Abstract
Purpose: To determine the specific components of family history and personal characteristics related to disease perceptions about breast, colon, and ovarian cancers.
Methods: Baseline, cross-sectional data on 2,505 healthy women aged 35–65 years enrolled from 41 primary care practices in the cluster-randomized Family Healthware™ Impact Trial, assessed for detailed family history and perceived risk, perceived severity, worry, and perceived control over getting six common diseases including breast, colon, and ovarian cancers.
Results: Participants provided family history information on 41,841 total relatives. We found evidence of underreporting of paternal family history and lower perceived breast cancer risk with cancer in the paternal versus maternal lineage. We observed cancer-specific perceived risks and worry for individual family history elements and also found novel “spillover” effects where a family history of one cancer was associated with altered disease perceptions of another. Having a mother with early-onset breast or ovarian cancer was strongly associated with perceived risk of breast cancer. Age, parenthood, and affected lineage were associated with disease perceptions and ran counter to empiric risks.
Conclusions: Understanding patients' formulation of risk for multiple diseases is important for public health initiatives that seek to inform risk appraisal, influence disease perceptions, or match preventive interventions to existing risk perceptions.
Similar content being viewed by others
Main
Family medical history is a time-honored tool used by clinicians to assess patients' risk of developing common, chronic diseases and less common genetic disorders. An analysis of family history can inform a differential diagnosis, guide early detection and prevention strategies, and provide clinicians with a means to develop rapport with patients. In a study assessing laypeople's attitudes about hypothetical disease risk, a positive family history was more concerning than a positive genetic test result.1 Although people make connections between their own health and their relatives' medical experiences, qualitative studies have shown that patients' and clinicians' interpretations of family history often diverge.2–4 The challenge to motivate patients to adopt and maintain healthy behaviors and to obtain recommended screening could be assisted by a better understanding of patients' disease perceptions and how these correlate with key elements of their family history.
In recent years, there has been a strong interest in the development of automated tools to efficiently gather family history and provide an objective risk assessment.5–9 The rationale for systematic familial risk assessment includes tailoring of screening recommendations, promotion of healthy behaviors (diet, exercise, etc.), and referral for more comprehensive evaluation, potentially including genetic counseling and genetic testing. One such tool, Family Healthware™, is a Web-based program developed by the Centers for Disease Control and Prevention (CDC) that collects medical history about first- and second-degree relatives, assesses and stratifies into three tiers familial risk for coronary heart disease, stroke, diabetes, breast cancer (BC), colon cancer (CC), and ovarian cancer (OC), and provides tailored recommendations for screening tests and lifestyle changes.5 The CDC selected three academic centers to evaluate the clinical utility of Family Healthware in primary care settings through the Family Healthware Impact Trial (FHITr).10
Perceptions of risk, severity, worry, and control are core components of theories that explain health behavior including the Health Belief Model,11,12 the Theory of Planned Behavior,13 the Common-Sense Model,14 and Extended Parallel Process Model.15 Therefore, we measured these perceptions in the FHITr trial.10 Individuals with a family history of cancer have a greater likelihood of undergoing cancer screening and have stronger intentions to undergo future screening.16,17 But, although risk perception18,19 and worry20 and having a positive family history are predictive of BC and CC screening adherence, these characteristics do not correlate tightly, suggesting that additional factors are crucially important as well. We have shown that, for example, among a large primary care population of FHITr study participants, the familial risk of common diseases was related to their perceived risk and worry about these diseases, before any intervention.21 However, the high rates of optimistic bias22,23 that we observed also may represent some of the factors contributing to nonideal rates of screening adherence.
The specific family history elements underlying health behaviors are mostly unexamined except for BC, where having affected first-degree relatives and the number of affected relatives correlate with a greater likelihood of screening24,25 and uptake of prophylactic mastectomy.26 The current analyses examine that which particular elements of participants' detailed family histories of BC, OC, and CC are related to their perceptions about their own susceptibility, severity, worry, and control of these common cancers. Although most studies examine perceptions for single diseases, patients often must gauge perceptions of multiple diseases. Here, we measure health beliefs simultaneously for three types of cancer to better understand variability of beliefs based on components of family history and family structure.
MATERIALS AND METHODS
Overview of the Family Healthware Impact Trial
Complete details of Family Healthware design5 and FHITr study design and surveys10 have been published elsewhere and are briefly summarized here. Family Healthware is a self-administered, internet-based tool that collects data on medical history of first- and second-degree relatives, health behaviors, and screening tests. Software algorithms analyze and stratify familial risk into three tiers (strong, moderate, and weak) based on the number of relatives affected, their age at disease onset, their sex, the degrees of relationship, and the combinations of diseases in the family.27 A second set of algorithms generates personalized prevention messages based on risk level, reported health behaviors (physical activity, diet, smoking, alcohol use, and aspirin use), screening history, sex, and age.
The primary aim of the FHITr study was to evaluate the clinical utility of familial risk stratification and tailored messaging from Family Healthware using a practice based cluster-randomized design.10 Participants were healthy adults aged 35–65 years, patients of 187 primary care clinicians in 13 states. Exclusion criteria included a personal history of coronary heart disease, diabetes, stroke, or any cancer other than nonmelanoma skin cancer; inability to speak or read English; and known pregnancy. Protocols were approved by institutional review boards at CDC and all three research centers: NorthShore University HealthSystem (formerly Evanston Northwestern Health care), University of Michigan, and Case Western Reserve University in cooperation with the American Academy of Family Physicians' National Research Network. Informed consent was obtained from all subjects. Recruitment took place from November 2005 to March 2007.
Purpose of these analyses
The objective of this analysis was to determine the components of family history and personal characteristics (e.g., age and parenthood) that are most closely related to participants' perceptions of risk, severity, worry, and control for BC, OC, and CC. We used cross-sectional data measuring disease perceptions and family history information. The analysis was restricted to women as two of the three cancers studied primarily affect women. To limit complexity, analysis of family history elements pertaining to heart disease, stroke, and diabetes and analyses in males are relegated to future reports.
Items and instruments
All participants completed a baseline survey that included questions about perceived risk, perceived severity, worry, and perceived control (collectively called disease perceptions) related to developing each disease.28 Each group subsequently recorded their detailed family medical history using Family Healthware: at baseline in the intervention group and at the end of the follow-up approximately 6 months later in the control group. After the baseline survey, the control group received generic prevention messages, which are not expected to foster inquiries into their family history. Familial risk distributions were compared between the study arms and were not significantly different for any of the cancers, supporting the use of family history data assessed 6 months apart between groups. Therefore, for this analysis, we combined baseline survey and family history data from intervention and control participants.
Dependent variables
The disease perception measures constituted the dependent variables. These were assessed by single-item questions using 5-point Likert scales and measured the following constructs for each disease: Perceived risk: “Compared to most people your age and sex, what would you say your chances are for developing _____ [disease]? (Much lower than average to much higher than average)”22,23; Perceived severity: “Getting/Having _____ [disease] would be a very serious problem. (Strongly disagree to strongly agree)”; Worry: “During the past 4 weeks, how often have you thought about your chances of getting _____ [disease]? (Not at all to almost all the time)”29; Perceived control: “There's a lot I can do to prevent _____ [disease]. (Strongly disagree to strongly agree).”30
Independent variables
Current literature indicates that family history variables such as total number of relatives with BC, young age when affected, death from the disease, proximity of relationship, and total number of first-degree relatives with cancer are associated with disease perceptions.31–34 Others have found that young age and parenthood are associated with a greater uptake of risk-reducing breast surgery and genetic testing.35 We constructed a set of independent variables referred to as “family history elements” based on this literature, before undertaking any analyses. These family history elements are listed in Table 1 and include, for example, participant age, total number of relatives with a specific cancer (BC, OC, or CC), cancer on the maternal or paternal side (excluding the parent), and having a mother with early onset BC or early onset OC. Age was treated as a continuous variable in the models and was divided by 10 to aid interpretation of odds ratios (ORs). Age was dichotomized (35–40 vs. 41–65 years) as part of defining young versus old parents.
Statistical analysis
Baseline characteristics were compared across the two study arms using a clustered logistic regression model for categorical variables and a linear mixed effects model for continuous variables in an effort to evaluate whether the distributions were skewed between the groups. The analysis demonstrated that familial risk distributions between the study arms were not significantly different for any of the three cancers.
To model the 5-level ordinal dependent variables, proportional odds models for ordinal logistic regression were used. Models were fit using PROC GENMOD in SAS 9.1 (SAS, Cary, NC) with cumulative logit link function and multinomial distribution. For each dependent variable, the following procedure was used: (1) performed univariate tests for each independent variable; (2) the strongest predictor, based on χ2 statistics, is selected; (3) all other variables tested individually after adjustment for the first selected variable; (4) select the next strongest predictor; (5) repeat until no additional variables are significantly related to dependent variable (P < 0.05). These analyses are considered exploratory, and no adjustment was made for multiple comparisons.
RESULTS
Participant characteristics
Family Healthware was completed by 3,585 participants, of whom 70% were female. This report focuses on the 2,505 women who completed the baseline survey and Family Healthware, providing family history information on 41,841 total relatives. Participants' demographic characteristics were age, 35–65 years; mean age, 50.6 years; 91% white; 70% college educated; 75% married; and 50% indicated a household income of >$75,000.
Distribution of family history elements
The distribution of the individual family history elements is presented in Table 1. Most (85.5%) participants were aged 41–65 years. Approximately three quarters were mothers. Fifty-seven percent had at least one relative with BC, OC, or CC. Only rarely did participants report having three or more first-degree relatives with BC, OC, or CC or a combination of these cancers. Three percent reported having a mother who had early-onset BC or OC. When excluding their parents' cancer diagnoses, women were significantly more likely to report having cancer in their maternal versus paternal lineage (28.6% vs. 21.8%, P < 0.001). Covariate adjustment for total number of relatives reported had no impact on the lineage-related associations in any of the models.
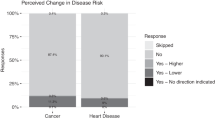
Family history elements and perceived risk of developing BC
This section illustrates the analysis of family history elements and perceived risk for BC. Similar analyses were performed for all four disease perceptions pertaining to each type of cancer. The distributions of risk perception for BC, OC, and CC are summarized in Table 2. We found that 18.3% of women perceived their risk of BC as higher or much higher than average, whereas 24.2% perceived their risk as lower or much lower than average. Many elements of family history were significantly related to perceived risk of BC (Table 3). The most significant predictor by far was having any first-degree relatives with BC (OR: 16.1; 95% confidence interval [CI]: 12.6–20.6 in univariate testing). The variables selected for inclusion in the final multivariable model (Table 3) were, in decreasing order of magnitude: any first-degree relatives with BC (OR: 5.95; 95% CI: 4.41–8.01), total number of relatives with BC (OR: 2.35; 95% CI: 2.03–2.72), mother with early onset BC or OC (OR: 2.42; 95% CI: 1.48–3.94), age per 10 years (OR: 0.80; 95% CI: 0.73–0.88), and cancer on the paternal side (OR: 0.80; 95% CI: 0.65–0.99).
Of note, increasing age and cancer on the paternal side decreased the odds of being in a higher perceived risk category. A shift from an OR for cancer on the paternal side of 1.29 in the univariate analyses to 0.80 in the multivariable model indicates the presence of confounding with other variables in the model. Further investigation revealed an interaction between the presence of cancer on the paternal side and the total number of relatives with BC (P = 0.002): in women with no cancer on the paternal side, total number of relatives with BC was associated with higher perceived risk of BC (OR: 2.78; 95% CI: 2.31–3.35); whereas in women with cancer on the paternal side, total number of relatives with BC was associated with lower perceived risk (OR: 0.69; 95% CI: 0.55–0.88).
Family history elements and disease perceptions for each type of cancer
Significant findings using multivariable models on associations of disease perceptions and family history elements are summarized in Table 4.
Age
Older age, independent of other aspects of family history, was associated with lower perceived risks for BC and OC, lower perceived severity for all three types of cancer, higher perceived ability to prevent CC, and decreased worry about developing BC.
Number of relatives and affected first-degree relatives
As expected, the total number of affected relatives and the presence of any first-degree relative with a particular cancer were significantly and independently associated with higher perceived risk for each of the three types of cancer. The three highest ORs found in this study pertained to having any first-degree relative with BC, OC, or CC and perceived risk for those specific cancers, signifying clinical relevance. Frequency of worrying about getting each type of cancer followed the same pattern as perceived risk, except that total number of relatives with OC was not significant. Total number of relatives with CC was associated with greater perceived control over preventing CC.
We also observed cross-correlations between different cancers—“spillover” effects—from a family history of a particular cancer to perceptions about another cancer. For example, the total number of relatives with BC was associated with a higher perceived risk of OC and decreased perceived ability to prevent OC. On the other hand, having a first-degree relative with BC was associated with lower worry about OC or CC. Having a first-degree relative with CC was associated with a higher perceived risk of OC. In contrast, the total number of relatives with OC was associated with lower perceived risk of CC.
As we had hypothesized based on the literature, having a mother with early-onset BC or OC was strongly associated with women's perceived risk of BC, independent of other family history characteristics. Having a mother with early BC or OC was also associated with decreased perceived severity of CC. When controlling for early-onset BC or OC in the mother, participant age and other aspects of family history, having a parent with cancer decreased the perceived severity of BC.
Parity
Older women with children compared with childless women reported more frequent worry about getting BC and CC, and younger women with children had decreased perceived ability to prevent BC. Total number of children was associated with lower perceived risk of OC.
DISCUSSION
Strengths and limitations
The prevalence of a family history of BC, CC, or OC in our cohort (57%) is similar to the prevalence of a family history of cancer (61% among female respondents) found in the large Prostate, Lung, Colorectal, and Ovarian screening trial.36 The FHITr study, with detailed family history from 2,505 women, comprises the largest reported data set in which to evaluate the specific components of family history, which are associated with disease perceptions. On the other hand, the sample primarily represents well-educated, well-to-do Midwestern women. Associations between risk perception and socioeconomic status have been inconsistent37; nonetheless, caution must be exercised in generalizing these results to other populations.
This was an exploratory analysis using multiple comparisons. Replication studies would be valuable as some of the observed associations could reflect false-positive/type I errors. We chose to report multivariate analyses, showing independent contributions of each variable in the model, thus potentially underestimating the effects of family history configurations that are less prevalent. The disease perception outcomes were quantitative data, obtained from single questionnaire items to minimize respondents' burden. Thus, potentially key explanatory variables related to individual interpretations of family history were not measured.
Effects of parental lineage on reporting and risk perception
Our findings indicate that knowledge of family history and risk perception each differ according to parental lineage. These findings have important implications about the analytic validity of family history and could influence the uptake of both family history-based referral and health recommendations.
The epidemiologic risk of BC associated with having affected second-degree relatives—those captured in this analysis—is similar for each lineage.38 Thus, known genetic factors do not explain these findings of differential family history reporting. Differential reporting of BC family history, with same directionality that we observed, has been seen in women's health clinic39 and high-risk settings.34,40 To our knowledge, this is the first study performed in a primary care setting, which reveals marked differences in family history reporting according to parental lineage, and is also the largest study highlighting this phenomenon.
Although the FHITr study did not assess the accuracy of family history self-reporting, published studies generally show high sensitivity and good specificity compared with “gold standards” (e.g., review of relatives' medical records or death certificates and interviews with relatives' physicians).41 However, such studies are prone to partial verification bias for several reasons such as limited verification of unaffected relatives' health status, exclusion of relatives with “don't know” status, or noninvestigation of deceased relatives.41
Our findings suggest that paternal family history is underreported (not that maternal family history is overreported). In fact, women reported an average of 0.39 “don't know” responses (of three maximum: BC, OC, and CC) per maternal relative and an average of 1.05 “don't know” responses per paternal relative (P < 0.001). Interestingly, the FHITr study found that men responded “don't know” on family history questioning more often than women (P < 0.001).10 Possibly, women's limitations on reporting paternal family history stem from a reliance on their father as a source of information. Less than ideal sensitivity in reported paternal family history could result in reduced accuracy of familial risk assessment and lost opportunities for cancer prevention strategies.
In addition to lineage-based reporting differences, we found a lower perceived risk for BC for a paternal versus maternal family history of cancer. Various lines of evidence suggest that there exists a prevalent belief that the risk of BC and OC is a maternally inherited trait. A significant proportion of individuals endorse the statement that “a daughter inherits more of her genes from her mother than her father,”42 reflecting a limited understanding of Mendelian inheritance on the part of the lay public. Furthermore, a study of women in a familial OC registry found that few realized the risk could pass through fathers.43
In the high-risk setting, completion of genetic testing among families with BRCA1/2 mutations is significantly lower in the paternal lineage.44 Although many gender differences likely contribute, this suggests that the significance of paternal inheritance of BC and OC risk is unclear to patients, even when autosomal dominant inheritance is evident from the genotype. This is borne out by knowledge assessment of index cases who have undergone genetic counseling and testing for BRCA1/2, showing that the risk of transmission by men and women and the parental origin of a positive result are poorly understood concepts.45 More than half of health professionals are unaware of the importance of paternal family history of BC and OC,46,47 and physicians' limited understanding might account for some of the relatively stronger effects that maternal lineage has on risk perception.40,48,49
Participant age and disease perceptions
Participant age was the characteristic most frequently found to have significant associations with disease perceptions. Although increasing age is the single most important risk factor for BC, OC, and many other cancers of adulthood,50 female FHITr participants' perceived risk of BC and OC ran counter to their age-related empiric risks. Increasing age was associated with lower worry for BC, lower perceived severity for all three cancers, and higher perceived control for CC.
Patients may recognize that as they age, their remaining lifetime risk diminishes; however, respondents were asked to rate their risks in comparison with most people of their age and sex. Perhaps older, unaffected women gauge their perceived risks in comparison with women they have known who were diagnosed with BC or OC and may feel that because they are cancer free, their own risk is lower. We must cautiously interpret our findings in terms of reflecting an effect of aging and instead may be observing a birth cohort effect. We note that other studies have also found that age is poorly recognized by older women as a cancer risk factor.51–54
Findings of agreement between medical and lay interpretations of family history
As expected, we found that having a family history of a particular cancer—both the total number of affected relatives and having any affected first-degree relative—is associated with a higher perceived risk of that cancer. This effect was particularly strong for having any affected first-degree relatives. The lack of significance found between disease-specific risk perception and either the total number of relatives with any cancer or the total number of first-degree relatives with any cancer further suggests that risk perceptions are generally cancer specific.
Our findings for BC and CC mirror those reported in the literature, where perceived risk is generally congruent with having a family history of that specific disease.55,56 BC has been the most widely studied cancer; several57–59 but not all53,60,61 studies have shown a relationship between a positive BC family history and higher perceived risk of BC. One study found that only 20% of individuals who had a sibling with CC cited heredity as a risk factor.62 Our findings parallel those reported in a large cross-sectional study of middle-aged adults registered with general practitioners in the United Kingdom, which found increasing levels of CC risk perception for having none, one, and two or more first-degree relatives with CC.37 Among the few studies examining family history elements and perceived risk, some found associations with total number of relatives with BC and perceived risk31–33 as we did, whereas others did not.53 Use of the model by Gail et al.,63 which limits BC family history collection to first-degree relatives and does not consider age of onset, imposes methodological limitations for many studies. One study using the model by Gail et al. found that perceived risk did not correlate with family history.61 This seems surprising in light of our finding that having any first-degree relatives with BC was the factor most strongly associated with BC risk perception.
In general, the literature has not addressed the relationship between risk perception and age of relatives' cancer diagnosis. One study did not find this association for BC.53 Our finding of increased perceived risk for women whose mother had early-onset BC or OC could indicate an awareness that early-onset cancer is a stronger risk factor. Alternatively, this finding may reflect participants' own young ages when their mother was affected: women who experience a mother's BC illness during their own childhood and puberty have been reported to have a higher perceived risk of BC.64
Most studies on OC family history and disease perceptions focus on high-risk families. One study of a racially diverse, population-based sample of BC and OC survivors and their unaffected female relatives found that perceived risk for OC was associated with a family history of OC and was greater than perceived risk of BC.33 Female FHITr participants' perceived risk of BC and OC did not differ, but worry was greater for BC than OC whereas perceived severity was greater for OC than BC.28 The risk conveyed by having a family history of OC seems to be understood by women who have had BRCA1 and BRCA2 genetic testing in an academic setting based on the greater uptake of prophylactic oophorectomy in those with a family history of OC,65 but the awareness in the general population has been unclear. The inverse relationship seen between the total number of children and perceived risk of OC correlates well with the known protective effect of parity on OC risk and the additional protective effect of increasing parity.66
Although we found agreement between medical and lay interpretations of family history, this does not necessarily mean that individuals' risk perceptions are based on beliefs about genes. Rather, having relatives affected by a certain cancer may provide individuals with an experience of cancer illness, which then leads to a personal sense of vulnerability.37
Perceptions less congruent with medical interpretations of family history
On the other hand, medical assessments of familial risk are not always congruent with patients' perceptions. A previous analysis found that many FHITr participants at strong or moderate familial risk did not perceive themselves to be at increased risk for BC (48%), CC (54%), or OC (70%).21 Although familial risk was not found to be related to perceived control for any of the six diseases,21 this study uncovered further associations for perceived control and severity. We suspect that “optimistic bias”22,23 and various of these associations may reflect unmeasured variables related to women's interpretation of their family cancer history—such as personal experiences of a relative's illness or its outcome or beliefs about causation and preventability of these cancers.3,4
Indeed, our findings may shed light on elements that contribute to a “personal sense of vulnerability” in a theoretical framework proposed following a systematic review and synthesis of qualitative studies of family history.2 This study found evidence of key constructs such as experience of a relative's illness, personalization of risk (including resemblance to relatives or whether the relative was of the same sex), and control of familial risk and then formulated and tested a model of familial risk perception3,4 drawing from Common Sense Model of Self–Regulation by Leventhal et al.14 We found several parallels, such as having an affected parent (lower perceived severity for BC), being a parent (higher BC and CC worry and lower perceived control of BC), lineage-specific effects (greater perceived severity of CC with cancer on the paternal side), and experience of a relative's illness (higher perceived control for CC and total number of relatives with CC). Comparative disease ratings may underlie some associations—when one type of cancer has a dramatic impact on a family, possibly other cancers may be perceived as less serious than the one that was actually experienced (e.g., lower perceived severity for CC with early-onset BC or OC in the mother).
“Spillover” effects
Spillover effects—perceptions of one cancer associated with family history of another—were seen between family history elements for BC and CC and a higher perceived risk of OC. In contrast, the total number of relatives with OC was associated with a lower perceived risk of CC. To our knowledge, this is the first report showing a relationship between family history of a specific cancer and either a higher perceived risk of a different cancer or a perceived protective effect.
Possibly, patients understand that in general, having a family history of one type of cancer raises the risk of a variety of other types of cancers67,68; however, this would not explain why we found specific associations but not others. Patients may associate abdominopelvic cancers with each other based on anatomic location, without fully appreciating the distinct causative factors of CC and OC. They may relate “hormonally driven” or “female” cancers (BC and OC) to each other. The news media or advertising campaigns69 may have conveyed information to participants about the connection between BC and OC via BRCA1 and BRCA2 mutations. We only detected this relationship in one direction (having a family history of OC was not found to be associated with a higher perceived risk of BC) but note that most such campaigns emphasize BC and not OC.
Implications for risk communication
Understanding the individual components that contribute to patients' disease perceptions has important implications for risk communication through automated family history tools, by health care providers, and via public health campaigns. The technological implications are nontrivial: Family Healthware was programmed not only to provide tailored messages5,70 but also to delineate which specific family history elements contributed to the risk level (e.g., the affected relatives and age of disease onset). Provision of this degree of detail back to the user required complex mapping of input data to messaging output, which contributed to a strain on computing resources. Whether this degree of individualization is useful in risk communication, in terms of aligning objective and perceived risk or fostering participation in screening programs, remains unclear.5
Finding that disease risk perceptions may not be congruent with objective risk estimates raises the specter of providing health advice that runs counter to or ignores the patient's perceptions and their personal sense of vulnerability. Some have suggested that public health should place a stronger emphasis on patient-centered approaches aimed at helping patients achieve informed choices instead of promoting in general the positive value of screening, preventive surgery, or genetic testing.70,71 The integration of patient- and provider-centered approaches (including provider competencies) has been advocated by the American Society of Preventive Oncology's Behavioral Oncology and Cancer Communication special interest group as a key research focus72 and is supported by our work.
The perception of risk is a core element—whether explicit or implicit—of nearly all theories of preventive behavior.73,74 This work identifies key areas for consideration in ongoing research in message design and tailored feedback used to encourage healthy behaviors. For example, female primary care patients seem to have a limited understanding of the relevance of their age or paternal family history for cancer susceptibility. This creates an opportunity for a public health education approach, which could influence the uptake of family history-based referral and lead to greater adherence to screening recommendations. The efficacy of tailored risk communication for influencing risk perception and screening adherence is largely unmapped territory and is ripe for research on family history elements. Putative barriers to screening, such as optimistic bias and perceptions about family history that are incongruent with medical interpretations, present unique opportunities to better understand patients' formulation of risk and ultimately to influence health behaviors. In future research, measurement of additional variables related to the personal meaning of family history and the use of qualitative methods, in the context of a theoretical framework, are needed to better understand patients' formulations of disease perceptions. Comparative disease ratings and spillover effects revealed in the FHITr study may become increasingly germane to the field of genomics, where simultaneous assessment of innumerable disease risks will become increasingly commonplace. Understanding the effects that one's family history has on multiple disease risks will be important for public health initiatives that seek to inform risk appraisal, to influence disease perceptions, or to match preventive interventions to existing perceptions of risk.
REFERENCES
Tarini BA, Singer D, Clark SJ, Davis MM . Parents' concern about their own and their children's genetic disease risk: potential effects of family history vs genetic test results. Arch Pediatr Adolesc Med 2008; 162: 1079–1083.
Walter FM, Emery J, Braithwaite D, Marteau TM . Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Ann Fam Med 2004; 2: 583–594.
Walter FM, Emery J . ‘Coming down the line’—patients' understanding of their family history of common chronic disease. Ann Fam Med 2005; 3: 405–414.
Walter FM, Emery J . Perceptions of family history across common diseases: a qualitative study in primary care. Fam Pract 2006; 23: 472–480.
Yoon PW, Scheuner MT, Jorgensen C, Khoury MJ . Developing Family Healthware, a family history screening tool to prevent common chronic diseases. Prev Chronic Dis 2009; 6: A33.
Carmona RH, Wattendorf DJ . Personalizing prevention: the U.S. Surgeon General's Family History Initiative. Am Fam Physician 2005; 71: 36, 39.
Acheson LS, Zyzanski SJ, Stange KC, Deptowicz A, Wiesner GL . Validation of a self-administered, computerized tool for collecting and displaying the family history of cancer. J Clin Oncol 2006; 24: 5395–5402.
Cohn WF, Ropka ME, Pelletier SL, et al. Health Heritage, a web-based tool for the collection and assessment of family health history: initial user experience and analytic validity. Public Health Genomics 2010; 13: 477–491.
Ozanne EM, Loberg A, Hughes S, et al. Identification and management of women at high risk for hereditary breast/ovarian cancer syndrome. Breast J 2009; 15: 155–162.
O'Neill SM, Rubinstein WS, Wang C, et al. Familial risk for common diseases in primary care: the Family Healthware Impact Trial. Am J Prev Med 2009; 36: 506–514.
Becker MH, editor. The health belief model and personal health behavior [serial (book, monograph)]. Health Educ Monogr. 1974; 2: 324–473.
Janz NK, Becker MH . The Health Belief model: a decade later. Health Educ Q 1984; 11: 1–47.
Ajzen I . The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211.
Leventhal H, Brissette I, Leventhal EA . The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behavior. New York, NY: Routledge, 2003; 42–65.
Witte K . Putting the fear back into fear appeals: the extended parallel process model [serial (book, monograph)]. Commun Monogr 1992; 59: 329–349.
Shah M, Zhu K, Palmer RC, Jatoi I, Shriver C, Wu H . Breast, colorectal, and skin cancer screening practices and family history of cancer in U.S. women. J Womens Health (Larchmt) 2007; 16: 526–534.
Holden D, Harris R, Porterfield D, et al. Enhancing the use and quality of colorectal cancer screening. Evidence Report/Technology Assessment No. 190. Prepared by the RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-2007-10056-1. Rockville, MD: Agency for Healthcare Research and Quality, AHRQ Publication No. 10-E-002, 2010.
Isaacs C, Peshkin BN, Schwartz M, DeMarco TA, Main D, Lerman C . Breast and ovarian cancer screening practices in healthy women with a strong family history of breast or ovarian cancer. Breast Cancer Res Treat 2002; 71: 103–112.
Helzlsouer KJ, Ford DE, Hayward RS, Midzenski M, Perry H . Perceived risk of cancer and practice of cancer prevention behaviors among employees in an oncology center. Prev Med 1994; 23: 302–308.
Hay JL, McCaul KD, Magnan RE . Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Prev Med 2006; 42: 401–408.
Acheson LS, Wang C, Zyzanski SJ, et al. Family history and perceptions about risk and prevention for chronic diseases in primary care: a report from the Family Healthware Impact Trial. Genet Med 2010; 12: 212–218.
Weinstein ND . Unrealistic optimism about susceptibility to health problems. J Behav Med 1982; 5: 441–460.
Weinstein N . Unrealistic optimism about future life events. J Pers Soc Psychol 1980; 39: 806–820.
McCaul KD, Branstetter AD, Schroeder DM, Glasgow RE . What is the relationship between breast cancer risk and mammography screening? A meta-analytic review. Health Psychol 1996; 15: 423–429.
Antill YC, Reynolds J, Young MA, et al. Screening behavior in women at increased familial risk for breast cancer. Fam Cancer 2006; 5: 359–368.
Antill Y, Reynolds J, Young MA, et al. Risk-reducing surgery in women with familial susceptibility for breast and/or ovarian cancer. Eur J Cancer 2006; 42: 621–628.
Scheuner MT, Wang SJ, Raffel LJ, Larabell SK, Rotter JI . Family history: a comprehensive genetic risk assessment method for the chronic conditions of adulthood. Am J Med Genet 1997; 71: 315–324.
Wang C, O'Neill SM, Rothrock N, et al. Comparison of risk perceptions and beliefs across common chronic diseases. Prev Med 2009; 48: 197–202.
Anderson MR, Smith R, Meischke H, Bowen D, Urban N . Breast cancer worry and mammography use by women with and without a family history in a population-based sample. Cancer Epidemiol Biomarkers Prev 2003; 12: 314–320.
Witte K, Cameron KA, McKeon JK, Berkowitz JM . Predicting risk behaviors: development and validation of a diagnostic scale. J Health Commun 1996; 1: 317–341.
Lipkus IM, Rimer BK, Strigo TS . Relationships among objective and subjective risk for breast cancer and mammography stages of change. Cancer Epidemiol Biomarkers Prev 1996; 5: 1005–1011.
Gilpin CA, Carson N, Hunter AG . A preliminary validation of a family history assessment form to select women at risk for breast or ovarian cancer for referral to a genetics center. Clin Genet 2000; 58: 299–308.
Mellon S, Gold R, Janisse J, et al. Risk perception and cancer worries in families at increased risk of familial breast/ovarian cancer. Psychooncology 2008; 17: 756–766.
Green J, Richards M, Murton F, Statham H, Hallowell N . Family Communications and genetic counseling: the case of hereditary breast and ovarian cancer. J Genet Couns 1997; 6: 45–60.
Meijers-Heijboer EJ, Verhoog LC, Brekelmans CT, et al. Presymptomatic DNA testing and prophylactic surgery in families with a BRCA1 or BRCA2 mutation. Lancet 2000; 355: 2015–2020.
Pinsky PF, Kramer BS, Reding D, Buys S . Reported family history of cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Epidemiol 2003; 157: 792–799.
Robb KA, Miles A, Wardle J . Demographic and psychosocial factors associated with perceived risk for colorectal cancer. Cancer Epidemiol Biomarkers Prev 2004; 13: 366–372.
Couto E, Hemminki K . Estimates of heritable and environmental components of familial breast cancer using family history information. Br J Cancer 2007; 96: 1740–1742.
Quillin JM, Ramakrishnan V, Borzelleca J, Bodurtha J, Bowen D, Baer WD . Paternal relatives and family history of breast cancer. Am J Prev Med 2006; 31: 265–268.
Tinley ST, Lynch HT . Integration of family history and medical management of patients with hereditary cancers. Cancer 1999; 86: 2525–2532.
Qureshi N, Wilson B, Santaguida P, et al. Family history and improving health. Evid Rep Technol Assess (Full Rep) 2009: 1–135.
Richards M, Ponder M . Lay understanding of genetics: a test of a hypothesis. J Med Genet 1996; 33: 1032–1036.
Green J, Murton F, Statham H . Psychosocial issues raised by a familial ovarian cancer register. J Med Genet 1993; 30: 575–579.
Finlay E, Stopfer JE, Burlingame E, et al. Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test 2008; 12: 81–91.
Blandy C, Chabal F, Stoppa-Lyonnet D, Julian-Reynier C . Testing participation in BRCA1/2-positive families: initiator role of index cases. Genet Test 2003; 7: 225–233.
Mouchawar J, Klein CE, Mullineaux L . Colorado family physicians' knowledge of hereditary breast cancer and related practice. J Cancer Educ 2001; 16: 33–37.
Yong MC, Zhou XJ, Lee SC . The importance of paternal family history in hereditary breast cancer is underappreciated by health care professionals. Oncology 2003; 64: 220–226.
Burke W, Culver J, Pinsky L, et al. Genetic assessment of breast cancer risk in primary care practice. Am J Med Genet A 2009; 149A: 349–356.
Culver JO, Bowen DJ, Reynolds SE, Pinsky LE, Press N, Burke W . Breast cancer risk communication: assessment of primary care physicians by standardized patients. Genet Med 2009; 11: 735–741.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ . Cancer statistics, 2009. CA Cancer J Clin 2009; 59: 225–249.
Gerend MA, Aiken LS, West SG, Erchull MJ . Beyond medical risk: investigating the psychological factors underlying women's perceptions of susceptibility to breast cancer, heart disease, and osteoporosis. Health Psychol 2004; 23: 247–258.
Aiken LS, Fenaughty AM, West SG, Johnson JJ, Luckett TL . Perceived determinants of risk for breast cancer and the relations among objective risk, perceived risk, and screening behavior over time. Womens Health 1995; 1: 27–50.
Audrain J, Lerman C, Rimer B, Cella D, Steffens R, Gomez-Caminero A . Awareness of heightened breast cancer risk among first-degree relatives of recently diagnosed breast cancer patients. The High Risk Breast Cancer Consortium. Cancer Epidemiol Biomarkers Prev 1995; 4: 561–565.
Breslow RA, Sorkin JD, Frey CM, Kessler LG . Americans' knowledge of cancer risk and survival. Prev Med 1997; 26: 170–177.
Vernon SW . Risk perception and risk communication for cancer screening behaviors: a review. J Natl Cancer Inst Monogr 1999: 101–119.
Vernon SW, Myers RE, Tilley BC, Li S . Factors associated with perceived risk in automotive employees at increased risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev 2001; 10: 35–43.
Zakowski SG, Valdimarsdottir HB, Bovbjerg DH, et al. Predictors of intrusive thoughts and avoidance in women with family histories of breast cancer. Ann Behav Med 1998; 19: 362–369.
Mouchawar J, Byers T, Cutter G, Dignan M, Michael S . A study of the relationship between family history of breast cancer and knowledge of breast cancer genetic testing prerequisites. Cancer Detect Prev 1999; 23: 22–30.
Erblich J, Bovbjerg DH, Norman C, Valdimarsdottir HB, Montgomery GH . It won't happen to me: lower perception of heart disease risk among women with family histories of breast cancer. Prev Med 2000; 31: 714–721.
Hughes C, Lerman C, Lustbader E . Ethnic differences in risk perception among women at increased risk for breast cancer. Breast Cancer Res Treat 1996; 40: 25–35.
Daly MB, Lerman CL, Ross E, Schwartz MD, Sands CB, Masny A . Gail model breast cancer risk components are poor predictors of risk perception and screening behavior. Breast Cancer Res Treat 1996; 41: 59–70.
Blalock SJ, DeVellis BM, Afifi RA, Sandler RS . Risk perceptions and participation in colorectal cancer screening. Health Psychol 1990; 9: 792–806.
Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 1989; 81: 1879–1886.
van OI, Meijers-Heijboer H, Duivenvoorden HJ, et al. Experience of parental cancer in childhood is a risk factor for psychological distress during genetic cancer susceptibility testing. Ann Oncol 2006; 17: 1090–1095.
Uyei A, Peterson SK, Erlichman J, et al. Association between clinical characteristics and risk-reduction interventions in women who underwent BRCA1 and BRCA2 testing: a single-institution study. Cancer 2006; 107: 2745–2751.
Whittemore AS, Harris R, Itnyre J . Characteristics relating to ovarian cancer risk: collaborative analysis of 12 US case-control studies. II. Invasive epithelial ovarian cancers in white women. Collaborative Ovarian Cancer Group. Am J Epidemiol 1992; 136: 1184–1203.
Amundadottir LT, Thorvaldsson S, Gudbjartsson DF, et al. Cancer as a complex phenotype: pattern of cancer distribution within and beyond the nuclear family. PLoS Med 2004; 1: e65.
Gerend MA, Aiken LS, West SG . Personality factors in older women's perceived susceptibility to diseases of aging. J Pers 2004; 72: 243–270.
Mouchawar J, Hensley-Alford S, Laurion S, et al. Impact of direct-to-consumer advertising for hereditary breast cancer testing on genetic services at a managed care organization: a naturally-occurring experiment. Genet Med 2005; 7: 191–197.
Edwards A, Unigwe S, Elwyn G, Hood K . Effects of communicating individual risks in screening programmes: Cochrane systematic review. BMJ 2003; 327: 703–709.
Braithwaite D, Sutton S, Smithson WH, Emery J . Internet-based risk assessment and decision support for the management of familial cancer in primary care: a survey of GPs' attitudes and intentions. Fam Pract 2002; 19: 587–590.
Kiviniemi MT, Hay JL, James AS, et al. Decision making about cancer screening: an assessment of the state of the science and a suggested research agenda from the ASPO Behavioral Oncology and Cancer Communication Special Interest Group. Cancer Epidemiol Biomarkers Prev 2009; 18: 3133–3137.
Sulls J, Wallston K . Social psychological foundations of health and illness. In: Tennen H, Affleck G, editors. Health pyschology and behavioral medicine. Malden, MA: Blackwell Publishing, 2003.
Glanz K, Rimer B, Lewis F . Health behavior and health education: theory, research and practice, 3rd ed. San Francisco, CA: Jossey-Bass, Inc, 2002.
Acknowledgements
The Family Healthware™ Impact Trial (FHITr) was supported through cooperative agreements between the Centers for Disease Control and the Association for Prevention Teaching and Research Grant ENH-U50/CCU300860 TS-1216 and the American Association of Medical Colleges Grant UM-U36/CCU319276 MM-0789 and CWR-U36/CCU319276 MM0630.
The Family Healthware Impact Trial (FHITr) Group consists of the collaborators listed below:
From the Centers for Disease Control and Prevention: Paula W. Yoon, ScD, MPH; Rodolfo Valdez, PhD; Margie Irizarry-De La Cruz, MPH; Muin J. Khoury, MD, PhD; Cynthia Jorgensen, DrPH
From the Veterans Administration Greater Los Angeles Healthcare System: Maren T. Scheuner, MD, MPH
From NorthShore University HealthSystem, Evanston, Illinois: Wendy S. Rubinstein, MD, PhD, Co-Principal Investigator; Suzanne M. O'Neill, MA, MS, PhD, Co-Principal Investigator; Nan Rothrock, PhD; Jennifer L. Beaumont, MS; Shaheen Khan, MS, MBA, MPH; Dawood Ali, MS
From the University of Michigan: Mack T. Ruffin IV, MD, MPH, Principal Investigator; Donald Nease, MD
From Case Western Reserve University, University Hospitals Case Medical Center: Louise S. Acheson, MD, MS, Principal Investigator; Stephen J. Zyzanski, PhD; Georgia L. Wiesner, MD; James Werner, PhD
From Boston University School of Public Health: Catharine Wang, PhD, MSc
From the American Academy of Family Physicians' National Research Network: Wilson D. Pace, MD, Principal Investigator; James M. Galliher, PhD; Elias Brandt, BS, BA
From the University of Illinois at Chicago: Erin J. Starzyk, MPH
From the University of Rochester: Robert Gramling, MD, DSc
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rubinstein, W., O'Neill, S., Rothrock, N. et al. Components of family history associated with women's disease perceptions for cancer: A report from the Family Healthware™ Impact Trial. Genet Med 13, 52–62 (2011). https://doi.org/10.1097/GIM.0b013e3181fbe485
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181fbe485
Keywords
This article is cited by
-
The Effects of Personalizing Colorectal Cancer Risk Communication on Risk Perceptions and Health Behavior Intentions: a Randomized Trial of Average-Risk Adults
Journal of Cancer Education (2021)
-
Effectiveness of interventions to identify and manage patients with familial cancer risk in primary care: a systematic review
Journal of Community Genetics (2020)
-
Heart disease versus cancer: understanding perceptions of population prevalence and personal risk
Journal of Behavioral Medicine (2017)
-
Lay Awareness of the Relationship between Age and Cancer Risk
Annals of Behavioral Medicine (2017)
-
Breast cancer epidemic in the early twenty-first century: evaluation of risk factors, cumulative questionnaires and recommendations for preventive measures
Tumor Biology (2016)