Abstract
Purpose: Up to 16% of patients with the hereditary von Hippel-Lindau disease develop endolymphatic sac tumors of the inner ear. Early diagnosis and treatment of endolymphatic sac tumors can prevent audiovestibular morbidity, but optimal endolymphatic sac tumor surveillance strategy has yet to be determined. We aimed to evaluate endolymphatic sac tumor surveillance to determine the best surveillance strategy.
Methods: In a national prospective study, 40 VHL mutation carriers were interviewed about audiovestibular symptoms and had audiological examinations and magnetic resonance imaging of the inner ear. Further, we performed a meta-analysis including all reported endolymphatic sac tumor von Hippel-Lindau disease cases in the literature (N = 140 with 156 endolymphatic sac tumors).
Results: In the prospective study, endolymphatic sac tumors were suspected based on audiovestibular symptoms, audiometry, and magnetic resonance imaging in 34%, 30%, and 12.5% of subjects, respectively. In total, more than 90% of radiologically diagnosed endolymphatic sac tumors were associated with abnormal audiometric findings. No endolymphatic sac tumor genotype-phenotype correlations were found.
Conclusion: We recommend annual audiometry as a first-line endolymphatic sac tumor screening tool, and in countries where periodic surveillance magnetic resonance imaging of the central nervous system is performed, specific images of the inner ear should be included. Audiometric abnormalities in patients with von Hippel-Lindau disease without magnetic resonance imaging-visible endolymphatic sac tumors could be due to microscopic endolymphatic sac tumors. Determination of audiometric endolymphatic sac tumor characteristics could further target screening and improve endolymphatic sac tumor diagnosis.
Similar content being viewed by others
Main
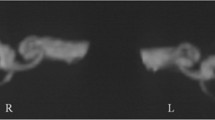
Endolymphatic sac tumors (ELSTs) are locally aggressive tumors of the petrous bone (Fig. 1), which can lead to severe and irreversible hearing loss and other audiovestibular and neurologic symptoms.1 ELSTs rarely occur in the general population but have been found in up to 16% of patients with the hereditary multisystemic von Hippel-Lindau disease (vHL) (OMIM#: 193300).1,2 vHL is caused by inactivation of the tumor suppressor gene VHL, and affected individuals are especially predisposed to development of hemangioblastomas in the central nervous system and retina, renal clear cell carcinoma, renal and pancreatic cysts, and pheochromocytomas. vHL manifestations can lead to severe disability and mortality, which can to some degree be prevented by prophylactic surveillance and early manifestation treatment.3 Prevention of particularly audiovestibular morbidity due to ELSTs is crucial for vHL patients, who are also at risk of blindness and balance impairment due to retinal and cerebellar hemangioblastomas. Early diagnosis of ELSTs is essential because surgical excision of tumors can preserve the preoperative hearing level and eliminate most other audiovestibular symptoms.1,2,4–8
Although the association between ELST and vHL was first established by Manski et al.1 in 1997 and several case reports have been published,4–38 only a few studies have included more than four vHL patients with an ELST.1,2,39,40 To date, there is no evidence as to what is the optimal strategy for ELST surveillance in vHL patients, and no uniform international guidelines exist. Magnetic resonance imaging (MRI) of the inner ear is considered the gold standard in ELST diagnosis and is typically required in surgical planning.1,4,7,12,39 Many institutions perform regular surveillance MRI of the central nervous system in vHL patients, but unfortunately, MRI is expensive and is not easily accessible at regular intervals all over the world. Cheaper methods such as interviews about subjective audiovestibular symptoms or audiological examinations have been proposed as first-line screening tools to identify high-risk patients who should have a diagnostic MRI.1,28,41
Genotype-phenotype correlations have given rise to a subclassification of vHL into vHL type 1 without pheochromocytoma, predominately caused by mutations truncating the protein product of VHL, and vHL type 2 with pheochromocytoma, mainly caused by missense mutations.3 It has been hypothesized that correlations between ELSTs and certain genotypes can be used to identify high-risk families for ELST development and target screening, but previous studies have been too small to demonstrate such a correlation.1,2,34,37
The overall objective of this study was to evaluate ELST surveillance and determine a practical first-line screening approach based on a prospective national study of VHL mutation carriers and a meta-analysis of all published cases and cohorts of vHL patients with ELST.
MATERIALS AND METHODS
The prospective study
In this national study, we initially included 41 VHL mutation carriers older than 15 years: 21 females and 20 males from 19 unrelated vHL families, comprising 90% of all known living adult Danish VHL mutation carriers. Subjects and their clinical features have previously been described.42 All subjects were systematically referred to (1) interview about ELST-related symptoms, (2) audiological examination, and (3) MRI of the inner ear. In cases where an ELST was detected on MRI, all available earlier MRIs of the brain and inner ear were retrospectively assessed to identify first signs of the ELST. One patient died during the study period and was excluded. Of the 40 remaining subjects, 36 underwent both the interview, MRI of the inner ear, and the audiological examination. Three subjects did not have an audiological examination and two did not complete an interview due to worsening of other vHL manifestations (3/4) and of unknown cause (1/4). Median age at the first study examination was 39 years (range: 15–65 years), and median interval between audiological examination and MRI was 2 months (range: 1–18 months).
Interview about subjective audiovestibular symptoms
Subjects were interviewed about subjective symptoms of hearing loss, tinnitus, aural fullness, ear pain, dizziness, and balance disturbances. Reported audiovestibular symptoms that clearly could be attributed to irrelevant causes (e.g., ear trauma, brain surgery, and noise exposure) were disregarded.
Audiological examination
The audiological examinations comprised otoscopy, pure tone audiometry (air and bone conduction thresholds), tympanometry, and determination of stapedial reflex thresholds. Speech reception thresholds and discrimination loss were determined by the standardized speech material “Dantale.”43
MRI of the inner ear
The majority of MRIs of the inner ear (31/40) were carried out at the Danish National Hospital in Copenhagen using a 3T Siemens Magnetom TrioTim syngo B17 scanner with high-resolution MRI scanning of the brain, the 8th cranial nerve and inner ear. T1-weighted images were obtained before and after contrast media (MultiHance 0.1 mmol/kg) using a 3D magnetization preparation with rapid imaging sequence (repetition time [TR] = 2250 milliseconds/echo time [TE] = 2.94 milliseconds/inversion time = 900 milliseconds) with 1 mm isotropic resolution. Coronal T2-weighted FLAIR (TR = 9000 milliseconds/TE = 57 milliseconds/inversion time = 2500 milliseconds) and axial T2-weighted blade turbo spin echo (TR = 5500 milliseconds/TE = 113 milliseconds) images of the whole brain were acquired with 4 and 5 mm slice thickness, respectively. 3D T2-weighted turbo spin echo images (TR = 750 milliseconds/TE = 114 milliseconds) were acquired of the 8th cranial nerve, inner ear, and endolymphatic sac with 0.6 mm isotropic resolution. The MRIs that were not carried out at the Danish National Hospital in Copenhagen and those that were retrospectively reviewed for earlier ELST signs did not fulfill the described protocol of inner ear. These MRIs were predominantly axial T1 weighted obtained before and after contrast media and axial T2 weighted (both matrix = 2562 and FOV = 25 × 25 cm), both with 5 mm slice thickness.
Data assessment
All imaging data were collected and described by the same senior radiology specialist (C.T.) who identified the endolymphatic duct and sac on the 3D T1- and T2-weighted images and reported tumors and contrast enhancement. The audiological data were analyzed by the same senior ear-nose-throat specialist (S.G.) for signs of cochlear or retrocochlear pathology, with particular attention to interaural asymmetry and the configuration of the audiograms to assess whether an ELST could be suspected.
The meta-analysis
Through a review of the literature, we identified clinical descriptions of 135 additional vHL patients who were diagnosed with at least one radiologic confirmed ELST. The Pub Med database was searched for publications in English using combinations of the search words “ELST”/“Endolymphatic sac tumor/tumour” and “vHL”/“von Hippel-Lindau disease,” assessing all resulting papers and related papers published since 1993 when ELST was first described as a disease entity.44 Also, publications of vHL populations were reviewed and those containing patients with an ELST selected. Information of each ELST patient's age at diagnosis, audiovestibular symptoms, audiological examinations, symptom duration, type of VHL germline mutation, and vHL phenotype were extracted, pooled, and evaluated.
Ethics
The study was approved by the Danish Regional Committees on Biomedical Research Ethics and the Danish Data Protection Agency. All subjects in the prospective study gave their oral and written consent to participation.
RESULTS
The prospective study
Table 1 lists details of interviews, audiological examinations, and MRIs for all subjects, whereas Table 2 lists characteristics of subjects with an MRI-diagnosed ELST.
The overall occurrence of MRI-diagnosed ELSTs in this study population was 12.5% (5/40 subjects). Overall, 34% (13/38) of subjects reported subjective audiovestibular symptoms, and of these, three (23%) also had ELST suspect audiograms, and four (31%) were found to have MRI-visible ELSTs. Four of the five subjects with an MRI-diagnosed ELST had an ELST suspect audiometry, and three of these also reported subjective audiovestibular symptoms. Apart from the audiometric results, nothing further could be concluded based on the other test parameters of the audiological examination.
A retrospective review of the five ELST subjects' earlier MRIs, on which no ELSTs had previously been diagnosed, revealed that in two subjects the lesions could be seen 16.5 months and 51.5 months before ELST diagnosis, respectively. Neither of these two lesions had been acknowledged before this investigation even though both patients had undergone 3 and 2 MRIs, respectively. These two ELSTs were surgically removed, and histology confirmed one to be an ELST but revealed that the other was a hemangioblastoma. The subject with the hemangioblastoma that had been mistaken for an ELST radiologically (Subject 2 in Tables 1 and 2) had unremarkable audiometric findings and did not report any subjective audiovestibular symptoms.
The meta-analysis
Overall, 140 vHL patients with 156 radiologic confirmed ELSTs were identified in the literature and our prospective study (Table 3).
Approximately 11% (16/140) were reported to have bilateral ELSTs. Approximately 96% had at least one audiovestibular symptom at the time of ELST diagnosis. Among these, sensorineural hearing loss was found in 91% (N = 82/90), tinnitus in 64% (N = 58/90), vertigo in 52% (N = 47/90), disequilibrium in 18% (N = 16/90), sensation of aural fullness in 14% (N = 13/90), aural pain in 4% (N = 4/90), and facial nerve paresis in 8% (N = 7/90).1,2,4–15,18–28,30–34,37,40,45,46 The median time from subjective onset of symptoms, including cases with sudden onset, to ELST diagnosis was 3 years (range: 0 to >20 years, N = 26), and 27% of these patients (7/26) reported to have had subjective symptoms for more than 10 years.
Information from patients' audiological examinations was available for 102 ears with radiologically visible ELSTs, and 92% (94/102 ears) were described as being abnormal. Detailed information of audiometric patterns was given for 18 ears with ELSTs in the combined prospective study and meta-analysis.4–7,11 A distinct low-frequency hearing loss was described in 8 of these 18 ears, including three ears in the prospective study.4,6,7 In seven of the eight cases, audiograms were available for evaluation, demonstrating that the low-frequency hearing loss was exclusive, not involving frequencies above 1000 Hz. Tumor sizes were reported in six of the eight ELSTs associated with low-frequency hearing loss, and mean diameter was 2.5 mm (range: 1.4–11 mm).4,6,7 The remaining nine ELST ears with audiometric details showed various patterns, predominately severe to profound sensorineural hearing loss of all frequencies. Tumor size was only reported for two of these tumors, which were 2 mm and 12 mm in diameter, respectively.
DISCUSSION
We present the first systematic evaluation of ELST surveillance in the largest collective population of patients with vHL and ELST presented to date, based on a prospective national study including 90% of all known VHL mutation carriers in Denmark, and a meta-analysis of all reported patients with vHL and ELST in the literature since 1993. Our results indicate that annual audiometry is suitable as a first-line ELST screening tool among patients with vHL, especially in countries where surveillance MRIs are inaccessible. In countries where routine MRI of the central nervous system is performed every 12–36 months as part of a vHL surveillance program, the inner ear may be included in these examinations.
Based on the present findings, the use of subjective audiovestibular symptoms alone to target ELST screening is a too insensitive and unspecific approach, because these symptoms represent a broad and unspecific spectrum of symptoms. Further, it has been demonstrated that neither severity nor duration of audiovestibular symptoms are associated with radiologically determined tumor size39 and that there is no difference in the incidence of subjective hearing loss or tinnitus in vHL patients without radiologic ELST signs compared with their family members without vHL.2 Even though there was a high frequency of subjective symptoms of approximately 35% among subjects in the prospective study, almost 70% (9/13 subjects) of these subjects showed no ELST signs on either MRI or audiological examination. Furthermore, ELSTs are not always subjectively symptomatic at diagnosis as also seen in the prospective study.1,4,6,39 The high frequency of almost 100% of subjective audiovestibular symptoms before ELST diagnosis found in the meta-analysis might reflect bias in the included studies. Most studies identified patients unsystematically, and some patients may have been selected because of audiovestibular symptoms, rendering a group not representative of the general vHL population. This notion is supported by the long period of time from symptom onset to ELST diagnosis found in the meta-analysis where more than a fourth of ELST patients had audiovestibular symptoms for more than 10 years before an ELST was diagnosed.
Audiometry seems to be a good first-line screening tool in ELST surveillance for vHL patients. More than 90% of vHL patients with radiologically diagnosed ELSTs had abnormal audiometric findings when including only the studies reporting audiological parameters in the combined meta-analysis and prospective study.1,2,4,5,7,11,16,17,39 These results might be influenced by publication bias, because the three largest studies in the meta-analysis, overall accounting for 77 of the ELST ears with audiological data, were all from the same institution, without information of whether the same patients were included in more than one of the three series.1,2,39 Based on present results, use of audiometry seems to be more cost-effective than use of a full audiological examination, as audiometry alone is simpler to perform, and as we found no further ELST indicators based on the rest of test parameters in the full audiological examination.
In ELST patients with hearing loss, subjective symptom onset was described as being sudden in approximately half of patients and progressive in the other half.2,39 Based on the combined prospective study and meta-analysis, the development of progressive hearing loss seems to correlate with a characteristic audiological pattern.4–7,11 A distinct and exclusive low-frequency hearing loss was reported in almost half of ELST cases (8/18 ears) in which detailed audiologic data were available, and all were small ELSTs (mean diameter 2.5 mm). Larger ELSTs are described to cause profound sensorineural hearing loss involving all frequencies, yielding a flat audiometric curve.5,6 The mechanism for the sudden onset of hearing loss is described by Butman et al.39 to be tumor-associated intralabyrinthine hemorrhaging and can occur in even the smallest ELSTs. It is, however, not known whether ELST patients with sudden onset of hearing loss have had audiometric signs of a yet asymptomatic ELST before subjective symptom debut.
In the future, audiometry might be able to diagnose early-stage ELSTs before they can be seen on MRI. Audiovestibular symptoms and audiometric suspicion of ELSTs have been described to precede the visualization of ELSTs on MRI.4,47 In the prospective study, only two of the five subjects with an ELST had had both an audiological examination and MRIs of the inner ear before the study, and one of these subjects did have audiometric documented hearing loss 2 years before an ELST could be identified. Furthermore, almost 20% (14/74) of ears in the prospective study had audiometric suspicion of ELST without having MRI-visible ELSTs. Manski et al.1 also found an even higher incidence of almost 60% (29/49) with audiometric abnormalities among vHL patients without ELST imaging evidence. It cannot be excluded that these audiometric abnormalities are caused by microscopic ELSTs. Nevertheless, audiometry indicative of ELST without radiologic evidence does not warrant surgical intervention at this point, and better knowledge of clinical and audiometric patterns of ELSTs is needed. For this purpose, we have recently initiated an international collaborative study of audiological data and radiologic imaging in vHL patients with and without ELST (http://icmm.ku.dk/english/icmm-staff/marie_luise_bisgaard/vhl_collaborative_research/).
High-resolution MRI of the inner ear is considered to be the gold standard in ELST diagnosis.1,4,41,48,49 Nevertheless, many radiologic differential diagnoses exist for ELSTs such as paragangliomas, inner ear adenomas, inflammatory pseudotumors of the endolymphatic sac, and especially for vHL patients: hemangioblastomas and metastases from renal carcinoma.30,41,50
Diaz et al.30 have pointed out that with increasing focus on ELSTs as a part of vHL and simultaneous increased use of high-resolution MRI in inner ear diagnosis, more contrast-enhancing lesions of various origin are likely to be identified near the endolymphatic sac, increasing the rate of false-positive ELST diagnoses. Some lesions are radiologically indistinguishable from ELSTs, and histology is the only sure way of differentiation.30 In the meta-analysis, histological diagnosis of the ELSTs was only reported for approximately two third of cases. MRI-visible ELSTs that do not cause audiologic abnormalities could represent a margin of error of radiologic diagnosis. The true fraction of radiologically misdiagnosed ELSTs is unknown, as reports of tumors initially misdiagnosed as ELSTs are unlikely to be published. Also, especially small ELST may be overlooked on vHL patients' regular MRI surveillances if inner ear structures are not specifically evaluated. Manski et al.1 demonstrated that routine MRI of the posterior fossa missed 20% (3/15) of ELSTs that were visible on an MRI that also focused on the petrous bone. In the prospective study, two of the five MRI-diagnosed ELSTs had been missed on two and three previous brain surveillance MRIs before this study, on which the lesions could be identified retrospectively. Also, the long duration of symptoms before diagnosis found in the meta-analysis could partly be explained by these radiologic challenges.
Early identification of ELST may pose a dilemma for clinicians toward timing of surgical management of ELSTs: On one hand, the risk of sudden hearing loss may argue in favor of early surgical excision of tumors.4,6,8 On the other hand, risk of iatrogenic deafness and nerve damage after misdiagnosis and unwarranted operation could point to initial conservative management, as long as the ELST remains stable clinically and radiologically. Peyre et al.37 recently described a many-year conservative management of two ELSTs, which demonstrated a stuttering growth pattern and a prolonged stability in tumor size for more than 10 years in one case.
Indication for surgical removal weighs more heavily if the patient's bilateral hearing is threatened due to bilateral ELSTs or unilateral deafness in the opposite ear.6 In previous reports, the frequency of bilateral ELSTs has been reported to be as high as about 30% (14/43 patients),6 yielding a great risk of bilateral hearing loss. However, previous estimates are likely to be overestimations due to selection and publication bias, as we found a frequency of 11% (16/140) in the combined meta-analysis and prospective study.
We hypothesized that possible genotype-phenotype correlations could help target ELST surveillance through identification of high-risk vHL patients. In the combined data of the meta-analysis and the prospective study, we did, however, not find evidence to suggest that ELST surveillance can be individualized according to VHL genotype (Table 3). The proportion of mutations truncating the p.VHL to missense mutations did not differ significantly between ELST patients (59% and 41%) and the general vHL population (70% and 30%).3
As current ELST screening recommendations are based on best assessment and vary greatly between countries, there is a considerable need for international and evidence-based screening guidelines. Current Danish ELST screening guidelines, which correlate with the surveillance guidelines from the American vHL Family Alliance (personal communication), recommend one baseline audiometry in adolescence and MRI of the inner ear only when audiovestibular symptoms are present. However, as use of subjective audiovestibular symptoms is too unspecific a measure for ELST, and as manifest hearing loss is generally irreversible, this current approach is not adequate enough to prevent severe audiovestibular morbidity.
Based on our results, audiometry is a suitable first-line screening tool, and we recommend annual audiometry for vHL patients. This approach is minimally invasive and in many countries more easily accessible than regular MRI scans. An optimal interval for ELST surveillance could not be determined based on present results, and annual examinations are based on our best assessment. Further studies with long-term follow-up are needed to determine the optimal ELST surveillance interval.
Preoperative high-resolution MRI is still necessary to support the diagnosis in cases of audiometric ELST suspicion and to preoperatively map the lesion's location and extent. In countries where routine MRI of the central nervous system is performed every 12–36 months as part of a vHL surveillance program, we recommend that specific images of the petrous bone and endolymphatic sac should be included in these examinations.
Determination of audiological ELST characteristics could further target screening, and we have initiated an international collaborative study of audiological ELST characteristics.
References
Manski TJ, Heffner DK, Glenn GM, et al. Endolymphatic sac tumors. A source of morbid hearing loss in von Hippel-Lindau disease. JAMA 1997 277: 1461–1466
Choo D, Shotland L, Mastroianni M, et al. Endolymphatic sac tumors in von Hippel-Lindau disease. J Neurosurg 2004 100: 480–487
Maher ER Von Hippel-Lindau disease. Curr Mol Med 2004 4: 833–842
Kim HJ, Butman JA, Brewer C, et al. Tumors of the endolymphatic sac in patients with von Hippel-Lindau disease: implications for their natural history, diagnosis, and treatment. J Neurosurg 2005 102: 503–512
Jagannathan J, Lonser RR, Stanger RA, et al. Cochlear implantation for hearing loss associated with bilateral endolymphatic sac tumors in von Hippel-Lindau disease. Otol Neurotol 2007 28: 927–930
Megerian CA, Haynes DS, Poe DS, Choo DI, Keriakas TJ, Glasscock ME III, Hearing preservation surgery for small endolymphatic sac tumors in patients with von Hippel-Lindau syndrome. Otol Neurotol 2002 23: 378–387
Lonser RR, Kim HJ, Butman JA, Vortmeyer AO, Choo DI, Oldfield EH Tumors of the endolymphatic sac in von Hippel-Lindau disease. N Engl J Med 2004 350: 2481–2486
Hansen MR, Luxford WM Surgical outcomes in patients with endolymphatic sac tumors. Laryngoscope 2004 114: 1470–1474
Gaffey MJ, Mills SE, Boyd JC Aggressive papillary tumor of middle ear/temporal bone and adnexal papillary cystadenoma. Manifestations of von Hippel-Lindau disease. Am J Surg Pathol 1994 18: 1254–1260
Delisle MB, Uro E, Rouquette I, Yardeni E, Rumeau JL Papillary neoplasm of the endolymphatic sac in a patient with von Hippel-Lindau disease. J Clin Pathol 1994 47: 959–961
Jagannathan J, Butman JA, Lonser RR, et al. Endolymphatic sac tumor demonstrated by intralabyrinthine hemorrhage. Case report. J Neurosurg 2007 107: 421–425
Megerian CA, McKenna MJ, Nuss RC, et al. Endolymphatic sac tumors: histopathologic confirmation, clinical characterization, and implication in von Hippel-Lindau disease. Laryngoscope 1995 105: 801–808
Kempermann G, Neumann HP, Scheremet R, et al. Deafness due to bilateral endolymphatic sac tumours in a case of von Hippel-Lindau syndrome. J Neurol Neurosurg Psychiatry 1996 61: 318–320
Tibbs RE Jr, Bowles AP Jr, Raila FA, Fratkin JD, Hutchins JB Should endolymphatic sac tumors be considered part of the von Hippel-Lindau complex? Pathology case report. Neurosurgery 1997 40: 848–855
Ouallet JC, Marsot-Dupuch K, Van ER, et al. Papillary adenoma of endolymphatic sac origin: a temporal bone tumor in von Hippel-Lindau disease. Case report. J Neurosurg 1997 87: 445–449
Vortmeyer AO, Choo D, Pack SD, et al. von Hippel-Lindau disease gene alterations associated with endolymphatic sac tumor. J Natl Cancer Inst 1997 89: 970–972
Kawahara N, Kume H, Ueki K, et al. VHL gene inactivation in an endolymphatic sac tumor associated with von Hippel-Lindau disease. Neurology 1999 53: 208–210
Ayadi K, Mahfoudh KB, Khannous M, et al. Endolymphatic sac tumor and von Hippel-Lindau disease: imaging features. AJR Am J Roentgenol 2000 175: 925–926
Horiguchi H, Sano T, Toi H, Kageji T, Hirokawa M, Nagahiro S Endolymphatic sac tumor associated with a von Hippel-Lindau disease patient: an immunohistochemical study. Mod Pathol 2001 14: 727–732
de MC, Giraud S, Bordure P, Richard S, Huy PT Radiology quiz case. Papillary neoplasm of the endolymphatic sac in a patient with von Hippel-Lindau disease. Arch Otolaryngol Head Neck Surg 2002 128: 855–856
Korner M, Linder T, Gebbers JO Secretory IgA in the endolymphatic sac tumour. Histopathology 2003 42: 98–99
Williamson RA, Coker NJ Endolymphatic sac tumor in von Hippel-Lindau disease. Otol Neurotol 2003 24: 832
Kupferman ME, Bigelow DC, Carpentieri DF, Bilaniuk LT, Kazahaya K Endolymphatic sac tumor in a 4-year-old boy. Otol Neurotol 2004 25: 782–786
Hashimoto M, Yokota A, Urasaki E, Imada H, Yamamoto H Surgical treatment of endolymphatic sac tumor with adjunctive stereotactic radiation therapy—case report. Neurol Med Chir (Tokyo) 2004 44: 595–599
Jensen RL, Gillespie D, House P, Layfield L, Shelton C Endolymphatic sac tumors in patients with and without von Hippel-Lindau disease: the role of genetic mutation, von Hippel-Lindau protein, and hypoxia inducible factor-1alpha expression. J Neurosurg 2004 100: 488–497
Muzumdar DP, Goel A, Fattepurkar S, Goel N Endolymphatic sac carcinoma of the right petrous bone in Von Hippel-Lindau disease. J Clin Neurosci 2006 13: 471–474
Schipper J, Maier W, Rosahl SK, et al. Endolymphatic sac tumours: surgical management. J Otolaryngol 2006 35: 387–394
Kilickesmez O Endolymphatic sac tumor in a patient with von Hippel-Lindau disease: MR imaging findings. Diagn Interv Radiol 2006 12: 14–16
Bisceglia M, D'Angelo VA, Wenig BM Endolymphatic sac papillary tumor (Heffner tumor). Adv Anat Pathol 2006 13: 131–138
Diaz RC, Amjad EH, Sargent EW, Larouere MJ, Shaia WT Tumors and pseudotumors of the endolymphatic sac. Skull Base 2007 17: 379–393
Pavesi G, Feletti A, Berlucchi S, et al. Neurosurgical treatment of von Hippel-Lindau-associated hemangioblastomas: benefits, risks and outcome. J Neurosurg Sci 2008 52: 29–36
Skalova A, Sima R, Bohus P, Curik R, Lukas J, Michal M Endolymphatic sac tumor (aggressive papillary tumor of middle ear and temporal bone): report of two cases with analysis of the VHL gene. Pathol Res Pract 2008 204: 599–606
Safatle PP, Farage L, Sampaio A, et al. Endolymphatic sac tumor and von Hippel-Lindau disease in a single family. Arq Neuropsiquiatr 2009 67: 1097–1099
Codreanu CM, Duet M, Hautefort C, et al. Endolymphatic sac tumors in von Hippel-Lindau disease: report of three cases. Otol Neurotol 2010 31: 660–664
Gomy I, Molfetta GA, de Andrade BE, et al. Clinical and molecular characterization of Brazilian families with von Hippel-Lindau disease: a need for delineating genotype-phenotype correlation. Fam Cancer 2010 9: 635–642
Rao Q, Zhou J, Wang JD, et al. Endolymphatic sac tumor with von Hippel-Lindau disease: report of a case with analysis of von Hippel-Lindau gene and review. Ann Diagn Pathol 2010 14: 361–364
Peyre M, Gaillard S, Van ER, Giraud S, Richard S Conservative management of endolymphatic sac tumors in von Hippel-Lindau disease: case report. Acta Neurochir (Wien) 2011; 153: 42–47; discussion 47.
Hes FJ, van der Luijt RB, Janssen AL, et al. Frequency of Von Hippel-Lindau germline mutations in classic and non-classic Von Hippel-Lindau disease identified by DNA sequencing, Southern blot analysis and multiplex ligation-dependent probe amplification. Clin Genet 2007 72: 122–129
Butman JA, Kim HJ, Baggenstos M, et al. Mechanisms of morbid hearing loss associated with tumors of the endolymphatic sac in von Hippel-Lindau disease. JAMA 2007 298: 41–48
Lonser RR, Baggenstos M, Kim HJ, Butman JA, Vortmeyer AO The vestibular aqueduct: site of origin of endolymphatic sac tumors. J Neurosurg 2008 108: 751–756
Mukherji SK, Albernaz VS, Lo WW, et al. Papillary endolymphatic sac tumors: CT, MR imaging, and angiographic findings in 20 patients. Radiology 1997 202: 801–808
Poulsen ML, Budtz-Jorgensen E, Bisgaard ML Surveillance in von Hippel-Lindau disease (vHL). Clin Genet 2010 77: 49–59
Elberling C, Ludvigsen C, Lyregaard PE DANTALE: a new Danish speech material. Scand Audiol 1989 18: 169–175
Li JC, Brackmann DE, Lo WW, Carberry JN, House JW Reclassification of aggressive adenomatous mastoid neoplasms as endolymphatic sac tumors. Laryngoscope 1993 103: 1342–1348
Priesemann M, Davies KM, Perry LA, et al. Benefits of screening in von Hippel-Lindau disease—comparison of morbidity associated with initial tumours in affected parents and children. Horm Res 2006 66: 1–5
Codreanu C, Tran Ba HP Isolate vertigo crisis revealing an endolymphatic sac tumor. Rom J Morphol Embryol 2010 51: 387–389
Butman JA, Linehan WM, Lonser RR Neurologic manifestations of von Hippel-Lindau disease. JAMA 2008 300: 1334–1342
Lo WW, Applegate LJ, Carberry JN, et al. Endolymphatic sac tumors: radiologic appearance. Radiology 1993 189: 199–204
Bambakidis NC, Megerian CA, Ratcheson RA Differential grading of endolymphatic sac tumor extension by virtue of von Hippel-Lindau disease status. Otol Neurotol 2004 25: 773–781
Connor SE, Leung R, Natas S Imaging of the petrous apex: a pictorial review. Br J Radiol 2008 81: 427–435
Acknowledgements
This work was supported by King Christian the 10th's Foundation, Frode V. Nyegaard and his wife's Foundation, Consul General Friedrich Bøhm and daughter Else Bøhm's Foundation, Minister Erna Hamilton's Grant for Science and Art, the Harboe Foundation, and the Michaelsen Foundation. The authors especially thank all participating vHL patients and the Danish vHL Patient Association for their help. They are grateful to consultants Leif Christensen and Preben Sørensen, Professor Kim Brixen, and doctors Boye Berthelsen and Irene Kibæk Nielsen for referral and care of study patients and to consultant Lars Poulsgaard for helpful discussions and surgical treatment of ELSTs.
Author information
Authors and Affiliations
Corresponding author
Additional information
Work done in collaboration with the Danish von Hippel-Lindau Coordination Group.
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Poulsen, M., Gimsing, S., Kosteljanetz, M. et al. von Hippel-Lindau disease: Surveillance strategy for endolymphatic sac tumors. Genet Med 13, 1032–1041 (2011). https://doi.org/10.1097/GIM.0b013e31822beab1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31822beab1
Keywords
This article is cited by
-
Clinicoradiologic characteristics of endolymphatic sac tumors
European Archives of Oto-Rhino-Laryngology (2019)
-
Identification of 3 novel VHL germ-line mutations in Danish VHL patients
BMC Medical Genetics (2012)