual depletion or exhaustion of a presumed finite supply of EPCs.23, 24
Although the present study did not document the level of circulating EPCs as an independent predictor of future stroke, we found that many risk factors, especially EPCs taken together with SBP, BMI, hypertension history, total cholesterol and hs-CRP, are multivariate predictors as revealed by discriminate function coefficients suggest the possibility of a stroke. Thus, monitoring the level of circulating EPCs may be particularly useful for identifying the presence of ongoing risk factor-induced endothelial injury.
The reduction of EPCs following stroke may be secondary to a variety of mechanisms.25, 26 Potential impairments in EPCs production and mobilization and continuous exhaustion of circulating EPCs in stroke patients warrant further investigation. The impact of the level of circulating EPCs on clinical outcomes after stroke is uncertain. We did not find a prognostic effect of EPCs, either through the effect of EPCs increment on neurological outcome or the infarct volume, although a greater increase in circulating EPCs was seen during the first week. This increase in circulating EPCs is independently associated with a better clinical outcome in acute ischemic stroke patients.27 Another study found that a low level of circulating EPCs at 48 h after ischemic stroke was strongly and independently predictive of severe neurological impairment.28 However, we did not find such a correlation of circulating EPCs with the Chinese Stroke scale or the Barthel Score. Possible reasons for these discrepancies may include differences in the study subjects and the surface markers of EPCs used. In this study, patients with potential influences on the number of EPCs or hs-CRP were excluded.29, 30, 31 Furthermore, EPCs identified as CD133/KDR double-positive cells are more likely to reflect immature progenitor cells. The mechanisms by which risk factors reduce the number of circulating EPCs remain to be elucidated. Some of these factors were associated with a smaller increase of EPCs during the study, so we cannot completely rule out a confounding effect of these related variables. No correlation was noted between the number of circulating EPCs and the volume of an intracerebral hemorrhage or ischemia. This may be caused by multiple risk factors and cell types contributing to the progression of vascular lesions in major arteries.
One limitation of the present study was the short observation time (28 days following stroke) of the participants. Moreover, we did not test the functional activity of the EPCs, which may not result in sufficient information to fully evaluate the effects of acute cerebrovascular disease on circulating EPCs. Whether circulating EPCs are able to incorporate into brain ischemic areas and promote regenerative angiogenesis and neurogenesis in humans requires further study. A larger cohort with cerebrovascular diseases could establish a prognostic value of EPCs in stroke patients and better inform therapy.
References
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM . Isolation of putative progenitor endothelial cells for angiogenesis. Science 1997; 275: 964–967.
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, Kearne M, Magner M, Isner JM . Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 1999; 85: 221–228.
Orlic D, Kajstura J, Chimenti S, Limana F, Jakoniuk I, Quaini F, Nadal-Ginard B, Bodine DM, Leri A, Anversa P . Mobilized bone marrow cells repair the infarcted heart, improving function and survival. Proc Natl Acad Sci USA 2001; 98: 10344–10349.
Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T . Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med 2003; 348: 593–600.
Vasa M, Fichtlscherer S, Aicher A, Adler K, Urbich C, Martin H, Zeiher AM, Dimmeler S . Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res 2001; 89: E1–E7.
Shintani S, Murohara T, Ikeda H, Ueno T, Honma T, Katoh A, Sasaki K, Shimada T, Oike Y, Imaizumi T . Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation 2001; 103: 2776–2779.
Beck H, Voswinckel R, Wagner S, Ziegelhoeffer T, Heil M, Helisch A, Schaper W, Acker T, Hatzopoulos AK, Plate KH . Participation of bone marrow-derived cells in long-term repair processes after experimental stroke. J Cereb Blood Flow Metab 2003; 23: 709–717.
Fan CL, Li Y, Gao PJ, Liu JJ, Zhang XJ, Zhu DL . Differentiation of endothelial progenitor cells from human umbilical cord blood CD 34+ cells in vitro. Acta Pharmacol Sin 2003; 24: 212–228.
Adams Jr HP, Adams RJ, Brott T, del Zoppo GJ, Furlan A, Goldstein LB, Grubb RL, Higashida R, Kidwell C, Kwiatkowski TG, Marler JR, Hademenos GJ, Stroke Council of the American Stroke Association. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke 2003; 34: 1056–1083.
Broderick JP, Adams Jr HP, Barsan W, Feinberg W, Feldmann E, Grotta J, Kase C, Krieger D, Mayberg M, Tilley B, Zabramski JM, Zuccarello M . Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 1999; 30: 905–915.
Park J, Hopwood V, White AR, Ernst E . Effectiveness of acupuncture for stroke: a systematic review. J Neurol 2001; 248: 558–563.
Shah S, Vanclay F, Cooper B . Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 1989; 42: 703–709.
Clatterbuck RE, Sipos EP . The efficient calculation of neurosurgically relevant volumes from computed tomographic scans using Cavalieri′s Direct Estimator. Neurosurgery 1997; 40: 339–342.
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J . The ABCs of measuring intracerebral hemorrhage volumes. Stroke 1996; 27: 1304–1305.
Stocchetti N, Croci M, Spagnoli D, Gilardoni F, Resta F, Colombo A . Mass volume measurement in severe head injury: accuracy and feasibility of two pragmatic methods. J Neurol Neurosurg Psychiatry 2000; 68: 14–17.
Wang HY, Gao PJ, Ji KD, Shen WF, Fan CL, Lu L, Zhu DL . Circulating Endothelial Progenitor Cells, C-Reactive Protein and Severity of Coronary Stenosis in Chinese Patients with Coronary Artery Disease. Hypertens Res 2007; 30: 133–141.
Ghani U, Shuaib A, Salam A, Nasir A, Shuaib U, Jeerakathil T, Sher F, O′Rourke F, Nasser AM, Schwindt B, Todd K . Endothelial progenitor cells during cerebrovascular disease. Stroke 2005; 36: 151–153.
Blake GJ, Rifai N, Buring JE . Blood pressure, C-reactive protein, and risk of future cardiovascular events. Circulation 2003; 108: 2993–2999.
Ridker PM, CH, Buring JE Rifai N . C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 2000; 342: 836–843.
Pinto A, Tuttolomondo A, Di Raimaondo D, Fernandez P, Licata G . Cerebrovascular risk factors and clinical classification of strokes. Semin Vasc Med 2004; 4: 287–303.
Taguchi A, Matsuyama T, Moriwaki H, Hayashi T, Hayashida K, Nagatsuka K, Todo K, Mori K, Stern DM, Soma T, Naritomi H . Circulating CD34-positive cells provide an index of cerebrovascular function. Circulation 2004; 109: 2972–2975.
Verma S, Kuliszewski MA, Li SH, Szmitko PE, Zucco L, Wang CH, Badiwala MV, Mickle DA, Weisel RD, Fedak PW, Stewart DJ, Kutryk MJ . C-reactive protein attenuates endothelial progenitor cell survival, differentiation, and function: further evidence of a mechanistic link between C-reactive protein and cardiovascular disease. Circulation 2004; 109: 2058–2067.
Umemura T, Soga J, Hidaka T, Takemoto H, Nakamura S, Jitsuiki D, Nishioka K, Goto C, Teragawa H, Yoshizumi M, Chayama K, Higashi Y . Aging and hypertension are independent risk for induced number of circulating endothelial progenitor cells. Am J Hypentens 2008; 21: 1203–1209.
Chen JZ, Zhang FR, Tao QM, Wang XX, Zhu JH, Zhu JH . Number and activity of endothelial progenitor cells from peripheral blood in patients with hypercholesterolemia. Clin Sci 2004; 107: 273–280.
Lapergue B, Mohammad A, Shuaib A . Endothelial progenitor cells and cerebrovascular diseases. Prog Neurobiol 2007; 83: 349–362.
Hristov M, Erl W, Weber PC . Endothelial progenitor cells: mobilization, differentiation, and homing. Arterioscler Thromb Vasc Biol 2003; 23: 1185–1189.
Sobrino T, Hurtado O, Moro MA, Rodríguez-Yáñez M, Castellanos M, Brea D, Moldes O, Blanco M, Arenillas JF, Leira R, Dávalos A, Lizasoain I, Castillo J . The increase of circulating endothelial progenitor cells after acute ischemic stroke is associated with good outcome. Stroke 2007; 38: 2759–2764.
Yip HK, Chang LT, Chang WN, Lu CH, Liou CW, Lan MY, Liu JS, Youssef AA, Chang HW . Level and value of circulating endothelial progenitor cells in patients after acute ischemic stroke. Stroke 2008; 39: 69–74.
Yao EH, Fukuda N, Matsumoto T, Kobayashi N, Katakawa M, Yamamoto C, Tsunemi A, Suzuki R, Ueno T, Matsumoto K . Losartan improves the impaired function of endothelial progenitor cells in hypertension via an antioxidant effect. Hypertens Res 2007; 30: 1119–1128.
Ando H, Nakanishi K, Shibata M, Hasegawa K, Yao K, Miyaji H . Benidipine, a dihydropyridine-Ca2+ channel blocker, increases the endothelial differentiation of endothelial progenitor cells in vitro. Hypertens Res 2006; 29: 1047–1054.
Imanishi T, Kobayashi K, Hano T, Nishio I . Effect of estrogen on differentiation and senescence in endothelial progenitor cells derived from bone marrow in spontaneously hypertensive rats. Hypertens Res 2005; 28: 763–772.
Acknowledgements
This work was supported by the National Key Project for Basic Research (2004CB518603, 2006CB503804, 2009CB521905), the National High-tech R&D Program (2006AA02Z179) and a grant from the Shanghai Science and Technology Committee (08JC1417400, 08DZ2200400, 08410702400).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, Wj., Zhu, Dl., Yang, Gy. et al. Circulating endothelial progenitor cells in Chinese patients with acute stroke. Hypertens Res 32, 306–310 (2009). https://doi.org/10.1038/hr.2009.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.16
Keywords
This article is cited by
-
Evaluation of Endothelial Progenitor Cell Characteristics as Clinical Biomarkers for Elderly Patients with Ischaemic Stroke
Stem Cell Reviews and Reports (2023)
-
Role of Stromal Cell-Derived Factor-1 in Endothelial Progenitor Cell-Mediated Vascular Repair and Regeneration
Tissue Engineering and Regenerative Medicine (2021)
-
Mobilization of endothelial progenitor cell in patients with acute ischemic stroke
Neurological Sciences (2018)
-
Endothelial progenitor cells in ischemic stroke: an exploration from hypothesis to therapy
Journal of Hematology & Oncology (2015)