Abstract
Purpose: The success of any surveillance program depends not solely on its technological aspects but also on the commitment of participants to adhere to follow-up investigations, which is influenced by the psychological impact of surveillance. This study investigates the psychological impact of participating in a pancreatic cancer surveillance program.
Methods: High-risk individuals participating in an endoscopic ultrasonography-magnetic resonance imaging-based pancreatic cancer surveillance program received a questionnaire assessing experiences with endoscopic ultrasonography and magnetic resonance imaging, reasons to participate, psychological distress, and benefits and barriers of surveillance. High-risk individuals were individuals with a strong family history of pancreatic cancer or carriers of pancreatic cancer-prone gene mutations.
Results: Sixty-nine participants (85%) completed the questionnaire. Surveillance was reported as “very to extremely uncomfortable” by 15% for magnetic resonance imaging and 14% for endoscopic ultrasonography. Most reported reason to participate was that pancreatic cancer might be detected in a curable stage. Abnormalities were detected in 27 respondents, resulting in surgical resection in one individual and a shorter follow-up interval in five individuals. Surveillance outcomes did not influence cancer worries. Overall, 29% was “often” or “almost always” concerned about developing cancer. Six respondents (9%) had clinical levels of depression and/or anxiety. According to 88% of respondents, advantages of surveillance outweighed disadvantages.
Conclusions: Although endoscopic ultrasonography is more invasive than magnetic resonance imaging, endoscopic ultrasonography was not perceived as more burdensome. Despite one third of respondents worrying frequently about cancer, this was not related to the surveillance outcomes. Anxiety and depression levels were comparable with the general population norms. Advantages of participation outweighed disadvantages according to the majority of respondents. From a psychological point of view, pancreatic cancer surveillance in high-risk individuals is feasible and justified.
Similar content being viewed by others
Main
With a median survival of less than 6 months and a 5-year survival of <5%, pancreatic cancer (PC) is one of the most fatal of human malignancies.1,2 The poor prognosis is mainly due to the late onset of symptoms and the aggressiveness of this tumor type, such that the majority of patients presents with incurable disease. A way to improve the prognosis of this disease would be to diagnose precursor lesions or a malignancy at an early asymptomatic stage when resection offers the best chance for cure. PC surveillance of the general population is not feasible because of the relatively low incidence of PC (10/100,000 in the Western World)3,4 and the lack of a noninvasive, reliable, and cheap surveillance tool. However, surveillance might be worthwhile when offered to subpopulations of individuals who are at high risk of developing PC.
Currently, several groups of individuals at high risk of developing PC have been identified. These include (1) mutation carriers of PC-prone hereditary syndromes (syndromic PC) and (2) individuals with a strong family history of PC but without a known underlying genetic defect (familial PC [FPC]).5 The lifetime risk of developing PC in these inherited and familial syndromes is strongly increased compared with the general population. This lifetime risk is estimated to be ∼10% in mutation carriers of BRCA1, BRCA2, mismatch repair genes, and TP53 from families affected by at least two PC cases, up to 17% for CDKN2A mutation carriers, up to 36% for patients with the Peutz Jeghers syndrome, and can exceed 40% in FPC family members with three affected first-degree relatives (FDR).6
Some studies have already provided information about the effectiveness of surveillance.7–12 In these studies, the effectiveness of different surveillance techniques, such as computed tomography, magnetic resonance imaging (MRI), and endoscopic ultrasonography (EUS), were investigated. Preliminary results of these studies are promising, although it is still unclear whether surveillance will actually improve survival. When assessing the success of a surveillance program, it is important not only to focus on technological aspects such as test performance but also to focus on the psychological aspects related to surveillance.13 For example, a surveillance tool might be technologically successful in detecting cancer in a curable stage. However, if individuals do not participate in the surveillance program because the psychological burden of surveillance is too high, a surveillance program will ultimately not be successful. To date, knowledge about the psychological aspects of PC surveillance is limited. Thus far, only three articles have been published that address the psychological aspects of PC surveillance.14–16 These studies provide relevant information on patient views regarding the value of genetic counseling for FPC in the absence of predictive genetic testing,16 psychological well-being of high-risk individuals participating in PC surveillance,15 and intentions of high-risk individuals to participate in PC surveillance.14 Knowledge is limited about the specific experiences of high-risk individuals with PC surveillance, their perceived burden, and expectations of such a surveillance program.
These are important topics that should to be taken into account when studying the feasibility of a PC surveillance program from a psychological point of view.17 Therefore, this study was undertaken to investigate the psychological impact of an EUS-MRI-based PC surveillance among high-risk individuals and to evaluate whether PC surveillance is psychologically feasible. Specific aims of this study were to (1) investigate participants' experienced burden of a PC surveillance program, (2) investigate their motivations to participate in such a program, (3) investigate general levels of distress and, and (4) identify factors associated with anxiety experienced during an EUS-MRI-based surveillance program.
METHODS
Sample
Eligible for this psychological questionnaire study were all participants of a Dutch PC surveillance study. This is a multicenter prospective study investigating the effectiveness of PC surveillance in high-risk individuals. High-risk individuals were defined as (1) FDR of patients with FPC and (2) carriers of a PC-prone gene mutation. FPC kindreds are defined as families with (1) at least two FDR with PC, (2) at least three relatives with PC (FDR or second-degree relative [SDR]), or (3) at least two SDR relatives with PC of which one was <50 years at time of diagnosis. PC-prone gene mutations include CDKN2A (familial atypical multiple mole melanoma syndrome), LKB1 (Peutz Jeghers syndrome), BRCA1 (hereditary breast and ovarian cancer syndrome), BRCA2 (hereditary breast and ovarian cancer syndrome), mismatch repair genes (Lynch syndrome), and TP53 (Li-Fraumeni syndrome). Carriers of a BRCA1/2 mutation, mismatch repair gene, or TP53 mutation are only eligible when at least two family members are affected by PC. The minimal age for inclusion is 45 years or at least 10 years younger than the age of the youngest relative with PC. Patients with Peutz Jeghers syndrome have to be at least aged 30 years. Before inclusion, all high-risk individuals were extensively evaluated by a clinical geneticist. This evaluation included (1) obtaining a detailed personal and family medical history, (2) verification of clinical diagnoses reported by patients and family members, by review of medical and pathologic records, and by revision of histological slides whenever available, and (3) based on the medical information, genetic testing for the suspected gene mutation(s). Clinical geneticists informed all high-risk individuals that EUS and MRI surveillance was offered as part of a research protocol and that the effectiveness of PC surveillance has not been proven yet. In this counseling, the possibility of false-positive and false-negative outcomes of the PC screening was also explained, as well as a possible cancer diagnosis, or findings of undetermined significance.
Procedure of PC surveillance study
Enrolment in the PC surveillance study started in October 2006 and is currently ongoing in four Dutch medical centers (Erasmus MC-University Medical Center in Rotterdam, University Medical Center Groningen, Academic Medical Center in Amsterdam and The Netherlands Cancer Institute-Antoni van Leeuwenhoek Hospital in Amsterdam). Surveillance entails EUS and MRI. Both tests are scheduled on different days, at maximum 2 weeks apart. EUS is performed under conscious sedation (midozalam/fentanyl). Individuals without pancreatic abnormalities and individuals with a small cystic lesion without malignant features are scheduled for annual follow-up. Whenever EUS and/or MRI detect an abnormality, management is based on consensus agreement of an expert panel (experienced endosonographers, surgeons, and radiologists). This management strategy can either be (1) surgical resection in case of a highly suspicious lesion (solid lesion, main duct intraductal papillary mucinous neoplasm [IPMN], or branch type IPMN > 30 mm and/or with malignant features) or (2) shortening of the follow-up interval to 3 months.
Psychological questionnaire study
Since October 2008, a questionnaire study was added to this PC surveillance study. The institutional review boards of the participating hospitals approved the psychosocial questionnaire study. All participants of the PC surveillance study received a letter of invitation by their gastroenterologist and a questionnaire 4 weeks after receiving their surveillance results. Those who did not respond to the initial letter of invitation were sent a reminder letter and a copy of the questionnaire approximately 2 weeks later.
Measurements
Sociodemographic and clinical data.
Data were obtained by medical records and our questionnaire on age, sex, marital status, offspring, level of education, personal cancer history, family cancer history, genetic background, surveillance results, and surveillance follow-up policy.
Family history of PC.
Participants were asked whether and, if so, how many FDR (i.e., parents, siblings, or children) and SDR (i.e., uncles, aunts, grandparents, nieces, and nephews) ever had cancer. Parallel questions were posed regarding the death of a FDR and/or SDR due to cancer (i.e., At what age did a close relative die of (pancreatic) cancer?).
Participants' view on surveillance
Motivations to undergo PC surveillance.
Participants were asked to select from a checklist their motive(s) for undergoing PC surveillance. Space was also provided for additional reasons not listed in the checklist.18
Attitudes toward, and experiences with, participation in PC surveillance.
A 16-item questionnaire comprising four subscales was used, assessing communication (with the physician), reassurance, nervous anticipation, and specific perceived disadvantages.19 Furthermore, specific questions about experiences with each of the surveillance interventions (EUS and MRI) were developed by our group, for example: “How did you experience undergoing a MRI? Was this experience: not uncomfortable, slightly uncomfortable, very uncomfortable or extremely uncomfortable.”
Benefits and barriers.
The perceived benefits and barriers to PC surveillance were assessed with six questions adapted from previous work.20,21
Perceived risk.
Respondents were asked to report their perceived risk of developing cancer (again) compared with that of an average person in the Dutch population of their age (item adapted from Lerman et al.22). Response categories ranged from “lower” to “much higher.” Furthermore, participants were asked on a scale from 0 to 100 what they thought their chance was of developing PC with and without undergoing yearly PC surveillance.
Psychological distress
Cancer-related worries.
Cancer-related worries were assessed with the eight-item Cancer Worry Scale.23–25 Scores range from 8 to 32, with higher scores indicating more frequent worries about cancer. Internal consistency in this study was indicated by a Cronbach's alpha of 0.84, which is considered high.
Anxiety and depression.
Anxiety and depression levels were measured with the 14-item Hospital Anxiety and Depression Scale (HADS).26–28 Generalized anxiety (HADS-A) and depression (HADS-D) were measured with two seven-item subscales. Response options range from 0 (not at all) to 3 (very much), adding to a maximum score of 21 for each subscale. A score of ≥11 on a subscale reflects a high level of anxiety or depression and is considered a clinically significant disorder. A score between 8 and 10 is defined as a “moderate level of distress,” suggesting a mild disorder. Cronbach's alpha in this study was 0.82 for the Anxiety Subscale and 0.80 for the Depression Subscale.
Data analyses
Descriptive statistics was generated to describe the study sample in terms of sociodemographic and clinical background characteristics, to report on the experiences with the surveillance interventions, and to document the prevalence of psychological distress.
Depending on the level of measurement, χ2 test or Student's t test was used to identify sociodemographic (i.e., age, gender, education, marital status, and offspring), clinical (i.e., history of cancer and surveillance result), or psychological (i.e., risk perception and experiences with MRI and EUS) variables significantly associated with anxiety at the univariate level, using “a low level of anxiety” (scores between 0 and 7 on the anxiety scale of the HADS) and “moderate to high levels of anxiety” (scores ≥8) as dependent variable. All analyses were conducted using the Statistical Package for the Social Sciences (version 17.0; SPSS Institute, Chicago, IL).
RESULTS
Response
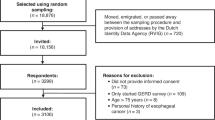
Of the 81 eligible individuals, 69 (85%) returned a completed questionnaire. None of the nonrespondents had had cancer, whereas 20 (29%) of the respondents had been treated for cancer (P = 0.03). No statistically significant differences were found between the respondents and nonrespondents with respect to any other sociodemographic (age and gender) and clinical (genetic background, personal cancer history, surveillance technique undergone, baseline or follow-up surveillance, surveillance results, and type of abnormality found) variables. The 69 respondents stemmed from 50 families.
Characteristics of the study sample
As listed in Table 1, the mean age of the sample was 52 years (range = 20–71 years). Men and women were equally represented. Thirty-eight respondents (55%) carried a proven PC-prone gene mutation. Twenty respondents (29%) had been treated for any type of cancer (Table 1). The mean number of relatives with cancer (including FDR, SDR, and third-degree relatives) was 6.8 (range = 0–22, SD 3.6). The mean number of relatives with PC was 1.9 (range = 0–5, SD 1.10).
Nearly all respondents (96%) had undergone both EUS and MRI surveillance investigations. Three individuals (4%) did not undergo MRI, two because of claustrophobia, and in one, MRI was contraindicated (because of a metallic expander in the breast). Twenty-eight respondents (41%) completed the questionnaire after they had undergone their first-time (baseline) surveillance; all others had already undergone at least one surveillance investigation before. Thus far, there are no dropouts in the surveillance program. In 27 respondents (39%), EUS and/or MRI detected an abnormality. The most frequent detected abnormalities were cystic lesions. In 20 individuals, a total of 35 cystic lesions were detected by EUS and/or MRI. The median size of the cystic lesions was 5.5 mm (SD: 3.6, range: 2–18 mm). None of the cysts showed malignant features. In one individual, a solid lesion was detected, which was morphological suspicious for a malignancy and, therefore, surgically resected. Pathologic examination did not reveal a malignancy, but premalignant lesions (PanIN-2 and an incipient IPMN) were detected. Five individuals were rescheduled for interval investigations after 3 months, four because of the detection of a lesion of undetermined significance and one because of the suspicion of a newly developed cyst found during follow-up investigations.
Motivations to participate
As listed in Table 2, all respondents reported that a reason to participate in the PC surveillance program was that surveillance might lead to early detection of PC in a stage when it is still curable. Contributing to scientific research was the second most frequently reported motivation. When asked for their opinion about the effectiveness of PC surveillance, 43 respondents (62%) reported that a tumor in the pancreas can “certainly” be detected by EUS and MRI, and 25 (36%) reported that a tumor in the pancreas can “probably” be detected by EUS and MRI (not in the table).
Experiences with EUS and MRI
Seventeen respondents (25%) had experienced the EUS and/or the MRI investigation as very to extremely uncomfortable. Of these respondents, three experienced both EUS and MRI as very to extremely uncomfortable. Seven respondents (10%) experienced only EUS as very to extremely uncomfortable, mostly because the sedation was experienced as inadequate or related to postsedation effects as prolonged drowsiness. Seven other respondents (11%) reported MRI to be very or extremely uncomfortable, predominantly because of claustrophobia. There was no statistically significant difference in the frequency that respondents were dreading one of the two procedures. In Table 3, detailed information on experiences and attitudes toward PC surveillance is presented. One fifth of the respondents reported to be nervous before a follow-up visit and to dread the follow-up visits. However, only five respondents (7%) preferred follow-up visits less frequently. With respect to the general disadvantages, only 10 (14%) of the respondents experienced the investigations as burdensome and 12 (17%) reported that the follow-up visits reminded them of PC while they would rather think less often about it. Approximately 70% of the respondents reported that the surveillance investigations gave them a sense of security and that they would worry more about the disease if there were no follow-up visits. Approximately 90% said that perceived advantages of follow-up outweighed perceived disadvantages.
PC risk perception
Forty respondents (58%) perceived their risk of developing PC as moderately to extremely elevated compared with the general population. Thirty-seven respondents (54%) reported a lower personal risk percentage if participating in surveillance compared with not participating in surveillance, whereas 30 respondents (43%) reported the same personal risk to develop PC with or without surveillance.
Psychological distress
Cancer worries
Respondents worried most about the possibility of getting cancer (n = 20, 29%), and 17 individuals (25%) worried about the chance of family members developing cancer (Table 4). There was no correlation between PC surveillance results and cancer worries. Even those individuals in whom the positive PC surveillance results led to a change of management (n = 1 surgical resection, n = 5 shortening of follow-up interval) did not experience more concerns about cancer. In the majority of respondents (99%), cancer worries did not affect their mood and did not interfere with their daily activities.
Anxiety and depression
The mean scores of the HADS subscales were 4.2 on the anxiety scale (range: 0–14, SD = 3.7) and 3.0 on the depression scale (range: 0–13, SD = 3.2). Scores above 10 on the HADS subscales indicate a significant clinical level of anxiety or depression and were represented in six respondents (9%). One of them scored above cutoff on the depression subscale, two of them scored above the cutoff on the anxiety subscale, and three respondents scored above the cutoff on both the anxiety and the depression subscales.
In Table 5, the anxiety scale of the HADS is divided into two groups: (1) low-anxiety levels (scores 0–7) and (2) moderate to high anxiety levels (score = 8). Fifty-eight participants had low-anxiety levels, and 11 participants had moderate to high anxiety levels. None of the sociodemographic (i.e., age, gender, education, marital status, and offspring), clinical (i.e., history of cancer, surveillance result, and approaching the age at which a close relative died of cancer), or psychological (i.e., risk perception and experiences with MRI and EUS) variables were significantly associated with moderate to high levels of anxiety except for “worrying about follow-up investigations” (P = 0.04). Having worries about the next MRI was significantly associated with higher levels of anxiety.
Furthermore, individuals with a positive surveillance result (abnormalities found during surveillance) were not more anxious, depressed, and did not have more worries about developing cancer, than individuals with a negative surveillance result.
DISCUSSION
For a surveillance program to be effective, it is not only important to use sensitive screening techniques but it is also crucial that participants adhere to the program. Adherence to a surveillance program is influenced by one's experiences with the program, and therefore, insight in the psychological experiences with this surveillance program is of great importance. Insight in these experiences is particularly relevant for this high-risk group as most individuals have experienced multiple losses due to PC, contributing to a higher psychological burden of undergoing these procedures. Second, because of their lifelong PC risk, they should adhere to the screening on a lifelong regimen. Because of this repetitive nature of surveillance, it is of great importance that the burden of the procedures in this high-risk group is studied in detail, allowing possible adaptations in the procedure in a way that they are well tolerated by high-risk individuals. To our knowledge, this is the first study to investigate the specific experiences, such as the perceived burden, of high-risk individuals with a PC surveillance program, consisting of annual surveillance by MRI and EUS. Our results show that EUS-MRI-based PC surveillance among individuals at high risk for developing PC is feasible from a psychological point of view. This is supported by the fact that the majority of respondents did not experience surveillance by EUS (with sedation) and MRI as psychologically too burdensome.
One of the aims of this study was to investigate the motivation of high-risk individuals to participate in a PC surveillance program. Although the effectiveness of PC surveillance seems promising based on theoretical reasoning and preliminary (pre) clinical data, we currently lack long-term results that indicate that PC surveillance will actually prevent people from dying of PC. This unproven efficacy was extensively discussed with all potential participants before they decided whether to participate in the surveillance study. Nevertheless, the most frequently reported reason to participate was that surveillance might lead to early detection of PC at a stage when it is still curable. All respondents indicated this reason as being one of their motivations to participate. It is important to realize that because of the posttest design of our study, these results are based on information from individuals who had decided to participate in the PC surveillance program. Nonparticipants may not believe in the ability of early detection of PC. Future results of our ongoing prospective psychological study that includes both participants and nonparticipants of the surveillance study will provide information about reasons not to participate. Preliminary results of this ongoing prospective study show that only a small proportion (14%) of the high-risk individuals decline participation in the PC surveillance program (unpublished data). We, therefore, expect that our current data are not severely biased with respect to those reporting a favorable attitude. Furthermore, this study has a high response rate (85%), suggesting that the results are representative for the total group of high-risk individuals participating in the PC surveillance program.
At present, EUS is the most promising PC surveillance technique.7,9,29 Compared with MRI, EUS is an invasive technique, and for this reason, we hypothesized that the acceptability of EUS would be lower compared with MRI. Remarkably, we found that EUS and MRI were regarded as equally burdensome. One explanation might be the routine use of conscious sedation for EUS. Another perspective was given by Lewis et al.,14 who stated that individuals with a family history of PC or a personal history of cancer often prefer the more invasive surveillance techniques.
Another aim of this study was to investigate the general psychological distress participants might experience and the extent to which levels of anxiety are related to participating in the surveillance program. With respect to cancer-specific worries, Maheu et al.15 reported that pretest cancer worries remained the most important predictor for cancer worries after undergoing PC surveillance. This suggests that the frequency of cancer worries reported in this study by high-risk individuals after undergoing PC surveillance may have been the same before undergoing surveillance. This is in concordance with the finding that the surveillance result itself did not have an impact on the level of cancer worries. Despite the fact that approximately a quarter of respondents worried about the possibility of getting cancer themselves or worried about their relatives developing cancer, these worries did not interfere with their daily activities, suggesting that respondents seem to cope well with these worries.
Anxiety and depression scores at a level that does indicate a need for professional psychosocial care were present in approximately 10% of the respondents. This is comparable with the proportion of individuals in the general Dutch population30 and suggests that the levels of distress found in respondents are not a result of participation in the surveillance program but may have other causes.
In contrast to our expectations, we did not find a statistically significant association between surveillance results and levels of anxiety. The only factor that was significantly associated with a higher level of anxiety was anticipating worries about undergoing follow-up MRI.
In this study, respondents completed questionnaires after receiving their surveillance results. Therefore, it is not possible to investigate possible changes in distress levels and risk perception as a result of participation in the PC surveillance program. Future results of our ongoing prospective psychological study, which includes both participants and nonparticipants, will provide more information on possible causal relationships between the surveillance program and participants' psychological well-being. These results in combination with results of additional studies will hopefully shed greater light on perceived burden of PC surveillance, the perceived distress of surveillance, motivations to participate, and the emotional response to the test results.
In summary, results of our study indicate that PC surveillance by EUS and MRI is feasible from a psychological point of view. Although EUS is more invasive than MRI, there is no significant difference in the percentage of respondents who perceived one of the surveillance methods as more burdensome. Although almost one third of respondents worry frequently about cancer and a minority of respondents actually have anxiety and depression levels that indicate clinically significant disorder, there was no association with surveillance results, and the large majority of participants expressed a positive attitude toward the PC surveillance program.
References
Edwards BK, Brown ML, Wingo PA, et al. Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst 2005 97: 1407–1427
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin 2009 59: 225–249
National Cancer Institute. Surveillance epidemiology and end results. Available at: http://seer.cancer.gov/statfacts/html/pancreas. Accessed March 15, 2011.
Integrale Kanker Centra N. Kankerregistratie. Available at: www.ikcnet.nl. Accessed March 15, 2011.
Brand RE, Lerch MM, Rubinstein WS, et al. Advances in counselling and surveillance of patients at risk for pancreatic cancer. Gut 2007 56: 1460–1469
Klein AP, Brune KA, Petersen GM, et al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res 2004 64: 2634–2638
Canto MI, Goggins M, Hruban RH, et al. Screening for early pancreatic neoplasia in high-risk individuals: a prospective controlled study. Clin Gastroenterol Hepatol 2006 4: 766–781
Langer P, Kann PH, Fendrich V, et al. Five years of prospective screening of high-risk individuals from families with familial pancreatic cancer. Gut 2009 58: 1410–1418
Poley JW, Kluijt I, Gouma DJ, et al. The yield of first-time endoscopic ultrasonography in screening individuals at a high risk of developing pancreatic cancer. Am J Gastroenterol 2009 104: 2175–2181
Rulyak SJ, Brentnall TA Inherited pancreatic cancer: surveillance and treatment strategies for affected families. Pancreatology 2001 1: 477–485
Verna EC, Hwang C, Stevens PD, et al. Pancreatic cancer screening in a prospective cohort of high-risk patients: a comprehensive strategy of imaging and genetics. Clin Cancer Res 2010 16: 5028–5037
Vasen HF, Wasser M, van Mil A, et al. Magnetic resonance imaging surveillance detects early-stage pancreatic cancer in carriers of a p16-Leiden mutation. Gastroenterology 2011 140: 850–856
Wilson JM, Jungner YG [Principles and practice of mass screening for disease] Principios y metodos del examen colectivo para identificar enfermedades. Bol Oficina Sanit Panam 1968 65: 281–393
Lewis ZK, Frost CJ, Venne VL Pancreatic cancer surveillance among high-risk populations: knowledge and intent. J Genet Couns 2009 18: 229–238
Maheu C, Vodermaier A, Rothenmund H, et al. Pancreatic cancer risk counselling and screening: impact on perceived risk and psychological functioning. Fam Cancer 2010 9: 617–624
Axilbund JE, Brune KA, Canto MI, et al. Patient perspective on the value of genetic counselling for familial pancreas cancer. Hered Cancer Clin Pract 2005 3: 115–122
Bleiker EM, Menko FH, Taal BG, et al. Screening behavior of individuals at high risk for colorectal cancer. Gastroenterology 2005 128: 280–287
Bleiker EM, Aaronson NK, Menko FH, et al. Genetic counseling for hereditary cancer: a pilot study on experiences of patients and family members. Patient Educ Couns 1997 32: 107–116
Stiggelbout AM, de Haes JC, Vree R, et al. Follow-up of colorectal cancer patients: quality of life and attitudes towards follow-up. Br J Cancer 1997 75: 914–920
Champion VL Instrument development for health belief model constructs. Adv Nurs Sci 1984 6: 73–85
Kash KM, Holland JC, Osborne MP, Miller DG Psychological counseling strategies for women at risk for breast cancer. J Natl Cancer Inst 1995 17: 73–79
Lerman C, Kash K, Stefanek M Younger women at increased risk for breast cancer: perceived risk, psychological well-being, and surveillance behavior. Monogr Natl Cancer Inst 1995 16: 171–176
Lerman C, Daly M, Masny A, et al. Attitudes about genetic testing for breast-ovarian cancer susceptibility. J Clin Oncol 1994 12: 843–850
Douma KF, Aaronson NK, Vasen HF, et al. Psychological distress and use of psychosocial support in familial adenomatous polyposis. Psychooncology 2010 19: 289–298
Lammens CR, Aaronson NK, Wagner A, et al. Genetic testing in Li-Fraumeni syndrome: uptake and psychosocial consequences. J Clin Oncol 2010 28: 3008–3014
Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002 52: 69–77
Zigmond AS, Snaith RP The hospital anxiety and depression scale. Acta Psychiatr Scand 1983 67: 361–370
Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 1997 27: 363–370
Canto MI, Goggins M, Yeo CJ, et al. Screening for pancreatic neoplasia in high-risk individuals: an EUS-based approach. Clin Gastroenterol Hepatol 2004 2: 606–621
de Graaf R, Ten Have M, van Gool C, et al. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol [published online ahead of print January 1, 2011]. doi: 10.1007/s00127-010-0334-8.
Acknowledgements
On behalf of a Dutch Research Group of Pancreatic Cancer Surveillance in High-Risk Individuals (in alphabetical order): Amsterdam Medical Center: Cora M. Aalfs, Marcel G. W. Dijkgraaf, Paul Fockens, Elsemieke M. Gimpel, Dirk J. Gouma, Jeanin E. van Hooft, C. Yung Nio, Theo A. M. van Os, and Ellen M. A. Smets; Erasmus Medical Center: Katharina Biermann, Marco J. Bruno, Henny van Duijl, Casper H. J. van Eijck, Femme Harinck, John J. Hermans, Nanda Krak, Jan-Werner Poley, and Anja Wagner; The Netherlands Cancer Institute, Antoni van Leeuwenhoek Hospital: Eveline M. A. Bleiker, Annemieke Cats, Irma Kluijt, Tanja Nagtegaal, Anja van Rens, Senno Verhoef; and University Medical Center Groningen: Hendrik M. van Dullemen and Rolf H. Sijmons.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first two authors contributed equally to this work.
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Harinck, F., Nagtegaal, T., Kluijt, I. et al. Feasibility of a pancreatic cancer surveillance program from a psychological point of view. Genet Med 13, 1015–1024 (2011). https://doi.org/10.1097/GIM.0b013e31822934f5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31822934f5
Keywords
This article is cited by
-
Long-term positive psychological outcomes in an Australian pancreatic cancer screening program
Familial Cancer (2020)
-
Health behaviours and beliefs in individuals with familial pancreatic cancer
Familial Cancer (2019)
-
Mindfulness-Based Interventions for Psoriasis: a Randomized Controlled Trial
Mindfulness (2019)
-
Familial pancreatic cancer—status quo
International Journal of Colorectal Disease (2014)
-
Factors influencing receptivity to future screening options for pancreatic cancer in those with and without pancreatic cancer family history
Hereditary Cancer in Clinical Practice (2012)