Abstract
Summary of Recommendations: The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group found adequate evidence to recommend against routine testing for Factor V Leiden (FVL) and/or prothrombin 20210G>A (PT) in the following circumstances: (1) adults with idiopathic venous thromboembolism (VTE). In such cases, longer term secondary prophylaxis to avoid recurrence offers similar benefits to patients with and without one or more of these mutations. (2) Asymptomatic adult family members of patients with VTE and an FVL or PT mutation, for the purpose of considering primary prophylactic anticoagulation. Potential benefits are unlikely to exceed potential harms. The overall certainty of these findings was deemed “moderate.” The evidence was insufficient to determine whether FVL/PT testing might have clinical utility in some circumstances, such as for identifying FVL homozygosity among asymptomatic family members of adults with idiopathic VTE or counseling patients about the risks and benefits of antithrombotic therapy. Based on the available evidence, the certainty of net health benefit was deemed “low.” The recommendations do not extend to patients with other risk factors for thrombosis, such as contraceptive use, as the evidence review that serves as the basis for the recommendations focused primarily on idiopathic VTE.
Rationale: In developing these recommendations the EGAPP Working Group considered evidence in the following three areas.
Analytic Validity: There is adequate evidence that testing accurately and reliably detects the R506Q (FVL) and 20210G>A (PT) variants in the Factor V and PT genes, respectively (a more complete definition of analytic validity, clinical validity, and clinical utility is contained under the “Clinical Considerations” section).
Clinical Validity: The presence of a heterozygous FVL variant seems to be a weak risk factor for recurrence of VTE (odds ratio [OR]: 1.56). Rare homozygous FVL mutations present somewhat greater risks of VTE recurrence (OR: 2.65). The evidence for this increased risk is convincing, but the magnitude of excess risk is not as great as previously thought. The evidence is insufficient to draw conclusions about excess VTE recurrence risk resulting from compound heterozygosity (FVL and PT), but it is likely to be at least as high as with FVL alone. The OR for compound heterozygosity is 6.69. The evidence is insufficient to draw conclusions about VTE recurrence risks associated with PT mutations alone. For family members of index VTE cases, there is convincing evidence that both heterozygosity and homozygosity for FVL are associated with higher risks for VTE occurrence (ORs 3.49 and 17.84, respectively) than for family members without FVL variants.
Clinical Utility: There is convincing evidence that longer term secondary prophylaxis after an initial idiopathic VTE event yields comparable benefits to those with and without a FVL or PT mutation. For asymptomatic family members of index cases, no prophylaxis trials have been reported. Hence, there is no direct evidence of particular benefit to family members. Potential net harm is possible if primary prophylaxis is administered to asymptomatic family members with one or more mutations, because the absolute risk of an initial VTE event is low, and the risk of anticoagulant-induced hemorrhage is relatively high.
Similar content being viewed by others
CLINICAL CONSIDERATIONS
Definitions used by evaluation of genomic applications in practice and prevention
-
Factor V Leiden (FVL; R506Q), the most common known inherited risk factor for thrombosis, results from a base change from G to A at position1691 of the gene encoding coagulation Factor V. The associated amino acid substitution eliminates one of three activated Protein C cleavage sites in the Factor V protein, resulting in Factor V being inactivated more slowly and generating more thrombin, thereby enhancing the potential for clot formation.
-
Prothrombin (PT; 20210G>A), the second most common known inherited risk factor for thrombosis, is a gene variant that produces an amino acid substitution in the PT protein, which results in higher circulating PT levels and an enhanced potential for clot formation.
-
Venous thromboembolism (VTE), including deep venous thrombosis and pulmonary embolism, is characterized by pathologic thrombosis occurring in the venous circulatory system.1–3 The present report deals with idiopathic VTE (also referred to as “unprovoked” VTE), meaning that the event occurs in the absence of a known precipitating factor, such as oral contraceptives, surgery, trauma, or cancer.
-
Thrombophilia refers to an acquired or inherited condition that predisposes to the development of pathologic thromboses.
-
Analytic validity refers to the ability of a test to accurately and reliably measure the genotype or analyte of interest, in this case the above-described mutations in Factor V and PT genes.
-
Clinical validity is defined as a test's ability to accurately and reliably identify or predict the disorder or phenotype of interest, in this case the ability of FVL and PT mutation testing to predict occurrence or recurrence of VTE.
-
Clinical utility defines the balance of benefits and harms associated with the use of the test in practice, including improvement in measurable clinical outcomes and usefulness/added value in clinical management and decision making, compared with not using the test. In the present context, clinical utility depends on the extent to which identification of a FVL or PT mutation alters management in index cases with VTE and leads to health-related outcomes that are significantly improved over current practice. Among family members of index cases, clinical utility again depends on the extent to which management changes when a mutation is identified and most importantly how effectively such management leads to avoidance of VTE. A test may be found to have clinical validity (i.e., be a legitimate risk factor for the disorder) without having clinical utility if there is not sufficient evidence to show benefits resulting from use of the test. In the present context, clinical utility of FVL and PT will depend on whether their identification affects patient management and outcome.
Patient population under consideration
These recommendations apply to adults with a history of idiopathic VTE and their asymptomatic adult family members. The recommendations do not extend to individuals with other known risk factors for thrombosis, such as contraceptive use.
BACKGROUND AND CLINICAL CONTEXT FOR THE RECOMMENDATION
Venous thromboembolism
The following background information is for general orientation and does not include data from the recent evidence review that is the primary basis for our recommendation statement.2 VTE is a common source of morbidity and mortality in the United States. Most often, the thrombotic event begins as deep vein thrombosis (DVT) in the legs. Subsequently, a portion of the clot may break off and migrate to the pulmonary arteries, obstructing the blood flow. VTE has been estimated to occur at an annual rate of 48–66 per 100,000 and pulmonary embolism in 33–69 per 100,000 in the general population.4,5 Individuals who have experienced one episode of VTE are at increased risk for suffering a recurrent thrombotic event. In the absence of continued anticoagulant medication, VTE will recur in approximately 20% of patients within 5 years and 30% within 10 years.6,7 Unprovoked VTE may be viewed as a chronic disease because of its high frequency of recurrence.8 The American College of Chest Physicians currently recommends that patients with unprovoked DVT be treated with a Vitamin K antagonist for at least 3 months. After 3 months of anticoagulant therapy, all patients with unprovoked DVT should be evaluated for the risk-to-benefit ratio of long-term therapy. Long-term treatment is recommended for patients with a first unprovoked episode of proximal DVT, when risk factors for bleeding are absent and good anticoagulant monitoring is achievable. The duration of therapy to avoid recurrence depends on a balance between persistent risk factors and risk of bleeding.9
In addition to the FVL and PT mutations, heritable causes of VTE include deficiencies in natural anticoagulants such as antithrombin, Protein C, and Protein S. Examples of acquired causes include cancer, surgery, chemotherapy, autoimmune disease, contraceptives (oral, patch, and ring), and estrogen replacement therapy. Laboratory evaluation commonly involves testing for activated Protein C resistance and/or FVL, PT, antithrombin, Protein C, and Protein S deficiencies, lupus anticoagulant, anticardiolipin antibodies, anti-β2-glycoprotein-1 antibodies, and Factor VIII levels. Such testing is commonly performed after a diagnosis of VTE, particularly after an early-onset event, thrombosis at an unusual body site, recurrent thrombosis, or thrombosis during pregnancy. In most patients with VTE, including up to half of those who are genetically predisposed, a combination of thrombophilic risk factors is present. Such factors tend to act synergistically.
Risk factors for either a primary or a recurrent VTE event are also classified according to whether they can be modified by an individual's actions. In addition to the heritable risks described earlier, increased risks for VTE during pregnancy and with advancing age are considered unmodifiable, as are the increased recurrence risks associated with being male.10–12 A wide variety of medical disorders and surgical interventions carry increased risk for VTE as well, and it is important for these to be factored into clinical decision making.
The International Cooperative Pulmonary Embolism Registry13 found an overall 3-month mortality of 17.4% for all patients with pulmonary embolism, with 45% of deaths ascribed directly to the embolic event. Two other studies14,15 found lower rates of 1.0% and 2.2%, respectively, but those study designs excluded patients with massive pulmonary embolism requiring thrombolytic treatment.
The postthrombotic syndrome occurs as a result of venous hypertension because of outflow obstruction and damage to the venous valves. Clinical characteristics are leg pain, skin changes, and swelling. The cumulative incidence of this syndrome is 22.8% after 2 years, 28% after 5 years, and 29.1% after 8 years.16 In patients with a first episode of proximal deep venous thrombosis, the cumulative incidence of mild-to-moderate postthrombotic syndrome is approximately 50% and of severe postthrombotic syndrome 23%.13 The postthrombotic syndrome is more likely to occur after recurrent episodes of deep venous thrombosis and can have great impact on quality of life, with leg ulcers being one of the most serious complications. After a first episode of venous thrombosis, elastic stockings reduce the risk of developing postthrombotic syndrome by 50%.13
FVL and PT frequency
In the United States, approximately 5.1%, 2.0%, and 1.2% of the non-Hispanic white, Hispanic white, and African American populations are heterozygous for the FVL mutation, respectively. Corresponding rates of homozygosity are much lower (65, 10, and 4 per 100,000 individuals, respectively).17–19 An FVL mutation is present in 15–20% of individuals with an initial episode of VTE, making it the most common known heritable thrombophilic risk factor.20 Population studies have suggested that a single FVL variant (heterozygosity) increases risk for an initial episode of VTE by 4- to 7-fold over the annual background risk of less than one per thousand, whereas two copies (homozygosity) increase that risk by 9- to 80-fold.19–21 A recent retrospective study, involving subjects who were first-degree relatives of patients who had experienced DVT, PE, or arterial thrombosis before reaching the age of 50 years, found the annual incidence of DVT to be 0.41% (95% confidence interval [CI], 0.28–0.58) among carriers and 0.19% (95% CI, 0.16–0.23) among noncarriers of FVL, for a relative risk of 2.1 (95% CI, 1.4–3.2). When inheritance of additional known thrombophilic mutations was excluded from the analysis, relative risk for DVT increased to 7.0 (95% CI, 2.3–21.7) among FVL carriers.22
The PT mutation is the second most common heritable risk factor for VTE. In the United States, approximately 2.2%, 2.2%, and 0.6% of non-Hispanic white, Hispanic white, and African American populations, respectively, are heterozygous for the PT mutation.17 Individuals homozygous for this mutation are rare (12, 12, and <1 per 100,000 individuals, respectively). The PT mutation is present in 6% of individuals with an initial episode of venous thrombosis and seems to increase risk for VTE by 2- to 4-fold.19,23
In the general population, individuals with both an FVL mutation and PT mutation (compound heterozygotes) occur at the rate of 22 per 100,000.17 In such individuals, there is an estimated 20-fold increased risk for an initial episode of VTE.19,20,24 Among patients with VTE who are heterozygous for FVL, 12% will also be heterozygous for PT.19,20,24
There is some evidence that the prevalence of the FVL mutation is higher in patients with uncomplicated deep venous thrombosis (i.e., without pulmonary embolism) than in patients with pulmonary embolism (with or without deep venous thrombosis).23,25 By contrast, the frequency of the PT mutation among individuals with uncomplicated deep venous thrombosis is not different from those with pulmonary embolism.19,24
Clinical context
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) commissioned an evidence-based review to address an overarching question regarding the following specific clinical scenario: “Does FVL mutation testing, alone or in combination with PT mutation testing, lead to improved clinical outcomes (e.g., avoidance of recurrent VTE) in adults with a personal history of VTE or to improved outcomes (e.g., avoidance of an initial VTE) in adult family members of mutation-positive individuals? Are the testing results useful in medical, personal, or public health decision-making?”2 The present recommendation relies on evidence from that review, which was aimed at documenting the extent to which FVL and PT testing leads to improved health outcomes for individuals with VTE and one or more of these thrombophilic risk factors (by individualized treatment) and for members of these individuals' families (by management strategies to minimize both initial and recurrent thrombotic events).
REVIEW OF SCIENTIFIC EVIDENCE
This statement summarizes the supporting scientific evidence used by the EGAPP Working Group (EWG) to make recommendations regarding the use of FVL and PT mutation testing in adults with a personal history of VTE and in asymptomatic adult family members of mutation-positive individuals.
Methods
EGAPP is a project developed by the Office of Public Health Genomics at the Centers for Disease Control and Prevention to support a rigorous, evidence-based process for evaluating genetic tests and other genomic applications being proposed (or used in) clinical and public health practice in the United States.3 A key goal of the EWG is to develop conclusions and recommendations regarding clinical genomic applications and to establish clear linkage to the supporting scientific evidence. The EWG members are nonfederal multidisciplinary experts convened to establish methods and processes, set priorities for review topics, participate in technical expert panels for commissioned evidence review topics, and develop and publish recommendations.
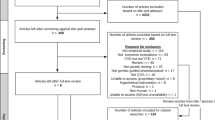
EGAPP commissioned an evidence review through the Agency for Health care Research and Quality, and this review was conducted by investigators at The Johns Hopkins University Evidence-Based Practice Center. The final report “Outcomes of Genetic Testing in Adults with a History of Venous Thromboembolism” is available online.2 Peer-reviewed summary reports of the evidence for analytic validity26 and clinical validity27 have also been published. Because it was anticipated that data might not be available to directly answer the overarching question, the EWG constructed an analytic framework and key questions to address different components of evaluation (e.g., analytic validity, clinical validity, and clinical utility) for the purpose of providing relevant indirect evidence of efficacy. Established Agency for Healthcare Research and Quality Evidence-based Practice Center methods were followed in conducting this review. A Technical Expert Panel that included three EWG members provided expert guidance during the course of the review.
EWG members reviewed the evidence report, key primary publications, other sources of information, and comments on the evidence report from the test developers. The process also included assessment of key gaps in knowledge and relevant contextual factors (e.g., availability of diagnostic or therapeutic alternatives, feasibility and practicality of implementation, and cost-effectiveness). The final EWG recommendation statement was formulated based on magnitude of effect, certainty of evidence, and consideration of contextual factors.3
Technology
Methods currently in use can be determined from the 2009 College of American Pathologists (CAP) Proficiency Testing Survey that included 335 laboratories that tested for FVL (325 of these also performed PT testing). Most laboratories use a polymerase chain reaction method or the Invader technology. Smaller numbers use allele-specific polymerase chain reaction/amplification refractory mutation system, microarray technologies, bead arrays, oligoligation assays, pyrosequencing, and other methods. Many of these laboratory methodologies are described in the American College of Medical Genetics Standards and Guidelines for Clinical Genetic Laboratories (http://www.acmg.net/Pages/ACMG_Activities/stds-2002/g.htm).
Analytic validity
In the current clinical scenario, analytic validity is defined as a laboratory's ability to accurately and reliably detect the FVL mutation (R506Q) and a single PT mutation (20210 G<A). Given that there are two alleles for each of the genes, the genetic test(s) may identify individuals with no mutations, individuals with a single mutation (heterozygous), or individuals with two mutations (homozygous or compound heterozygous).
Two categories of studies are available to assess analytic validity: proficiency testing exercises and method comparisons between an experimental test and a referent test. The evidence review commissioned by the EWG summarized findings from 37 method comparison studies involving FVL and 19 involving PT.2 Despite shortcomings inherent in method comparison studies, which may include investigational and clinical tests, the overall conclusions are consistent with those from proficiency testing studies (described later).
Proficiency testing programs assess laboratory performance by means of interlaboratory comparisons. The proficiency testing program sends blinded samples to multiple laboratories for testing. The results are returned to the proficiency testing provider, graded, and compared with the results obtained by other laboratories. Participants typically receive reports that describe the laboratory's individual performance and the aggregate performance of the other participating laboratories. Proficiency testing programs document pre- and post-analytical testing errors and assay performance. They often categorize results obtained with specific assay methods and report consensus findings by participating laboratories of alleles tested and genotypes identified in each exercise. Data from proficiency testing have been suggested to be a reliable source for assessing overall laboratory performance under real-world conditions.3,27
Identification of FVL and PT mutations has been reported from proficiency testing schemes in the United States,28 the United Kingdom/Europe,28 and Australia.29 Collectively, these reports show an overall error rate of 1.0% for FVL, an analytic sensitivity of 98.8%, and an analytic specificity of 99.3%. The overall error rate for identifying PT mutations is 0.9%, with an analytic sensitivity of 98.3% and an analytic specificity of 99.6%. The reliability of test performance is high, therefore, for both FVL and PT. One of the reports29 noted that 3 of 39 laboratories were responsible for 46% of the errors, underscoring the opportunity to identify individual poor performance and encourage remedial steps.
In Appendix E of its report on genetic oversight, the Secretary's Advisory Committee on Genetics Health and Society summarized the CAP proficiency testing data for FVL and PT during 2006.30 Overall correct response rates were between 98.9% and 99.6%. In the 2009 CAP survey, the 335 laboratories that performed FVL testing participated in three challenges. Among the 1005 test results, two errors were recorded. Similar performance was found for the 325 laboratories testing for PT mutations. This indicates that laboratory testing performance continues to be reliable for these mutations.
Analytic validity conclusions
There is convincing evidence that analytic validity is high for both FVL and PT.
Most laboratories can test for FVL and PT with a high degree of reliability.
Clinical validity
Clinical validity is defined as a test's ability to accurately and reliably identify or predict the disorder or phenotype of interest. As used in the evidence report and in this recommendation, clinical validity refers to the ability of FVL and PT mutation testing to predict recurrence of VTE in index cases and also to predict occurrence of VTE in asymptomatic family members of index cases who are found to carry at least one of these mutations.
Table 1 summarizes the odds ratios calculated in the evidence review after pooling data from appropriate studies that examined the relationship between FVL and PT mutations and recurrent VTE in index cases. Median duration of follow-up ranged from 0.5 to 8 years. Mean annual event rates for recurrent VTE ranged from 1.8 to 7.5% (mean 3.25%).
Table 2 summarizes odds ratios calculated from the evidence review after pooling data from appropriate studies that examined the relationship between FVL and prothrombin 20210G>A mutations and the occurrence of VTE in asymptomatic family members of index cases. Mean duration of follow-up was between 2.8 and 5.7 years. Annual rates for an initial VTE event ranged from 0.09 to 0.56%.
Three studies examined age-related relative risks among individuals with one or more copies of FVL mutations in comparison with family members without a FVL mutation. Table 3 summarizes the results. The first showed a considerably higher relative rate for first lifetime VTE events in the youngest age group of FVL carriers than in older age groups, when compared with family members with no FVL mutations.31 The second and third studies, however, found that relative rates did not differ significantly by age.32,33 Overall relative rates ranged from 2.8 to 4.2, similar to the rates shown in Table 2 for individuals with FVL mutations (either one copy or unspecified).
Among relatives with no FVL mutation, annual VTE incidence rates for the three studies were: 0.1%, 0.09%, and 0.15%, respectively.
The evidence review found low-grade evidence that homozygosity for FVL in pregnant family members is predictive of VTE. Evidence was insufficient, however, to reliably determine the predictive value of heterozygosity for FVL, PT G20210A, or the two in combination in pregnant family members.2,34–38
Clinical validity conclusions
Index cases (patients).
There is convincing evidence that the presence of heterozygous or homozygous FVL is associated with an increased risk of recurrent VTE in index cases (Table 1). The magnitude of this excess risk, however, is small in comparison with the baseline recurrence risk conferred by the history of idiopathic VTE alone. There is convincing evidence that one copy of a PT mutation is not predictive of VTE recurrence. The evidence is inadequate to draw conclusions about the extent of excess risk for VTE recurrence resulting from combined heterozygosity (FVL and PT), but it is likely to be at least as high as with FVL, alone.
Relatives.
There is convincing evidence that homozygosity for FVL is associated with an increased risk for an initial episode of VTE in asymptomatic family members of index cases, and there is convincing evidence that heterozygosity for FVL in family members is also predictive of VTE (Table 2). The magnitude of increased occurrence risks associated with FVL is considerably greater than recurrence risks after an initial episode of VTE. One possible explanation, mentioned in the preceding paragraph, is that other risk factors predominate after VTE has occurred. There is no agreement about the influence of age on VTE rates in family members with an FVL mutation, when compared with family members without a mutation. Adequate evidence indicates that compound heterozygosity (for FVL and PT) in asymptomatic family members is predictive of VTE (the excess risk is likely to be at least as great as with heterozygosity for FVL, alone). Insufficient data are available to draw conclusions about the predictive power of a heterozygous PT mutation for VTE in family members of index cases. Homozygosity for PT is a rare genotype, and its association with VTE in asymptomatic family members cannot presently be determined due to lack of data. Data concerning pregnant family members are sparse.
Clinical utility
Behavior/treatment patterns
A study in Washington State surveyed 112 primary care physicians who ordered FVL testing as part of their practices. Eighty-two percent indicated that they would use test results to counsel their patients about VTE recurrence risks, whereas 67% would use results to make decisions about treatment and prevention. The degree of confidence of these physicians in their ability to interpret or communicate test results was not high, and the physicians were not confident about when the test should be ordered.39 A second study by the group in Washington used a record review to examine the use of FVL testing in clinical practice. Uptake of testing did not follow existing recommendations, and test results were used to influence patient management in the absence of supporting evidence related to health outcomes.40
Intervention effectiveness: Warfarin use in FVL carriers
The four studies summarized below examined recurrence rates of VTE during anticoagulation. None of these studies was designed to examine how FVL or PT testing influences patient management or whether choosing treatment based on such testing alters outcomes.
Study 1.
Table 4 contains data from a prespecified cohort study nested within a randomized controlled trial of long-term, low-intensity warfarin therapy for the prevention of recurrent VTE in the United States.41 At baseline, 36.8% and 40.0% of participants in placebo and warfarin treatment groups, respectively, had experienced two or more episodes of VTE. All patients had been given 3 months of uninterrupted warfarin treatment before randomization and were followed for up to 4.5 years (mean length of follow-up: 2.1 years). Low-intensity warfarin reduced VTE recurrence by 75% among individuals with FVL or PT mutations and by 58% among those without mutations (difference not significant). Numbers of homozygotes and compound heterozygotes were not specified. Based on this prespecified subgroup analysis, the study concluded that the protective effect of warfarin did not differ based on mutation status.
Study 2.
Table 5 summarizes data from a cohort analysis nested within a randomized controlled trial in Canada that sought to compare VTE recurrence rates during treatment with low-intensity versus conventional doses of warfarin.42 Before being randomized, all patients received 3 months of uninterrupted treatment with warfarin. At baseline, 51% of all participants had experienced two previous episodes of VTE, whereas 16% had experienced three and 6% four previous episodes of VTE. Follow-up was for an average of 2.3 years. Comparative recurrence rates for the two treatment regimens are presented in the table and were limited to two categories: (1) all thrombophilias (including FVL and PT mutations, as well as antiphospholipid antibodies, Factor VII/XI elevations, and others) and (2) no thrombophilias. The rate of VTE recurrence was 0.8 per 100 person years among patients with FVL mutation(s), when both levels of treatment were combined. This was not different from the rate among patients without FVL. Insufficient data were available to estimate a hazard ratio for PT mutations.
Study 3.
A European randomized controlled trial examined the extent to which oral ximelagatran reduces VTE recurrence compared with placebo during an 18-month study period.43 Ximelagatran was a new drug with anticoagulant properties that allowed more convenient long-term management because of a lesser need for frequent laboratory monitoring. It was withdrawn from the market in 2006 because of occasional severe liver complications. Patients with one to four previous episodes of VTE were included in the randomized trial. However, the majority of participants had experienced only a single episode at baseline.44 All patients had received 6 months of uninterrupted warfarin before randomization, with an average length of 1.5 years follow-up. Table 6 summarizes a cohort analysis nested within that trial showing that ximelagatran treatment significantly lowered the rate of recurrence among patients with FVL and that the impact of treatment on recurrence was similar for patients with and without an FVL mutation. There were too few patients with PT mutations to obtain an accurate estimate.
Study 4.
A prospective cohort study, also from Europe, documented rates of VTE recurrence among patients with idiopathic VTE on long-term anticoagulation with warfarin in comparison to those not on treatment.45 Only participants with a single previous VTE episode were included in the prospective followup. Average follow-up was 5.6 years. The study included a subset of FVL patients, but there were too few FVL patients on long-term treatment to derive a reliable estimate. Table 7 presents the data from that study, which indicate that FVL mutation carriers have a lower observed point estimate for the rate of recurrence, but the differences are not statistically significant (P = 0.184). For the study as a whole, the VTE recurrence rate was significantly lower among those on warfarin treatment than among FVL patients not receiving anticoagulation.
Decision modeling studies
Although no direct evidence of thrombophilia testing on clinical outcomes is available, several decision modeling studies have examined potential outcomes and are summarized in the recent evidence report.2 Those studies provided indirect evidence that, under certain modeled scenarios, testing for FVL alone, PT alone, or the two in combination could be cost-effective when caring for selected patients with VTE or their family members. However, the model inputs used are not consistent with current knowledge of the risk imparted by FVL or PT variants and the findings of these studies should be reassessed. One study46 did evaluate a clinical scenario relatively consistent with the data compiled in the evidence review. In this scenario, the risk of VTE was approximately 7%, and the strategy of FVL testing followed by 3 years of warfarin treatment compared with no FVL testing and standard warfarin prophylaxis had essentially identical clinical outcomes. The authors also found that in the base case scenario (with a higher assumed VTE risk), if the risk of major bleeding was above 1.9%/year, then FVL testing may lead to poorer overall outcomes. If the VTE risk is actually lower as suggested by the recent evidence review, the threshold for major bleeding would be even lower and well within the realm of known risk of major bleeding from warfarin. Thus, in summary, informally applying current estimates of risk imparted by FVL or PT variants to previous cost-effectiveness studies suggests that routine testing is not effective and not cost-effective. Formal updates of these analyses would be helpful in further clarifying these issues.
Patients who have experienced a VTE event related to a modifiable risk factor such as oral contraceptives generally are not candidates for long-term warfarin therapy. The presence of FVL homozygosity might, however, represent an indication for such extended treatment. In the absence of formal studies, evaluation of the potential risks and benefits in this patient population is challenging, given the complexity of the clinical scenario and inherent risk-benefit trade-off of warfarin therapy.
FVL and PT testing among relatives
Data summarized in the present report indicate that the risk for an initial VTE event to occur in an asymptomatic family member with one copy of an FVL mutation is approximately 3.5 times as high as among family members who do not have the mutation. If we assume that this baseline is comparable with an annual population background VTE incidence rate of approximately 10 per 10,000 (among relatives with no FVL mutation, annual VTE incidence rates for the three studies in Table 3 were 0.1%, 0.09%, and 0.15%, respectively), the rate among relatives with a single copy of FVL would be approximately 35 per 10,000. As a counterbalancing factor, anticoagulant treatment carries an annual risk for hemorrhage of at least 100 per 10,000 patient years.47,48 Thus, the risk of a hemorrhagic event is at least three times as great as a thrombotic event. This unfavorable benefit/harm ratio might explain why no studies are available involving anticoagulation of family members with FVL. The greatest increase in risk for VTE occurs when a family member is identified with homozygous FVL. In this situation, the current data indicate that the annual risk for an initial VTE event is approximately 18 times as high as for relatives who do not have a FVL mutation, translating into a rate of approximately 180 per 10,000 per year under the assumptions mentioned earlier. The risk for an initial VTE event in these patients is thus sufficiently high to consider preemptive anticoagulation therapy, but there are no data on the outcomes of anticoagulation in such asymptomatic patients.
Although FVL homozygosity is rare (approximately 1 per 5000 in the general population), it is theoretically possible to design a selective strategy for identifying homozygous family members that begins with FVL testing in index cases of VTE. As an example, a hypothetical cohort of 1000 non-Hispanic white patients with VTE might be genotyped for FVL, with 200 identified as having at least one FVL mutation. The spouses of those 200 with FVL mutations would then be genotyped, eight of whom would also be heterozygous. Assuming 16 offspring for those eight couples (two per family), four would be homozygous. This scenario assumes 100% participation. The preceding example, although subject to modification and refinement, offers a reasonable expectation of new homozygous individuals identified among family members, under optimal conditions. No formal studies assessing preemptive anticoagulation in family members were identified.
Summary
The present recommendation statement is based on an evidence report that focused on a prespecified clinical scenario involving adults with a history of idiopathic VTE and their asymptomatic adult family members. The evidence report did not extend to patients with other known risk factors for thrombosis, such as contraceptive use.
Testing for patients
For index cases with VTE, clinical utility depends on the extent to which identification of a FVL or PT mutation alters management to incrementally prevent recurrence of VTE, thereby leading to health-related outcomes that are improved over current practice. There is evidence that longer term anticoagulation benefits patients both with and without FVL or PT mutations. Longer term warfarin administration assumes that there are no contraindications and that there is access to, and compliance with, accurate therapeutic monitoring. There is evidence from one chart review survey that management may be altered by knowledge that one of these mutations is present. However, uptake of testing did not follow existing recommendations, and test results were used to influence patient management in the absence of supporting evidence related to health outcomes.40
The net benefit of warfarin therapy includes consideration of both benefits (prevention of VTE) and harms (bleeding risk). The most immediate potential harm with instituting prolonged anticoagulation arises from anticoagulant-induced hemorrhage. The risk of major bleeding due to anticoagulant treatment is at least 1–3% per year, of which one in five cases is fatal.47,48 The risk of bleeding complications rises significantly with age and the achieved International Normalized Ratio.49 A net benefit would be achieved if enough VTE recurrences could be prevented that risk of an occasional hemorrhagic event would be acceptable. The data indicate that this balance of benefits and harms should be applied to post-VTE patients, regardless of mutation status, and that a favorable balance may be achieved through longer term anticoagulation. Special considerations, such as might occur when VTE is associated with oral contraceptives or hormone replacement therapy, are not considered here.
Testing of relatives
There are no published comparative trials involving primary chronic anticoagulant administration to asymptomatic family members of index cases with one or more of these mutations. Clinical utility again depends on the extent to which management changes when a mutation is identified and, most importantly, how effectively such management leads to avoidance of VTE. If any strategy to achieve this improvement would prominently include use of anticlotting agents, such as warfarin, then the most immediate potential harm would be a hemorrhagic event. The balance between benefits and harms will differ from that in index cases, however, because the risk for an initial VTE event to occur among heterozygous family members is much lower than that for a recurrent event in an index case.
Clinical utility conclusions
-
There is no evidence that knowledge of FVL/PT mutation status in patients with VTE affects anticoagulation treatment to avoid recurrence.
-
There is convincing evidence that anticoagulation beyond 3 months reduces recurrence of VTE, regardless of mutation status.
-
There is no evidence that knowledge of FVL/PT mutation status among asymptomatic family members of patients with VTE leads to anticoagulation aimed at avoiding initial episodes of VTE.
Clinical trials
A search was done on the website ClinicalTrials.gov, using the terms “factor V Leiden,” “R506Q,” “G1691A,” and “G20210A” (October 2, 2009). No clinical validity or clinical utility-related implications were identified that would be expected to affect future recommendations relating to the current specific clinical scenario. Regarding analytic validity, one ongoing external validation study was found comparing performance of FVL and PT testing using VeraCode Genotyping on a BeadXpress System versus bidirectional sequencing (http://clinicaltrials.gov/ct2/show/NCT00959504?term=factor+v+leiden&rank=4). No relevant additional results were obtained from searches of the WHO International Clinical Trials Registry Platform (http://www.who.int/ictrp/en/), using the same search terms on the same date.
Contextual issues important to the recommendation
Cost-effectiveness
-
Cost-effectiveness modeling studies in this area require updating with current VTE risk estimates but are suggestive that routine FVL/PT testing is not cost-effective.
Research gaps
The research literature is insufficient in many respects, and the EWG recommends further studies that could address important gaps in knowledge. Among these gaps, the EWG found the following:
-
Few data on how either homozygosity for FVL/PT or compound heterozygosity might lead to individualized management and thereby avoid either occurrence or recurrence of VTE.
-
No information about how knowledge of FVL/PT mutation status might affect behavior (i.e., motivation) for adherence to anticoagulation treatment after a VTE episode.
-
No information about other related issues, such as relief of anxiety that might result from identification of FVL status.
-
No formal risk-benefit or cost-effectiveness analyses using current estimates of VTE risk imparted by FVL/PT variants.
It is speculated that absence of data on anticoagulation strategies for asymptomatic family members who are heterozygous for FVL might be explained by an unfavorable risk/benefit balance because of low absolute risk for VTE. This is not considered a gap in knowledge.
Recommendations of other groups
Several guidelines and recommendations pertinent to our present clinical scenario for FVL/PT mutation testing have been published. Because EGAPP aims to address clinical and public health practice issues within the US health care system, we have limited discussion in this section to US guidelines and recommendations.
American College of Medical Genetics Consensus Statement on FVL mutation testing includes the following50:
-
“[…] There is growing consensus that FVL testing should be performed, following the same general recommendations as for any thrombophilia. Random screening of the general population for factor V Leiden is not recommended.”
-
“Patients testing positive for factor V Leiden or APC resistance should be considered for molecular genetic testing for […] the prothrombin 20210A variant…”
CAP consensus recommendations include the following:
-
“Tests for factor V Leiden […], and prothrombin G20210A mutation are appropriate in patients with VTE (particularly for idiopathic VTE), for younger patients, and/or for patients with a family history of thrombosis.[63 references cited] Level 2, with a small number of level 1 studies”51
-
“Heterozygous or homozygous FVL carriers with a first lifetime deep vein thrombosis or pulmonary embolism should be treated in standard fashion…”52
American College of Chest Physicians evidence-based clinical practice guidelines, antithrombotic therapy for venous thromboembolic disease, acknowledge that9:
-
“The presence of hereditary thrombophilia has not been used as a major factor to guide duration of anticoagulation for VTE in these guidelines because evidence from prospective studies [13 reports cited] suggests that these factors are not major determinants of the risk of recurrence.”
Also state that:
-
“For patients with DVT secondary to a transient (reversible) risk factor, we recommend treatment with a VKA [vitamin K antagonist] for 3 months over treatment for shorter periods (Grade 1A).”
-
“For patients with unprovoked DVT, we recommend treatment with a VKA for at least 3 months (Grade 1A). We recommend that after 3 months of anticoagulant therapy, all patients with unprovoked DVT should be evaluated for the risk-to-benefit ratio of long-term therapy (Grade 1C). For patients with a first unprovoked VTE that is a proximal DVT, and in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable, we recommend long-term treatment (Grade 1A). Values and preferences: This recommendation attaches a relatively high value to prevention of recurrent VTE and a lower value to the burden of long-term anticoagulant therapy.”
Although recommendations and guidelines from international groups are not covered in the present recommendation statement, interested readers may find comparisons of our findings with international guidelines such as these (British Committee on Standards in Hematology53; European Genetics Foundation, Cardiovascular Disease Educational and Research Trust, International Union of Angiology, Mediterranean League on Thromboembolism54; French Group on Hemostasis and Thrombosis, and French Society of Vascular Medicine55) to be both interesting and illuminating.
REFERENCES
Ginsberg JS . Management of venous thromboembolism. N Engl J Med, 1996; 335: 1816–1828.
Segal JB, Brotman DJ, Emadi A, et al. Outcomes of genetic testing in adults with a history of venous thromboembolism. Evidence report/technology assessment no. 180. AHRQ publication no. 09-E011, prepared by Johns Hopkins University Evidence Based Practice Center under contract no. HHSA 290-2007-10061-1. Rockville, MD: Agency for Healthcare Research and Quality, 2009.
Teutsch SM, Bradley LA, Palomaki GE, et al. The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) initiative: methods of the EGAPP Working Group. Genet Med, 2009; 11: 3–14.
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ 3rd . Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med, 1998; 158: 585–593.
White RH . The epidemiology of venous thromboembolism. Circulation, 2003; 107: I4–I8.
Hansson PO, Sörbo J, Eriksson H . Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med, 2000; 160: 769–774.
Heit JA, Mohr DN, Silverstein MD, Petterson TM, O'Fallon WM, Melton LJ 3rd . Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med, 2000; 160: 761–768.
Schafer AI . Venous thrombosis as a chronic disease. N Engl J Med, 1999; 340: 955–956.
Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ, American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest, 2008; 133( suppl 6): 454S–545S.
Kyrle PA, Minar E, Bialonczyk C, Hirschl M, Weltermann A, Eichinger S . The risk of recurrent venous thromboembolism in men and women. N Engl J Med, 2004; 350: 2558–2563.
Seligsohn U, Lubetsky A . Genetic susceptibility to venous thrombosis. N Engl J Med, 2001; 344: 1222–1231.
Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE . Venous thromboembolism according to age: the impact of an aging population. Arch Intern Med, 2004; 164: 2260–2265.
Goldhaber SZ, Visani L, De Rosa M . Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet, 1999; 353: 1386–1389.
Low-molecular-weight heparin in the treatment of patients with venous thromboembolism. The Columbus Investigators. N Engl J Med, 1997; 337: 657–662.
Simonneau G, Sors H, Charbonnier B, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for acute pulmonary embolism. The THESEE Study Group. Tinzaparine ou Heparine Standard: Evaluations dans l'Embolie Pulmonaire. N Engl J Med, 1997; 337: 663–669.
Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med, 1996; 125: 1–7.
Chang MH, Lindegren ML, Butler MA, et al. Prevalence in the United States of selected candidate gene variants: Third National Health and Nutrition Examination Survey, 1991–1994. Am J Epidemiol, 2009; 169: 54–66.
Ridker PM, Miletich JP, Hennekens CH, Buring JE . Ethnic distribution of Factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA, 1997; 277: 1305–1307.
Spector EB, Grody WW, Matteson CJ, et al. Technical standards and guidelines: venous thromboembolism (Factor V Leiden and prothrombin 20210G >A testing): a disease-specific supplement to the standards and guidelines for clinical genetics laboratories. Genet Med, 2005; 7: 444–453.
Kujovich J, ( Updated March 9, 2010). Factor V Leiden thrombophilia. In: GeneReviews at GeneTests: Medical Genetics Information Resource (database online). Copyright, University of Washington, Seattle. 1997–2010. Available at: http://www.genetests.org. Accessed July 13, 2010.
Rosendaal FR, Reitsma PH . Genetics of venous thrombosis. J Thromb Haemost, 2009; 7( suppl 1): 301–304.
Mäkelburg AB, Veeger NJ, Middeldorp S, et al. Different risk of deep vein thrombosis and pulmonary embolism in carriers with Factor V Leiden compared with non-carriers, but not in other thrombophilic defects. Results from a large retrospective family cohort study. Haematologica, 2010; 95: 1030–1033.
Martinelli I, Bucciarelli P, Margaglione M, De Stefano V, Castaman G, Mannucci PM . The risk of venous thromboembolism in family members with mutations in the genes of Factor V or prothrombin or both. Br J Haematol, 2000; 111: 1223–1229.
Emmerich J, Rosendaal FR, Cattaneo M, et al. Combined effect of Factor V Leiden and prothrombin 20210A on the risk of venous thromboembolism—pooled analysis of 8 case-control studies including 2310 cases and 3204 controls. Study Group for Pooled-Analysis in Venous Thromboembolism. Thromb Haemost, 2001; 86: 809–816.
Manten B, Westendorp RG, Koster T, Reitsma PH, Rosendaal FR . Risk factor profiles in patients with different clinical manifestations of venous thromboembolism: a focus on the Factor V Leiden mutation. Thromb Haemost, 1996; 76: 510–513.
Emadi A, Crim MT, Brotman DJ, et al. Analytic validity of genetic tests to identify Factor V Leiden and prothrombin G20210A. Am J Hematol, 2010; 85: 264–270.
Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of Factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA, 2009; 301: 2472–2485.
ACCE review: venous thromboembolism. ACCE model system for collecting, analyzing, and disseminating information on genetic tests, 2004. Available at: http://www.cdc.gov/genomics/gtesting/ACCE/FBR/index.htm. Accessed July 8, 2010.
Hertzberg M, Neville S, Favaloro E, McDonald D . External quality assurance of DNA testing for thrombophilia mutations. Am J Clin Pathol, 2005; 123: 189–193.
Secretary's Advisory Committee on Genetics, Health, and Society. U.S. system of oversight of genetic testing: a response to the charge of the secretary of health and human services, 2008. Available at: http://oba.od.nih.gov/oba/SACGHS/reports/SACGHS_oversight_report.pdf. Accessed October 13, 2010.
Middeldorp S, Henkens CM, Koopman MM, et al. The incidence of venous thromboembolism in family members of patients with Factor V Leiden mutation and venous thrombosis. Ann Intern Med, 1998; 128: 15–20.
Lensen R, Rosendaal F, Vandenbroucke J, Bertina R . Factor V Leiden: the venous thrombotic risk in thrombophilic families. Br J Haematol, 2000; 110: 939–945.
Simioni P, Sanson BJ, Prandoni P, et al. Incidence of venous thromboembolism in families with inherited thrombophilia. Thromb Haemost, 1999; 81: 198–202.
Couturaud F, Kearon C, Leroyer C, et al. Incidence of venous thromboembolism in first-degree relatives of patients with venous thromboembolism who have Factor V Leiden. Thromb Haemost, 2006; 96: 744–749.
Martinelli I, Battaglioli T, De Stefano V, et al. The risk of first venous thromboembolism during pregnancy and puerperium in double heterozygotes for Factor V Leiden and prothrombin G20210A. J Thromb Haemost, 2008; 6: 494–498.
Martinelli I, Legnani C, Bucciarelli P, Grandone E, De Stefano V, Mannucci PM . Risk of pregnancy-related venous thrombosis in carriers of severe inherited thrombophilia. Thromb Haemost, 2001; 86: 800–803.
Tormene D, De Stefano V, Grandone E, et al. The G20210A prothrombin variant and the risk of venous thromboembolism or fetal loss in pregnant women: a family study. J Thromb Haemost, 2007; 5: 2193–2196.
Tormene D, Simioni P, Prandoni P, et al. Factor V Leiden mutation and the risk of venous thromboembolism in pregnant women. Haematologica, 2001; 86: 1305–1309.
Hindorff LA, Burke W, Laberge AM, et al. Motivating factors for physician ordering of Factor V Leiden genetic tests. Arch Intern Med, 2009; 169: 68–74.
Laberge AM, Psaty BM, Hindorff LA, Burke W . Use of Factor V Leiden genetic testing in practice and impact on management. Genet Med, 2009; 11: 750–756.
Ridker PM, Goldhaber SZ, Danielson E, et al. Long-term, low-intensity warfarin therapy for the prevention of recurrent venous thromboembolism. N Engl J Med, 2003; 348: 1425–1434.
Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood, 2008; 112: 4432–4436.
Wåhlander K, Eriksson H, Lundström T, et al. Risk of recurrent venous thromboembolism or bleeding in relation to thrombophilic risk factors in patients receiving ximelagatran or placebo for long-term secondary prevention of venous thromboembolism. Br J Haematol, 2006; 133: 68–77.
Schulman S, Wåhlander K, Lundström T, Clason SB, Eriksson H, THRIVE III Investigators. Secondary prevention of venous thromboembolism with the oral direct thrombin inhibitor ximelagatran. N Engl J Med, 2003; 349: 1713–1721.
Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol, 2005; 25: 1992–1997.
Eckman MH, Singh SK, Erban JK, Kao G . Testing for Factor V Leiden in patients with pulmonary or venous thromboembolism: a cost-effectiveness analysis. Med Decis Making, 2002; 22: 108–124.
Palareti G, Leali N, Coccheri S, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet, 1996; 348: 423–428.
van der Meer FJ, Rosendaal FR, Vandenbroucke JP, Briët E . Bleeding complications in oral anticoagulant therapy. An analysis of risk factors. Arch Intern Med, 1993; 153: 1557–1562.
Hirsh J, Lee AY . How we diagnose and treat deep vein thrombosis. Blood, 2002; 99: 3102–3110.
Grody WW, Griffin JH, Taylor AK, Korf BR, Heit JA, ACMG Factor V Leiden Working Group. American College of Medical Genetics consensus statement on Factor V Leiden mutation testing. Genet Med, 2001; 3: 139–148.
Van Cott EM, Laposata M, Prins MH . Laboratory evaluation of hypercoagulability with venous or arterial thrombosis. Arch Pathol Lab Med, 2002; 126: 1281–1295.
Press RD, Bauer KA, Kujovich JL, Heit JA . Clinical utility of Factor V leiden (R506Q) testing for the diagnosis and management of thromboembolic disorders. Arch Pathol Lab Med, 2002; 126: 1304–1318.
Baglin T, Gray E, Greaves M, et al. Clinical guidelines for testing for heritable thrombophilia. Br J Haematol, 2010; 149: 209–220.
Nicolaides AN, Breddin HK, Carpenter P, et al. Thrombophilia and venous thromboembolism. International consensus statement. Guidelines according to scientific evidence. Int Angiol, 2005; 24: 1–26.
Pernod G, Biron-Andreani C, Morange PE, et al. Recommendations on testing for thrombophilia in venous thromboembolic disease: a French consensus guideline. J Mal Vasc, 2009; 34: 156–203.
Author information
Authors and Affiliations
Consortia
Additional information
Disclaimer: This recommendation statement is a product of the independent EGAPP Working Group. Although the Centers for Disease Control and Prevention (CDC) provides support to the EGAPP Working Group, including staff support in the preparation of this document, recommendations made by the EGAPP Working Group should not be construed as official positions of the CDC or the US Department of Health and Human Services.
E-mail: egappinfo@egappreviews.org.
Disclosure: Steven Teutsch is a former employee, and an option holder in Merck & Co., Inc.
Rights and permissions
About this article
Cite this article
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group. Recommendations from the EGAPP Working Group: Routine testing for Factor V Leiden (R506Q) and prothrombin (20210G>A) mutations in adults with a history of idiopathic venous thromboembolism and their adult family members. Genet Med 13, 67–76 (2011). https://doi.org/10.1097/GIM.0b013e3181fbe46f
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181fbe46f