Abstract
Purpose:
The initial breast cancer genetic counseling visit is mainly educational, with large amounts of relatively standard information and little counselee participation. Counselors might provide more counselee-specific information if counselees would participate more. A pre-visit website providing computer-tailored information and a question prompt sheet (QPS) might help counselees to pursue a more active role.
Methods:
Counselees were randomized to receive usual care (UC) or UC plus the pre-visit website. The QPS questions were sent to the counselor before the visit. All counselees completed a baseline questionnaire, and visits were videotaped.
Results:
Intervention-group counselees (n = 102) did not ask more questions than UC-group counselees (n = 90). However, counselees in the intervention group more often shared their agenda (B = 10.37; confidence interval (CI) 2.68–18.06; P = 0.01), directed the communication (B = 0.41; CI 0.28–0.53; P = 0.01), and paraphrased the counselors’ words (B = 5.18; CI 0.43–9.92; P = 0.03). Counselors introduced and answered the QPS questions. As a result, they provided more information about the topics of these questions, and the information provided was more specific to whether there was an indication for DNA testing.
Conclusion:
A pre-visit website with QPS helped counselees to communicate more assertively. As a result, the information provided was more counselee specific, without affecting the visit duration.
Genet Med 2012:14(5):535–542
Similar content being viewed by others
Introduction
Breast cancer genetic counseling primarily aims to increase realistic risk perception and adherence to surveillance recommendations.1 Crucial in the process of counseling is the counselee’s ability to make well-informed decisions with regard to DNA testing and the adoption of preventive options, i.e., surveillance or risk-reducing surgery.2 In a process of informed decision making, the counselee’s pros and cons regarding testing and preventive options should be discussed.3
However, previous studies have described the initial cancer genetic counseling visit as predominantly educational, with large amounts of standard information and little counselee participation.4,5,6,7 Because lay understanding of Mendelian genetics is poor,8,9,10,11,12 a large part of the counselor communication is education about hereditary breast cancer, inheritance, and DNA testing.13 Moreover, counselors direct the communication, initiate the discussion of most topics,14 and seldom build on the counselee’s perspective, i.e., her needs, knowledge, and risk perception.15,16 By providing pre-visit education, more consultation time might be left to discuss the counselee’s decision and counselees can be helped to request information.14
Studies of computer-based pre-visit information for breast cancer genetic counselees indeed indicate that the focus within the consultation shifted away from basic education toward more counselee-specific information about risk, decision making, and preventive options.17 Also, the use of the program shortened the first visit.17,18 However, these studies are based on a counselor survey and lacked observations of the visits. Observations are known to give the best indication of interaction in a consultation and might contradict physicians’ reports and patients’ self-reports.19
Interventions to enhance counselee question asking have not yet been applied in genetic counseling. A question prompt sheet (QPS), which prompts patients to articulate their questions before their consultation, has been shown effective in other settings.20 Observation studies in oncology consultations have shown that QPS use increased patient question asking,19,21,22 especially when the QPS was actively endorsed by the physician.19 Additionally, patients were empowered to raise topics.22
A randomized, controlled trial investigated whether a counselee activating intervention23 could facilitate more tailored communication in the first visit for breast cancer genetic counseling. For this purpose, a pre-visit website providing computer-tailored information including a QPS, named E-info geneca, was developed.24 The information on the website was computer tailored to counselees’ individual situation: age, personal and family cancer history, and the topics of the counseling procedure, preventive options, the meaning of being a carrier of a BRCA1/2 gene mutation, emotional consequences, and hereditary breast cancer. Additionally, communication advice was provided to stimulate question asking and other assertive communication. Finally, the website provided a blank QPS to encourage counselees to formulate their questions that remained after having read the website or that were prompted by the information on the website. These questions were sent to the counselor. Previous articles showed that the website was used by all intervention-group counselees and that almost half of them wrote questions on the QPS.25 This website use resulted in more realistic expectations and higher pre-visit levels of knowledge.26 Counselees were thus better prepared for their first breast cancer genetic counseling visit, and this might result in more tailored communication. Hypothesized effects of E-info geneca in the consultation were increased counselee question asking, assertive communication,23 and increased interactivity between counselor and counselee.27 Moreover, we expected that the provided information was counselee specific instead of generic. This might reduce the amount of information given to the counselee during the consultation and result in shorter consultations.
Materials and Methods
This study was conducted at the Department of Medical Genetics of the University Medical Center Utrecht. This department offers breast cancer genetic counseling according to the Dutch guidelines.28 The study was approved by the medical ethical committee of the hospital and was registered in the Dutch Trial Register (ISRCTN82643064).
Study design
A sample of 200 counselees was intended. With 100 counselees in each group, there was an 80% power to detect effect sizes of d = 0.40 or higher. We succeeded in including 197 counselees. Consecutive new counselees were included from February 2008 to April 2010 (see Supplementary Figure S1 online). Counselees who were female, aged ≥18 years, and who were the first of their first-degree family to seek breast cancer genetic counseling were sent information about the study and an opt-out form. The opt-out form included a question about reasons for withdrawal. Counselees were ineligible if they lacked Internet or e-mail access or when they requested presymptomatic DNA testing because of an identified BRCA1/2 gene mutation in a relative. All counselees who did not return the opt-out form were randomly assigned 1:1 to the usual-care (UC) group or the intervention group (UC + website E-info geneca) by a secretary unaware of respondent characteristics using sequentially numbered, sealed, opaque envelopes. UC comprised a brief standard pre-visit leaflet with information about the counseling procedure. Counselees received a login to access the Web-based baseline questionnaire. After completion of this questionnaire, the intervention-group respondents received a link to access the website E-info geneca. At the start of the consultation, the counselor collected the informed consent form. Consultations were recorded on videotape and showed only the counselor’s face. All 14 breast cancer genetic counselors of the department participated and recorded 4–29 consultations each. Three were clinical geneticists, and five were clinical geneticists in training (all but two were female). Six were genetic counselors (all female; three in training). Counselors were instructed to endorse the QPS because previous studies showed that counselors should help counselees feel comfortable asking questions.19,22 The instructions scripted them to refer to the QPS at the start of each intervention-group visit, to introduce the questions posed on the QPS if any, to welcome any other questions, and to add that counselees were welcome to interrupt them and that asking questions is important to fulfilling their needs. Counselors were reminded of the QPS by a printout of this question sheet, which was put in front of the medical file by a secretary.
Counselee characteristics
Age, referral, whether counselees had children, personal and family cancer history, and educational attainments were collected in the baseline counselee questionnaire. All but the latter were derived from the medical file if the baseline questionnaire was not completed. Additionally, whether or not there was an indication for DNA testing for the counselee or an affected family member was determined from the medical files.
Coding of videotapes
Communication was coded directly from the videotapes, using Observer XT7 software (Noldus, Wageningen, The Netherlands), which allowed analysis of the number, time, and sequence of utterances in the dialogue.29 Verbal communication was analyzed with RIASgene, an adaptation for the genetic counseling setting of Roter’s Interaction Analysis System (RIAS).14 In RIAS, all verbal dialogue is coded.30 RIASgene has inserted categories for the counselee’s agenda.14 Additionally, the content of questions and information was coded based on the QUOTE-geneca questionnaire of counselees’ needs31 (see Table 3). Interactivity was calculated from the RIAS codes as the average number of turns per minute.27
Additionally, the QPS endorsement by the counselor was coded as absent, basic (counselor refers to QPS and introduces questions on QPS), or extended (counselor invites counselee to interrupt and ask any other questions, reviews questions, explains importance of asking questions), as was performed previously by Clayton et al.32 Coders rated whether the counselor introduced and answered the questions written on the QPS and invited further questions, and whether the QPS questions were reviewed at the end of the consultation. Coding was conducted by three trained coders. Interrater reliability was calculated on a random 10% of the consultations observed by the main coder (n = 75) for categories with mean occurrence >2%.33 Intercoder reliability coefficients (intraclass correlation coefficient) for counselee categories averaged 0.92 (range 0.85–0.99) and for counselor categories 0.93 (range 0.87–0.98). Intracoder reliability was calculated on a random 10% of the main coder’s recoding of her consultations. Intracoder reliability coefficients (intraclass correlation coefficient) averaged 0.86 (range 0.62–0.99) for counselee categories and 0.87 (range 0.58–0.99) for counselor categories. Average intercoder reliability of the topics (intraclass correlation coefficient) was 0.91 (range 0.74–0.99), and intracoder reliability was 0.88 (range 0.70–0.95).
Analysis
Applying an intention-to-treat analysis in accordance with the Cochrane criteria,34 we analyzed respondents in the groups to which they were randomized regardless of whether they actually read E-info geneca. Seven missing values on education were imputed with the median. If two counselors were present, their utterances were added. If a spouse or relative was present, these utterances were added to those of the counselee. We applied random-effects multilevel regression analyses35 to account for the fact that consultations (level 1) were nested within counselors (level 2) (i.e., each counselor performed several consultations). The amount of variance explained at the counselor level varied from 6% for counselees’ orienting statements to 24% for counselors’ paraphrases. Linear analyses were used for the frequent utterances and logistic analyses for infrequent utterances (transformed in no/yes) and for counselor endorsement. Analyses were controlled for counselees’ disease status (breast cancer), age, having children, education, receiving an indication for DNA testing, the presence of a companion or a second counselor, whether the counselor was a clinical geneticist or a genetic counselor, and whether the counselor was still in training. Analyses were conducted using Stata 10 (StataCorp, College Station, TX) with two-sided significance testing at P < 0.05.
Results
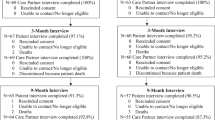
Twenty-four counselees (6.5%) were ineligible because of lack of Internet or e-mail access. During 27 months, 336 eligible counselees received information about the study, and 197 were willing to participate. The response was 58.6%. There were no significant differences between participants and decliners in age (t = 1.62; P = 0.11), disease status (χ2 = 0.05; P = 0.81), family history of cancer (χ2 = 0.06; P = 0.82), and referral pathway (χ2 = 87; P = 0.35). Half of the decliners (n = 70; 50.4%) indicated a reason; most did not want to participate because the consultation was being videotaped (n = 46). Five consultations were not videotaped because of technical or logistic failure, resulting in 192 videotaped consultations. Supplementary Figure S1 online shows a flowchart of the study procedure.
Counselees
As shown in Table 1 , the UC- and intervention-group respondents were similar with regard to age, having children, educational attainment, referral pattern, and indication for BRCA1/2 testing. One counselee was affected with ovarian cancer. There was a trend toward counselees in the intervention group being more often affected with breast or ovarian cancer (χ2 = 3.84; P = 0.053). Most intervention- and UC-group counselees were accompanied by a spouse or relative (67% vs. 58%; χ2 = 1.70; d.f. = 1; P = 0.19). In 112 (58%) consultations, one companion was present, and 13 (7%) consultations were attended by two or more companions.
Counselors’ endorsement of the QPS
The counselees’ questions as filled in on the QPS were almost always introduced by the counselor at the start of the consultation (34 of 41; 83%). In 58% of the consultations in the intervention group versus 12% in the UC group, the counselor explicitly welcomed any other questions (odds ratio = 14.56; P = 0.000). In 29% of the consultations in the intervention group versus 7% in the UC group, the counselor added that counselees should not hesitate to interrupt him/her (odds ratio = 12.58; P = 0.000). The counselor reviewed the counselee’s questions at the end of the consultation, to make sure that the counselee had understood the answers, in 37% of the intervention-group consultations versus 3% of the UC-group consultations (odds ratio = 24.10; P = 0.000). Although included in the script, counselors did not say that it is important for counselees to ask questions in any of the consultations, either in the intervention or control group. Additionally, we checked for changes in counselors’ communication between the intervention and UC groups ( Table 2 ). In intervention-group consultations, counselors paraphrased the counselee’s words more in order to check their understanding of what the counselee was saying (B = 7.79; confidence interval (CI) 0.69–14.90; P = 0.03).
Counselee participation
All intervention-group counselees had accessed E-info geneca, and they spent on average 21 min (SD = 20) reading a mean of 11 Web pages (SD = 8). A majority (81%; n = 83) had read the Web page providing communication advice. Of the intervention-group counselees, 42% (n = 42) had written questions on the QPS (mean 3.1 questions, SD = 1.1). The number of counselee questions in the consultation did not significantly differ between the intervention and UC groups ( Table 2 ). When the questions on the QPS were added to the questions posed during the visit, QPS users posed 18.9 questions (SD = 13.0), compared with 15.6 (SD=12.7) in the UC group. Due to the large standard deviations, this difference was not significant (P = 0.13; Table 3 ). There were no significant differences between intervention-group counselees who did and those who did not use the QPS, 16.6 (SD = 13.8; P = 0.48).
However, counselees who used the QPS posed significantly more questions about their own and their family members’ risk of breast cancer ( Table 3 ). QPS questions focused mostly on preventive options (n = 20), risk for counselee (n = 18) and relatives (n = 16), DNA testing (n = 14), prevalence of breast cancer (n = 14), and inheritance (n = 7). A little more than one-third of all utterances in the consultation were from the counselee, and this did not differ between the intervention and UC groups ( Table 2 ). Neither did the interactivity, i.e., mean number of turns per minute, differ between the groups.
In contrast to the counselee questions, the other assertive communication behaviors did increase. Counselees in the intervention group shared their agenda more than counselees in the UC group did (B = 10.37; CI 2.68–18.06; P = 0.01; Table 2 ), by talking about their reasons for concern, their knowledge of hereditary breast cancer, and their risk perception. Also, counselees in the intervention group directed the communication more by giving orienting statements (B = 0.41; CI 0.28–0.53; P = 0.01). For example, they would interrupt the counselor by saying that they would like to check their understanding or go back to a previous topic, e.g., “another thing…”, “excuse me…”, “if I can repeat what you’re saying…” Additionally, counselees paraphrased the counselor’s words more by summarizing and checking information from the counselor (B = 5.18; CI 0.43–9.92; P = 0.03). Overall, there were more task-oriented utterances of counselees in the intervention group (B = 7.47; CI 1.52–13.41; P = 0.01). Counselees who did not receive an indication for DNA testing uttered significantly less often more than two disagreements in the intervention compared with the UC group (B = −2.58; CI −4.82 to −0.33; P = 0.02).
Discussion of topics during the visit
If counselees had written questions on the QPS about preventive options (B = 17.17; P = 0.01), the breast cancer risk for themselves (B = 2.20; P = 0.04) or family members (B = 2.70; P = 0.001), DNA testing (B = 17.12; P = 0.03), or inheritance of hereditary breast cancer (B = 2.45; P = 0.03), counselors provided significantly more information about these topics as compared with the UC consultations (see Table 4 ). This was especially important concerning the risk for family members because this topic was not discussed in most (68%) of the consultations.
Provision of counselee-specific information
There were some changes in the provision of counselee-specific information, i.e., information adjusted to whether the counselee received an indication for DNA testing ( Table 5 ). Counselees who did not receive an indication received less information about DNA testing in the intervention group (B = −13.41; P = 0.04). Counselees who did receive an indication were provided with more information about preventive options in the intervention group (B = 7.54; P = 0.04).
Visit duration
Consultations in the intervention group lasted on average 46.7 min (SD = 17.0), compared with 44.9 min (SD = 15.1) in the UC group (B = 2.19; P = 0.31).
Discussion
This is the first study that presents observational data of the communication in the first visit for breast cancer genetic counseling after counselee use of a pre-visit educational website with QPS. Results showed that intervention-group counselees did not ask more questions than UC-group counselees. However, intervention-group counselees did communicate more assertively by sharing their agenda, directing the communication, and paraphrasing the counselor’s words. The QPS enhances tailoring of information to the individual counselee; counselees who had used the QPS received more information than others about the topics of these questions. Also, information received by the intervention-group counselees was slightly more specific to whether they received an indication for DNA testing than information for UC-group counselees.
When counselees had sent questions ahead (QPS), the counselor conscientiously introduced and answered these. Questions posed on the QPS were predominantly about the risk of breast cancer and preventive options for both the counselee and her relatives. As a result of these QPS questions, these topics were significantly more discussed. Because counselees’ risk perception accuracy has been found to be only scarcely improved by genetic counseling,36 more questions and information about the risks for the counselee and relatives seem to be a turn in the right direction, even more so because the topic of risk for relatives mostly remained untouched in the UC-group consultations. This is consistent with the results of QPS use for oncology visits, in which a QPS also shifted the focus of the consultation.22 The unexpected finding that counselees in the intervention group did not ask more questions might be due to the omission of example questions. A blank QPS was chosen to enable counselees to put forward their own agendas. However, counselees might find it hard to articulate their questions.25 Studies reviewing effects of a QPS evaluated those with example questions.20 Provision of example questions next to space for own questions might increase counselee use of the QPS and is advised for future studies.
Although the intervention was primarily aimed at counselees’ communication behavior, it also showed an effect on counselors’ communication due to the instruction to endorse the QPS. In the intervention-group consultations, counselors invited further questions and reviewed questions significantly more often as compared with the UC group. Also, the counselors tended to paraphrase the counselee’s words more, which indicates increased rapport building and might facilitate mutual understanding. The instruction together with the QPS questions thus resulted in more counselee-centered communication. In the intervention-group visits, information was better adapted to whether the counselee received an indication for DNA testing, but counselors did not reduce the amount of information. As a result, the counselor’s verbal dominance was unchanged. Studies have consistently found verbal dominance by counselors in the first visits for breast cancer genetic counseling,7 and previous attempts to reverse this were unsuccessful.37 Instead of the percentage of counselee talk, the recently developed measure of interactivity based on RIAS might give enhanced insight to the reciprocity of the communication.38,39 In this study, the manner of presentation of genetics education did not appear more interactive. Future studies should untangle how to increase interactivity.
Finally, contrary to our expectations the visit duration was not affected. Previous studies of pre-visit counselee information showed a significant decrease in consultation length of 8 min.17,18 However, these studies were from the United States, where first consultations in genetics centers lasted on average almost 90 min.40 By contrast, the consultations in this study averaged 45 min, which is similar to the average visit duration in other Dutch genetic centers.14
Limitations
This study has some limitations. First, some counselees (6.5%) were excluded from the study because they lacked Internet or e-mail access. However, computer ability did not seem to be a barrier. Because the website did not require advanced computer skills, counselees navigated the website well.25 Second, although appropriate randomization methods were used,34 more counselees who were affected with breast cancer were allocated to the intervention group than to the control group. Randomization does not guarantee that characteristics are evenly distributed over study groups as, although unlikely, based on coincidence uneven distributions can happen. All analyses were corrected for disease status. Third, due to the need for the counselor to endorse the QPS, counselors could not be blinded to group allocation. Coders were not blinded either, because the counselor’s endorsement of the QPS often gave away the intervention condition. Fourth, because randomization was conducted on the counselee level instead of the counselor level, counselors might have changed their communication behavior not only in the intervention group but also in the UC-group consultations as an effect of the intervention. This might have led to an underestimation of the intervention effects.
Conclusion
This study showed that a pre-visit website with QPS indeed empowered counselees by making them more assertive, e.g., in sharing their agenda, directing the communication, and checking whether or not they had understood the counselor. However, it did not result in more counselee questions or more overall counselee talk. Counselors who received QPS questions in advance introduced and answered these in the visit. As a result, information was more specific to whether the counselee received an indication for DNA testing without affecting the visit duration.
Disclosure
The authors declare no conflict of interest.
References
Biesecker BB . Goals of genetic counseling. Clin Genet 2001;60:323–330.
ASCO. American Society of Clinical Oncology policy statement update: Genetic testing for cancer susceptibility. J Clin Oncol 2003;21:2397–2406.
Elwyn G, Gray J, Clarke A . Shared decision making and non-directiveness in genetic counselling. J Med Genet 2000;37:135–138.
Ellington L, Roter D, Dudley WN,et al. Communication analysis of BRCA1 genetic counseling. J Genet Couns 2005;14:377–386.
Ellington L, Baty BJ, McDonald J,et al. Exploring genetic counseling communication patterns: the role of teaching and counseling approaches. J Genet Couns 2006;15:179–189.
Roter DL, Erby LH, Larson S, Ellington L . Assessing oral literacy demand in genetic counseling dialogue: preliminary test of a conceptual framework. Soc Sci Med 2007;65:1442–1457.
Meiser B, Irle J, Lobb E, Barlow-Stewart K . Assessment of the content and process of genetic counseling: a critical review of empirical studies. J Genet Couns 2008;17:434–451.
Henneman L, Timmermans DR, van der Wal G . Public experiences, knowledge and expectations about medical genetics and the use of genetic information. Community Genet 2004;7:33–43.
Calsbeek H, Morren M, Bensing J, Rijken M . Knowledge and attitudes towards genetic testing: a two year follow-up study in patients with asthma, diabetes mellitus and cardiovascular disease. J Genet Couns 2007;16:493–504.
Morren M, Rijken M, Baanders AN, Bensing J . Perceived genetic knowledge, attitudes towards genetic testing, and the relationship between these among patients with a chronic disease. Patient Educ Couns 2007;65:197–204.
Mesters I, Ausems A, De Vries H . General public’s knowledge, interest and information needs related to genetic cancer: an exploratory study. Eur J Cancer Prev 2005;14:69–75.
Walter FM, Emery J, Braithwaite D, Marteau TM . Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Ann Fam Med 2004;2:583–594.
Butow PN, Lobb EA . Analyzing the process and content of genetic counseling in familial breast cancer consultations. J Genet Couns 2004;13:403–424.
Pieterse AH, van Dulmen AM, Ausems MG, Beemer FA, Bensing JM . Communication in cancer genetic counselling: does it reflect counselees’ previsit needs and preferences? Br J Cancer 2005;92:1671–1678.
Lobb EA, Butow PN, Meiser B,et al. Tailoring communication in consultations with women from high risk breast cancer families. Br J Cancer 2002;87: 502–508.
Pieterse AH, van Dulmen S, van Dijk S, Bensing JM, Ausems MG . Risk communication in completed series of breast cancer genetic counseling visits. Genet Med 2006;8:688–696.
Green MJ, Peterson SK, Baker MW,et al. Use of an educational computer program before genetic counseling for breast cancer susceptibility: effects on duration and content of counseling sessions. Genet Med 2005;7:221–229.
Wang C, Gonzalez R, Milliron KJ, Strecher VJ, Merajver SD . Genetic counseling for BRCA1/2: a randomized controlled trial of two strategies to facilitate the education and counseling process. Am J Med Genet A 2005;134A:66–73.
Butow P, Devine R, Boyer M, Pendlebury S, Jackson M, Tattersall MH . Cancer consultation preparation package: changing patients but not physicians is not enough. J Clin Oncol 2004;22:4401–4409.
Kinnersley P, Edwards A, Hood K,et al. Interventions before consultations to help patients address their information needs by encouraging question asking: systematic review. BMJ 2008;337:a485.
Brown RF, Butow PN, Dunn SM, Tattersall MH . Promoting patient participation and shortening cancer consultations: a randomised trial. Br J Cancer 2001;85:1273–1279.
Dimoska A, Tattersall MH, Butow PN, Shepherd H, Kinnersley P . Can a “prompt list” empower cancer patients to ask relevant questions? Cancer 2008;113:225–237.
Epstein RM, Street RL . Patient-centered communication in cancer care: promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute, 2007.
Albada A, van Dulmen S, Otten R, Bensing JM, Ausems MG . Development of E-info gene(ca): a website providing computer-tailored information and question prompt prior to breast cancer genetic counseling. J Genet Couns 2009;18:326–338.
Albada A, Ausems MG, Otten R, Bensing JM, van Dulmen S . Use and evaluation of an individually tailored website for counselees prior to breast cancer genetic counselling. J Cancer Educ 2011;26:670–681.
Albada A, van Dulmen S, Lindhout D, Bensing JM, Ausems MG . A pre-visit tailored website enhances counselees’ realistic expectations and knowledge and fulfils information needs for breast cancer genetic counselling. Fam Cancer 2011. DOI: 10.1007/s10689-011-9479-1.
Roter DL, Larson SM, Beach MC, Cooper LA . Interactive and evaluative correlates of dialogue sequence: a simulation study applying the RIAS to turn taking structures. Patient Educ Couns 2008;71: 26–33.
STOET, Association Clinical Genetics Netherlands, Working Group Clinical Oncogenetics. Hereditary tumours: Guidelines for diagnostics and prevention [Erfelijke tumoren: Richtlijnen voor diagnostiek en preventie]. Leiden, The Netherlands: STOET, 2010.
Noldus LP, Trienes RJ, Hendriksen AH, Jansen H, Jansen RG . The Observer Video-Pro: new software for the collection, management, and presentation of time-structured data from videotapes and digital media files. Behav Res Methods Instrum Comput 2000;32: 197–206.
Roter D, Larson S . The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns 2002;46:243–251.
Pieterse A, van Dulmen S, Ausems M, Schoemaker A, Beemer F, Bensing J . QUOTE-gene(ca): development of a counselee-centered instrument to measure needs and preferences in genetic counseling for hereditary cancer. Psychooncology 2005;14:361–375.
Clayton JM, Butow PN, Tattersall MH,et al. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol 2007;25: 715–723.
Roter D. The Roter Method of Interaction Process Analysis. Johns Hopkins School of Public Health: Baltimore, MD, 2006.
Higgins JPT, Green S (eds). Cochrane Handbook for Systematic Reviews of Interventions 4.2.6. Wiley: Chichester, UK, 2006.
Hox JJ. Multilevel Analysis, Techniques and Applications. Taylor & Francis: London, 2010.
Schlich-Bakker KJ, ten Kroode HF, Ausems MG . A literature review of the psychological impact of genetic testing on breast cancer patients. Patient Educ Couns 2006;62:13–20.
Pieterse AH, van Dulmen AM, Beemer FA, Ausems MG, Bensing JM . Tailoring communication in cancer genetic counseling through individual video-supported feedback: a controlled pretest-posttest design. Patient Educ Couns 2006;60:326–335.
Kessels RP . Patients’ memory for medical information. J R Soc Med 2003;96:219–222.
Sousa DA . Memory, retention and learning. In: Sousa DA (ed). How the Brain Learns. Sage: Thousand Oaks, CA, 2006:77–116.
Kausmeyer DT, Lengerich EJ, Kluhsman BC, Morrone D, Harper GR, Baker MJ . A survey of patients’ experiences with the cancer genetic counseling process: recommendations for cancer genetics programs. J Genet Couns 2006;15:409–431.
Acknowledgements
We thank the counselees who participated in this study. We also thank the clinical geneticists, genetic counselors, and residents in clinical genetics of the Department of Medical Genetics of the University Medical Center Utrecht, in particular Angela Schoemaker and Ivette Wieffer who arranged study logistics. Also, we thank Tesse van Velduyzen, Paulien Groen-Van Dorsten, and Kirsty Gortzak for coding the videotapes. This study was funded by a grant from the Dutch Cancer Society (Nivel2006-3469).
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1.
(TIFF 1565 kb)
Rights and permissions
About this article
Cite this article
Albada, A., van Dulmen, S., Ausems, M. et al. A pre-visit website with question prompt sheet for counselees facilitates communication in the first consultation for breast cancer genetic counseling: findings from a randomized controlled trial. Genet Med 14, 535–542 (2012). https://doi.org/10.1038/gim.2011.42
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2011.42
Keywords
This article is cited by
-
Communication about breast cancer genetic counseling with patients with limited health literacy or a migrant background: evaluation of a training program for healthcare professionals
Journal of Community Genetics (2021)
-
Online BRCA1/2 screening in the Australian Jewish community: a qualitative study
Journal of Community Genetics (2020)
-
Community attitudes towards a Jewish community BRCA1/2 testing program
Familial Cancer (2017)
-
Counselees’ Expressed Level of Understanding of the Risk Estimate and Surveillance Recommendation are Not Associated with Breast Cancer Surveillance Adherence
Journal of Genetic Counseling (2016)
-
Design and Feasibility of an Intervention to Support Cancer Genetic Counselees in Informing their At‐Risk Relatives
Journal of Genetic Counseling (2016)