Abstract
Purpose: Mutations in the CDKL5 gene have been associated with an X-linked dominant early infantile epileptic encephalopathy-2. The clinical presentation is usually of severe encephalopathy with refractory seizures and Rett syndrome (RTT)-like phenotype. We attempted to assess the role of mosaic intragenic copy number variation in CDKL5.
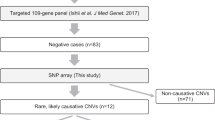
Methods: We have used comparative genomic hybridization with a custom-designed clinical oligonucleotide array targeting exons of selected disease and candidate genes, including CDKL5.
Results: We have identified mosaic exonic deletions of CDKL5 in one male and two females with developmental delay and medically intractable seizures. These three mosaic changes represent 60% of all deletions detected in 12,000 patients analyzed by array comparative genomic hybridization and involving the exonic portion of CDKL5.
Conclusion: We report the first case of an exonic deletion of CDKL5 in a male and emphasize the importance of underappreciated mosaic exonic copy number variation in patients with early-onset seizures and RTT-like features of both genders.
Similar content being viewed by others
Main
The cyclin-dependent kinase-like 5 (CDKL5) gene (also known as seronine-threonine kinase 9) encodes a protein of 1030 amino acids with highly conserved serine-threonine kinase domain in the N-terminal region and a large C-terminal region involved in either the catalytic activity or the subcellular localization.1 CDKL5 is particularly expressed in the brain and has homology to the mitogen-activated protein kinase and CDK families.2
Mutations in CDKL5 (OMIM# 300203) are X-linked dominant and have been described in females with severe neurodevelopmental disorders characterized by early-onset seizures, infantile spasms and severe psychomotor impairments, and Rett Syndrome (RTT)-like phenotypes.3 The phenotypic resemblance to Rett syndrome is likely related to similar function of the CDKL5 and MeCP2 proteins in the molecular pathways and regional pattern of expression during neurodevelopment.4,5 Recently, copy number variations (CNVs) involving the CDKL5 gene have been reported in girls with severe epilepsy and a RTT-like phenotype. The increasing availability of array comparative genomic hybridization (CGH) has led to several publications describing different deletions in CDKL5 in females.6–9 These data emphasize that deletion CNVs involving CDKL5 are more common than first appreciated, especially in females.
CDKL5 mutations have been found very rarely in males, suggesting that nullisomy might be incompatible with life. To date, only two frameshifts and four missense mutations have been reported in males with severe encephalopathy and early-onset intractable epilepsy.10–13 In addition, an approximately 2.8-Mb deletion involving CDKL5 and 15 other genes has been reported in a boy with severe encephalopathy, tetralogy of Fallot, and bilateral cataracts.14 Also, an approximately 136-kb deletion disrupting exons 17–20 of CDKL5 and the RS1 and PPEF1 genes has been described in a male with retinoschisis and epilepsy.15
We report in this study the first cases of mosaic exonic deletions of CDKL5 identified in a boy with severe developmental delay and refractory seizures (Patient 1), in a girl with Rett-like phenotype (Patient 2), and in a girl with severe developmental delay and intractable seizures (Patient 3). Our report emphasizes the importance of array CGH as a diagnostic tool in children with developmental delay and seizures. Moreover, it sheds light on the previously underestimated importance of CDKL5 mosaic changes in males with refractory early-onset seizures and developmental delay, and in females with variable phenotype due to a combination of mosaicism and X inactivation.
MATERIALS AND METHODS
Clinical description
We received DNA samples from probands with epilepsy and their family members after obtaining their informed consent, using protocols approved by the Institutional Review Boards for Human Subject Research at Institute of Mother and Child and Baylor College of Medicine (BCM).
Patient 1
The proband is a 15-month-old male with a history of severe developmental delay with possible regression. Family history is negative for mental retardation and seizures. He was the product of a full-term gestation, born to a 35-year-old G3, P2, mother who had good prenatal care. Pregnancy complications included pneumonia during the 7th month of pregnancy and treated maternal hypothyroidism. The patient was born by a C section: the mother had two prior C sections. Birth weight was 4030 g, birth length 49.5 cm, and occipitofrontal circumference was normal. At the age of 6 weeks, he developed focal seizures. The seizures gradually worsened up to 10–20 seizures per day with no good response to multiple antiseizure medications, including phenobarbital, levetiracetam, lamotrigine, folinic acid, and pyridoxine sulfate. Currently, the patient is on a ketogenic diet, on which he has 1–2 seizures per day lasting 10 seconds in duration. Significant findings in this patient's interictal electroencephalography (EEG) include abnormal slowing of the occipital dominant rhythm, multifocal sharp waves, and left frontal and central sharp waves. Seizures captured during video EEG monitoring were classified as complex partial seizures with secondary generalization. He used to spontaneously grasp objects at the age of 6 months but has since lost this developmental milestone. On physical examination at the age of 15 months, the boy was nondysmorphic, very floppy, hypotonic with poor deep tendon reflexes. He had severe motor and speech delay as he still did not sit, did not pass toys from hand to hand, and was only able to roll over and track with his eyes. In addition, there was also delay in his speech development; the patient could not speak any words and was only able to make sounds. Brain magnetic resonance imaging (MRI) and positron emission tomography-computed tomography scans were normal.
Patient 2
The proband is a 2-year-old girl, who was referred to the genetics clinic due to psychomotor retardation and epilepsy. She is the first child of a nonconsanguineous 36-year-old mother and a 41-year-old father with no contributing family history. The pregnancy was complicated by upper respiratory infection at 20 weeks of gestation. The proband was delivered without complications at 39 weeks of gestation with normal body parameters: birth weight 3900 g, birth length 56 cm, and occipitofrontal circumference 37 cm. Apgar scores at 1 and 5 minutes were 10/10 points. Treatment with Gancyclovir was given because of human cytomegalovirus identification in urine. The patient presented with focal clonic and tonic seizures at the age of 7 weeks, and over time, her clinical seizure pattern evolved into complex partial seizures and myoclonic seizures. The interictal EEG demonstrated a slow occipital dominant rhythm for age, spike waves in the left centrotemporal region and diffuse sharp waves and spikes in the right centrotemporal region at 2 years of age and multifocal spikes appeared thereafter in sleep. Therefore, this patient's epilepsy was classified as a medically intractable symptomatic mixed epilepsy syndrome. On physical examination, she had global hypotonia and severe psychomotor and speech delay. She was unable to sit and walk and did not control her head. She had “amimic” face, poor eye fixation, open mouth, protruding tongue, widely spaced teeth, full cheeks, and limited hand use with long tapering fingers. Hand stereotypies were periodically observed. Brain MRI was normal.
Patient 3
This 9-year-old girl was referred to the neurogenetics clinic because of severe intellectual disability, autism, and intractable seizures, which were diagnosed at age 16 months but were probably present since birth. Family history was noncontributory. She was born after an unremarkable pregnancy and was delivered by a repeat C section. The EEG showed nearly continuous bifrontal synchronous slow waves, frequent bursts of high-voltage mixed multifocal sharp and slow activity, and occasional generalized spikes. Previous treatments for her epilepsy included oxcarbazepine, felbamate, levetiracetam, diazepam and clonazepam, and vagus nerve stimulation, none of which controlled her seizures. Therefore, this patient's epilepsy was classified as a treatment-refractory symptomatic epilepsy syndrome. Head computed tomography scan and brain MRI were normal. On physical examination, head circumference was +1 SD above the mean for age, whereas the weight and length were within the normal limits. Neurologic examination in infancy was significant for decreased alertness, inability to follow commands, mild hypertonia mainly in her legs, and hyporeflexia. At the time, the encephalopathy was attributed to the high doses of antiseizure medications that she was receiving, as it had not been previously noted. At 9 years of age, she had the developmental skills of a 1-year-old child. She could only babble, walk, and run. She recently had surgery for G-tube placement due to dysphagia. Formal psychological evaluation at age 5 years resulted in a diagnosis of autism.
Methods
Microarray CGH
Genomic DNA was extracted from peripheral blood cells using a Puregene DNA Blood Kit (Qiagen, Gentra Systems, Minneapolis, MN) according to the manufacturer's protocol.
Custom-designed exon-targeted clinical array CGH was performed using 180K V8.0 OLIGO (Patient 1) and 105K V7.4 OLIGO (Patients 2 and 3) microarrays designed by Medical Genetics Laboratories at BCM (http://www.bcm.edu/geneticlabs/cma/tables.html) in cooperation with Department of Medical Genetics at Institute of Mother and Child and manufactured by Agilent Technology (Santa Clara, CA). V7.4 OLIGO (105K) covering the whole genome at an average resolution of 30 kb with increased coverage (10–20 kb) at known disease loci16 has the additional exon coverage for selected 24 genes (including CDKL5), with 10–15 oligos per exon. V8.0 OLIGO (180K) has similar genome-wide coverage and the exon coverage for over 1700 genes (including CDKL5), with on an average 4.2 oligos per exon and intronic gaps no larger than 10 kb. Digestion, labeling, and hybridization were performed following the manufacturer's instructions. The BCM web-based software platform was used for genomic copy number analysis.
Multiplex ligation-dependent probe amplification
Multiplex ligation-dependent probe amplification (MLPA) experiments (Patients 1 and 2) were performed according to the manufacturer's instruction with the kits P015 and P189 (MRC Holland) in the thermal cycler (Applied Biosystems, Foster City, CA). Both kits provide probes for the CDKL5 exons and control fragments for X chromosome and autosomes. Information regarding the probe sequence and ligation sites can be obtained at www.mlpa.com. Probes were analyzed using ABI3100 sequencer with size standard GeneScan 500 Rox (Applied Biosystems). Data analysis was done with GeneMarker v8.1 software from Softgenetics.
Fluorescence in situ hybridization analysis
Confirmatory fluorescence in situ hybridization (FISH) analyses were performed in the phytohemagglutinin-stimulated peripheral blood lymphocytes using standard procedures in Patient 1 with the bacterial artificial chromosome (BAC) clones RP11-558P14, specific for chromosome Xp22.13, and RP11-1017D24, specific for chromosome 3p26.1, and in Patient 3 with the BAC clone RP11-106N3, specific for chromosome Xp22.13. In Patient 3, FISH analysis was performed also on all nucleated cells from blood smears.
Long-range polymerase chain reaction and sequence analysis
Genomic sequence based on the oligonucleotide coordinates from the array CGH experiment was downloaded from the University of California Santa Cruz (UCSC) genome browser (Build 36, March 2006, [hg18]) and assembled using Sequencher software (Gene Codes Corporation, Ann Arbor, MI). Long-range polymerase chain reaction (LR-PCR) was performed in Patients 1 and 3 to amplify the junction fragments of the deletions according to manufacturer's instructions (Takara Bio Inc., Japan). PCR products were visualized on 1% agarose gel, purified with the ExoSAP Clean-up kit (USB Corp., Cleveland, OH), and sequenced (Lone Star, Houston, TX).
Real-time quantitative PCR
Real-time quantitative PCR was performed using primers specific for exon 4 of CDKL5 and β-tubulin (reference gene) and SYBR Green Master Mix (Patient 2).
X-inactivation studies
X-inactivation studies were performed as described previously.8
RESULTS
The three exonic mosaic deletions harboring CDKL5 have been found in more than 12,000 patients screened in the Medical Genetics Laboratories at BCM using chromosomal microarray analysis (CMA) Versions 7 OLIGO and 8 OLIGO, in which CDKL5 has been exon targeted. In this cohort, we also identified two nonmosaic constitutional deletion CNVs involving exons of CDKL5. Our collection of subjects referred for CMA includes mostly children with various combinations of developmental delay/mental retardation, autism, birth defects, and rarely isolated seizures. In this cohort, V7 OLIGO yielded a 15.4% detection rate.
Patient 1
CMA (V8.0 OLIGO) revealed a loss in copy number in the Xp22.13 region spanning a minimum of 105-kb and a maximum of 128-kb interval and encompassing exons 1–3 of the CDKL5 gene. The distal breakpoint was mapped between 18,331,857 and 18,343,025 and the proximal breakpoint between 18,447,902 and 18,460,326. The Cy5/Cy3 fluorescence log 2 ratios of the interrogating probes indicated a mosaicism (Fig. 1B). Additionally, CMA analysis revealed a 765-kb gain in copy number in 3p26.1.
Schematic representation of three exonic CNV deletions involving CDKL5 (A). CMA Versions 7 OLIGO and 8 OLIGO have 11 and 6 oligos per CDKL5 exon, respectively. The array CGH (aCGH) plots (B–D) and results of confirmatory studies using MLPA in Patients 1 and 2 (B, C) and FISH in Patient 3 (D). Note the log 2 ratios in array CGH plots and peak ratios in MLPA results, indicating mosaicism.
FISH studies confirmed the deletion in Xp22.13 and the duplication in 3p26.1 and revealed that deletion in Xp22.13 was present in 24% of cells analyzed. Parental FISH analyses revealed that the deletion of Xp22.13 occurred de novo; the duplication 3p26.1 was inherited from the phenotypically normal father and, therefore, most likely represents nonpathogenic familial copy number variant.
A junction fragment of the deletion was amplified using LR-PCR with primers F: GTGAGTGCATACACTGGCTACTGCATCATA and R: CCCTAGAACTACTTGAGCATGGTTTACAGAAGG and sequenced. The distal breakpoint was mapped at 18,334,623 and proximal at 18,449,201, thus the deletion is 114,579 bp in size. DNA sequence analysis of PCR product that spans the junction revealed no microhomology. The distal deletion breakpoint mapped within unique sequence, and the proximal deletion breakpoint mapped within a LINE element type L1MB5. The deletion removed exons 1–3 in both isoforms of CDKL5.
The MLPA analysis with a SALSA kit P189 (CDKL5, NTNG1, and ARX genes) showed an approximately 23% decreased signal for probes specific for exons 1–3 of the CDKL5 gene and confirmed the mosaicism detected by array CGH and FISH analyses (Fig. 1B).
Patient 2
CMA (V7.4 OLIGO) revealed a loss in copy number in the Xp22.13 region spanning a minimum of 1-kb and a maximum of 11-kb interval and encompassing only exon 4 of the CDKL5 gene (included in Ref. 17). The distal breakpoint was mapped between 18,492,177 and 18,492,235 and the proximal breakpoint between 18,492,821 and 18,503,003 (Fig. 1C). Similarly, the Cy3/Cy5 fluorescence log 2 ratios indicated a mosaicism. The MLPA analysis using SALSA kit P189 (CDKL5, NTNG1, and ARX genes) showed an approximately 35% decrease of signal intensities for probes specific for exon 4 of CDKL5 gene, supporting the finding of a mosaicism (Fig. 1C). The presence of this deletion was also confirmed by real-time quantitative PCR (data not shown). Parental real-time quantitative PCR analyses revealed that the deletion occurred de novo. As predicted by conceptual translation, this deletion results in a premature truncation of CDKL5. The patient had a random X-inactivation pattern.
Patient 3
CMA (V7.4 OLIGO) revealed a loss in copy number in the Xp22.13 region spanning a minimum of 172-kb and a maximum of 178-kb interval and encompassing exons 1–15 of the CDKL5 gene. The distal breakpoint was mapped between 18,369,992 and 18,370,016 and the proximal breakpoint between 18,541,598 and 18,547,638. The Cy5/Cy3 fluorescence log 2 ratios of the interrogating probes also indicated a mosaicism (Fig. 1D).
FISH studies revealed that deletion in Xp22.13 is present in 30% (59/200) of stimulated lymphocytes T and in 28% (56/200) of cells from the whole blood smear. Parental FISH analyses showed that this deletion occurred de novo (Fig. 1D). The patient had a random X-inactivation pattern.
A junction fragment of the deletion was amplified using LR-PCR with primers F: CCTCCAGACACCTTTAATCTGCTCGAAGTAT and R: GACACTAGGTTCCTATAGCCGGGAAGAATC and sequenced. The distal breakpoint was mapped at 18,365,835 and the proximal breakpoint at 18,545,735, thus the deletion is 179,900 bp in size. DNA sequence analysis of the junction fragment revealed a “TC” microhomology.
DISCUSSION
More than 50 missense, nonsense, and frameshift point mutations have been described in CDKL5.18 Mutations affecting the aminoterminal domain of CDKL5 are thought to result in a more severe phenotype in infancy followed by myoclonic epilepsy. The vast majority of these mutations have been identified in females manifesting three phases in epilepsy phenotype: frequent early-onset seizures starting before the age of 3 months, followed by epileptic encephalopathy, and later by myoclonic refracted epilepsy.19 The phenotypes of girls with deletion CNVs disrupting CDKL5 have been demonstrated to be very similar to those with point mutations and include early-onset epilepsy refractory to drug treatment. CDKL5 mutations or deletions in males are thought to be lethal, and there are only a handful of reported surviving cases with a more severe phenotype, including severe intellectual disability and intractable seizures, suggesting that some amino acid changes of CDKL5 may be tolerated.10,12 Two larger sized genomic deletions disrupting CDKL5 have been published in males with severe encephalopathy and epilepsy.10,12
In all three presented cases, the deletions disrupted only CDKL5, thus enabling their better correlation with the phenotypic features. The mosaic deletions of exons 1–3 in Patient 1 and exons 1–15 in Patient 3 likely result in loss of transcription start sites of both CDKL5 isoforms, whereas removal of exon 4 in Patient 2 is predicted by conceptual translation to cause protein truncation and its subsequent removal by RNA surveillance mechanisms, such as nonsense-mediated decay. The residual CDKL5 protein activity is likely insufficient for the normal function of the proposed MeCP2-CDKL5 pathway and is responsible for the epileptic phenotype. In general, a genotype-phenotype correlation in patients with CDKL5 deletion or mutation is difficult, especially in females, in whom the ratio of deletion mosaicisms and X-inactivation patterns can significantly vary between the brain and the peripheral blood. Supporting this notion, Erez et al.8 identified random and extremely skewed X-inactivation patterns in two females with CDKL5 deletions who despite the skewing had similar phenotypes, suggesting haploinsufficiency of CDKL5 in the brain. In addition, different translation initiation sites associated with other ATG codons can lead to alternative CDKL5 peptides, which can have either a dominant negative effect or partially rescue the phenotype. 8 Specifically for Patient 2, it is hard to assess the direct consequences of CDKL5 deletion as the patient was also diagnosed with congenital human cytomegalovirus infection, which may also cause seizures and developmental delay. However, the patient was treated with Gancyclovir immediately after birth, and brain imaging did not show any calcifications, suggesting that his seizures and developmental delay most probably result from CDKL5 deletion.
DNA sequence analysis of the junction fragment in Patient 3 revealed two base pair (TC) microhomology. Exonic rearrangements, such as exon shuffling, have been recently shown to result from DNA replication error mechanisms fork stalling and template switching/microhomology-mediated break-induced replication,20 thus are expected to occur in early postzygotic stage and be mosaic. In support of this hypothesis, Vanneste et al.21 have demonstrated a high frequency of chromosome rearrangements, including segmental deletions, duplications, and amplifications, in human cleavage-stage embryos. Recently, it has been shown that single-nucleotide polymorphism arrays can detect mosaicism as low as 5%22; however, given that the majority of single-nucleotide polymorphism probes map out of exons, these arrays are unlikely to detect exonic CNVs. Similarly, BAC clone arrays, estimated to have a potential to detect 10% mosaicism,23 cannot identify copy number changes smaller than approximately 50–100 kb. Conversely, oligonucleotide array CGH can be custom designed exon targeted and detect 20–30% mosaicism of small (exonic) CNVs.17,24,25
Our data reinforce the previously described genotype-phenotype correlation in patients with CDKL5 disruption. These patients may present with an initial relatively normal development, followed by early-onset infantile spasms, and subsequent medically intractable epilepsy with developmental delay. Although most of the published data focus mainly on heterozygous female patients, as male fetuses carrying a mutation or deletion have been thought to die in utero, our results demonstrate that the mosaic deletion CNV can be a more common occurrence than previously thought, even in male patients. Hence, we recommend array CGH testing for CDKL5 not only in patients of both genders with intractable epilepsy but also in those with unexplained intellectual disability, developmental delay, and mild dysmorphic features. Moreover, we highlight the capability of custom-designed exon-targeted array CGH to diagnose exonic mosaicism.17,26
REFERENCES
Bahi-Buisson N, Nectoux J, Rosas-Vargas H, et al. Key clinical features to identify girls with CDKL5 mutations. Brain 2008; 131: 2647–2661.
Montini E, Andolfi G, Caruso A, et al. Identification and characterization of a novel serine-threonine kinase gene from the Xp22 region. Genomics 1998; 51: 427–433.
Sprovieri T, Conforti FL, Fiumara A, et al. A novel mutation in the X-linked cyclin-dependent kinase-like 5 (CDKL5) gene associated with a severe Rett phenotype. Am J Med Genet A 2009; 149A: 722–725.
Lin C, Franco B, Rosner MR . CDKL5/Stk9 kinase inactivation is associated with neuronal developmental disorders. Hum Mol Genet 2005; 14: 3775–3786.
Mari F, Azimonti S, Bertani I, et al. CDKL5 belongs to the same molecular pathway of MeCP2 and it is responsible for the early-onset seizure variant of Rett syndrome. Hum Mol Genet 2005; 14: 1935–1946.
Russo S, Marchi M, Cogliati F, et al. Novel mutations in the CDKL5 gene, predicted effects and associatedphenotypes. Neurogenetics 2009; 10: 241–250.
Bahi-Buisson N, Girard B, Gautier A, et al. Epileptic encephalopathy in a girl with an interstitial deletion of Xp22 comprising promoter and exon 1 of the CDKL5 gene. Am J Med Genet B Neuropsychiatr Genet 2009; 153B: 202–207.
Erez A, Patel AJ, Wang X, et al. Alu-specific microhomology-mediated deletions in CDKL5 in females with early-onset seizure disorder. Neurogenetics 2009; 10: 363–369.
Mei D, Marini C, Novara F, et al. Xp22.3 genomic deletions involving the CDKL5 gene in girls with early onset epileptic encephalopathy. Epilepsia 2010; 51: 647–654.
Elia M, Falco M, Ferri R, et al. CDKL5 mutations in boys with severe encephalopathy and early-onset intractable epilepsy. Neurology 2008; 71: 997–999.
Sartori S, Di Rosa G, Polli R, et al. A novel CDKL5 mutation in a 47,XXY boy with the early-onset seizure variant of Rett syndrome. Am J Med Genet A 2009; 149A: 232–236.
Weaving LS, Christodoulou J, Williamson SL, et al. Mutations of CDKL5 cause a severe neurodevelopmental disorder with infantile spasms and mental retardation. Am J Hum Genet 2004; 75: 1079–1093.
Masliah-Plachon J, Auvin S, Nectoux J, et al. Somatic mosaicism for a CDKL5 mutation as an epileptic encephalopathy in males. Am J Med Genet A 2010; 152A: 2110–2111.
Van Esch H, Jansen A, Bauters M, et al. Encephalopathy and bilateral cataract in a boy with an interstitial deletion of Xp22 comprising the CDKL5 and NHS genes. Am J Med Genet A 2007; 143: 364–369.
Huopaniemi L, Tyynismaa H, Rantala A, et al. Characterization of two unusual RS1 gene deletions segregating in Danish retinoschisis families. Hum Mutat 2000; 16: 307–314.
El-Hattab AW, Smolarek TA, Walker ME, et al. Redefined genomic architecture in 15q24 directed by patient deletion/duplication breakpoint mapping. Hum Genet 2009; 126: 589–602.
Boone PM, Bacino CA, Shaw CA, et al. Detection of clinically relevant exonic copy-number changes by array CGH. Hum Mutat 2010; 31: 1326–1342.
Nemos C, Lambert L, Giuliano F, et al. Mutational spectrum of CDKL5 in early-onset encephalopathies: a study of a large collection of French patients and review of the literature. Clin Genet 2009; 76: 357–371.
Bahi-Buisson N, Kaminska A, Boddaert N, et al. The three stages of epilepsy in patients with CDKL5 mutations. Epilepsia 2008; 49: 1027–1037.
Zhang F, Khajavi M, Connolly AM, et al. The DNA replication FoSTeS/MMBIR mechanism can generate genomic, genic and exonic complex rearrangements in humans. Nat Genet 2009; 41: 849–853.
Vanneste E, Voet T, Le Caignec C, et al. Chromosome instability is common in human cleavage-stage embryos. Nat Med 2009; 15: 577–583.
Conlin LK, Thiel BD, Bonnemann CG, et al. Mechanisms of mosaicism, chimerism and uniparental disomy identified by single nucleotide polymorphism array analysis. Hum Mol Genet 2010; 19: 1263–1275.
Ballif BC, Rorem EA, Sundin K, et al. Detection of low-level mosaicism by array CGH in routine diagnostic specimens. Am J Med Genet A 2006; 140: 2757–2767.
Cheung SW, Shaw CA, Scott DA, et al. Microarray-based CGH detects chromosomal mosaicism not revealed by conventional cytogenetics. Am J Med Genet A 2007; 143A: 1679–1686.
Scott SA, Cohen N, Brandt T, et al. Detection of low-level mosaicism and placental mosaicism by oligonucleotide array comparative genomic hybridization. Genet Med 2010; 12: 85–92.
Miller DT, Adam MP, Aradhya S, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 2010; 86: 749–764.
Acknowledgements
Supported in part by Grants R13-0005-04/2008 and PBZ-KBN-122/P05/2004/1-4 from the Polish Ministry of Science and Higher Education and by DK081735 (A.E.). The authors are grateful to the patients and their families for participating in this study. They thank Dr. Melissa B. Ramocki for helpful discussion and Weihong Jin and Zhilian Xia for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first two authors contributed equally to this work.
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bartnik, M., Derwińska, K., Gos, M. et al. Early-onset seizures due to mosaic exonic deletions of CDKL5 in a male and two females. Genet Med 13, 447–452 (2011). https://doi.org/10.1097/GIM.0b013e31820605f5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31820605f5
Keywords
This article is cited by
-
Research progress on the pathogenesis of CDKL5 pathogenic variants and related encephalopathy
European Journal of Pediatrics (2023)
-
Low-level parental somatic mosaic SNVs in exomes from a large cohort of trios with diverse suspected Mendelian conditions
Genetics in Medicine (2020)
-
Identification of De Novo DNMT3A Mutations That Cause West Syndrome by Using Whole-Exome Sequencing
Molecular Neurobiology (2018)
-
The Impact of Next-Generation Sequencing on the Diagnosis and Treatment of Epilepsy in Paediatric Patients
Molecular Diagnosis & Therapy (2017)
-
Integrated analysis of whole-exome sequencing and transcriptome profiling in males with autism spectrum disorders
Molecular Autism (2015)