Abstract
Purpose: We evaluated the prevalence of cardiovascular abnormalities and the efficacy and safety of enzyme replacement therapy in patients with late-onset Pompe disease.
Methods: Ninety patients were randomized 2:1 to enzyme replacement therapy or placebo in a double-blinded protocol. Electrocardiograms and echocardiograms were obtained at baseline and scheduled intervals during the 78-week study period. Baseline cardiovascular abnormalities, and efficacy and safety of enzyme replacement therapy were described. Three pediatric patients were excluded.
Results: Eighty-seven patients were included. Median age was 44 years; 51% were men. At baseline, a short PR interval was present in 10%, 7% had decreased left ventricular systolic function, and 5% had elevated left ventricular mass on echocardiogram (all in mild range). There was no change in cardiovascular status associated with enzyme replacement therapy. No significant safety concerns related to enzyme replacement therapy were identified.
Conclusions: Although some patients with late-onset Pompe disease had abnormalities on baseline electrocardiogram or echocardiogram, those classically seen in infantile Pompe disease, such as significant ventricular hypertrophy, were not noted. Cardiovascular parameters were not impacted by enzyme replacement therapy, and there were no cardiovascular safety concerns. The cardiovascular abnormalities identified may be related to Pompe disease or other comorbid conditions.
Similar content being viewed by others
Main
Pompe disease (glycogen storage disease type II; OMIM# 232300) is an autosomal recessive disease caused by a deficiency in the lysosomal enzyme acid alpha-glucosidase. This enzyme defect impacts an estimated 1:40,000 live births and results in an accumulation of glycogen in tissues throughout the body including smooth, skeletal, and cardiac muscle.1,2 There is a wide spectrum of disease severity dependant on the level of residual enzyme activity. Classic infantile Pompe disease is characterized by residual enzyme activity of <1% and progressive hypotonia, hypertrophic cardiomyopathy, hepatomegaly, and respiratory insufficiency typically leading to death within the first year of life without enzyme replacement therapy (ERT).3,4 In contrast, late-onset Pompe disease (juvenile and adult) is caused by a partial deficiency of acid alpha-glucosidase and has a more insidious course.5–8 Typical symptoms in this form of the disease consist of slowly progressive proximal muscle weakness and respiratory difficulties.9–11 Previous studies have suggested that a smaller proportion of patients with late-onset Pompe disease (<10%) have cardiovascular involvement, including electrophysiological abnormalities and myocardial hypertrophy.12–14
Current treatment for Pompe disease consists of ERT with Chinese hamster ovary cell-derived recombinant human acid alpha-glucosidase. Infants have shown significant reduction in left ventricular mass, improvement in cardiac function, and reversal of electrocardiographic abnormalities after ERT.15–23 Studies have also demonstrated stabilization/improvement in both respiratory and motor symptoms in patients with late-onset Pompe disease.24–27 No studies to date have examined response of cardiovascular abnormalities to ERT in patients with late-onset Pompe disease.
The purpose of this analysis was to describe the cardiovascular abnormalities present at baseline in patients with late-onset Pompe disease and to evaluate the effects of ERT on cardiovascular efficacy and safety parameters.
MATERIALS AND METHODS
Study design
This study was a posthoc analysis of cardiovascular parameters in a double-blinded, multicenter, randomized controlled trial evaluating the efficacy and safety of acid alpha-glucosidase ERT versus placebo in patients with late-onset Pompe disease. The primary efficacy endpoints of the original trial consisted of the 6-minute walk test and the percent-predicted forced vital capacity in the upright position (ClinicalTrial.Gov identifier no. NCT00158600; Protocol No. AGLU02704). Results of the primary analysis have been recently published.28 The present analysis focuses on evaluation of cardiovascular endpoints. This study was approved by the Institutional Review Board/Ethics Committee at each primary site, and all patients provided informed consent.
Patient population and randomization
Patients aged 8 years or older with a diagnosis of Pompe disease based on deficient endogenous acid alpha-glucosidase activity in cultured skin fibroblasts of ≤40% of the normal mean of the testing laboratory and two or more acid alpha-glucosidase gene mutations were eligible for inclusion.28 Inclusion criteria included the ability to ambulate 40 meters on each 6-minute walk test performed on 2 consecutive days (use of assistive devices such as a walker, cane, or crutches was permitted), the ability to perform pulmonary function testing, and a forced vital capacity of ≥30% and <80% predicted in the upright position. A negative pregnancy test was also required for women of reproductive age. Exclusion criteria consisted of the following: previous exposure to acid alpha-glucosidase, current requirement for invasive ventilatory support or any ventilatory support while awake and in an upright position, exposure to other investigational therapies in the last 30 days, and major congenital anomalies or history of other medical conditions that may significantly interfere with study compliance.
Ninety patients were randomized 2:1 to the treatment arm using a minimization algorithm in an effort to balance the groups for disease severity.29 Groups were stratified according to baseline 6-minute walk test with a threshold of 300 meters and baseline upright forced vital capacity with a threshold of 55% of the predicted value.
Study interventions and data collection
The treatment arm received biweekly infusions of ERT at a dose of 20 mg/kg for the 78-week study period, and the control group received a volume-matched placebo infusion. ERT consisted of Chinese hamster ovary cell-derived recombinant human acid alpha-glucosidase.
Demographic parameters including age, gender, and race/ethnicity were obtained at baseline. Data on disease duration were also obtained and defined as the number of years since symptom onset. All study electrocardiograms (ECGs) and echocardiograms were performed at one of the eight principal study sites (Appendix). A 12-lead ECG was obtained at baseline and at 26, 52, and 78 weeks. All ECGs were interpreted at the central cardiology core laboratory by a cardiologist blinded to treatment arm. Rate, rhythm, intervals, axes, and voltages were evaluated in the usual manner, and normal thresholds were determined by accepted adult normative ranges. Tachycardia was defined as >100 beats/min and bradycardia as <55 beats/min. A short PR interval was defined as a PR interval ≤120 milliseconds. Prolonged QRS duration was defined as >120 milliseconds. The corrected QT interval was calculated using the Bazett formula, and normal value was defined as <440 milliseconds for men and <450 milliseconds for women. Ventricular hypertrophy and atrial enlargement were defined using standard adult criteria.30 Specifically, left ventricular hypertrophy on ECG was defined using a combination of the Sokolow-Lyon and Cornell criteria.
Echocardiographic evaluation of left ventricular size and function was performed at baseline, 52, and 78 weeks. All echocardiograms were interpreted at the central cardiology core laboratory by a cardiologist blinded to treatment allocation. Left ventricular ejection fraction was calculated from two-dimensional (2D) images using the modified Simpson rule in all patients. Abnormal ejection fraction was defined as <55%.31 Left ventricular mass was evaluated using 2D echocardiography and the truncated ellipsoid method.31 If the 2D image quality was not sufficient, M-mode assessment was performed, and left ventricular mass was calculated using the American Society of Echocardiography method.31 All left ventricular mass measurements were indexed to body surface area to calculate left ventricular mass index. American Society of Echocardiography guidelines were used to define normal and abnormal ranges for left ventricular mass index.31 For women, elevated left ventricular mass index was defined as >88 g/m2 for 2D measurements or >95 g/m2 for M-mode measurements. For men, elevated left ventricular mass index was defined as >102 g/m2 for 2D measurements or >115 g/m2 for M-mode measurements.31
Statistical analysis
Study variables were described using standard summary statistics. Categorical variables were expressed as frequencies and percentages, and continuous variables as medians and interquartile range. Demographic data at baseline were described in the overall cohort of patients and compared in the treatment and control groups using the Wilcoxon rank sum and Fisher exact test where appropriate. Similarly, cardiovascular status (including ECG and echocardiographic data) was described at baseline in the overall cohort of patients and compared in those with a disease duration <15 years versus ≥15 years. A duration of 15 years was chosen as this was the median duration of illness for the cohort. To determine cardiovascular efficacy of therapy, we evaluated the change from baseline to 78 weeks in ECG and echocardiographic parameters in the treatment and control groups. Only those patients with data points both at baseline and at 78 weeks were included in the efficacy analysis. For continuous variables, change from baseline in the control and treatment groups was compared using the Wilcoxon rank sum test. For dichotomous variables, logistic regression was used to assess status at 78 weeks, controlling for baseline status and treatment group. Finally, cardiovascular safety was evaluated by comparing the proportion of patients who developed any ECG or echocardiographic abnormalities at any time during the study period that were not present at baseline in the treatment and control groups using Fisher exact test. All analyses were conducted using STATA version 10 (College Station, TX). Reported P values are two tailed, and a P value <0.05 was considered statistically significant.
RESULTS
Patient characteristics
Of 108 patients screened, 90 were randomized: 60 to the treatment arm and 30 to the control arm. We excluded three patients younger than 17 years from the analysis as the ECG and echocardiography normative ranges used are only applicable to the adult population. Thus, 87 patients were included in the present analysis. Patient characteristics overall, and in each treatment arm, are listed in Table 1. Age, gender, race, and disease duration were similar in the treatment and placebo groups.
Baseline cardiovascular Status
Table 2 presents baseline ECG and echocardiographic data for the entire cohort. At baseline, 84 patients (97%) had an ECG performed, and 85 patients (98%) had an echocardiogram performed measuring left ventricular ejection fraction. Seventy-four patients (85%) had an echocardiogram of sufficient quality to determine left ventricular mass index. Overall, 46% of patients had one or more of the ECG or echocardiographic abnormalities listed in Table 2 at baseline. On echocardiogram, four patients overall (5%) had an elevated left ventricular mass index, all of which were in the mild range (three women, range: 92–97 g/m2; one man, 104 g/m2). Six patients (7%) had a left ventricular ejection fraction <55% (range: 41–54%). There was no overlap between the group with elevated left ventricular mass index and the group with decreased ejection fraction. The most common abnormalities seen on ECG were left ventricular hypertrophy in 12% and a short PR interval in 10% (range: 90–120 milliseconds). Of note, in the 10 patients (12%) with left ventricular hypertrophy on ECG, only one had elevated left ventricular mass index on echocardiography (although two others did not have a baseline echocardiogram). Of the four patients (5%) with an elevated left ventricular mass index on echocardiogram, only one had left ventricular hypertrophy on ECG.
Table 2 also lists the proportion of patients with cardiovascular abnormalities according to disease duration. There were no significant differences seen in those with disease duration <15 years versus ≥15 years. Of note, in the patients who developed symptoms before 10 years of age, three (60%) had one or more ECG or echocardiographic abnormalities.
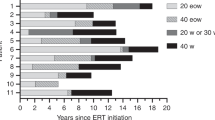
Follow-up
Five (8%) patients in the ERT group and four (14%) patients in the placebo group did not complete the study. Reasons for not completing the study in the treatment group included the following: hypersensitivity reactions related to the study medication (2), death unrelated to treatment (1), and switch to commercial ERT (2). In the control group, the reasons included adverse event not related to study medication (1), switch to commercial ERT (1), and missed 78-week study appointments (2). No events leading to discontinuation of the study were related to the cardiovascular system.
Efficacy of ERT
Table 3 lists ECG and echocardiographic data at baseline and 78 weeks in the treatment and placebo arms for those who completed the study. Of patients with baseline ECG data, 89% had follow-up ECG data. Of patients with baseline echocardiographic data, 80% had follow-up echocardiographic data. No significant changes in ECG or echocardiographic parameters were seen in association with ERT compared with placebo.
Cardiovascular safety of ERT
Table 4 lists data on the proportion of patients with an ECG and echocardiographic abnormality at any time during the study period which was not present at baseline. There were no significant differences between the treatment and placebo groups. Of note, a 40-year-old man in the treatment arm with a known history of Wolff-Parkinson-White syndrome and recurrent episodes of supraventricular tachycardia experienced an episode of supraventricular tachycardia 8 days after the week 6 treatment. This patient had normal left ventricular mass index and ejection fraction at baseline. He was admitted to the hospital and successfully converted to sinus rhythm. The Data Safety Monitoring Board classified this event as serious and possibly related to the study medication. This patient continued in the trial until 23 weeks into the study when he left to pursue commercial treatment. Another patient in the treatment group with a history of Wolff-Parkinson-White syndrome with a concealed pathway did not experience arrhythmias during the study. An additional patient in the enzyme replacement arm had new multiple premature ventricular contractions and sinus tachycardia (103 beats/min) on the 52-week ECG that normalized on subsequent ECGs. This was not classified as a clinically significant adverse event. This patient had a normal ejection fraction and left ventricular mass index at baseline and normal ejection fraction on the 52-week echocardiogram (measurements of left ventricular mass were not obtained on the 52-week echocardiogram).
DISCUSSION
This is the first analysis to evaluate cardiovascular response to ERT in patients with late-onset Pompe disease. Although some patients had abnormalities identified on ECG or echocardiogram at baseline, those such as severe ventricular hypertrophy classically associated with the infantile form of Pompe disease were not noted. There was no significant change in cardiovascular status during the 78-week study period and no significant cardiovascular safety concerns associated with enzyme replacement.
The most common abnormalities identified on baseline testing in our cohort were left ventricular hypertrophy (12%) and short PR interval on ECG (10%), and decreased ejection fraction on echocardiogram (7%). Only 5% of patients had elevated left ventricular mass index on echocardiogram, and these values were all in the mild range. These findings are in contrast to those described in infantile Pompe disease where ECG abnormalities are universal, and cardiac hypertrophy on echocardiogram is much more prevalent and severe.3,4,32 In late-onset Pompe disease, a previous study of 38 patients found a similar proportion of patients with a short PR interval (8%) compared with our study, however, did not observe any ventricular hypertrophy.13 Other studies have also reported a smaller proportion with left ventricular hypertrophy in comparison with our findings.12,14 For example, in a study of 68 patients with late-onset Pompe disease, there were only two patients with abnormal ECG and echocardiographic findings that could not sufficiently be explained by other causes and were potentially related to Pompe disease.12 Likely explanations for these differences may include the smaller patient population in previous studies, potential differences in normative criteria and techniques of assessment of left ventricular hypertrophy, or differences in the proportion of patients with other conditions such as hypertension and other factors which may also impact left ventricular size.12–14 Data from our study suggest that left ventricular hypertrophy as assessed by ECG is not specific for the diagnosis of increased left ventricular mass in patients with late-onset Pompe disease. Detailed information regarding hypertension and other comorbidities was not collected in this study precluding further analysis to ascertain the potential relationship of such factors to the cardiac abnormalities identified.
The underlying pathogenesis of the left ventricular hypertrophy seen in patients with infantile Pompe disease is thought to be related to intracellular glycogen accumulation leading to cellular hypertrophy.15,33 There is often both cardiac hypertrophy and decreased systolic function present, which can prompt the clinician to consider infiltrative processes such as Pompe disease as opposed to hypertrophic cardiomyopathy. There are limited data regarding late-onset Pompe disease. A single previous autopsy report has shown intracardiac glycogen accumulation, although to a much lesser degree than that seen in the infantile form of the disease.34 It is hypothesized that glycogen accumulation and left ventricular hypertrophy are less pronounced and much more rare in late-onset Pompe disease due to the presence of residual alpha-glucosidase activity.7
Wolff-Parkinson-White syndrome and a shortened PR interval are commonly seen in patients with both infantile and late-onset Pompe disease.12,13,32,35–37 These are thought to be related to disruption of the annulus fibrosis (which normally electrically separates the atria and ventricles and routes conduction through the atrioventricular node) by glycogen-filled myocytes allowing ventricular preexcitation and disruption of the normal conduction delay through the atrioventricular node.38,39 Other cardiovascular abnormalities seen in our study include bundle branch block (4%) and atrial enlargement (4%). Bundle branch block could be related to glycogen-laden cells affecting the bundle of His. Atrial enlargement may be a product of poor ventricular compliance and diastolic dysfunction due to glycogen deposition and ventricular hypertrophy. Diastolic dysfunction has been demonstrated in a previous study of patients with late-onset Pompe disease.14 Alternatively, these findings may be unrelated to Pompe disease. For example, in the general population, the prevalence of bundle branch block is approximately 2.5% in the 25–74-year age range.40
There was no significant change in echocardiographic or ECG parameters seen in our study in the enzyme replacement group versus placebo during the 78-week study period. In contrast, in the infantile form of the disease, normalization of the PR interval and reduction in left ventricular hypertrophy after ERT have been shown to occur.15,20,32,38,39 Given the mild cardiac abnormalities identified at baseline in our study, a significant change with ERT may not be expected. In addition, we would not expect to see a response in those subjects whose ECG or echocardiographic abnormalities are due to other comorbidities and not related to Pompe disease. Alternatively, it is possible that patients with late-onset Pompe disease, who are often not diagnosed until later in life, may already have entered the necrotic/fibrotic phase, which may not be reversible with ERT.15,20,21,32,41 It could also be possible that the treatment duration in this study may not have been long enough to effect change in certain cardiovascular parameters. The effect of ERT on general muscle and respiratory function has been shown to occur gradually during a 3-year period in patients with late-onset Pompe disease.24
There were no significant cardiovascular safety concerns associated with enzyme replacement. No difference in cardiac adverse events was seen in patients receiving ERT versus placebo. Significant ventricular ectopy has been reported previously in patients with infantile Pompe disease undergoing ERT in two studies with a prevalence of 17% and 18%, respectively.42,43 In our study, there was one patient in the treatment arm with ventricular ectopy; however, this consisted of infrequent, asymptomatic, isolated premature ventricular complexes on one ECG which resolved on follow-up. The only cardiac adverse event deemed to be “serious” in this trial was an episode of supraventricular tachycardia in the patient with Wolff-Parkinson-White syndrome that required hospital admission. However, this patient had a history of multiple episodes of supraventricular tachycardia, and it was unclear whether this episode was related to ERT.
Limitations
There are several limitations to this analysis. First, not every patient had an ECG or echocardiogram performed at each time point. Thus, our analysis was limited to those with complete baseline and follow-up data. In addition, assessment of left ventricular mass was undertaken with two different echocardiographic techniques. We did not assess changes in diastolic function in this study, and imaging was limited to echocardiography. Although this is the largest study of enzyme replacement in patients with late-onset Pompe disease to date, the relatively small sample size may have limited our ability to detect small differences between groups. Furthermore, the 78-week treatment duration precludes our ability to detect longer-term changes. Finally, we were not able to account for the presence of other comorbidities in our analysis of left ventricular size and function as these data were not available.
CONCLUSIONS
Although some patients with late-onset Pompe disease had abnormalities on ECG or echocardiogram at baseline, cardiovascular abnormalities such as severe ventricular hypertrophy classically associated with the infantile form of Pompe disease were not noted. There were no significant changes in cardiovascular status after 78 weeks of ERT, and we did not identify significant safety concerns. The cardiovascular abnormalities we identified may be related to Pompe disease or other comorbid conditions, and their clinical significance should be determined in consultation with the patient's primary physician. Longer-term evaluation of ERT in a larger cohort of patients with late-onset Pompe disease will be needed to further evaluate baseline characteristics of the multiple Pompe genotypes, comorbidities, additional risk factors, progression of disease, and potential response to long-term ERT.
References
Martiniuk F, Chen A, Mack A, et al. Carrier frequency for glycogen storage disease type II in New York and estimates of affected individuals born with the disease. Am J Med Genet 1998; 79: 69–72.
Ausems MG, Verbiest J, Hermans MP, et al. Frequency of glycogen storage disease type II in the Netherlands: implications for diagnosis and genetic counseling. Eur J Hum Genet 1999; 7: 713–716.
Kishnani PS, Wuh-Liang H, Mandel H, et al. A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr 2006; 148: 671–676.
Van Den Hout H, Hop W, Van Diggelen O, et al. The natural course of infantile Pompe's disease: 20 original cases compared with 133 cases from the literature. Pediatrics 2003; 112: 332–340.
Engel AG, Gomez MR, Seybold ME, Lambert EH . The spectrum and diagnosis of acid maltase deficiency. Neurology 1973; 23: 95–106.
Kishnani PS, Steiner RD, Bali D, et al. Pompe disease diagnosis and management guidelines. Genet Med 2006; 8: 267–288.
Hirschhorn R, Reuser AJ, Glycogen storage disease type II: acid alpha–glucosidase (acid maltase) deficiency. In: Scriver CR, Sly WS (eds) Metabolic and molecular basic of inherited disease. New York, McGraw Hill Companies, 2001; 3389–3420.
Van der Ploeg AT, Reuser A . Lysosomal storage disease 2: Pompe's disease. Lancet 2008; 372: 1342–1353.
Hagemans M, Winkel L, Hop W, Reuser A, Van Doorn P, Van der Ploeg A . Disease severity in children and adults with Pompe disease related to age and disease duration. Neurology 2005; 64: 2139–2141.
Hagemans M, Winkel L, Van Doorn P, et al. Clinical manifestations and natural course of late-onset Pompe's disease in 54 Dutch patients. Brain 2005; 128: 671–677.
Wokke J, Escolar D, Pestronik A, et al. Clinical features of late-onset Pompe disease: a prospective cohort study. Muscle Nerve 2008; 38: 1236–1245.
Van Der Beek N, Soliman O, Van Capelle C, et al. Cardiac evaluation in children and adults with Pompe disease sharing the common c.-32-13T>G genotype rarely reveals abnormalities. J Neuro Sci 2008; 275: 46–50.
Muller-Felber W, Horvath R, Gempel K, et al. Late onset Pompe disease: clinical and neurophysiological spectrum of 38 patients including long-term follow-up in 18 patients. Neuromuscular Disord 2007; 17: 698–706.
Soliman O, Van Der Beek N, Van Doorn P, et al. Cardiac involvement in adults with Pompe disease. J Intern Med 2008; 264: 333–339.
Levine JC, Kishnani PS, Chen YT, Herlong J, Li J . Cardiac remodeling after enzyme replacement therapy with acid alpha-glucosidase for infants with Pompe disease. Pediatr Cardiol 2008; 29: 1033–1042.
Van Den Hout J, Kamphoven J, Winkel L, et al. Long-term intravenous treatment of Pompe disease with recombinant human alpha-glucosidase from milk. Pediatrics 2004; 113: e448–e457.
Amalfitano AA, Bengur AR, Morse RP, et al. Recombinant human acid alpha-glucosidase enzyme therapy for infantile glycogen storage disease type II: results of a phase I/II clinical trial. Genet Med 2001; 3: 132–138.
Klinge L, Straub V, Neudorf U, et al. Safety and efficacy of recombinant acid alpha-glucosidase (RhGAA) in patients with classical infantile Pompe disease: results of a phase II clinical trial. Neuromuscular Disord 2005; 15: 24–31.
Van Den Hout H, Reuser AJ, Vulto AG, Loonen M, Cromme-Dijkhuis A, Van der Ploeg A . Recombinant human alpha-glucosidase from rabbit milk in Pompe patients. Lancet 2000; 356: 397–398.
Chen LR, Chen CA, Chiu SN, et al. Reversal of cardiac dysfunction after enzyme replacement in patients with infantile-onset Pompe disease. J Pediatr 2009; 155: 271–275.
Kishnani PS, Corzo D, Leslie ND, et al. Early treatment with alglucosidase alpha prolongs long-term survival of infants with Pompe disease. Pediatr Res 2009; 66: 329–335.
Kishnani PS, Corzo D, Nicolino M, et al. Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology 2007; 68: 99–109.
Kishnani PS, Nicolino M, Voit T, et al. Chinese hamster ovary cell-derived recombinant human acid alpha-glucosidase in infantile-onset Pompe disease. J Pediatr 2006; 149: 89–97.
Winkel L, Van Den Hout J, Kamphoven J, et al. Enzyme replacement therapy in late-onset Pompe's disease: a three-year follow-up. Ann Neurol 2004; 55: 495–502.
Merk T, Wibmer T, Schumann C, Kruger S . Glycogen storage disease type II (Pompe disease)—influence of enzyme replacement therapy in adults. Eur J Neurol 2009; 16: 159–162.
Strothotte S, Strigl-Pill N, Grunert B, et al. Enzyme replacement with alglucosidase alfa in 44 patients with late-onset glycogen storage disease type 2: 12-month results of an observational clinical trial. J Neurol 2010; 257: 91–97.
Case LE, Koeberl DD, Young SP, et al. Improvement with ongoing enzyme replacement therapy in advanced late-onset Pompe disease: a case study. Mol Genet Metab 2008; 95: 233–235.
van der Ploeg AT, Clemens PR, Corzo D, et al. A randomized study of alglucosidase alfa in late-onset Pompe's disease. N Engl J Med 2010; 362: 1396–1406.
Pocock SJ, Simon R . Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1975; 31: 103–115.
Surawicz B, Knilans T . Chou's electrocardiography in clinical practice—adult and pediatric, 5th ed. Philadelphia, PA, W.B. Saunders Company, 2009.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Ansong AK, Li JS, Nozik-Grayck E, et al. Electrocardiographic response to enzyme replacement therapy for Pompe disease. Genet Med 2006; 8: 297–301.
Kishnani P, Howell RR . Pompe disease in infants and children. J Pediatr 2004; 144( suppl 5): S35–S43.
Van der Walt JD, Swash M, Leake J, Cox EL . The pattern of involvement of adult onset acid maltase deficiency at autopsy. Muscle Nerve 1987; 10: 272–281.
Bulkley BH, Hutchins GM . Pompe's disease presenting as a hypertrophic myocardiopathy with Wolff-Parkinson-White syndrome. Am Heart J 1978; 96: 246–252.
Francesconi M, Auff E, Ursin C, Sluga E . WPW syndrome combined with AV block 2 in an adult with glycogenosis (Type II). Wien Klin Wochenschr 1982; 94: 401–404.
Tabarki B, Mahdhaoui A, Yacoub M, et al. Familial hypertrophic cardiomyopathy associated with Wolff-Parkinson-White syndrome revealing type II glycogenosis. Arch Pediatr 2002; 9: 697–700.
Bharati S, Serratto M, DuBrow I, et al. The conduction system in Pompe's disease. Pediatr Cardiol 1982; 2: 25–32.
Arad A, Moskowitz IP, Patel VV, et al. Transgenic mice overexpressing mutant PRKAG2 define the cause of Wolff-Parkinson-White syndrome in glycogen storage cardiomyopathy. Circulation 2003; 107: 2850–2856.
Bacquer DD, Backer GD, Kornitzer M . Prevalence of ECG findings in large population based samples of men and women. Heart 2000; 84: 625–633.
Griffin JL . Infantile acid maltase deficiency. Virchows Arch B 1984; 45: 23–61.
Cook AL, Kishnani PS, Carboni MP, et al. Ambulatory electrocardiogram analysis in infants treated with recombinant human acid alpha-glucosidase enzyme replacement therapy for Pompe disease. Genet Med 2006; 8: 313–317.
McDowell R, Li JS, Benjamin DK, et al. Arrhythmias in patients receiving enzyme replacement therapy for infantile Pompe disease. Genet Med 2008 10: 758–762.
Acknowledgements
This work was supported by Genzyme Corporation (P.K. and J.S.L.), the National Heart, Lung, and Blood Institute (S.K.P., 1K08HL103631-01), and the American Heart Association Mid-Atlantic Affiliate Clinical Research Program (S.K.P.), the National Institute of Child Health and Development (P.B.S., 1K23HD060040-01). The authors thank Joyce Ahn and Elisa Tsao for their assistance with data management and statistical analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Disclosure: P. Kishnani and J. Li have received research/grant support and honoraria from Genzyme Corporation. P. Kishnani is a member of the Pompe Disease and Gaucher Disease Registry Board for Genzyme Corporation. rhGAA, in the form of Genzyme's product, Myozyme/Lumizyme, has been approved by the US FDA and the European Union as therapy for Pompe disease. Duke University and inventors for the method of treatment and predecessors of the cell lines used to generate the enzyme (rhGAA) used in this clinical trial receive royalty payments pursuant to the University's Policy on Inventions, Patents and Technology Transfer. Dr. van der Ploeg provides consulting services for Genzyme Corp, Cambridge, MA, under an agreement between Genzyme Corp and Erasmus MC, Rotterdam, the Netherlands. This agreement also caters to financial support for Erasmus MC for research in Pompe disease. Erasmus MC and inventors for the method of treatment of Pompe disease by enzyme replacement therapy receive royalty payments pursuant to Erasmus MC policy on inventions, patents and technology transfer.
APPENDIX
APPENDIX
The eight primary investigational sites
-
University of Pittsburgh (Pennsylvania)
-
Children's National Medical Center (Washington, DC)
-
Tower Hematology Oncology Group (California)
-
Washington University (Missouri)
-
Mount Sinai Medical Center (New York)
-
Hôpital de la Pitié-Salpétrière, Institut de Myologie (France)
-
Erasmus Medical Center (The Netherlands)
-
Sophia Children's Hospital (The Netherlands)
Late-onset treatment study principle site investigators
Paula Clemens, MD (University of Pittsburgh), Diana M. Escolar, MD (Children's National Medical Center), Robert T. Leshner (Children's National Medical Center), Pascal Laforêt, MD (Institut de Myologie), Alan Pestronk, MD (Washington University), Melissa Wasserstein, MD (Mount Sinai School of Medicine), Ans van der Ploeg, MD, PhD (Sophia Children's Hospital, Erasmus Medical Center), and Barry Rosenbloom, MD (Mount Sinai Medical Center).
Late-onset treatment study transfer site investigators
Edward Culper, MD (Oregon Health and Science University), Eugen Mengel, MD (Kinderklinik der Universität Mainz), Robert Hopkin, MD (Cincinnati Children's Hospital Medical Center), Robin Casey, MD (Alberta Children's Hospital), Joel Charrow, MD (Children's Memorial Hospital), David Sillence, MD (Children's Hospital at Westmead), Bernard Lemieux, MD (Centre Hospitalier Universitaire de Sherbrooke), Katherine Sims, MD (Massachusetts General Hospital), C. Ronald Scott, MD (University of Washington Medical Center), Isablle Durieu, MD (Centre Hospitalier Lyon Sud), Alain Furby, MD (Hôpital Yves Le Foll), Fabien Zagnoli, MD (H.I.A. Clermont Tonnerre), Richard Barohn, MD (Kansas University Medical Center), Sharon Nations, MD (Southwestern Medical Center of Dallas), Reed Pyeritz, MD, PhD (University of Pennsylvannia School of Medicine), Terence Edgar, MD (Prevea Pediatric Neurology), Bruce Barship, MD, PhD (University of California, San Diego), Mark Olsen, MD (Oklahoma Oncology & Hematology, P.C.), James Tita, DO (St. Vincent Mercy Medical Center), G. Bradley Schaefer, MD (University of Nebraska Medical Center), and Kirk Aleck, MD (St Joseph's Hospital and Medical Center).
Rights and permissions
About this article
Cite this article
Forsha, D., Li, J., Smith, P. et al. Cardiovascular abnormalities in late-onset Pompe disease and response to enzyme replacement therapy. Genet Med 13, 625–631 (2011). https://doi.org/10.1097/GIM.0b013e3182142966
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3182142966
Keywords
This article is cited by
-
Pompe Disease: a Clinical, Diagnostic, and Therapeutic Overview
Current Treatment Options in Neurology (2022)
-
Pattern and prognostic value of cardiac involvement in patients with late-onset pompe disease: a comprehensive cardiovascular magnetic resonance approach
Journal of Cardiovascular Magnetic Resonance (2017)
-
Human heart disease: lessons from human pluripotent stem cell-derived cardiomyocytes
Cellular and Molecular Life Sciences (2017)
-
Disease modeling and lentiviral gene transfer in patient-specific induced pluripotent stem cells from late-onset Pompe disease patient
Molecular Therapy - Methods & Clinical Development (2015)
-
Effect of enzyme replacement therapy in late onset Pompe disease: open pilot study of 48 weeks follow-up
Neurological Sciences (2015)