Abstract
Purpose
Heterozygous germ-line activating mutations in PDGFRB cause Kosaki and Penttinen syndromes and myofibromatosis. We describe a 10-year-old child with a germ-line PDGFRB p.N666H mutation who responded to the tyrosine kinase inhibitor imatinib by inhibition of PDGFRB.
Methods
The impact of p.N666H on PDGFRB function and sensitivity to imatinib was studied in cell culture.
Results
Cells expressing the p.N666H mutation showed constitutive PDGFRB tyrosine phosphorylation. PDGF-independent proliferation was abolished by imatinib at 1 μM concentration. Patient fibroblasts showed constitutive receptor tyrosine phosphorylation that was also abrogated by imatinib with reduced proliferation of treated cells.
This led to patient treatment with imatinib at 400 mg daily (340 mg/m2) for a year with objective improvement of debilitating hand and foot contractures, reduced facial coarseness, and significant improvement in quality of life. New small subcutaneous nodules developed, but remained stable. Transient leukopenia, neutropenia, and fatigue resolved without intervention; however, mildly decreased growth velocity resulted in reducing imatinib dose to 200 mg daily (170 mg/m2). The patient continues treatment with ongoing clinical response.
Conclusion
To our knowledge, this is one of the first personalized treatments of a congenital disorder caused by a germ-line PDGF receptor mutation with a PDGFRB inhibitor.
Similar content being viewed by others
Introduction
Exome sequencing has emerged as a powerful diagnostic tool for identifying rare diseases of previously unknown etiology. As clinical use of this technology becomes more widespread, new genetic causes of disease are being identified and new phenotypes are being associated with previously known disease genes. One benefit of being able to identify the genetic cause of disease is to end the “diagnostic odyssey.” A less frequent but equally desirable benefit is the identification and implementation of an effective treatment plan for the patient with a rare genetic condition, which in some cases includes already available pharmaceutical compounds. Herein, we report a case where both benefits were achieved through the use of exome sequencing.
The platelet-derived growth factor family includes four growth factors (PDGF-A, -B, -C, and -D) that bind to two receptors (PDGFRα and PDGFRβ). The receptors are cell surface tyrosine kinase receptors that activate pathways leading to cell proliferation, growth, motility, and differentiation.1, 2, 3 PDGFRA (MIM 173490) and PDGFRB (MIM 173410), encoding PDGFRα and β respectively, are expressed in cell types of mesenchymal origin, such as fibroblasts and vascular smooth muscle cells.4
In contrast to many other receptor tyrosine kinases, mutations in PDGFRB are found in only a few conditions. As of 2015, mutations in the PDGFRB gene were known to cause at least five different phenotypes: idiopathic basal ganglia calcification, type 4 (MIM 615007); infantile myofibromatosis (MIM 228550); Kosaki overgrowth syndrome (MIM 616592); myeloproliferative disorder with eosinophilia (MIM 131440); and premature aging syndrome, Penttinen type (MIM 601812). Idiopathic basal ganglia calcification is caused by loss-of-function mutations, and myeloproliferative disorder with eosinophilia is caused by an acquired translocation that results in fusion of ETV6 (MIM 600618) and PDGFRB. The other three phenotypes—Kosaki, myofibromatosis, and Penttinen—are all caused by heterozygous germ-line activating mutations in PDGFRB. These conditions share overlapping phenotypic features, suggesting they may represent a spectrum of possible outcomes from activating mutations in PDGFRB.
Three germ-line mutations in PDGFRB have been reported to cause infantile myofibromatosis: p.R561C in 16 different families, and p.K567E and p.P660T each in one family.5, 6, 7, 8, 9, 10 Kosaki syndrome was described in two patients carrying a p.P584R substitution,11 while Penttinen was described in four unrelated patients with a p.V665A mutation.12 These substitutions were shown to constitutively activate PDGFRB, supporting the hypothesis that they cause disease.11, 12 In 2016, Arts et al. demonstrated that germ-line PDGFRB mutations promote the active confirmation of PDGFR in the absence of ligand, resulting in constitutive activation of downstream signaling pathways.13 These mutations were shown to be sensitive to tyrosine kinase inhibitors (TKIs) in vitro, suggesting their possible use as therapeutic agents in individuals with PDGFRB activating mutations.
The first generation TKI imatinib inhibits abnormally activated PDGFRA and PDGFRB by interfering with constitutively activated tyrosine kinase domains. This results in clinical response in myeloid malignancies with the PDGFRB fusion genes,14 dermatofibrosarcoma protuberans (MIM 607907) with the COL1A1-PDGFB fusion,15 idiopathic hypereosinophilic syndrome (MIM 607685) and its variants with the FIP1L1 (MIM 607686)–PDGFRA fusion,16 and gastrointestinal stromal tumors with PDGFRA mutations.17 We hypothesized that imatinib should have a similar effect on the activation of PDGFRB due to gain-of-function point mutations.
This hypothesis was tested in a patient with a complex clinical presentation whose clinical exome analysis results revealed a de novo heterozygous PDGFRB mutation, c.1996A>C (p.N666H). The patient underwent skin biopsy and fibroblasts showed constitutive tyrosine phosphorylation, which was abrogated by 1 μM of imatinib in vitro. Here we describe the marked clinical response of the patient to imatinib administration.
Materials and methods
The Institutional Review Board of Children’s Minnesota approved this publication. The patient’s parents consented to this publication and were provided with the manuscript before submission. The patient’s parents were counseled and consented in regard to clinical exome analysis, which was performed in a CLIA/CAP-certified reference laboratory as part of his clinical evaluation.
The patient was born after an unremarkable pregnancy and delivery; there was no polyhydramnios or other obvious pregnancy complications. Birth parameters included weight 4.2 kg (>95th percentile) and length 55.8 cm (>95th percentile). A hemangioma of the left chest wall, present at birth, was removed at 2 months of age. Sagittal craniosynostosis was first noted on the second day of life when a ridge formed on the back of his head. Surgical correction occurred at 5 months of age. He developed macrocephaly by 19 months of age that has persisted. Initial magnetic resonance imaging (MRI) at 6 months of age showed a large cisterna magna later described as a retrocerebellar cyst without evidence of a Dandy–Walker malformation. Subsequent MRIs have shown two cysts: a moderate-size retrocerebellar cyst and right middle cranial fossa arachnoid cyst that have persisted in size. At 4 years of age MRI of the brain revealed a left lateral orbital wall temporal bone dermoid cyst that, in retrospect, may have been a myofibroma that spontaneously resolved.
The most medically debilitating problem for this child developed between 5 and 7 years of age with progressive deformation of his hands. He developed brachydactyly and acro-osteolysis, brachymetacarpia with widened metacarpals and poor tubularization, and short broad phalanges with wider metaphyseal portions. He was diagnosed with carpal tunnel syndrome. The hand surgeon noted the synovium was quite thick and abnormal in appearance at the time of surgical release at 7.5 years. Pathology examinations for storage material and electron microscopy were negative. An inclusion cyst from his right index finger was removed at the time of his carpal tunnel release.
At 3 years old there were no concerns on dental exam. By 6 years old he developed gingival hypertrophy with multiple cysts, which were removed at age 8 years to facilitate tooth eruptions. A second procedure was required the following week to “unroof the gums,” allowing the teeth to erupt. His facial features progressed with time, becoming coarser with his hair becoming sparser.
In summary, this boy initially presented with a hemangioma requiring surgical removal, sagittal craniosynostosis, and intracranial cysts. With time he developed a cyst on his index finger, gingival hypertrophy requiring surgical release, and acro-osteolysis changes in the hands with progressive brachydactyly, contractures, and carpal tunnel syndrome. Throughout there were no intellectual concerns; his development was normal and he did well intellectually in school.
Extensive diagnostic testing was pursued beginning at 4 months old with no definitive diagnosis provided, including craniosynostosis genetic testing, Simpson–Golabi–Behmel syndrome genetic testing, and enzyme and genetic testing for storage disorders. Ultimately, clinical exome sequencing on the trio consisting of the patient and both parents was performed at 6.5 years old on blood. The testing was performed at Ambry Genetics as described by Farwell et al. in 2015.18 Initial results were negative; reanalysis a year later revealed a heterozygous PDGFRB mutation, c.1996A>C (p.N666H) classified as “likely deleterious.” The variant was submitted to ClinVar (accession number SCV000244150.3).
Evidence in the exome report supporting this interpretation included previous reports of deleterious mutations in PDGFRB affecting the same amino acid, the amino acid location affecting a functional domain, complete conservation of the amino acid on sequence alignment in all available vertebrates, absence of this variant from “healthy cohorts” and databases (see below), and confirmation that the mutation was not present in either parent. The patient’s clinical presentation was consistent enough with previous reports of patients with PDGFRB mutations to suggest that his features were related.
Applying the 2015 American College of Medical Genetics and Genomics scoring criteria,19 the p.N666H variant can be classified as “pathogenic” based on the presence of one strong (PS2: de novo in a patient with the disease and no family history) and three moderate (PM1: located in a mutational hot spot and/or critical and well-established functional domain without benign variation; PM2: absent from controls in the Exome Sequencing Project, 1000 Genomes, or ExAC; and PM5: novel missense change at an amino acid residue where a different missense change determined to be pathogenic has been seen before) criteria. Additionally, in silico predictions for this variant include SIFT (sorting intolerant from tolerant) algorithm prediction of “damaging,” PolyPhen prediction of “probably damaging,” and combined annotation dependent depletion (CADD) Phred-like score of 27.1 (predicted to be among the 1% most deleterious substitutions affecting the human genome), qualifying the variant for PP3 (multiple lines of computational evidence support a deleterious effect on the gene or gene product). Results of in vitro studies on the patient’s cells (see below) supported the damaging effect of p.N666H on the gene product, meaning criteria PS3 is also met. The final combination of criteria for pathogenicity of the p.N666H variant is two strong, three moderate, and one supporting.
In vitro studies described below showed unique sensitivity of the patient’s cells to imatinib. The use of imatinib was extensively discussed with the parents, including all potential side effects. Baseline blood cell counts, blood chemistry, coagulation tests, electrocardiogram, echocardiography, and a repeat MRI were performed before initiation of imatinib. The parents and medical team weighed extensively the risks of imatinib and the fact that there may no benefit to its use at all. They then agreed to the use of this medication.
The drug metabolizing enzyme and transporter (DMET) pharmacogenetic array Affymetrix (Santa Clara, CA, USA) was used for pharmacogenetic evaluation. Imatinib is metabolized in the liver (minimal excretion via kidneys) mainly by the P450 enzyme CYP3A4 (to a lesser extent CYP1A2, CYP2D6, CYP2C9, and CYP2C19 also metabolize the molecule). The main metabolite is bioactive. Half-life is 18 hours for imatinib and 40 hours for the metabolite. Pharmacogenetic testing showed *1/*1 alleles in CYP3A4, consistent with wild type; thus normal metabolizing is expected.
At age 8 years 10 months imatinib was started at a dose of 200 mg daily and after 2 weeks escalated to 400 mg daily (about 340 mg/m2). This imatinib dose is used by us for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia, as well as chronic myeloid leukemia, and is well tolerated in children. The patient was monitored for adverse effects by a pediatric oncologist (Y.H.M.) who has long experience with imatinib with scheduled blood cell counts, blood chemistry, electrocardiogram, echocardiography, and clinical assessments.
There was rapid improvement of the contractures of both hands as well as decrease in the coarse facial features noticeable by his family and medical team. Prior to initiating therapy, midfoot circumference was 9.25 inches bilaterally. After 10 months of treatment, midfoot circumference was 8.75 inches bilaterally. Interestingly, small subcutaneous nodules were first noted on exam after 3 months of imatinib therapy. They remain stable and nonprogressive, thus were never evaluated surgically or pathologically. Transient leukopenia and neutropenia was noted after 3 months of imatinib therapy with no infectious complication and resolved after 9 months of therapy with no dose modification. He also had transient fatigue that resolved. After 1 year of imatinib 400 mg daily (almost 10 years of age) decrease in growth velocity was noted, prompting decrease of imatinib dose to 200 mg daily. He remains on this dose with ongoing clinical improvement. Quality of life remains markedly improved as described by him and his family.
Molecular genetic testing
Exome analysis
This testing was performed at a commercial CLIA/CAP-certified reference laboratory (Ambry Genetics, Aliso Viejo, CA) on genomic DNA samples from the proband and both parents. DNA samples from two unaffected siblings were provided for segregation studies. Short tandem repeat markers were used for sample indexing. Samples were enriched using either SureSelect Target Enrichment System (Agilent Technologies, Santa Clara, CA) or SeqCap EZ VCRome 2.0 kit (Roche NimbleGen, Pleasanton, CA). Standard library prep was performed and final quantified libraries were seeded onto an Illumina (San Diego, CA) flow cell and sequenced using paired-end, 100 cycle chemistry on the Illumina HiSeq 2000 or HiSeq 2500 sequencer. Candidate sequence alterations were confirmed by dideoxy Sanger sequencing.
Pharmacogenetic testing
This testing was performed at a commercial CLIA/CAP-certified reference laboratory (Medical College of Wisconsin Developmental and Neurogenetics Laboratory, Milwaukee, WI). Analysis of purified genomic DNA samples for specific DMET gene variants within the human genome was performed using the Affymetrix (Santa Clara, CA) DMET Plus Assay. Data was analyzed by using DMET Console Software v.1.3.
The assay genotypes 1,931 markers in 233 genes and the copy number state in 5 genes. For these 5 genes the array can distinguish between two copy number states: both gene copies deleted versus one or more copies present.
Antibodies and reagents
Anti-phospho-tyrosine (PY99, sc-7020), anti-PDGFRB (958, sc-432), and anti-STAT5 (sc-835) antibodies were purchased from Santa Cruz Biotechnology (Dallas, Texas). Antiphospho-ERK1/2 (Thr202/Tyr204, #9101), anti-phospho-PLCγ1 (Tyr783, #2821), anti-PLCγ (#2822), anti-phospho-STAT3 (Tyr705, #9131), anti-STAT3 (#9132), anti-phospho-STAT5 (Tyr694, #9351) antibodies, and secondary antibodies conjugated to horseradish peroxidase (#7074, #7076) were purchased from Cell Signaling Technology (Danvers, MA). Anti-ERK2 rabbit polyclonal antibody was produced as described.20
PDGF-BB was purchased from PeproTech (Rocky Hill, NJ). Imatinib was purchased from LC Laboratories (Woburn, MA). Interleukin-3 (IL-3) was produced as described. 21, 22
Cell culture
The murine bone marrow–derived pro-B cell line Ba/F3 was cultured in Dulbecco’s Modified Eagle’s Medium (Gibco, Life Technologies, Grand Island, NY) supplemented with 10% fetal calf serum and 500 U/ml IL-3. Patient’s cells and normal human fibroblasts AG1518 (Coriell Institute for Medical Research, Camden, NJ) were grown in Quantum 333 medium for fibroblasts (A&E Scientific, Enghien, Belgium). HT-1080 cells, which are derived from a human fibrosarcoma and carry an oncogenic N-Ras mutant, are a kind gift from Anabelle Decottignies (de Duve Institute, Brussels, Belgium) and were grown in Iscove’s Modified Dulbecco’s Medium (Gibco) supplemented with 10% fetal calf serum.
Site-directed mutagenesis
The point mutations p.N666H and p.N666K were introduced in PDGFRB cloned in pEF/myc/cyto (Invitrogen, Life Technologies) by site-directed mutagenesis according to manufacturer’s protocol (QuikChange XL-II kit, Stratagene, La Jolla, CA). The constructs were verified by sequencing.
Production of Ba/F3 stable cell lines expressing PDGFRβ
Ba/F3 cells stably expressing the empty vector, wild-type PDGFRβ or the mutated receptors (PDGFRβ p.N666H and p.N666K) were produced as described.23 Ba/F3 cells transfected with the p.N666H and p.N666K mutants were sorted by flow cytometry for homogenous receptor expression and then selected in a medium supplemented with 10% fetal calf serum but lacking IL-3.
Western blot
Ba/F3 cells stably expressing the empty vector or the wild-type and mutated receptors were processed as previously described.23 Patient’s cells were washed twice and starved in Minimum Essential Medium (Gibco, Life Technologies) supplemented with 0.05% bovine serum albumin, 50 U/ml penicillin, 50 μg/ml streptomycin, and 2 mM glutamine (800,000 cells in 10-cm dishes). Twenty hours after starvation, cells were treated or not with 1 μM imatinib for 4 hours. Then, cells were stimulated with PDGF-BB (25 ng/ml) for 15 min or left untreated. Cell lysates and western blots were produced as described.24 Immunoprecipitation experiments were performed as described.25
[3H]-thymidine incorporation assay
Ba/F3 cells stably expressing the wild-type receptor or its mutants were washed twice and seeded in Dulbecco’s Modified Eagle’s Medium supplemented with 10% fetal calf serum without IL-3 (10,000 cells/well in 96-well plates). Then, PDGF-BB (25 ng/ml), imatinib, and/or IL-3 was added. [3H]-thymidine (0.5 μCi, GE Healthcare, Diegem, Belgium) was added 20 hours later for 4 hours and its incorporation was measured using a TopCount instrument (Perkin Elmer, Waltham, MA) as described previously.25
Living cell count
Patient’s cells were seeded at 75,000 cells/well in 6-well plates in Quantum 333 medium in triplicate and were treated or not with 1 μM imatinib. On days 3, 5, 7, and 9, living cells were counted in the presence of Trypan blue with a Cedex XS counter (Roche, Basel, Switzerland) or in a Bürker chamber.
Statistics
Experiments were performed at least three times (unless otherwise stated) and produced similar results. One representative experiment is shown and SD is indicated when it is appropriate. Normal distribution was tested.
Results
The p.N666H substitution constitutively activates PDGFRβ
Exome sequencing revealed a sequence change in the PDGFRB gene, a growth factor receptor (p.N666H, c.1996A>C). This change is considered a missense mutation and is de novo in this child with no mutation detected in his parents.
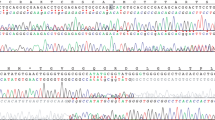
We first assessed if the p.N666H mutation could activate PDGFRβ kinase activity. For this purpose, we expressed this mutant in Ba/F3 cells, an IL-3-dependent cell line that is widely used to test the transforming potential of oncoproteins.26, 27 We compared the effect of the p.N666H substitution to that of p.N666K, a somatic mutation that was identified in infantile myofibromatosis and is known to activate the PDGF β receptor.6, 23 We assessed the phosphorylation of the receptor by western blot after immunoprecipitation and observed that the p.N666H mutant was constitutively phosphorylated on tyrosines, similarly to the p.N666K positive control (Figure 1a). The expression of the mutants was slightly reduced, which may be ascribed to normal degradation of activated receptors.
The PDGFRβ p.N666H mutant is constitutively activated. (a) Ba/F3 cells expressing wild-type (WT) PDGFRβ or the p.N666H and p.N666K mutants were starved for 4 hours. Then, cells were stimulated with PDGF-BB for 15 minutes or left untreated. After cell lysis, PDGF β receptors were immunoprecipitated with an anti-PDGFRβ antibody and the phosphorylation level was assessed by western blot, using an anti-phospho-tyrosine antibody. Finally, the membranes were reprobed with an anti-PDGFRβ antibody. As a negative control, cells expressing the empty vector were used. As previously described,32 two bands were detected for PDGFRβ. The lower band represents the immature form of the receptor located in the endoplasmic reticulum while the upper one corresponds to the mature glycosylated form at the cell surface. (b,c) Ba/F3 cells expressing the WT receptor or the p.N666H and p.N666K mutants were seeded in a medium without interleukin-3 (IL-3) and stimulated or not with PDGF-BB for 24 hours. Cell proliferation was assessed by measuring [3H]-thymidine incorporation. In (c), increasing doses of imatinib were added to the wells. As a control of the specificity of the treatment, cells expressing the empty vector were seeded in a medium with IL-3. (a–c) One representative experiment out of three is shown (with SD in (b) and (c); Student t-test; **P < 0.01; ***P < 0.001).
We then tested the ability of the mutants to stimulate cell proliferation. Untransfected Ba/F3 cells are unable to grow in the absence of IL-3. However, we could select growth factor–independent cells expressing either of the two mutants. We assessed the proliferation level of these cells in absence of IL-3 in a [3H]-thymidine incorporation assay (Figure 1b). Selected cells expressing PDGFRβ p.N666H, as well as selected cells expressing p.N666K, proliferated in absence of PDGF and their proliferation rate was not increased after stimulation. In contrast, cells expressing the wild-type receptor only proliferated when they were stimulated with PDGF. These results are in agreement with the phosphorylation level of the receptors.
Taken together, these observations demonstrate that the p.N666H mutation activates PDGFRβ, leading to cell proliferation. Thus, this mutation could be responsible for the patient’s phenotype.
The p.N666H mutant is sensitive to imatinib
Since p.N666H is an activating mutation, we investigated if a TKI, such as imatinib, could block the activity of the mutated receptors (Figure 1c). The proliferation of Ba/F3 cells expressing the p.N666H mutant was completely abolished after exposure to 1 μM imatinib. Furthermore, this mutated receptor seemed to be slightly more sensitive to the inhibitor than wild-type PDGFRβ and the p.N666K mutant (Figure 1c).
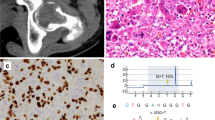
Patient’s cells express constitutively active PDGFRβ that is sensitive to imatinib
A primary cell culture was derived from patient tissue. We confirmed the presence of the p.N666H substitution by Sanger sequencing (data not shown). Next, we analyzed the expression and the phosphorylation of PDGFRβ in these patient cells, as well as downstream signaling molecules.
PDGFRβ was well expressed in patient’s cells (Figure 2a). Regarding PDGFRβ phosphorylation on tyrosines, constitutive phosphorylation was observed in patient’s cells and increased when cells were stimulated with PDGF. When cells were treated with 1 μM imatinib, this constitutive phosphorylation completely disappeared (Figure 2a). The analysis of downstream signaling mediators revealed that, among the different signaling pathways that were constitutively activated (phospholipase C gamma (PLCγ), signal transducer and activator of transcription 3 (STAT3), and mitogen activated protein (MAP) kinase (ERK1/2)), only PLCγ activation was affected by imatinib treatment (Figure 2b). Furthermore, STAT5 was not activated in the patient’s cells in absence of stimulation.
Patient’s cells are sensitive to imatinib. Cells derived from patient’s fibroblasts (patient’s cells) were starved for 20 h and treated or not with 1 μM imatinib for 4 hours. Then, cells were stimulated with PDGF-BB for 15 min or left untreated. (a) PDGFRβ was immunoprecipitated from cell lysates and, to assess its phosphorylation level, western blot experiments were performed with an anti-phospho-tyrosine antibody. Membranes were then reprobed with an anti-PDGFRβ antibody. (b) To assess the phosphorylation level of different signaling proteins, total cell lysates were analyzed by western blot with an antibody recognizing the phosphorylated form of the protein. As a loading control, membranes were reprobed with an antibody targeting the total amount of the corresponding protein. (c) Patient’s cells were seeded at 75,000 cells per well in 6-well plates and treated or not with 1 μM imatinib. Living cells were counted after the indicated period of time. (a–c) One representative experiment is shown (with SD in (c); ANOVA; ***, P < 0.001) (N = 3). (d) Patient’s cells and control cells (AG1518 and HT-1080) were seeded at 75,000 (patient’s cells) or 100,000 (control cells) cells per well in 6-well plates and treated or not with 1 μM imatinib on day 0 (in triplicates for each condition). Living cells were counted on day 9. The histogram represents the percentage of living cells after 9 days of imatinib treatment. For each cell line, the number of living cells with imatinib is normalized with the number of living cells in the untreated control condition. One representative experiment is shown with SD (Student’s t-test; NS, not significant; *P < 0.05; ***P < 0.001; N = 2).
Altogether, these results show that a constitutively activated PDGFRβ is present in patient’s cells and that its activity is inhibited by imatinib.
Imatinib inhibits proliferation of the patient’s cells
We next assessed patient’s cell proliferation in absence and in presence of 1 μM imatinib for 9 days in a living cell count (Figure 2c). The number of living cells was reduced upon imatinib treatment in comparison with untreated cells. The proliferation of normal fibroblasts (AG1518 cell line) was also decreased upon imatinib treatment, but to a lesser extent. This result was expected because fibroblast growth relies on serum growth factors, such as PDGF. In contrast, the number of living fibrosarcoma cells expressing PDGFRs and carrying an activating NRAS mutation (HT-1080) was not affected by imatinib, demonstrating the specificity of this inhibitor towards PDGF receptors (Figure 2d).
These observations demonstrate that imatinib inhibits patient’s cell proliferation, correlating with inhibition of PDGFRβ phosphorylation and PLCγ activation.
Discussion
Here, we describe a novel germ-line PDGFRB mutation in a patient with a complex disorder. We showed that the germ-line p.N666H substitution constitutively activates PDGFRβ, suggesting that the mutated receptor is responsible for the patient’s disease. Additionally, the mutant receptor is sensitive to imatinib. These results, obtained in Ba/F3 cells, are in line with the observations made in the patient’s fibroblasts. Indeed, the patient’s cells express a constitutively active form of PDGFRβ and their proliferation is decreased in response to imatinib. Furthermore, PLCγ phosphorylation was also inhibited by imatinib, in line with other studies demonstrating the importance of PLCγ activity in PDGF-induced cell proliferation.28, 29
A somatic mutation of the same PDGFRβ residue, N666K, had already been described in several patients with myofibromatosis.6 That variant had a stronger oncogenic activity and was also sensitive to imatinib in cultured cells.23 The N666 residue is located in a region that seems to be a “hot spot” for mutations in PDGFRβ. Indeed, the inactivating mutation p.L658P was associated with basal ganglia calcification24, 30 whereas the p.V665A substitution, which activates the receptor, was identified in patients diagnosed with Penttinen syndrome.12 In addition, in PDGFRα, the corresponding residue, N659, was found to be mutated in some cases of gastrointestinal stromal tumors.31 In the absence of crystal structure for the PDGF β receptor kinase domain, the role of this residue can be inferred from the highly homologous KIT receptor. The corresponding KIT residue (N655) participates in hydrogen bonds that stabilize the inactive conformation of the kinase domain.6 Mutation of PDGFRβ asparagine 666 into histidine likely disrupts these interactions and favors the active conformation.
The phenotypic features described in patients with infantile myofibromatosis, Kosaki overgrowth syndrome, and Penttinen premature aging syndrome overlap with the features observed in our patient (Table 1). This overlap suggests that activating germ-line mutations of PDGFRB can cause a spectrum of overlapping phenotypes, which might be grouped as PDGFRB-related syndromes. Infantile myofibromatosis, the first condition associated with mutations in PDGFRB, may also overlap with our patient who has flesh-colored nodules (first noted at 9 years old). However, these nodules have not been further characterized or biopsied. In addition, our patient had one presumptive myofibroma that spontaneously resolved, similar to that seen in infantile myofibromatosis.
Demonstrating the sensitivity of this patient’s mutation to imatinib allowed the clinical team to discuss extensively with the parents the potential use of this medication. Exhaustive baseline evaluation showed no direct contraindications for the use of imatinib. The team reviewed with the parents and the child the side effects known and the possibility that no benefit would be seen. As the parents and the child noted deteriorating use of hands and feet, they and the team believed that trying imatinib under close monitoring by an experienced pediatric oncologist (Y.H.M.) was in the interest of the child. They then proceeded with treatment that has significantly impacted the patient’s quality of life. He is now able to wear standard-sized shoes, and is able to tie shoelaces on his own. He has greater hand mobility, his facial features have softened, and hair growth has improved, lessening the difference between his physical appearance and that of his peers. While these measures are not objective, they were mentioned by the family as significant improvements. Imatinib therapy was associated with mild neutropenia and fatigue that rapidly resolved, but decreased growth velocity required reduction of imatinib from 400 mg daily (340 mg/m2) to 200 mg daily (170 mg/m2). The plan is to continue this therapy indefinitely, but if additional side effects appear to consider another TKI.
The use of imatinib in this case and another report10 of the use of sunitinib demonstrate the successful use of TKIs as a treatment for PDGFRB-related syndromes. This case illustrates the importance of identifying a specific genetic mutation in a rare disorder to carefully determine accurate diagnosis and direct medical treatment in a highly personalized fashion.
Off-label use
This paper discusses off-label use of the approved drug imatinib.
References
Demoulin JB, Essaghir A . PDGF receptor signaling networks in normal and cancer cells. Cytokine Growth Factor Rev 2014;25:273–283.
Soriano P . The PDGF alpha receptor is required for neural crest cell development and for normal patterning of the somites. Development 1997;124:2691–2700.
Soriano P . Abnormal kidney development and hematological disorders in PDGF beta-receptor mutant mice. Genes Dev. 1994;8:1888–1896.
Andrae J, Gallini R, Betsholtz C . Role of platelet-derived growth factors in physiology and medicine. Genes Dev. 2008;22:1276–1312.
Martignetti JA, Tian L, Li D et al. Mutations in PDGFRB cause autosomal-dominant infantile myofibromatosis. Am J Hum Genet 2013;92:1001–1007.
Cheung YH, Gayden T, Campeau PM et al. A recurrent PDGFRB mutation causes familial infantile myofibromatosis. Am J Hum Genet 2013;92:996–1000.
Linhares ND, Freire MCM . Cardenas RG, et al. Modulation of expressivity in PDGFRB-related infantile myofibromatosis: a role of PTPRG? Genet Mol Res. 2014;13:6287–6292.
Bick D, Fraser PC, Gutzeit MF et al. Successful application of whole genome sequencing in a medical genetics clinic. J Pediatr Genet 2017;6:61–76.
Murray N, Hanna B, Graf N et al. The spectrum of infantile myofibromatosis includes both non-penetrance and adult recurrence. Eur J Med Genet 2017;60:353–358.
Mudry P, Slaby O, Neradil J et al. Case report: rapid and durable response to PDGFR targeted therapy in a child with refractory multiple infantile myofibromatosis and a heterozygous germline mutation of the PDGFRB gene. BMC Cancer 2017;17:119–125.
Takenouchi T, Yamaguchi Y, Tanikawa A, Kosaki R, Okano H, Kosaki K . Novel overgrowth syndrome phenotype due to recurrent de novo PDGFRB mutation. J Pediatr 2015;166:483–486.
Johnston JJ, Sanchez-Contreras MY, Keppler-Noreuil KM et al. A point mutation in PDGFRB causes autosomal-dominant Penttinen syndrome. Am J Hum Genet. 2015;97:465–474.
Arts FA, Chand D, Pecquet C et al. PDGFRB mutants found in patients with familial infantile myofibromatosis or overgrowth syndrome are oncogenic and sensitive to imatinib. Oncogene. 2016;35:3239–3248.
Cheah CY, Burbury K, Apperley JF et al. Patients with myeloid malignancies bearing PDGFRB fusion genes achieve durable long-term remissions with imatinib. Blood. 2014;123:3574–3577.
Noujaim J, Thway K, Fisher C, Jones RL . Dermatofibrosarcoma protuberans: from translocation to targeted therapy. Cancer Biol Med 2015;12:375–384.
Roufosse F . Management of hypereosinophilic syndromes. Immunol Allergy Clin North Am 2015;35:561–575.
Tornillo L . Gastrointestinal stromal tumor—an evolving concept. Front Med (Lausanne) 2014;1:43.
Farwell KD, Shahmirzadi L, El-Khechen D et al. Enhanced utility of family-centered diagnostic exome sequencing with inheritance model-based analysis: results from 500 unselected families with undiagnosed genetic conditions. Genet Med 2015;17:578–586.
Richards S, Aziz N, Bale S et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015;17:405–424.
Lennartsson J, Blume-Jensen P, Hermanson M, Ponten E, Carlberg M, Ronnstrand L . Phosphorylation of Shc by Src family kinases is necessary for stem cell factor receptor/c-kit mediated activation of the Ras/MAP kinase pathway and c-fos induction. Oncogene. 1999;18:5546–5553.
Demoulin JB, Louahed J, Dumoutier L, Stevens M, Renauld JC . MAP kinase activation by interleukin-9 in lymphoid and mast cell lines. Oncogene. 2003;22:1763–1770.
Demoulin JB, Uyttenhove C, Lejeune D, Mui A, Groner B, Renauld JC . STAT5 activation is required for interleukin-9-dependent growth and transformation of lymphoid cells. Cancer Res. 2000;60:3971–3977.
Arts FA, Chand D, Pecquet C et al. PDGFRB mutants found in patients with familial infantile myofibromatosis or overgrowth syndrome are oncogenic and sensitive to imatinib. Oncogene 2016;35:3239–3248.
Arts FA, Velghe AI, Stevens M, Renauld JC, Essaghir A, Demoulin JB . Idiopathic basal ganglia calcification-associated PDGFRB mutations impair the receptor signalling. J Cell Mol Med 2015;19:239–248.
Velghe AI, Van Cauwenberghe S, Polyansky AA et al. PDGFRA alterations in cancer: characterization of a gain-of-function V536E transmembrane mutant as well as loss-of-function and passenger mutations. Oncogene. 2014;33:2568–2576.
Schonherr C, Ruuth K, Yamazaki Y et al. Activating ALK mutations found in neuroblastoma are inhibited by crizotinib and NVP-TAE684. Biochem J. 2011;440:405–413.
Nakahara M, Isozaki K, Hirota S et al. A novel gain-of-function mutation of c-kit gene in gastrointestinal stromal tumors. Gastroenterology 1998;115:1090–1095.
Caglayan E, Vantler M, Leppanen O et al. Disruption of platelet-derived growth factor-dependent phosphatidylinositol 3-kinase and phospholipase Cgamma 1 activity abolishes vascular smooth muscle cell proliferation and migration and attenuates neointima formation in vivo. J Am Coll Cardiol. 2011;57:2527–2538.
Roche S, McGlade J, Jones M, Gish GD, Pawson T, Courtneidge SA . Requirement of phospholipase C gamma, the tyrosine phosphatase Syp and the adaptor proteins Shc and Nck for PDGF-induced DNA synthesis: evidence for the existence of Ras-dependent and Ras-independent pathways. EMBO J. 1996;15:4940–4948.
Nicolas G, Pottier C, Maltete D et al. Mutation of the PDGFRB gene as a cause of idiopathic basal ganglia calcification. Neurology. 2013;80:181–187.
Lasota J, Stachura J, Miettinen M . GISTs with PDGFRA exon 14 mutations represent subset of clinically favorable gastric tumors with epithelioid morphology. Lab Invest 2006;86:94–100.
Keating MT, Harryman CC, Williams LT . Platelet-derived growth factor receptor inducibility is acquired immediately after translation and does not require glycosylation. J Biol Chem. 1989;264:9129–9132.
Acknowledgements
The authors are grateful to the patient and the patient’s family for their cooperation in this case study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pond, D., Arts, F., Mendelsohn, N. et al. A patient with germ-line gain-of-function PDGFRB p.N666H mutation and marked clinical response to imatinib. Genet Med 20, 142–150 (2018). https://doi.org/10.1038/gim.2017.104
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.104
Keywords
This article is cited by
-
Giant intracranial infantile myofibromatosis of the skull base: report of two cases
Child's Nervous System (2022)
-
Aggressive infantile myofibromatosis with intestinal involvement
Molecular and Cellular Pediatrics (2021)
-
PDGF receptor mutations in human diseases
Cellular and Molecular Life Sciences (2021)
-
Genetic testing and surveillance in infantile myofibromatosis: a report from the SIOPE Host Genome Working Group
Familial Cancer (2021)
-
The Master of Puppets: Pleiotropy of PDGFRB and its Relationship to Multiple Diseases
Journal of Molecular Neuroscience (2020)