Abstract
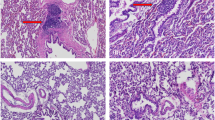
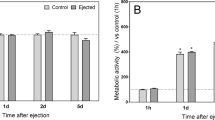
The genetic modification of freshly aspirated bone marrow may provide convenient tools to enhance the regenerative capacities of cartilage defects compared with the complex manipulation of isolated progenitor cells. In the present study, we examined the ability and safety of recombinant adeno-associated virus (rAAV) serotype 2 vectors to deliver various reporter gene sequences in primary human bone marrow aspirates over time without altering the chondrogenic processes in the samples. The results demonstrate that successful rAAV-mediated gene transfer and expression of the lacZ and red fluorescent protein marker genes were achieved in transduced aspirates at very high efficiencies (90–94%) and over extended periods of time (up to 125 days) upon treatment with hirudin, an alternative anticoagulant that does not prevent the adsorption of the rAAV-2 particles at the surface of their targets compared with heparin. Application of rAAV was safe, displaying neither cytotoxic nor detrimental effects on the cellular and proliferative activities or on the chondrogenic processes in the aspirates especially using an optimal dose of 0.5 mg ml−1 hirudin, and application of the potent SOX9 transcription factor even enhanced these processes while counteracting hypertrophic differentiation. The current findings demonstrate the clinical value of this class of vector to durably and safely modify bone marrow aspirates as a means to further develop convenient therapeutic approaches to improve the healing of cartilage defects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
O'Driscoll SW . The healing and regeneration of articular cartilage. J Bone Joint Surg Am 1998; 80: 1795–1812.
Minas T . The role of cartilage repair techniques, including chondrocyte transplantation, in focal chondral knee damage. Instr Course Lect 1999; 48: 629–643.
Jackson DW, Simon TM, Aberman HM . Symptomatic articular cartilage degeneration: the impact in the new millennium. Clin Orthop Relat Res 2001; (391 Suppl): S14–S25.
Cucchiarini M, Madry H . Gene therapy for cartilage defects. J Gene Med 2005; 7: 1495–1509.
Cucchiarini M, Venkatesan JK, Ekici M, Schmitt G, Madry H . Human mesenchymal stem cells overexpressing therapeutic genes: from basic science to clinical applications for articular cartilage repair. Biomed Mater Eng 2012; 22: 197–208.
Madry H, Cucchiarini M . Clinical potential and challenges of using genetically modified cells for articular cartilage repair. Croat Med J 2011; 52: 245–261.
Orth P, Rey-Rico A, Venkatesan JK, Madry H, Cucchiarini M . Current perspectives in stem cell research for knee cartilage repair. Stem Cells Cloning 2014; 7: 1–17.
Madry H, van Dijk CN, Mueller-Gerbl M . The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 2010; 18: 419–433.
Shapiro F, Koide S, Glimcher MJ . Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am 1993; 75: 532–553.
Breinan HA, Martin SD, Hsu HP, Spector M . Healing of canine articular cartilage defects treated with microfracture, a type-II collagen matrix, or cultured autologous chondrocytes. J Orthop Res 2000; 18: 781–789.
Frisbie DD, Oxford JT, Southwood L, Trotter GW, Rodkey WG, Steadman JR et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res 2003; (407): 215–227.
Buckwalter JA . Articular cartilage: injuries and potential for healing. J Orthop Sports Phys Ther 1998; 28: 192–202.
Evans CH . Advances in regenerative orthopedics. Mayo Clin Proc 2013; 88: 1323–1339.
Madry H, Cucchiarini M . Advances and challenges in gene-based approaches for osteoarthritis. J Gene Med 2013; 15: 343–355.
Kim JD, Lee GW, Jung GH, Kim CK, Kim T, Park JH et al. Clinical outcome of autologous bone marrow aspirates concentrate (BMAC) injection in degenerative arthritis of the knee. Eur J Orthop Surg Traumatol 2014; e-pub ahead of print 8 January 2014; doi: 10.1007/s00590-013-1393-9.
Ivkovic A, Pascher A, Hudetz D, Maticic D, Jelic M, Dickinson S et al. Articular cartilage repair by genetically modified bone marrow aspirate in sheep. Gene Therapy 2010; 17: 779–789.
Pascher A, Palmer GD, Steinert A, Oligino T, Gouze E, Gouze JN et al. Gene delivery to cartilage defects using coagulated bone marrow aspirate. Gene Therapy 2004; 11: 133–141.
Cucchiarini M, Madry H, Ma C, Thurn T, Zurakowski D, Menger MD et al. Improved tissue repair in articular cartilage defects in vivo by rAAV-mediated overexpression of human fibroblast growth factor 2. Mol Ther 2005; 12: 229–238.
Cucchiarini M, Ekici M, Schetting S, Kohn D, Madry H . Metabolic activities and chondrogenic differentiation of human mesenchymal stem cells following recombinant adeno-associated virus-mediated gene transfer and overexpression of fibroblast growth factor 2. Tissue Eng Part A 2011; 17: 1921–1933.
Pagnotto MR, Wang Z, Karpie JC, Ferretti M, Xiao X, Chu CR . Adeno-associated viral gene transfer of transforming growth factor-beta1 to human mesenchymal stem cells improves cartilage repair. Gene Therapy 2007; 14: 804–813.
Stender S, Murphy M, O'Brien T, Stengaard C, Ulrich-Vinther M, Soballe K et al. Adeno-associated viral vector transduction of human mesenchymal stem cells. Eur Cell Mater 2007; 13: 93–99.
Venkatesan JK, Ekici M, Madry H, Schmitt G, Kohn D, Cucchiarini M . SOX9 gene transfer via safe, stable, replication-defective recombinant adeno-associated virus vectors as a novel, powerful tool to enhance the chondrogenic potential of human mesenchymal stem cells. Stem Cell Res Ther 2012; 3: 22–36.
Berns KI, Linden RM . The cryptic life style of adeno-associated virus. Bioessays 1995; 17: 237–245.
Hacker UT, Gerner FM, Buning H, Hutter M, Reichenspurner H, Stangl M et al. Standard heparin, low molecular weight heparin, low molecular weight heparinoid, and recombinant hirudin differ in their ability to inhibit transduction by recombinant adeno-associated virus type 2 vectors. Gene Therapy 2001; 8: 966–968.
Schuettrumpf J, Zou J, Zhang Y, Schlachterman A, Liu YL, Edmonson S et al. The inhibitory effects of anticoagulation on in vivo gene transfer by adeno-associated viral or adenoviral vectors. Mol Ther 2006; 13: 88–97.
Summerford C, Samulski RJ . Membrane-associated heparan sulfate proteoglycan is a receptor for adeno-associated virus type 2 virions. J Virol 1998; 72: 1438–1445.
Tschudi M, Lammle B, Alberio L . Dosing lepirudin in patients with heparin-induced thrombocytopenia and normal or impaired renal function: a single-center experience with 68 patients. Blood 2009; 113: 2402–2409.
Cucchiarini M, Orth P, Madry H . Direct rAAV SOX9 administration for durable articular cartilage repair with delayed terminal differentiation and hypertrophy in vivo. J Mol Med (Berl) 2013; 91: 625–636.
Kube DM, Ponnazhagan S, Srivastava A . Encapsidation of adeno-associated virus type 2 Rep proteins in wild-type and recombinant progeny virions: Rep-mediated growth inhibition of primary human cells. J Virol 1997; 71: 7361–7371.
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L . Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 1994; 331: 889–895.
Haleem AM, Singergy AA, Sabry D, Atta HM, Rashed LA, Chu CR et al. The clinical use of human culture-expanded autologous bone marrow mesenchymal stem cells transplanted on platelet-rich fibrin glue in the treatment of articular cartilage defects: a pilot study and preliminary results. Cartilage 2010; 1: 253–261.
Nejadnik H, Hui JH, Feng Choong EP, Tai BC, Lee EH . Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. Am J Sports Med 2010; 38: 1110–1116.
Wakitani S, Nawata M, Tensho K, Okabe T, Machida H, Ohgushi H . Repair of articular cartilage defects in the patello-femoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. J Tissue Eng Regen Med 2007; 1: 74–79.
Colter DC, Piera-Velazquez S, Hawkins DF, Whitecavage MK, Jimenez SA, Stokes DG . Regulation of the human Sox9 promoter by the CCAAT-binding factor. Matrix Biol 2005; 24: 185–197.
Goldring MB, Fukuo K, Birkhead JR, Dudek E, Sandell LJ . Transcriptional suppression by interleukin-1 and interferon-gamma of type II collagen gene expression in human chondrocytes. J Cell Biochem 1994; 54: 85–99.
Haleem-Smith H, Derfoul A, Okafor C, Tuli R, Olsen D, Hall DJ et al. Optimization of high-efficiency transfection of adult human mesenchymal stem cells in vitro. Mol Biotechnol 2005; 30: 9–20.
Posey KL, Davies S, Bales ES, Haynes R, Sandell LJ, Hecht JT . In vivo human cartilage oligomeric matrix protein (COMP) promoter activity. Matrix Biol 2005; 24: 539–549.
Ikeda T, Kamekura S, Mabuchi A, Kou I, Seki S, Takato T et al. The combination of SOX5, SOX6, and SOX9 (the SOX trio) provides signals sufficient for induction of permanent cartilage. Arthritis Rheum 2004; 50: 3561–3573.
Kupcsik L, Stoddart MJ, Li Z, Benneker LM, Alini M . Improving chondrogenesis: potential and limitations of SOX9 gene transfer and mechanical stimulation for cartilage tissue engineering. Tissue Eng Part A 2010; 16: 1845–1855.
Guo X, Zheng Q, Yang S, Shao Z, Yuan Q, Pan Z et al. Repair of full-thickness articular cartilage defects by cultured mesenchymal stem cells transfected with the transforming growth factor beta1 gene. Biomed Mater 2006; 1: 206–215.
Evans CH, Liu FJ, Glatt V, Hoyland JA, Kirker-Head C, Walsh A et al. Use of genetically modified muscle and fat grafts to repair defects in bone and cartilage. Eur Cell Mater 2009; 18: 96–111.
Jiang Y, Chen LK, Zhu DC, Zhang GR, Guo C, Qi YY et al. The inductive effect of bone morphogenetic protein-4 on chondral-lineage differentiation and in situ cartilage repair. Tissue Eng Part A 2010; 16: 1621–1632.
Kuroda R, Usas A, Kubo S, Corsi K, Peng H, Rose T et al. Cartilage repair using bone morphogenetic protein 4 and muscle-derived stem cells. Arthritis Rheum 2006; 54: 433–442.
Mason JM, Breitbart AS, Barcia M, Porti D, Pergolizzi RG, Grande DA . Cartilage and bone regeneration using gene-enhanced tissue engineering. Clin Orthop Relat Res 2000; (379 Suppl): S171–S178.
Vogt S, Wexel G, Tischer T, Schillinger U, Ueblacker P, Wagner B et al. The influence of the stable expression of BMP2 in fibrin clots on the remodelling and repair of osteochondral defects. Biomaterials 2009; 30: 2385–2392.
Goodrich LR, Hidaka C, Robbins PD, Evans CH, Nixon AJ . Genetic modification of chondrocytes with insulin-like growth factor-1 enhances cartilage healing in an equine model. J Bone Joint Surg Br 2007; 89: 672–685.
Madry H, Kaul G, Cucchiarini M, Stein U, Zurakowski D, Remberger K et al. Enhanced repair of articular cartilage defects in vivo by transplanted chondrocytes overexpressing insulin-like growth factor I (IGF-I). Gene Therapy 2005; 12: 1171–1179.
Nixon AJ, Fortier LA, Williams J, Mohammed H . Enhanced repair of extensive articular defects by insulin-like growth factor-I-laden fibrin composites. J Orthop Res 1999; 17: 475–487.
Katayama R, Wakitani S, Tsumaki N, Morita Y, Matsushita I, Gejo R et al. Repair of articular cartilage defects in rabbits using CDMP1 gene-transfected autologous mesenchymal cells derived from bone marrow. Rheumatology (Oxford) 2004; 43: 980–985.
Liu TM, Guo XM, Tan HS, Hui JH, Lim B, Lee EH . Zinc-finger protein 145, acting as an upstream regulator of SOX9, improves the differentiation potential of human mesenchymal stem cells for cartilage regeneration and repair. Arthritis Rheum 2011; 63: 2711–2720.
Cucchiarini M, Terwilliger EF, Kohn D, Madry H . Remodelling of human osteoarthritic cartilage by FGF-2, alone or combined with Sox9 via rAAV gene transfer. J Cell Mol Med 2009; 13: 2476–2488.
Samulski RJ, Chang LS, Shenk T . A recombinant plasmid from which an infectious adeno-associated virus genome can be excised in vitro and its use to study viral replication. J Virol 1987; 61: 3096–3101.
Samulski RJ, Chang LS, Shenk T . Helper-free stocks of recombinant adeno-associated viruses: normal integration does not require viral gene expression. J Virol 1989; 63: 3822–3828.
Venkatesan JK, Rey-Rico A, Schmitt G, Wezel A, Madry H, Cucchiarini M . rAAV-mediated overexpression of TGF-beta stably restructures human osteoarthritic articular cartilage in situ. J Transl Med 2013; 11: 211–224.
Elsler S, Schetting S, Schmitt G, Kohn D, Madry H, Cucchiarini M . Effective, safe nonviral gene transfer to preserve the chondrogenic differentiation potential of human mesenchymal stem cells. J Gene Med 2012; 14: 501–511.
Acknowledgements
The authors thank RJ Samulski (The Gene Therapy Center, University of North Carolina, Chapel Hill, NC, USA) and X Xiao (The Gene Therapy Center, University of Pittsburgh, Pittsburgh, PA, USA) for providing genomic AAV-2 plasmid clones and the 293 cell line. This work was supported by grants from The German Research Society (DFG) and The AO Foundation, Davos, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rey-Rico, A., Frisch, J., Venkatesan, J. et al. Determination of effective rAAV-mediated gene transfer conditions to support chondrogenic differentiation processes in human primary bone marrow aspirates. Gene Ther 22, 50–57 (2015). https://doi.org/10.1038/gt.2014.90
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2014.90