Abstract
Purpose
Genomics services have the potential to reduce incidence and mortality of diseases by providing individualized, family health history (FHH)-based prevention strategies to clients. These services may benefit from the involvement of community health workers (CHWs) in the provision of FHH-based genomics education and services, as CHWs are frontline public health workers and lay health educators, who share similar ethnicities, languages, socioeconomic statuses, and life experiences with the communities they serve. We developed, implemented, and evaluated the FHH-based genomics training program for CHWs.
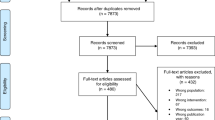
Methods
This theory- and evidence-based FHH-focused genomics curriculum was developed by an interdisciplinary team. Full-day workshops in English and Spanish were delivered to 145 Texas CHWs (91.6% were Hispanic/black). Preworkshop, postworkshop, and 3-month follow-up data were collected.
Results
CHWs significantly improved their attitudes, intention, self-efficacy, and knowledge regarding adopting FHH-based genomics into their practice after the workshops. At 3-month follow-up, these scores remained higher, and there was a significant increase in CHWs’ genomics practices.
Conclusion
This FHH-based genomics training successfully educated Texas CHWs, and the outcomes were promising. Dissemination of training to CHWs in and outside of Texas is needed to promote better access to and delivery of personalized genomics services for the lay and underserved communities.
Similar content being viewed by others
Introduction
Personalized or precision genomics services have the potential to reduce incidence, morbidity, and mortality of diseases by providing individualized, tailored prevention strategies to clients.1 One of the pivotal elements of personalized or precision genomics services is family health history (FHH).2,3 According to the risk stratification model, a comprehensive personalized genomics service requires individuals to first collect their FHH, which should then be translated into a FHH pedigree—an initial screening tool—to identify the risk levels for various diseases. These risk levels include an average risk (i.e., one similar to the general population’s risk), a moderate risk (i.e., one slightly higher than the general population’s risk), and a high risk (i.e., one significantly higher than the general population’s risk). Upon stratification, individuals can receive personalized recommendations tailored to their risk levels (e.g., further genetic evaluation and testing, screening at earlier ages, and/or individualized lifestyle changes).2,3
Genetics specialists are the ideal providers of FHH-based genomics services, yet several challenges exist. First, the number of genetics specialists (2,757 geneticists4 and 3,100 genetic counselors5) in the United States is insufficient, creating challenges in meeting the growing public demand.6,7 Second, genetics specialists are often located in high-density urban areas and large medical centers, leading to inequity in the genomics services between urban and rural areas.6,8 Third, within the limited amount of time allotted to a medical appointment, it is difficult for genetics specialists to guide, support, and monitor patients’ health behavior changes. Fourth, some patients may not have a comprehensive FHH and/or adequate genomic literacy to understand complex genomic information.9,10,11,12 Fifth, many racial/ethnic minorities are less likely to engage with genomics services,8,13 which precludes them from receiving relevant benefits.
Because of the above challenges, FHH-based genomics services can benefit from the involvement of community health workers (CHWs) in the provision of fundamental FHH-based genomics education and services to lay individuals and communities.14,15 There are 51,900 CHWs in the United States,16 with different levels of education (i.e., high school diploma or less, some college or an associate degree, and a bachelor’s degree or higher) and work/volunteer settings (e.g., health care, school, government, and community).17 CHWs are frontline public health workers and lay health educators, who have similar ethnicities, languages, socioeconomic statuses, and life experiences to those of the people they serve.18 The duties of CHWs are to help communities and individuals gain access to the necessary services and establish their capacity “by increasing health knowledge and self-sufficiency through a range of activities such as outreach, patient navigation and follow-up, community health education and information, informal counseling, social support, advocacy, and participation in clinical research.”19 Being constantly involved in communities, the trust of the community members enables CHWs to serve as the bridge between those communities and health-care (genomics) services.18
Although CHWs represent a potentially capable and culturally competent workforce in genomics, CHWs have been overlooked in genomics training and therefore lack the genomics competencies needed to provide fundamental FHH-based genomics education and services.7,20 The Centers for Disease Control and Prevention,21 the National Academy of Medicine,22 and the American Public Health Association23,24 have advocated the importance of educating CHWs. Nevertheless, CHWs have not received formal education/degrees in public health at school and thus are considered “nonprofessional public health workers.” Hence, along with the complexity of the subject of genomics, providing genomics training for CHWs has been perceived as a challenge.7
To address the need and the challenges in genomics education for CHWs, we developed and evaluated the FHH-focused genomics training program tailored for CHWs in Texas, taking into account the CHWs’ demographics, competencies, skills, education levels, and work settings. In showing the outcome of this training program, we report its positive effects on (i) CHWs’ attitudes, intention, and self-efficacy in providing fundamental FHH-based genomics education and services and (ii) their FHH-based genomics knowledge and practices. Participating CHWs’ assessment of the training is also presented.
Materials and methods
FHH-based genomics training curriculum
This study was approved by Texas A&M University’s Institutional Review Board. Working with a certified CHW instructor (CHWI) and health educator (D.S.), we adapted the eight-module curriculum of the FHH-based genomics education for health educators to be tailored to the competencies, educational levels, backgrounds, and work settings of CHWs. The curriculum, based on the Social Cognitive Theory,25 Theory of Planned Behavior,26 and Diffusion of Innovations Theory,27 was developed by an interdisciplinary team of health educators, geneticists, and genetic counselors with the guidance of an advisory board, which included nurses, dieticians, geneticists, genetic counselors, health education practitioners, and genomics education and professional development experts. The curriculum was sent to two additional genetic counselors and one health educator who is a leader in the genomics forum at the American Public Health Association for content validation and pilot testing with five health educators. As health educators and CHWs are both health-education team members with similar scopes of work, revising the curricula for health educators to meet CHWs’ needs and match their training was feasible.
The eight modules of the curriculum are composed of 20 parts, each with a learning objective (Table 1). The curriculum was later translated into Spanish. Pilot tests were conducted for the curricula with six English-speaking CHWs and eight Spanish-speaking CHWs. The curricula were revised based on the pilot testing results and then sent to the Texas Department of State Health Services (TDSHS) for review. The approval for six state-certified continuing education units for the CHWs was obtained (the final English and Spanish training curricula are available upon request to the corresponding author).
CHW recruitment and delivery of the training workshops
To recruit CHWs for this training program, an e-mail with registration information for the workshops was sent to every CHW in Texas. We also invited CHWs to attend the workshops through our own networks. Incentives (free registration, a $25 electronic gift card, six state-certified continuing education units, a training certificate, and complimentary refreshment) were used to motivate CHWs to attend the workshops. A bilingual CHWI (D.S.) delivered two full-day workshops in English and Spanish. Each participant was provided with a binder consisting of an information sheet, an overview of the project, printouts of the PowerPoint presentation, a mock case-study sheet, printed copies of the Surgeon General’s “My Family Health Portrait,”28 a list of genetic service providers in Texas, a glossary of the key terminologies, references, and resources, a FHH-based lifestyle recommendation table, and FHH-based genetic evaluation recommendation guidelines. The list of genetic service providers in Texas included the contact information of all genetic clinics and genetic counselors across Texas, allowing high-risk clients to choose and visit genetic professionals based on their preference and/or geographic proximity.
The morning session of the workshops focused on modules 1–4. Along with the lectures, participants watched a video which used a scenario depicting a Latina woman with a FHH of breast cancer to demonstrate how to create a FHH pedigree using the Office of the Surgeon General’s “My Family Health Portrait” tool online.28 The CHWI (D.S.) and a bilingual Hispanic team member also illustrated how to collect FHH and provide personalized lifestyle recommendations using role play. Participants were then asked to pair up and participate in a hands-on practice of FHH collection and lifestyle recommendations. Modules 5–8 were covered in the afternoon session, in which mock case studies with FHHs of cancers were demonstrated in addition to the lectures. Participants were divided up into small groups to determine whether the person in the case study should be referred to a genetic professional, based on the FHH pedigree of each case. At the end of each workshop, learning objectives and key summaries for all modules were presented.
Measurements
A preworkshop survey was administered before the start of the workshop. After the workshop, CHWs immediately completed the postworkshop survey. Each participant received three e-mails, one postcard, and one phone call asking them to complete the 3-month follow-up survey online, with a $10 electronic gift card as an incentive. The preworkshop, postworkshop, and 3-month follow-up surveys included:
-
1.
An 18-item attitudes scale (e.g., “how much do you agree or disagree that CHWs should help identify high-risk clients based on their FHH information for genetic evaluation and testing?”)
-
2.
A 13-item intention scale (e.g., “how likely are you to include FHH assessments in your routine work?”)
-
3.
A 13-item self-efficacy scale (e.g., “how confident are you that you can help find genetic services for high-risk clients?”)
-
4.
A knowledge scale with 24 multiple-choice questions
The preworkshop survey consisted of additional demographic questions, and the postworkshop survey included other open-ended and multiple-choice questions to collect participants’ feedback on the workshops. Behavior measures regarding adopting FHH-based genomics practices were assessed using 11 items in the preworkshop and 3-month follow-up surveys. An additional 16 items related to the clients served by the CHWs after the FHH training were included in the 3-month follow-up survey.
Data analysis
The scales of attitudes, intention, self-efficacy, knowledge, and behavior were examined for internal consistency (i.e., Cronbach’s alpha) and for construct validity (i.e., confirmatory factor analysis), and they were psychometrically sound. Content analysis was utilized to assess open-ended questions. Utilizing Mplus 8.0 (Muthén & Muthén, Los Angeles, CA) for the structural equation modeling approach with a maximum likelihood estimation and a robust standard errors method,29 we conducted paired t-tests to examine the changes in participants’ attitudes, intention, self-efficacy, knowledge, and behavior as shown in the preworkshop, postworkshop, and 3-month follow-up surveys. A full information maximum likelihood estimation method was used for the missing data.30 An attrition analysis was performed using SPSS 22.0 (IBM Corporation, Armonk, NY) by assessing the patterns of differences in participants’ sociodemographic information and outcome variables between attritors and non-attritors in the preworkshop, postworkshop, and 3-month follow-up surveys.
Results
Characteristics of workshop participants
A total of 145 CHWs attended the workshops (n = 95 for the English workshop and n = 50 for the Spanish workshop). Most of the participants were females (84.0%) and ethnic minorities (69.9% Hispanics and 21.7% blacks); had very little, if any, training in genomics (96.2%); and worked in community (53.1%) or health-care (32.7%) settings. Participants’ average age was 46.0 years (range 22–68). About one-third (33.8%) had bachelor’s degrees or above; some had a high school diploma or lower (19.9%), and the others had attended some college or had associate degrees (46.3%). Except for one participant in the English workshop, the participants completed the immediately-postworkshop survey. Furthermore, 87 participants completed the 3-month follow-up survey.
Attitudes, intention, and self-efficacy in adopting FHH-based genomics in practice
After the workshop, the immediately-posttraining data showed that attitudes (mean = 12.2; SD = 3.2; P < 0.001), intention (mean = 3.4; SD = 0.6; P < 0.001), and self-efficacy (mean = 8.2; SD = 2.0; P < 0.001) were significantly improved compared with the preworkshop scores (mean = 10.1; SD = 3.1 for attitudes; mean = 3.0; SD = 0.6 for intention; mean = 6.9; SD = 2.5 for self-efficacy). Although the decreases in the attitudes (mean = 10.8; SD = 3.3; P < 0.001), intention (mean = 3.1; SD = 0.6; P < 0.001), and self-efficacy (mean = 7.1; SD = 2.3; P < 0.001) scores were statistically significant compared with the postworkshop values, the 3-month follow-up scores remained significantly higher than those in the preworkshop survey (Table 2).
FHH-based genomics knowledge
The preworkshop knowledge mean score was 0.4 (SD = 0.1), which indicated that participants answered only 40% of the knowledge items correctly. After the training, the immediately-postworkshop knowledge scores significantly increased (mean = 0.6; SD = 0.1; P < 0.001) and sustained the improvement at 3-month follow-up (mean = 0.5; SD = 0.1; P < 0.001) compared with the preworkshop scores (Table 2).
FHH-based genomics practice
As seen in Table 2, compared with the preworkshop value (mean = 2.2; SD = 1.0), the behavior score was significantly higher in the 3-month follow-up (mean = 2.6; SD = 1.2; P = 0.005). Further analyses were conducted to examine each behavioral item. Seven behaviors showed a significant improvement from preworkshop to 3-month follow-up: (i) assisting clients in creating their FHH trees using the Surgeon General’s “My Family Health Portrait” tool (P < 0.001), (ii) encouraging clients to edit and/or add information to their FHH (P = 0.012), (iii) providing information to clients about genetic testing (P = 0.025), (iv) providing information to clients about genetic evaluations (P < 0.001), (v) identifying high-risk clients based on their FHH information (P = 0.035), (vi) helping find genetic services for high-risk clients (P < 0.001), and (vii) recommending high-risk clients for genetic evaluation and genetic testing (P < 0.001). Despite the absence of statistical significances, the four remaining behaviors all showed an increase from preworkshop to 3-month follow-up: (i) incorporating FHH assessments in CHWs’ routine work (P = 0.12), (ii) making appropriate behavioral or lifestyle recommendations to clients based on their FHH (P = 0.39); (iii) encouraging clients to consult relevant health-care providers about their FHH (P = 0.11); and (iv) encouraging clients to discuss their FHH with other family members (P = 0.22).
The 3-month follow-up results regarding the number of clients served and their behavior changes are shown in Table 3. Within 3 months, each CHW served an average of 16.3 clients (range 0–200) with regard to the FHH education, services, and outreach. Of these clients, each CHW conducted FHH assessments for approximately 14.4 clients and provided information regarding genetic testing and evaluation to about 11 clients. The means for the number of clients who had been encouraged to consult health-care providers about their FHH by each CHW and for the number of clients who had actually discussed FHH with their health-care providers were 14.7 and 8.5 respectively. Similarly, on average each CHW encouraged 14.1 clients to discuss their FHH with their family members, and 12 clients completed it. Furthermore, 7.4 clients per CHW had changed their lifestyles based on the recommendations provided by the CHWs. High-risk clients had been recommended for genetic evaluation and testing (mean = 4.8 per CHW), and 1.8 clients visited genetic professionals.
In the 3-month follow-up survey, participants were also asked to indicate barriers encountered in implementing FHH-based genomics. Its being outside the scope of their work was found to be the main barrier (e.g., “the type of work that I am currently involved in often does not afford me the opportunity to do this.”) Conversely, the notion of helping communities and clients was the leading motivator for CHWs in adopting FHH-based genomics practice. For example, “helping the community to improve their quality of life or prevent illnesses” was a motivator as reported by a CHW.
Workshop assessment
In the postworkshop assessment, the majority of CHWs either “agreed” or “strongly agreed” that our workshop was timely in terms of the public health practice. They also believed that the presenters mastered the topic (95%) and delivered the workshop effectively (90.7%). Moreover, participants were either “very satisfied” or “satisfied” with the order of modules (94.2%), the difficulty level of the materials (95.7%) as well as the organizations (95.7%) and the learning experience (95%) in the workshop. Nearly all (97.9%) of the participants said they were either “very willing” or “willing” to recommend this workshop to other CHWs, and 98.6% believed that other CHWs would take this training. Within 3 months, over half of the participants (55.2%) recommended our workshop to their colleagues. In addition to the quantitative data, qualitative data revealed that participating CHWs generally had positive feedback about the workshop. Participants found the workshop to be informative and enjoyed the role-play activities and the case studies. Some participants suggested hosting these workshops more often to help them and other CHWs serve their communities better. A few minor suggestions for improving the workshop included making the workshop more interactive, presenting more examples, having longer breaks, shortening the workshop, and delivering the curriculum on a Web-based platform.
Nearly all (97.8%) of the participants reported that the workshop assisted them in understanding how to conduct FHH-based education and services. We asked CHWs to rate the extent to which they believe that they could achieve each learning objective as a result of this training. Most of them said they either “strongly agreed” or “agreed” that they could meet those objectives (mean = 87.1; SD = 4.7; range = 77.1–94.3). Part 1 of module 1 had the highest rating; 94.3% of the CHWs indicated that after attending the workshop, they would be able to define the term “FHH” in health promotion. In contrast, part 3 of module 5 had the lowest rating; 77.1% of the CHWs strongly agreed/agreed that after the workshop they would be able to describe the “analytic validity, clinical validity, clinical utility, and ethical, legal, and social implications (ACCE) model,” which is used to evaluate genetic testing ( Table 1 ). Beyond assessing the learning objectives, 97.2% of the participants stated that they would be willing to learn more about FHH, genetic evaluation, genetic testing, and genomics in the future. The 3-month follow-up survey showed that 25% of the participants looked for such information by themselves.
Discussion
More than a decade has passed since the completion of the Human Genome Project, but the adoption of genomics in public health remains slow.31,32 One of the main factors is the lack of training among public health professionals.7,20,33 To the best of our knowledge, this is one of the first genomics training programs for CHWs,15,20 and it was a success. Participants’ attitudes, intention, self-efficacy, and knowledge regarding adopting FHH-based genomics into their practice were improved immediately after the workshops. Scores for those abilities remained higher at 3-month follow-up than in the preworkshop data. Moreover, CHWs’ FHH-based genomics practices significantly increased. These CHWs served many clients who collected their FHH, changed unhealthy lifestyles, and received education about genetic testing and evaluation. CHWs had also identified high-risk clients, who then visited genetic professionals for genetic evaluation.
Because CHWs are indispensable public health professionals who undertake community outreach and education, they can collaborate with genetic professionals to offer basic FHH-based genomics education and services to individuals and communities to increase genomic literacy and access to genetic services.14 Furthermore, CHWs are often from racial/ethnic minorities.17 In this study, 91.6% of the participating CHWs were Hispanic or black. As racial/ethnic minority communities are frequently underserved in genomics services,8,13 and there has been an issue with mistrust in health-care systems,8,34 CHWs with minority backgrounds may be a resource for mitigating these challenges by serving as a bridge between the underserved communities and genetic service providers, to promote better utilization of genomics services and to minimize genomics-related health disparities.
Notably, the behavior scale, which was computed as the mean of 11 behavior questions, significantly improved from the preworkshop survey to the 3-month follow-up. However, further analysis indicated that four items were found not to be statistically significant, which might be a result of the small number of participants who completed the 3-month follow-up survey. In addition, several participants skipped behavioral questions because they were listed at the end of the survey. Although the attrition analysis showed no significant differences between attritors and non-attritors in the sociodemographic and outcome scores, it is still imperative to reduce the attrition rate for behavior items. Future research is recommended to train a larger number of CHWs and place behavior items in the beginning of the survey.
Interestingly, the baseline knowledge scores in the beginning of the workshop were low; participants answered only 40% of the questions correctly. The knowledge scores significantly improved after the workshop. Nevertheless, the postworkshop knowledge scores remained low, with an accuracy of merely 60%, although most participants reported that they could meet the learning objectives for each module. We suspected that the information presented in a full-day workshop might be overwhelming for the CHWs. Additionally, 24 knowledge questions might be too many for the CHW training, especially when some knowledge questions required participants to memorize the genetic-evaluation recommendation guidelines. Thus, reducing the context of the training materials, presenting key information in the workshop, dividing the workshop materials over several days, and allowing participants to refer to the training materials for applied questions might be helpful to enhance CHWs’ comprehension of genomics training materials.
Regarding learning objectives, part 3 of module 5 (“being able to describe the ACCE model, which is used to evaluate genetic testing”) had the lowest rating of understanding. Although the ACCE model proposed by the Centers for Disease Control and Prevention35 is a useful framework in which to evaluate genetic tests, this model might be more important for genetic professionals in determining which genetic test they should offer to their patients. For CHWs who do not have formal degrees in public health, it may be necessary to simplify such information and make it more practically applicable. Specifically, instead of defining analytic validity, clinical validity, clinical utility, and the associated ethical, legal, and social implications of the ACCE model, it may be sufficient to (i) emphasize that genetic testing is not “one size fits all” and that there is an evaluation system for use by genetic professionals to determine which test is appropriate and (ii) simply discuss the ethical, legal, and social implications of genetic testing.
The results of this study are promising, but some limitations should be discussed. The first is the self-reported nature of the behavioral data, which have commonly been used to evaluate the effectiveness of genomics training for health professionals.20 We relied on CHWs’ self-reporting because it was challenging to directly collect clients’ data in this study owing to the variability in the CHWs’ work settings and the large numbers of their clients. Moreover, it is unlikely that CHWs would report inaccurate data since they were aware that the data were utilized for research purposes and they would receive the same incentives regardless of the numbers of clients they served. Future organizers of training, however, might consider approaching CHWs in a specific setting and further collecting data from their clients and/or their health-care providers directly. Second, our workshops might have attracted CHWs who were already motivated to implement genomics or FHH in their practice. It is imperative for future research to reach and educate CHWs who either are not overtly interested in these topics or are not planning to incorporate FHH into their work. Third, as is done in most genomics training for nongenetics health professionals,20 we adopted a pre- and posttest design. More rigorous study designs, such as randomized controlled trials, may be considered in the future. Fourth, we report only 3-month follow-up data in this paper. Intermediate and long-term follow-up data are needed to assess the changes in behavior and associated factors among CHWs over time. Finally, although we used various approaches (e-mails, postcards, and phone calls) and incentives ($10 gift cards) for the workshop participants, the 3-month follow-up rate was not as high as desired (60.4%). Nevertheless, our follow-up rate is within the ranges reported in similar studies with CHW participants (59.5–71.5%).36,37
Another factor worth noting is that as we were developing this first theory-based, FHH-focused genomics training program for CHWs, our target population was lay health educators who had not received formal training in public health. We started our genomics training with CHWs in Texas because Texas is one of the few states in the United States that has an official training and certification program for CHWs, which is regulated by the TDSHS.7,38 In order to be certified as a CHW in Texas, one must be a Texas resident who has conducted more than 1,000 h of community health outreach within 6 years or has completed 160 h of training in health promotion (provided by TDSHS-approved CHW training centers),39 which covers eight CHW competencies: Communication, Teaching, Organization, Advocacy, Interpersonal Skills, Service Coordination, Capacity Building, and Knowledge Base.40 Once certified by the TDSHS, as a state rule, CHWs must obtain 20 continuing education units every 2 years to maintain their certification (at least 10 units are needed to be TDSHS-certified).39 Recruiting from this population in our study enabled us to take the first step in demonstrating the value and success of this FHH-based genomics training program for CHWs. Researchers might consider implementing similar training programs for non-Texas CHWs in the future. However, more obstacles may surface and impact the training procedure and outcomes, if those states do not have certification or training requirements for CHWs. In view of this, it is essential to establish a national standard in certifying and regulating CHWs in the United States to ensure that all CHWs have a certain level of knowledge and experience to facilitate their learning in genomics.
In summary, this genomics training for CHWs successfully educated CHWs in Texas (most of whom were racial/ethnic minorities), and the outcomes were promising. We addressed the concern raised by the genomics field by showing improvement in Texas CHWs’ attitudes, intention, self-efficacy, knowledge, and behavior after the genomics training.7 Although our curriculum covered a variety of diseases, in-depth training focusing on a specific disease might be developed for CHWs who provide services and education involving that disease. Given that CHWs play an important role in community outreach and education, disseminating our training program in and outside Texas is vital in promoting better access to and delivery of personalized or precision genomics service for the lay and underserved communities in the United States.
References
Jameson JL, Longo DL. Precision medicine—personalized, problematic, and promising. N Engl J Med 2015;372:2229–2234.
Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med 2002;4:304–310.
Yoon PW, Scheuner MT, Khoury MJ. Research priorities for evaluating family history in the prevention of common chronic diseases. Am J Prev Med 2003;24:128–135.
American Board of Medical Genetics.Number of certified specialists in genetics. 2016. http://www.abmgg.org/pdf/Modified%20Statistics%20for%20all%20years%20end%20date%202015%20with%20footnotes.pdf. Accessed 28 October 2017.
Bureau of Labor Statistics, US Department of Labor. Occupational outlook handbook, 2016-17 edition, genetic counselors. 2017. https://www.bls.gov/ooh/healthcare/genetic-counselors.htm. Accessed 8 December 2017.
Radford C, Prince A, Lewis K, Pal T. Factors which impact the delivery of genetic risk assessment services focused on inherited cancer genomics: expanding the role and reach of certified genetics professionals. J Genet Couns 2014;23:522–530.
Secretary’s Advisory Committee on Genetics Health and Society, U.S. Department of Health & Human Services. Genetics education and training. 2011. https://www.genome.gov/pages/careers/healthprofessionaleducation/sacghs-educationreport2011.pdf. Accessed 28 October 2017.
Forman AD, Hall MJ. Influence of race/ethnicity on genetic counseling and testing for hereditary breast and ovarian cancer. Breast J 2009;15:S56–S62.
Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics 2011;14:279–289.
Syurina E, Brankovic I, Probst-Hensch N, Brand A. Genome-based health literacy: a new challenge for public health genomics. Public Health Genomics 2011;14:201–210.
Centers for Disease Control and Prevention. Awareness of family health history as a risk factor for disease—United States, 2004. MMWR Morb Mortal Wkly Rep 2004;53:1044.
Welch BM, O’connell N, Schiffman JD. 10 years later: assessing the impact of public health efforts on the collection of family health history. Am J Med Genet A 2015;167:2026–2033.
Shields AE, Burke W, Levy DE. Differential use of available genetic tests among primary care physicians in the US: results of a national survey. Genet Med 2008;10:404.
Allen CG, McBride CM, Balcazar HG, Kaphingst KA. Community health workers: an untapped resource to promote genomic literacy. J Health Commun 2016;21(suppl 2):25–29.
Kaphingst KA, Lachance CR, Gepp A, Hoyt D’Anna L, Rios-Ellis B. Educating underserved latino communities about family health history using lay health advisors. Public Health Genomics 2011;14:211–221.
Bureau of Labor Statistics, US Department of Labor. Occupational outlook handbook, 2016-17 edition, community health workers. 2017. https://www.bls.gov/oes/current/oes211094.htm. Accessed 28 October 2017.
Arizona Prevention Research Center, The University of Arizona. 2014 National Community Health Worker Advocacy Survey Reports: National Report. 2014. https://azprc.arizona.edu/sites/default/files/pdf/12Nov14%20NATIONAL.pdf. Accessed 28 October 2017.
Nemcek MA, Sabatier R. State of evaluation: community health workers. Public Health Nurs 2003;20:260–270.
Texas Department of State Health Services. Community health workers—promotor(a) or community health worker training and certification program. 2017. http://www.dshs.texas.gov/mch/chw.shtm. Accessed 28 October 2017.
Talwar D, Tseng T-S, Foster M, Xu L, Chen L-S. Genetics/genomics education for nongenetic health professionals: a systematic literature review. Genet Med 2017;19:725–732.
Center for Disease Control and Prevention. Genomic workforce competencies. 2010. https://www.cdc.gov/genomics/translation/competencies/. Accessed 28 October 2017.
Institute of MedicineWho Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century. Washington, DC: National Academies Press, 2003.
American Public Health Association. Strengthening genetic and genomic literacy. 2010. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/30/16/37/strengthening-genetic-and-genomic-literacy. Accessed 28 October 2017.
American Public Health Association. Advancing cancer genomics in public health. 2013. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/23/10/25/advancing-cancer-genomics-in-public-health. Accessed 28 October 2017.
Kelder S, Hoelscher D, Perry CHow individuals, environments, and health behaviors interact. In: Glanz K, Rimer B, Viswanath K(eds). Health Behavior: Theory, Research, and Practice. 5th ed. New York: Wiley, 2014: 159–182.
Montano D, Kasprzyk DTheory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer B, Viswanath K(eds). Health Behavior: Theory, Research, and Practice. 5th ed. New York: Wiley, 2014: 95–124.
Brownson R, Tabak R, Stamatakis K, Glanz KImplementation, dissemination, and diffusion of public health interventions. In: Glanz K, Rimer B, Viswanath K(eds). Health Behavior: Theory, Research, and Practice. 5th ed. New York: Wiley, 2014: 301–326.
Office of the Surgeon General. My Family Health Portrait tool. 2017. https://familyhistory.hhs.gov/FHH/html/index.html. Accessed 28 October 2017.
Muthén B, Muthén L. Mplus User’s Guide. 8th ed. Los Angeles, CA: Muthén & Muthén, 2017.
Enders CK. Applied Missing Data Analysis. New York: Guilford Press, 2010.
McBride CM, Bowen D, Brody LC et al. Future health applications of genomics: priorities for communication, behavioral, and social sciences research. Am J Prev Med 2010;38:556–565.
Ozdemir V, Burke W, Khoury MJ, Knoppers BM, Zimmern RGenomics and public health. In: Detels R, Gulliford M, Karim QA, Tan CC(eds). Oxford Textbook of Global Public Health. 6th ed. Oxford, UK: Oxford University Press, 2015.
Khoury MJ, Bowen MS, Burke W et al. Current priorities for public health practice in addressing the role of human genomics in improving population health. Am J Prev Med 2011;40:486–493.
Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health 2007;97:1283–1289.
Centers for Disease Control and Prevention. ACCE model process for evaluating genetic tests. 2010. https://www.cdc.gov/genomics/gtesting/acce/. Accessed 28 October 2017.
Holt CL, Santos SLZ, Tagai EK et al. Using technology for improving population health: comparing classroom vs. online training for peer community health advisors in African American churches. Implement Sci 2015;10(suppl 1):A60.
Josiah Willock R, Mayberry RM, Yan F, Daniels P. Peer training of community health workers to improve heart health among African American women. Health Promot Pract 2015;16:63–71.
Association of State and Territorial Health Officials. CHW certification and training information. 2017. http://www.astho.org/Public-Policy/Public-Health-Law/Scope-of-Practice/CHW-Certification-Standards-Map/. Accessed 28 October 2017.
Texas Department of State Health Services. Community health workers - certification information. 2017. http://www.dshs.texas.gov/mch/chw/chwdocs.aspx. Accessed 8 December 2017.
Texas Department of State Health Services. Community health workers’ core competencies. 2017. http://www.dshs.texas.gov/mch/chw/docs/Core-CompetencyAreasPg.pdf. Accessed 28 October 2017.
Acknowledgments
This study was funded through the Prevention Grants from the Cancer Prevention and Research Institute in Texas (PP140210 and PP170015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, LS., Zhao, S., Stelzig, D. et al. Development and evaluation of a genomics training program for community health workers in Texas. Genet Med 20, 1030–1037 (2018). https://doi.org/10.1038/gim.2017.236
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.236
Keywords
This article is cited by
-
Development of a Hereditary Breast and Ovarian Cancer and Genetics Curriculum for Community Health Workers: KEEP IT (Keeping Each other Engaged Program via IT) Community Health Worker Training
Journal of Cancer Education (2024)
-
Development of a community health workers perceptual and behavioral competency scale for preventing non-communicable diseases (COCS-N) in Japan
BMC Public Health (2022)
-
Driving the precision medicine highway: community health workers and patient navigators
Journal of Translational Medicine (2019)
-
Family health history and genetic services—the East Baltimore community stakeholder interview project
Journal of Community Genetics (2019)