Abstract
Purpose:
We sought to identify characteristics of genetic services that facilitate or hinder adoption.
Methods:
We conducted semi-structured key informant interviews in five clinical specialties (primary care, medical oncology, neurology, cardiology, pathology/laboratory medicine) within 13 Veterans Administration facilities.
Results:
Genetic services (defined as genetic testing and consultation) were not typically characterized by informants (n = 64) as advantageous for their facilities or their patients; compatible with organizational norms of low cost and high clinical impact; or applicable to patient populations or norms of clinical care. Furthermore, genetic services had not been systematically adopted in most facilities because of their complexity: knowledge of and expertise on genetic testing was limited, and organizational barriers to utilization of genetic services were formidable. The few facilities that had some success with implementation of genetic services had knowledgeable clinicians interested in developing services and organizational-level facilitators such as accessible genetic test–ordering processes.
Conclusion:
Adoption and implementation of genetic services will require a multilevel effort that includes education of providers and administrators, opportunities for observing the benefits of genetic medicine, strategies for reducing the complexity of genomic medicine, expanded strategies for accessing genetics expertise and streamlining utilization, and resources dedicated to assessing the value of genetic information for the outcomes that matter to health-care organizations.
Genet Med 2014:16(3):238–245.
Similar content being viewed by others
Introduction
Genomic information can enhance delivery of patient-centered care through individualized diagnosis, prognosis, risk assessment, and selection of treatment. It has been widely recognized, however, that uptake of genetic services is challenging, with a considerable gap between genomic discoveries and translation to genetic services.1,2 Furthermore, even when genomic applications have proven validity and utility, there is low adoption within health-care organizations.3 Barriers to the adoption of genetic services have been identified at multiple levels: health-care systems lack structures and processes to facilitate genetic medicine practice; health professionals are not typically educated in genetics and have little time to incorporate genetic services into their practice; and guidelines for genetic testing, referral, and management are limited.4,5,6,7,8 Addressing barriers to implementation is complex, requiring a multilevel approach that targets patient, provider, organizational, and policy issues.5 To that end, it is critical to improve our understanding of these multilevel barriers so that implementation strategies may be developed and executed to improve the integration of genomic information into routine health-care delivery.
We conducted an exploratory study to identify characteristics of genetic services that may facilitate or hinder their adoption in a health-care organization. We investigated these characteristics across five different specialties in the Veterans Health Administration (VHA), the largest health-care system in the United States, providing care to more than 6 million veterans at 153 health-care facilities and their associated clinics across the country. As it is to many integrated health-care systems in the United States, genetic medicine is relatively new to the VHA. The infrastructure is developing, with the establishment of a national Genomic Medicine Service in 2010 and the recent creation of a few clinical genetics programs based at VHA facilities in Houston, Los Angeles, and Boston. Widespread implementation has not occurred, so we characterize this study as a “pre-implementation” study, i.e., a “developmental evaluation” of existing conditions relevant to adoption and delivery of genetic services, as a precursor to full-fledged implementation efforts.9
Materials and Methods
Theoretical model
Using diffusion of innovation theory, we assessed pre-implementation conditions by investigating how genetic services (the “innovation,” defined at the outset of each interview as “genetic testing and consultation,” consistent with the Institute of Medicine definition)10 have begun to diffuse into the health-care system and the attributes of the innovation that have fostered or hindered uptake.11,12 The theory posits that certain attributes of emergent practices or innovations influence the ease with which they may naturally diffuse into routine use, versus those that require active, targeted implementation strategies. The theory also provides a framework to predict the likelihood of implementation success. It postulates that an innovation, such as genetic services, will be successfully adopted if it is perceived to be advantageous (relative advantage); compatible with organizational and individual values, norms, and needs (compatibility); simple to implement (complexity); usable in preliminary fashion on a small scale (trialability); clearly beneficial (observability); and amenable to adaptation (reinvention). For example, if clinicians observe benefits to patients who receive genetic services, or if they are able to manage the complexity of genetic services utilization, the diffusion of innovation theory would predict that utilization of genetic services would be more likely.12 This article examines these attributes (relative advantage, compatibility, complexity, trialability, observability, and reinvention ( Table 1 ) of genetic services, a complex, multifaceted innovation that is emergent in the US Department of Veterans Affairs (VA) health-care system.
Sample
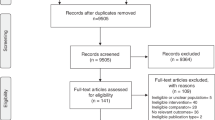
To inform our understanding of multilevel barriers and facilitators to organizational adoption and implementation, we conducted interviews with leaders of five clinical specialties within the VHA: primary care, medical oncology, neurology, cardiology, and pathology and laboratory medicine. These specialties were selected because pilot work and our clinical experience suggested that they span the spectrum of demand for and utilization of genetic services. From pilot work, we expected that thematic saturation in interviews would be achieved with 10–15 “key informants” (i.e., individuals who are uniquely knowledgeable, reliable, and able to generalize about their cultural or organizational settings)13 per specialty. Therefore, we aimed to interview 50–75 key informants (10–15 per clinical specialty) located in 5 facilities within the United States. Using publically available information, we identified the clinical chief from each of the specialties at the five facilities. Service chiefs were invited by e-mail or telephone to participate as key informants in a 30- to 45-min semi-structured telephone interview about the adoption and delivery of genetic services at their facility. Due to low response rate at one original facility, two facilities were added to the initial sample, for a total of six facilities in the initial sampling frame. Subsequently, in a snowball sampling approach, informants in the initial sample were asked to identify additional, potentially knowledgeable interview candidates either within or outside of their facility, resulting in key informants from an additional seven facilities.14 The institutional review board at the VA Greater Los Angeles Healthcare System approved all study procedures.
Data collection
All interviews were conducted by the lead author (A.H.), supported by at least two secondary interviewers (M.S., S.O., and/or C.G.) using a semi-structured interview guide covering six general domains that addressed the following pre-implementation organizational conditions: (i) existing genetic services and arrangements for providing genetic services; (ii) types, training, and roles of professionals who provide services; (iii) procedures for ordering genetic tests; (iv) barriers to adoption and delivery of genetic services; (v) relative priority of genetic services in specialty areas; and (vi) factors necessary for further development of genetic services, including professional development activities. After providing our definition of genetic services (see above), we began by asking our key informants to talk about genetic tests ordered by themselves, colleagues in their specialty, or other providers at their VA, allowing for mention of any test with a genetic basis that could actually be ordered at their site. Later in the interview, we queried about the availability and type of genetic consultative services. Therefore, a wide range of possible tests and consultation arrangements was described and helped to characterize a previously unknown spectrum of genetic services and service arrangements in the VA. Interviewers debriefed after each interview. Interviews were conducted between December 2009 and February 2011. Interviews were digitally recorded and professionally transcribed verbatim.
Data analysis
The interview transcripts were reviewed and edited for accuracy and were then analyzed using ATLAS.ti (ATLAS.ti Scientific Software Development; www.atlasti.com). Each set of interviews was analyzed by specialty, followed by cross-specialty analysis within and across sites. Analysis was led by A.H. and also conducted by S.O. and C.G., with frequent feedback from the broader team. The initial code list was based on the interview guide, using top-level codes to broadly categorize responses to each interview question. After applying these broad codes, the content of each code (i.e., the segments of text to which the code was assigned) was examined for central themes, with additional inductive codes created for themes that were held in common across a substantial proportion (typically 50%) of informants. As transcripts became available from each specialty, codes and subcodes were revisited and refined, if needed. For example, the original “barriers to adoption” code became too voluminous and multidimensional, so it was replaced by codes for each type of barrier that was frequently described (e.g., “barrier—cost of genetic tests”). A subset (at least 20%) of each specialty-specific cluster was independently coded by A.H. and either S.O. or C.G. after code definitions were developed by the team. Intercoder reliability in the application of codes was established over time by comparing independent coding, identifying discrepancies, and discussing and resolving discrepancies with a team consensus process. Characteristics of the innovation were identified by clustering interviews (i.e., making document “families”) with similar characteristics (e.g., oncology, cardiology) and comparing code content within each cluster of interviews (e.g., benefits/advantages of genetic tests for oncology). In addition, A.H., S.O., and C.G. independently extracted quotations that illustrated each of the innovation attributes; they compared their findings, collaboratively selected illustrative quotations, and reviewed with the broader team to achieve consensus.
Results
Key informant characteristics
Sixty-four key informants completed the interview: 16 in primary care; 13 cardiology; 10 oncology; 12 neurology; and 13 pathology ( Table 2 ). Most of these key informants (70%) were from the initial sampling frame (six facilities).
Characteristics of genetic services: a complex organizational innovation
Genetic services were consistently referred to by informants as a “new technology” or an “innovation,” consistent with our a priori characterization of these services as relatively new to the VHA overall. Although some informants described “hot spots” of activity related to genetic services, most were not aware of genetic services at their respective facilities, or they were aware of limited services (e.g., ability to order some genetic tests in the laboratory menu in the electronic health record) that were not being routinely utilized. Themes identified as relevant to genetic service attributes that may foster or hinder adoption are summarized in Table 3 , with accompanying illustrative quotations, and described below.
Relative advantage
Mention of clearly advantageous genetic tests or consultation services tended to be specialty specific, with primary-care and cardiology informants citing very few advantages, and oncology, neurology, and pathology informants sometimes referencing specific tests and genetic services compatible with those specialties (see the section on “Compatibility” below). Many of the informants had difficulty even assessing advantage, citing limited access to information on available genetic tests, the utility of genetic tests, and the appropriate use of genetic consultative services. Many discussed advantages or disadvantages of some generally well-known tests (e.g., BRCA1/2 for hereditary breast–ovarian cancer syndrome), although they themselves may not have ordered them. Pathologists frequently questioned the cost-effectiveness of genetic tests, citing limited clinical utility in the face of high cost.
In general, informants from all specialties described ambiguous added value of genetic testing for predicting disease or treatment outcomes as compared with existing practice, particularly for common diseases. Some pointed out that advantage could be lessened to the point of disadvantage, and even danger, when providers misunderstand test results. With respect to whole-genome/whole-exome testing, informants indicated that although there is future promise, current applicability to clinical care is unclear. Furthermore, while some informants emphasized the importance of having a knowledgeable professional to interpret test results, perceived low volumes of applicable cases contributed to a general sense that hiring such professionals would not be cost-effective.
Compatibility
The organizational value consistently raised across specialties was clinical utility, with many describing the VHA as “a utilitarian system.” Genetic tests that would most directly inform clinical decision making, diagnosis, and prognosis tended to be seen as most compatible with overall organizational standards, or with specialty-specific norms. For example, in neurology, value was associated with genetic tests that could provide diagnostic certainty and prognostic clarity, particularly for rare, potentially devastating diseases, even if clinical management would not change. Contributions of test results to quality of life and counseling for lifestyle decision making and family-risk considerations were mentioned as valuable in neurology.
Testing that could provide specific guidance for chemotherapeutic choices and counseling for difficult decisions around personal cancer risk, as well as cancer risk for family members, was described as valuable in oncology. Applicability of genetic testing to cardiology practice was uniformly described as low, and there was no use of consultative services reported. In primary care, where the occasional rare genetic disease would be difficult to recognize, and the added value of genetic testing was ambiguous (see above), the “fit” with professional norms was not portrayed as compatible, except for the occasional usefulness of factor V Leiden testing and testing for hemochromatosis.
Access to a VA-based geneticist was reported at only 1 of the 13 sites and was described as compatible with “ways of working” when deciding whether to order genetic tests and what to do with the results. None of the informants reported having genetic counselors on site. However, many described access to genetic consultative services through arrangements with non-VA organizations, particularly academic medical centers.
Complexity
Informants described nearly every aspect of using genetic services as fraught with complexity for their specialties and their facilities. The knowledge base required for identifying patients with indications for genetic tests, meaningfully collecting and applying family history information, and selecting appropriate tests for a given case was described as vast. Interpretation of genetic test results was also viewed as having complex dimensions with implications for family members that many clinicians were not trained to consider. Complex logistic “hoop jumping” in genetic test ordering and approval processes were frequently described as frustrating barriers to testing. Navigating the leadership hierarchy to adopt even approved pathology laboratory practices was also described as a complicated process.
Trialability
Due to the limited access to clinical genetic consultative services and the limited ability to order genetic tests using the electronic health record, most informants had no first-hand experiences with genetic services. Experimentation with tests and off-site consultation was largely self-motivated and limited by the complexities outlined above; however, at the site that had recently implemented on-site genetic consultative services, an oncology informant reported using the service and appreciating improvements in ease of test ordering (through the geneticist), as well as the welcome solution to the problem of counseling patients about results with complex issues relating to disease risk and options for management.
Observability
Overall, observability of the benefits of genetic services was seldom reported, again likely due to limited access and utilization. A small number of informants described learning of benefits through observation of use by a colleague in another specialty, or by experiences that arose in their work at other organizations, such as university clinics. Pathologists occasionally described difficulty implementing genetic testing in the laboratory until administrative leaders observed cost savings related to the use of such testing in the population served.
Reinvention
Informants did not report opportunities to make their own modifications to test ordering or consult request processes to suit their specialty-specific needs. When asked what modifications might prove helpful, informants suggested possible adaptations to the electronic health record, such as genetic test menus; checklists with criteria for ordering tests; embedded links to relevant guidelines; and automated support for collecting family histories. At one facility, local adopters had successfully created a neurogenetics clinic, but such sophisticated adaptations to local environments were rare.
Discussion
We found that the characteristics of genetic services as an “innovation” are not compatible with uptake into the health-care organization by simple diffusion; instead, adoption of clinical genetic services will require development of targeted organizational supports to strengthen the likelihood of adoption and implementation. Informant characterizations supported our a priori assumption that the VHA is, at best, in the early stages of adoption of genetic services. Informants reported a general lack of familiarity with and activity around genetic services in their facilities, with only a few facilities where knowledgeable clinicians had taken a particular interest in developing these services. For the most part, adoption of genetic services was in the “let it happen” mode, meaning that incorporation of these services into organizational practice was typically unpredictable, uncertain, emergent, adaptive, and self-organizing, occurring via mechanisms that were rarely facilitated, i.e., the services occurred by “osmosis,” as one informant stated.12
Informants’ perspectives on clinical genetic services suggest that considerable work is needed to improve knowledge and provide opportunities for organizations to experience the benefits of this innovation. Overall, relative advantage of genetic services was not compelling, with many informants indicating that evidence of clinical utility and guidelines for genetic tests were lacking, leading to obstacles in their use. This issue of evidence has been highlighted in recent commentaries. For example, Evans and Khoury15 suggest that accrual of evidence is critical to implementation and that “premature implementation,” i.e., implementation without sufficient evidence of superior outcomes, can “carry a high price tag in terms of patient suffering and cost.”
Informants indicated that benefits did not outweigh the costs of genetic services. Organizational values, in particular, were described as incompatible with the notion of using expensive tests for little clinical gain, and there was infrequent consideration of gains beyond clinical management of patients (e.g., gains in quality of life or related to reproductive decision making). Further compounding the challenging context for adoption was the commonly shared viewpoint that genetics as a field is highly complex and that the expertise needed to appropriately use genetic information is not typically available. Clearly, efforts to simplify the implementation of genetic services are needed to mitigate their complexity and clarify the applicability of specific tests and consultation practices to specific clinical contexts. Finally, because few informants’ facilities had actually developed genetic services through a multilevel approach that, for example, limited the “hoop jumping” for ordering tests, the trials (trialability), observations (observability), and reinventions that might have contributed to knowledge and experience of previously unappreciated advantages and clinical compatibility were limited; only the few who had successfully used genetic services could speak to these characteristics.
Our findings support the need for structured and targeted implementation strategies for genetic services, rather than passive diffusion. The VHA is well positioned to achieve successful implementation of genetic services given the investment in the Million Veterans Program (a medical database designed to study how genes affect health; http://www.research.va.gov/mvp/) and the recent creation of the national Genomic Medicine Service, which is developing organizational structures and processes to improve delivery and outcomes relating to genetic services. Informed by the seven steps (noted in italics) for successful diffusion of innovations, we propose the following implementation strategies for the VHA’s national Genomic Medicine Service: support technology assessment to inform evidence-based guidance and policy for genomic applications (find sound solutions); act as the hub to support and unify the clinical genetic programs that exist throughout the system (find and support innovators, invest in early adopters), and provide genetic counseling services via telehealth where such expertise is lacking (lead by example); convene meetings, perhaps virtually, of the genetic service providers in the VHA and highlight accomplishments to clinical and administrative leadership (make early adopter activity visible); and foster development of educational materials and clinical tools in the electronic health record systems at each VHA facility, creating opportunities for genetic service utilization (create slack for change) with the ability for local adaptation (trust and enable reinvention).16 In a recent review paper, Manolio et al.3 provide many specific suggestions for solutions to implementation challenges that are compatible with those suggested here.
Our study has a number of strengths and limitations that deserve mention. First, our findings are exploratory and not generalizable to the VHA or to other health-care organizations. Second, we designed our investigation to view implementation through the lens of five specialties with varying genetic services needs, which gave us a breadth of perceptions. However, we did not include administrators or others in the organizational hierarchy, nor did we include the patients themselves. It is likely that information drawn from nonclinicians and patients would provide different perspectives on the implementation and utility of genetic services. Finally, our qualitative approach allowed us to delve into key informants’ perceptions and concerns. However, we cannot use these data to quantify the extent of our findings; instead, we have used these findings to inform the development of a Web-based, structured survey for administration to clinical chiefs at every VHA facility.
This study represents one of the first efforts to identify the characteristics of genetic services that hinder or facilitate their organizational adoption and implementation. However, other studies of innovation adoption have reported similar conclusions to ours, e.g., that the need for and potential compatibility of the innovation should be assessed in implementation planning14 and that evidence of effectiveness (in this case, evidence of clinical utility and cost-effectiveness) is a prerequisite for the initiation of innovation.17,18 Diffusion of innovation theory facilitated the interpretation of our findings and generated essential lessons that demonstrate gaps and inform strategies for improving adoption and implementation of genetic services. Understanding the attributes of genetic services—and how these attributes interrelate—can guide design of active, planned, multilevel implementation efforts5 with tailored application supports for health-care organizations seeking to adopt these services.
Disclosure
The authors declare no conflict of interest.
References
Khoury MJ, Berg A, Coates R, Evans J, Teutsch SM, Bradley LA . The evidence dilemma in genomic medicine. Health Aff (Millwood) 2008;27:1600–1611.
Rogowski WH, Grosse SD, Khoury MJ . Challenges of translating genetic tests into clinical and public health practice. Nat Rev Genet 2009;10:489–495.
Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med 2013;15(4):258–267.
Hedgecoe A . From resistance to usefulness: sociology and the clinical use of genetic tests. BioSocieties 2008;3:183–194.
Khoury MJ, Coates RJ, Fennell ML, et al. Multilevel research and the challenges of implementing genomic medicine. J Natl Cancer Inst Monographs 2012;2012:112–120.
Scheuner MT, Sieverding P, Shekelle PG . Delivery of genomic medicine for common chronic adult diseases: a systematic review. JAMA 2008;299:1320–1334.
Suther S, Goodson P . Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genet Med 2003;5:70–76.
Taylor MR, Edwards JG, Ku L . Lost in transition: challenges in the expanding field of adult genetics. Am J Med Genet C Semin Med Genet 2006;142C:294–303.
Stetler CB, Legro MW, Wallace CM, et al. The role of formative evaluation in implementation research and the QUERI experience. J Gen Intern Med 2006;21(suppl 2):S1–S8.
Institute of Medicine (US) Roundtable on Translating Genomic-Based Research for Health. Innovations in Service Delivery in the Age of Genomics: Workshop Summary. Genetic Service Delivery: The Current System and Its Strengths and Challenges. National Academies Press: Washington, D.C., 2009.
Rogers EM . Diffusion of Innovations, 5th edn. Free Press: New York, 2003.
Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O . Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581–629.
Kumar N, Stern LW, Anderson JC . Conducting interorganizational research using key informants. Acad Manage J 1993;36:1633–1651.
Patton MQ . Qualitative Research & Evaluation Methods, 3rd edn. Sage: Thousand Oaks, 2001.
Evans JP, Khoury MJ . The arrival of genomic medicine to the clinic is only the beginning of the journey. Genet Med 2013;15(4):268–269.
Berwick DM . Disseminating innovations in health care. JAMA 2003;289:1969–1975.
Carlfjord S, Lindberg M, Bendtsen P, Nilsen P, Andersson A . Key factors influencing adoption of an innovation in primary health care: a qualitative study based on implementation theory. BMC Fam Pract 2010;11:60.
Barnett J, Vasileiou K, Djemil F, Brooks L, Young T . Understanding innovators’ experiences of barriers and facilitators in implementation and diffusion of healthcare service innovations: a qualitative study. BMC Health Serv Res 2011;11:342.
Acknowledgements
This study was funded by the VA Health Services Research & Development (HSR&D) Service (IBD 09-101); pilot work conducted through the HSR&D-funded Health Services Genomics Pilot Program (DNA 08-128) also informed this paper. At the time of the study, A.B.H. was an investigator with the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University, St. Louis; supported through an award from the National Institute of Mental Health (R25 MH080916-01A2) and VA HSR&D QUERI. E.M.Y.’s effort was supported by a VA HSR&D Senior Research Career Scientist Award (RCS 05-195). This work was further supported by the VA Greater Los Angeles HSR&D Center of Excellence (HFP 94-028). A.B.H. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors are employed by the Department of Veterans Affairs. A.B.H., E.M.Y., and M.T.S. receive research funding from the VA HSR&D Service.
The views expressed within are solely those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government. Portions of this paper were presented in poster form at the VA HSR&D/QUERI National Conference, National Harbor, MD, July 2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamilton, A., Oishi, S., Yano, E. et al. Factors influencing organizational adoption and implementation of clinical genetic services. Genet Med 16, 238–245 (2014). https://doi.org/10.1038/gim.2013.101
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2013.101
Keywords
This article is cited by
-
Uptake of funded genomic testing for syndromic and non-syndromic intellectual disability in Australia
European Journal of Human Genetics (2023)
-
Whole genome sequencing in oncology: using scenario drafting to explore future developments
BMC Cancer (2021)
-
Evaluation and comparison of hereditary Cancer guidelines in the population
Hereditary Cancer in Clinical Practice (2021)
-
Anticipating the primary care role in genomic medicine: expectations of genetics health professionals
Journal of Community Genetics (2021)
-
Underutilization of Lynch Syndrome Screening at Two Large Veterans Affairs Medical Centers
Digestive Diseases and Sciences (2020)