Abstract
Mucopolysaccharidosis I (MPS I) is a rare autosomal recessive multisystem lysosomal storage disorder. It is caused by biallelic loss-of-function variants in IDUA, encoding alpha-l iduronidase. Here, we describe an individual affected by MPS I due to a paternally inherited deletion of IDUA exons 1 and 2, c.(?_-88)_(299+1_300-1)del and a whole-gene deletion of IDUA (?_-88?)_(*136?)del secondary to maternal somatic mosaicism. We define a previously unreported mutational mechanism for this disorder.
Similar content being viewed by others
Mucopolysaccharidosis type I (MPS I) is a rare, recessively inherited lysosomal storage disorder resulting from a deficiency of the enzyme alpha-l iduronidase (IDUA; EX 3.2.1.76) secondary to biallelic loss-of-function variants in the gene IDUA (MIM #252800).1 Deficiency of the enzyme results in accumulation of glycosaminoglycans in tissues, which leads to a constellation of progressive clinical features. Affected individuals typically present with clinical manifestations in the first year of life, including facial dysmorphism, hepatosplenomegaly, upper airway obstruction, skeletal deformity, corneal clouding and cardiomyopathy.2 Historically, three subtypes of MPS I: Hurler Syndrome (MIM #607014), Hurler-Scheie syndrome (MIM #607015) and Scheie syndrome (MIM #607016) have been described based on clinical severity. The biochemical defects are indistinguishable and the three subtypes represent a continuum of disease, such that MPS I is increasingly described as either severe or attenuated. In its most severe form, MPS I results in a reduced life span if untreated, with death usually occurring in the first 10 years of life. Current recommended treatment for MPS I is early hematopoietic stem cell transplantation.3,4
MPS I is genetically homogeneous with biallelic variants in IDUA accounting for all molecularly characterised cases.5,6 Over 200 pathogenic variants in IDUA have been reported7 with most being private.8 The spectrum includes missense, nonsense, splice site, small deletions and insertions, with nonsense variants being the most commonly reported.9 Although phenotypic correlation with enzyme levels has been inconsistent, patients with nonsense variants on both alleles have the most severe subtype of MPS I.9 Individuals with missense variants can have residual enzyme activity associated with less severe disease, and genotype is used as part of a suggested algorithm for predicting MPS I phenotype.10
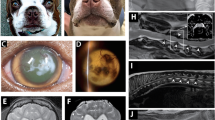
The second child of non-consanguineous parents was born at term after a normal pregnancy, with a birth weight of 3 kg (9-25th centile). An umbilical hernia was noted at birth and a newborn screen determined bilateral sensorineural hearing loss. She presented at 8 months of age due to mild motor delay, nasal congestion, recurrent ear infections and a gibbus deformity. On examination, there were coarse facial features, hepatomegaly 3 cm below the costal margin, a large sacral mongolian blue spot, mild corneal clouding and a thoracic gibbus deformity. The hands appeared normal. Urine testing showed an increase in dermatan and chondroitin sulphates by 2D electrophoresis of extracted glycosaminoglycans with an increased total glycosaminoglycan level of 232 mg/mmol creatinine (normal for age <35). Dermatan sulphate/chondroitin sulphate ratio was 2.3 (normal 0). The clinical diagnosis of severe MPS I was confirmed by leucocyte enzyme testing with a low iduronidase activity of 0.01 umol/g/hr (normal range 10–50 umol/g/hr). Normal enzyme levels of 32.29 μmol/g/hr were measured in the mother, with levels of 19.00 μmol/g/hr, consistent with carrier status in the father. Following biochemical diagnosis, enzyme replacement therapy with alpha-L-iduronidase was initiated followed by a matched sibling donor hematopoietic stem cell transplant, which was completed with no complications. At 3 years, echocardiogram shows moderate mitral valve incompetence and right ventricular hypertrophy. Developmentally, there has been progress, with independent walking and improved speech. Genetic testing was undertaken to confirm the clinical and biochemical diagnosis, and to provide information for reproductive decision making.
Sanger sequencing of the 14 exons of IDUA (primers available on request) was undertaken on a sample of lymphocytic DNA from the proband. Amplification of exons 1 and 2 was unsuccessful, indicating a possible homozygous deletion encompassing these exons. No putative pathogenic variants were detected. Sequencing all IDUA exons in lymphocyte DNA from each parent did not reveal any putative pathogenic variant. However, a number of common IDUA sequence variants were identified (Figures 1a–c). Of note, the father was heterozygous for a number of variants through exons 3 to 12 of IDUA, which were apparently monoallelic in the affected daughter’s sample. This data indicated that the proband had inherited at least one allele from the father. The father was apparently homozygous for three variants in exons 1. Hemizygosity for these variants would be consistent with a heterozygous exonic deletion.
Known single nucleotide polymorphisms (SNPs) identified upon sequencing of IDUA in father, affected daughter and mother. (a) Not-to-scale scheme of IDUA with exons numbered, and the exonic/intronic positions of 22 relevant SNP (dbSNP build 144) indicated. (b) Pedigree. (c) Apparent haplotypes based on the SNPs in (a) (grey boxes indicate failure to amplify the corresponding genomic fragment from the patient’s DNA). Note that the apparently homozygous haplotype of the daughter corresponds to the father‘s haplotype 2 from intron 2 onwards, and that none of the mother‘s haplotypes is found in the daughter.
Sequence analysis of IDUA from a lymphocyte sample from the mother identified five heterozygous variants, none of which were present in the affected daughter (Figures 1a–c). Heterozygosity for the three variants in exon 1 did not provide evidence of a heterozygous deletion encompassing exon 1 in the mother.
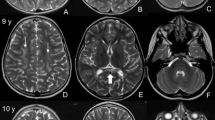
The Sanger sequencing results of IDUA suggested alternative genetic mechanisms underlying the clinical and biochemical diagnosis: (i) uniparental disomy (UPD) of a paternal allele containing an exon 1 and 2 deletion or (ii) inheritance of a paternal allele containing an exon 1 and 2 deletion and a de novo deletion of the maternal allele. To establish the presence of copy number variation, custom-designed multiplex ligation-dependent probe amplification (MLPA) of IDUA (Figure 2a) was undertaken in the affected child. Absence of both copies of exons 1 and 2 and loss of one copy of the remaining 12 exons of IDUA was established (Figure 2b). MLPA determined that the father was heterozygous for a deletion of IDUA exons 1 and 2 c.(?_-88)_(299+1_300-1)del, NM_000203.3 whereas initial MLPA of the mother’s sample did not detect any copy number variation. This initial result indicated de novo somatic deletion of the whole maternal allele in the proband, i.e., a scenario associated with a low recurrence risk.
IDUA copy number screening and evidence for maternal mosaicism. (a) To scale scheme of the IDUA genomic region with introns and extragenic sequence represented by horizontal lines, and IDUA exons by boxes (narrow: untranslated region, wide: coding sequence). Arrows denote targets of MLPA probes; the star marks the position of the rs3832289 indel polymorphism in intron 4. bp, base pairs; ex, exon; prom, promoter; 3’reg, 3’region. (b) MLPA findings for all family members and for three controls. MLPA signals of ~1.0 indicate normal diploid copy number, while signals of ~0.5 and 0.0 suggest the presence of heterozygous and homozygous absence of target sequence, respectively. (c) PCR of a genomic region containing the 20 bp indel SNP rs3832289 in two heterozygous carriers. (d) Quantification of the two IDUA alleles based on relative intensities of the two PCR products in individuals heterozygous for rs3832289 (compare c).
However, repeated MLPA analysis on lymphocyte extracted DNA suggested an alternative mechanism, in which the mother was a somatic mosaic for a whole gene deletion of IDUA c.[=/ (?_-88?)_(*136?)del (Figure 2c). The mosaic whole gene deletion was supported by dosage analysis of a common intron 4 deletion variant rs3832289 (minor allele frequency 0.14) by quantification of the PCR products in the heterozygous mother versus in seven heterozygous controls (Figure 2d).
Subsequent testing of the proband’s clinically unaffected brother revealed that he is a carrier for the paternal deletion of exons 1 and 2 of IDUA.
We describe a novel mechanism underlying a diagnosis of MPS I. Exonic or whole-gene deletions of IDUA have not been reported previously.2 Likewise, this is the first report of a somatic mosaic disease-causing variant in IDUA. The combination of these events leading to a diagnosis of MPS I in a single family is unprecedented.
Somatic mosaicism for exonic deletions has been described in many other conditions, including neurofibromatosis type I11 and spinal muscular atrophy.12 In some conditions, for example, Duchenne muscular dystrophy, the presence of maternal mosaicism for deletions has been long recognised as a mechanism of recurrence, and is an important consideration for counselling when genetic testing has not provided evidence that the causative deletion is maternally inherited.13 Increasingly, somatic mosaicism in unaffected parents is being recognized as the mechanism of disease occurring in offspring,14,15 and identification is predicted to become more frequent as whole-genome sequencing and copy number analysis of targeted panels and exome data are being implemented in routine clinical practice.14 These technologies have greater sensitivity than previously available approaches to detect mosaicism.
This case demonstrates the value of comprehensive genetic testing to clarify the recurrence risk, which in the context of the initial molecular results was considered low, but was revised to be potentially up to 25%.
References
References
Scott HS, Guo XH, Hopwood JJ, Morris CP . Structure and sequence of the human alpha-L-iduronidase gene. Genomics 1992; 13: 1311–1313.
Clarke LA . Mucopolysaccharidosis Type I in: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH et al. (eds). GeneReviews [Internet]. University of Washington, Seattle: Seattle, WA, USA, 1993-2016.
Wraith JE . The first 5 years of clinical experience with laronidase enzyme replacement therapy for mucopolysaccharidosis I. Expert Opin Pharmacother 2005; 6: 489–506.
Kakkis ED, Muenzer J, Tiller GE, Waber L, Belmont J, Passage M et al. Enzyme-replacement therapy in mucopolysaccharidosis I. N Engl J Med 2001; 344: 182–188.
Beesley CE, Meaney CA, Greenland G, Adams V, Vellodi A, Young EP et al. Mutational analysis of 85 mucopolysaccharidosis type I families: frequency of known mutations, identification of 17 novel mutations and in vitro expression of missense mutations. Hum Genet 2001; 109: 503–511.
Li P, Wood T, Thompson JN . Diversity of mutations and distribution of single nucleotide polymorphic alleles in the human alpha-L-iduronidase (IDUA) gene. Genet Med 2002; 4: 420–426.
Wraith JE, Jones S . Mucopolysaccharidosis type I. Pediatr Endocrinol Rev 2014; 12 (Suppl 1): 102–106.
Bertola F, Filocamo M, Casati G, Mort M, Rosano C, Tylki-Szymanska A et al. IDUA mutational profiling of a cohort of 102 European patients with mucopolysaccharidosis type I: identification and characterization of 35 novel α-L-iduronidase (IDUA) alleles. Hum Mutat 2011; 32: E2189–E2210.
Terlato NJ, Cox GF . Can mucopolysaccharidosis type I disease severity be predicted based on a patient’s genotype? A comprehensive review of the literature. Genet. Med 2003; 5: 286–294.
Kingma SD, Langereis EJ, de Klerk CM, Zoetekouw L, Wagemans T, IJlst L et al. An algorithm to predict phenotypic severity in mucopolysaccharidosis type I in the first month of life. Orphanet J. Rare Dis 2013; 8: 99.
Irene Bottillo IT . Germline mosaicism in neurofibromatosis type 1 due to a paternally derived multi-exon deletion. Am J Med Genet A 2010; 152A: 1467–1473.
Eggermann T, Zerres K, Anhuf D, Kotzot D, Fauth C, Rudnik-Schöneborn S et al. Somatic mosaicism for a heterozygous deletion of the survival motor neuron (SMN1) gene. Eur J Hum Genet 2005; 13: 309–313.
Bakker E, Veenema H, Den Dunnen JT, van Broeckhoven C, Grootscholten PM, Bonten EJ et al. Germinal mosaicism increases the recurrence risk for ‘new’ duchenne muscular dystrophy mutations. J Med Genet 1989; 26: 553–559.
Pham J, Shaw C, Pursley A, Hixson P, Sampath S, Roney E et al. Somatic mosaicism detected by exon-targeted, high-resolution aCGH in 10,362 consecutive cases. Eur J Hum Genet 2014; 22: 969–978.
Campbell IM, Yuan B, Robberecht C, Pfundt R, Szafranski P, McEntagart ME et al. Parental somatic mosaicism is underrecognized and influences recurrence risk of genomic disorders. Am J Hum Genet 2014; 95: 173–182.
Data Citations
Newman, William G HGV Database (2016) http://dx.doi.org/10.6084/m9.figshare.hgv.876
Newman, William G HGV Database (2016) http://dx.doi.org/10.6084/m9.figshare.hgv.879
Acknowledgements
We thank the family for their support with this study and Dr Andrew Wallace for clarification of nomenclature. The nucleotide sequence data reported are available in the GenBank databases under the accession number(s) #00072212 (variants #0000115927, #0000117527).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Breen, C., Mercer, J., Jones, S. et al. Maternal mosaicism for IDUA deletion clarifies recurrence risk in MPS I. Hum Genome Var 3, 16031 (2016). https://doi.org/10.1038/hgv.2016.31
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/hgv.2016.31