Abstract
Purpose: This study evaluates the Alzheimer disease risk perceptions of individuals who accurately recall their genetics-based Alzheimer disease risk assessment.
Methods: Two hundred forty-six unaffected first-degree relatives of patients with Alzheimer disease were enrolled in a multisite randomized controlled trial examining the effects of communicating APOE genotype and lifetime Alzheimer disease risk information.
Results: Among the 158 participants who accurately recalled their Alzheimer disease risk assessment 6 weeks after risk disclosure, 75 (47.5%) believed their Alzheimer disease risk was more than 5% points different from the Alzheimer disease risk estimate they were given. Within this subgroup, 69.3% believed that their Alzheimer disease risk was higher than what they were told (discordant high), whereas 30.7% believed that their Alzheimer disease risk was lower (discordant low). Participants with a higher baseline risk perception were more likely to have a discordant-high risk perception (P < 0.05). Participants in the discordant-low group were more likely to be APOE ε4 positive (P < 0.05) and to score higher on an Alzheimer disease controllability scale (P < 0.05).
Conclusion: Our results indicate that even among individuals who accurately recall their Alzheimer disease risk assessment, many people do not take communicated risk estimates at face value. Further exploration of this clinically relevant response to risk information is warranted.
Similar content being viewed by others
Main
Recalling and interpreting probabilistic disease risk information is often difficult for patients.1–4 One area of medicine where such risk information is heavily used is the rapidly growing field of genetic susceptibility testing for common, complex diseases. Within the medical genetics literature, patients' knowledge of their disease risk appears to improve after genetic counseling but remains far from perfect. Across nearly a dozen studies in the hereditary breast and ovarian cancer literature, the proportion of patients who accurately stated their breast cancer risk at baseline ranged from 6.6–59% and improved to 14.6–82% after receiving genetic counseling.5–15 The broad variation in the proportion of “accurate” responders may reflect differences in how the risk was communicated (e.g., relative risk versus absolute risks), how accuracy was measured (e.g., exact risk recall versus within 200% of the quoted risk estimate), and when the follow-up was conducted (e.g., immediately after the counseling session versus 3 months later).
Even if accurate knowledge of risk information was measured in a more systematic way, this variable is an imperfect measure of risk communication efficacy. Several authors have argued that evaluations of risk communication processes should not focus solely on patients' knowledge of risk information but also on their perception of risk.1,3,16 Risk perception is a key concept in the self-regulation model of genetic counseling described by Shiloh17 and may play an important role in patients' subsequent psychological adjustment and health behaviors, such as obtaining cancer screening.4,5,18
Two recent systematic reviews suggest that genetic counseling may improve the accuracy of patients' risk perception, but the results have been inconsistent across studies.18,19 Several studies have suggested that cognitive and emotional factors, such as personal experience and disease-specific worry, and demographic characteristics, such as age, gender, and education, have a greater impact on risk perception than the actual risk estimates provided by health care professionals.19–23 However, these studies have not directly and simultaneously evaluated both patients' knowledge of the risk provided by their clinician and their postcounseling risk perception. Without this comparison, it is impossible to tell whether the discrepancies between patients' postcounseling perceived risk and the communicated risk assessment are because of inaccurate recall of the factual information or other psychosocial factors suggested above. A clear delineation between the recall of factual information (i.e., communicated risk) and the interpretation of that information (perceived risk) is, therefore, needed. Defining appropriate risk recall and risk perception outcomes is especially important when evaluating genetic susceptibility testing, given the imprecision inherent in these risk models and the expected growth in their utilization across multiple common adult-onset diseases, both within the health care system and via direct-to-consumer “personal genomics” services.24–26
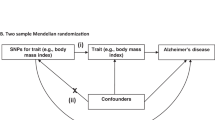
To begin addressing these important issues, we explored the relationship between risk recall and risk perception among individuals who demonstrated an accurate recall of their quoted Alzheimer disease (AD) risk assessment, using data from a randomized clinical trial involving disclosure of APOE genotype information to first-degree relatives of patients with AD. We posed two hypotheses based on the available risk recall and risk perception literature and findings from our earlier work: (1) participants' perceived risk of AD would differ significantly from their accurately recalled risk estimates; and (2) certain personal characteristics (e.g., older age, female gender, lower education or numeracy, and higher disease-specific worry) would be associated with discordance between recalled and perceived AD risk.27–29
MATERIALS AND METHODS
Overview
This post hoc analysis was conducted using data collected during the second funding period of a multicenter National Institute of Health-funded clinical trial, the Risk Evaluation and Education for Alzheimer's Disease (REVEAL) study. The REVEAL study was designed to evaluate the safety, efficacy, and impact of providing genetic-based AD risk assessments to first-degree relatives of patients with AD. Details regarding the development of the AD risk estimates, study methods, and primary study outcomes from the first clinical trial have been reported elsewhere.30,31 These findings indicate that, in the context of a comprehensive education and counseling protocol, APOE genotype and AD risk information can be provided to first-degree relatives of AD patients in a relatively safe and effective manner.27,31–33
A second clinical trial was developed to examine the safety and efficacy of providing APOE genotype disclosure and risk assessment through a condensed educational, risk disclosure, and counseling protocol. This second clinical trial is the basis for the current analysis and is described in more detail in the Participants and Procedures sections below. Institutional review board approval was obtained at each of the four study sites: Boston University, Weill Medical College of Cornell University, Case Western Reserve University, and Howard University. All study participants completed an informed consent process at the time of enrollment.
Participants
Cognitively intact men and women who were aged older than 18 years and who had one living or deceased first-degree relative affected by late-onset AD were eligible for study participation. Individuals who had more than one affected first-degree relative or whose affected family members' average age of AD onset was <60 years old were excluded. Participants were self-referred, having typically heard about the REVEAL Study through the internet, community outreach events, word-of-mouth, or through other AD research studies at the respective REVEAL Study sites.
Of the 437 individuals who expressed interest in the study, 131 declined participation, 14 did not meet family history eligibility criteria, and 12 were screened out because of possible cognitive, mood, or anxiety disorders. The resulting 280 participants received AD risk assessment and completed the 6-week follow-up visit (Fig. 1). Thirty-four participants were excluded from this analysis because of inadequate data for the communicated risk, risk recall, and/or risk perception measures. African Americans (participants were asked to self-identify their race/ethnicity and these variables were included in the study after careful consideration, which is described in detail in Ref.34), condensed protocol participants, individuals with only one affected relative in their immediate and extended family, and individuals with lower numeracy scores were significantly overrepresented among those with missing data (P < 0.05; data not shown). A total of 246 participants were included in the final analysis.
Procedures
Demographic information and baseline AD-related attitudes were assessed during a brief phone interview. Individuals who elected to continue participating in the study were then randomized to one of two AD genetics education and counseling protocols. The same information regarding AD risk factors, the relationship between APOE genotype and AD risk, and the potential risks and benefits of receiving genetic testing was provided to all participants. However, participants in the condensed arm were educated via a four-page brochure mailed to their home in advance of their genetic counseling and testing appointment. Participants in the extended arm attended a separate in-person education session conducted by a genetic counselor before their genetic counseling and testing appointment.
The same protocol was used for all participants, regardless of study arm, during the genetic counseling and testing appointment. After the administration of pretest surveys, participants were screened for symptoms of cognitive impairment, anxiety, and depression. The genetic counselor then reviewed the participant's family history of AD and offered to review the educational materials and address any participant questions or concerns before continuing with the blood draw. Samples from eligible consenting participants were sent to a CLIA-approved laboratory (Athena Diagnostics, Worcester, MA) for genotype analysis.
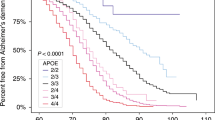
At the in-person disclosure session, participants in both arms of the study received their APOE genotype results and an estimated lifetime risk of developing AD, which was defined as the risk of developing AD from birth to age of 85 years. The estimates were based on gender- and genotype-specific AD risk curves developed for African American and white participants.34 As illustrated in Table 1 participants who carried at least one copy of the APOE ε4 allele were given lifetime AD risk estimates ranging from 25–77%. Individuals without an APOE ε4 allele received lifetime AD risk estimates from 13–49%.30,34 Participants were shown a set of graphs representing the age-, gender- and race-specific AD risks for various groups, including (1) the general population, (2) first-degree relatives of patients with AD, and (3) individuals classified by APOE genotype. A standard script was used to provide participants with a verbal explanation of their AD risk estimate and the personal information that was used to generate the risk estimate (e.g., their APOE genotype, family history, gender, race, and age). Participants also received a standardized written summary of the risk estimate and its limitations. No formal review of the pretest educational material was offered, but participants were free to ask questions and discuss any concerns related to their test results. Participants were asked to complete three follow-up surveys during the 12 months after AD risk disclosure. We focus solely on 6-week follow-up data in this analysis because of its close proximity to the risk disclosure session. Similar results were also found at the 6-month and 12-month follow-up time points, but the sample size decreased as fewer participants accurately recalled their risk estimates at these later dates (data not shown).
Measures
For the purposes of this analysis, communicated risk refers to the AD risk estimate provided by the study clinician during the disclosure session. As part of both the preeducation (baseline) survey and the 6-week follow-up survey, perceived personal risk was measured by asking “On a scale of 0–100%, what do you believe your chances are of developing Alzheimer's disease sometime in your life?” Although Katapodi et al.35 have suggested that using this type of numerical scale may lead to a bias toward responses of 50%, we chose this measure of perceived personal risk to allow for direct comparisons with the communicated risk estimates that were provided on the same scale (Table 1).
In a separate section of the 6-week follow-up survey, participants were asked to “Please write in (or approximate if you can't remember the exact number) the percentage you were given as your lifetime risk of developing Alzheimer's disease.” This number was recorded as the recalled risk. If the recalled risk was within ±5 points of the communicated risk, the participant was considered to have accurately recalled risk. Three risk recall-perception subgroups were established among those participants who accurately recalled their AD risk assessment: concordant, discordant-high, and discordant-low (see Fig. 1 for definitions) groups.
Before the educational component of the protocol, participants completed three measures of AD-related attitudes. To assess AD concern, participants used a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree) to rate five statements regarding their concern over potentially developing AD and the severity of AD relative to other conditions. AD treatment optimism was also measured on the same 5-point Likert scale, with participants responding to six statements regarding the likelihood of new preventive, treatment, and/or curative agents for AD being developed within the next 5 years or within their lifetime. Perceptions of personal control over the development of AD were assessed, again using the 5-point Likert scale, with four questions measuring the degree to which the participant believed the onset or severity of AD could be modified by personal actions. Items used for each scale were based on measures used with good reliability (Cronbach α = 0.78–0.88) in previous research on illness perceptions among relatives of people with AD.36,37
Anxiety was measured using the Beck Anxiety Inventory, with higher scores indicating greater levels of generalized anxiety.38 The Center for Epidemiological Studies-depression scale was also administered, with higher scores indicating a greater level of depression symptoms.39
Participants provided their age, gender, race, highest year of schooling completed, annual household income, and number of first-degree and more distant relatives affected by AD. In addition to these basic sociodemographic variables, we also assessed participants' health numeracy, which has been defined as “the degree to which individuals have the capacity to access, process, interpret, communicate, and act on numerical, quantitative, graphical, biostatistical, and probabilistic health information needed to make effective health decisions.”40 Numeracy scores for each participant were measured using a well-validated measure from Lipkus et al.,41 with scores ranging from 0 (low numeracy) to 8 (high numeracy). Because the distribution of numeracy scores was skewed toward high levels of numeracy, we created a dichotomous variable of lower (score of 6 or lower) versus higher (score of 7 or 8) numeracy.
Data analysis
Unadjusted Fisher exact tests were used to detect significant demographic differences between the concordant and discordant-high groups and the concordant and discordant-low groups. Between-group differences in the mean values for continuous measures of baseline AD risk perception, AD concern, AD treatment optimism, and AD control, anxiety, and depression were assessed with independent Student t tests.
In addition to exploring potential associations between group status and demographic characteristics, baseline AD attitudes, and general mood, we also sought to identify potential predictors of group status using a stepwise multinomial logistic regression model. Six variables were selected for inclusion in the regression model based on theorized predictors of perceived personal risk from the literature: baseline measures of perceived personal risk, depression, anxiety, AD concern, and AD control score, and APOE ε4 status.17,19,42,43 Gender, race, and age group were added as potential confounders. We hypothesized that baseline AD risk perception would be the strongest predictor of group membership. SPSS 14.0 was used to conduct all statistical analyses.44
RESULTS
Participant information
Of the 246 participants with valid data for this question, 101 (41.1%) recalled their AD risk estimate exactly, whereas another 57 (23%) accurately recalled their AD risk within ±5% points of their communicated risk. The risk estimate recall of these 158 participants (64.2% of the sample) was categorized as “accurate” for the purposes of this analysis. The remaining 88 participants were considered “inaccurate” and were more likely to be ≥60 years old (P ≤ 0.01), female (P ≤ 0.05), have a lower numeracy score (P ≤ 0.05), and report that they had been a primary caregiver for a relative with AD (P ≤ 0.05) when compared with participants with accurate recall. These findings are consistent with similar analyses conducted on participants from our previous clinical trial conducted with a different group of participants.27
All of the following analyses were restricted to the subset of 158 participants who accurately recalled their risk estimate; their demographic characteristics are reported in Table 2. We found no significant differences in our primary outcome measures when comparing participants in the condensed study arm with those in the extended study arm (Table 2). Accordingly, the regression analyses described in Tables 3 and 4, reflect all 158 participants and are not stratified by study arm.
Communicated AD risk estimates and AD risk perception
At baseline, the mean perceived personal risk of developing AD among our sample was 53.0% (SD = 22.03; range = 0–100%). Within this group, a significant decrease in mean perceived personal risk was observed 6 weeks after risk disclosure (mean = 43.3%; SD = 23.5; P < 0.01). However, the 6-week follow-up mean perceived personal risk remained significantly higher than the mean communicated risk of 36.8% (SD = 15.5; P < 0.01).
This pattern held true within most of the demographic groups described in Figure 2. However, the mean baseline perceived personal risk among African Americans was lower than both the group mean communicated risk and 6-week perceived personal risk. In addition, the mean 6-week perceived personal risk value among participants aged 60 years and older was virtually identical to their mean communicated risk.
Mean baseline perceived personal risk values were significantly higher among women relative to men; among whites relative to African Americans; and among younger participants relative to older participants (P-values for all group differences ≤0.05). Six weeks after risk disclosure, group-level differences in mean perceived personal risk remained significant between the gender and age groups (P ≤ 0.05), but not between the racial groups. Although it is not surprising that, at the 6-week follow-up time point, participants who were positive for at least one APOE ε4 allele perceived their AD risk to be significantly higher than APOE ε4 negative participants, it is interesting to note that APOE ε4 positive participants also reported a significantly higher mean baseline perceived personal risk than their APOE ε4 negative counterparts (P ≤ 0.05).
Postassessment risk perception among participants demonstrating accurate risk recall
Just more than half (52.5%) of the participants were classified as concordant in terms of their risk recall and risk perception responses. Figure 3 describes the distribution of individuals who provided responses that were concordant, discordant high (n = 52), and discordant low (n = 23). Of note, 36 of the 52 participants in the discordant-high group (22.8% of all accurate recallers) stated that their perceived personal risk was more than 20% points higher than their accurately recalled risk.
Characteristics of participants in the discordant-low and discordant-high groups
As given in Table 2, African Americans were significantly overrepresented in the discordant-low group relative to whites. There was also a trend toward APOE ε4 positive participants being overrepresented in the discordant-low arm (P < 0.10). Table 3 illustrates that, in comparison with the concordant group, discordant-low participants also had higher mean baseline scores on measures of AD control (3.47 vs. 3.01, P ≤ 0.01) and anxiety (5.43 vs. 2.76, P ≤ 0.01). However, the mean anxiety score of discordant-low participants still fell well below clinically significant levels.38 Finally, participants in the discordant-high group had a significantly higher baseline AD risk perception (65 vs. 48%, P ≤ 0.01) when compared with the concordant group.
Predictors of discordant-low and discordant-high group status
The results of the full regression model are reported in Table 4. Three statistically significant predictors of group status were observed. For every 1-point increase in baseline perceived risk, the odds ratio of being in the discordant-high group (versus the concordant group) increased by 1.06 (95% confidence interval [CI] = 1.03–1.09). When comparing the discordant-low group with the concordant group, a 1-point increase in a participant's baseline score on the personal control over AD scale increased the odds of being in the discordant-low group by 3.0 (95% CI = 1.23–7.26). In addition, participants who were found to be APOE ε4 positive were nearly six times more likely to be in the discordant-low group than in the concordant group (95% CI = 1.66–20.69). In earlier stepwise regression models (data not shown) and in the unadjusted Fisher exact test given in Table 2, African Americans were significantly more likely to be in the discordant-low group. However, once baseline anxiety scores were included, this relationship was no longer significant.
DISCUSSION
This study examined the perceived AD risk of individuals who accurately recalled their communicated AD risk. Among those who accurately recalled their communicated risk, nearly one half did not fully adjust their perceived personal risk of AD to match their communicated AD risk estimate. Our findings suggest that baseline perceived AD risk, baseline feelings of control over AD, and genotype information are the strongest predictors of these discordant risk perceptions.
We found that participants modify their perceived personal risk of AD in the direction of the mean communicated risk after genetic education and counseling. However, as a group, the posttest mean perceived personal risk remains somewhere in between baseline the mean perceived personal risk and the mean communicated risk. This pattern held true within each of the observed sociodemographic subgroups (Fig. 2).
In addition, we observed wide variation in posttest perceived personal risk among individual study participants who accurately recalled their AD risk estimate. Nearly one third of the participants with accurate risk recall reported their posttest perceived personal risk to be higher than their recalled risk, which we referred to as being discordant high. Conversely, approximately 15% felt that their AD risk was lower than their accurately recalled risk and were subsequently referred to as being discordant low. Our logistic regression analysis found that greater baseline levels of perceived personal risk were predictive of being in the discordant-high category, whereas greater baseline feelings of control over developing AD and testing positive for one more APOE ε4 alleles were each predictive of being in the discordant-low group.
There are several plausible explanations as to why some participants do not adjust their perceived disease risk to match their personalized health risk assessments. One explanation involves an anchoring-and-adjustment bias,45 which is described as the adjustment of perceived risk toward—but not equal to—the objective risk provided by health care providers. Our results shown in Figure 2 illustrate this phenomenon. In addition, the significant relationship between higher baseline levels of perceived risk and being in the discordant-high group may be related at least in part to anchoring-and-adjustment biases.
Similar results from two recent studies suggest that the anchoring-and-adjustment bias exists across various diseases and risk groups. Weinstein et al.29 surveyed 353 individuals scheduled for nonurgent primary care appointments immediately before and after a computer-based presentation on colon cancer risks. Among the participants randomized to receive a personalized colorectal cancer risk estimate, only 45% reported agreement between their recalled communicated risk and personal risk perception, whereas 47% perceived their risk to be higher than the communicated risk estimate.29 Discordance between participants' postintervention perceived risk and their self-reported communicated risk was associated with their baseline perceived risk of colon cancer. Gurmankin et al.28 examined the risk recall and perception of 108 women who received genetic counseling for (1) their risk of carrying a mutation in the BRCA1/2 genes that confer high risk of breast and/or ovarian cancer and (2) their risk of being diagnosed with breast cancer. Although the group's postcounseling perceived risks were significantly higher than their recalled communicated risks, they were also significantly lower than their baseline perceived risk.28
In addition to the potential subconscious anchoring-and-adjustment bias, participants may have made rational adjustments to their risk estimates based on their understanding of less well-defined risk or protective factors that are not included in the REVEAL study's AD risk calculations. For example, participants who regularly engage in rigorous mental or physical activity may have perceived their personal AD risk to be somewhat lower than the communicated risk, given their beliefs about the protective effects of their lifestyle. Although there has been a considerable amount of lay press coverage of the potential AD risk-reducing benefits of mental and physical exercise, the risk estimates used in this study do not incorporate this information.30 Future studies in this area should ascertain what, if any, additional objective factors participants consider when interpreting their disease risk.
Although participants may be incorporating unmeasured risk factors into their perceived personal risk of AD, it is also likely that individual attributes, such as coping style, influence risk perception.19 Previous work with participants in the first REVEAL study clinical trial suggests that receiving a personalized AD risk estimate may increase feelings of control or reduce feelings of uncertainty, thereby serving both problem-focused and emotion-focused coping mechanisms.46 Our current finding that APOE ε4 positive individuals are more likely to be in the discordant-low group also suggests that minimizing one's perceived AD risk is another a way to cope with unfavorable risk information. This explanation is supported by the work of Etchegary and Perrier,42 who provide a comprehensive review of “defensive processing of threatening health information.” In brief, individuals may use various cognitive mechanisms to cope with the distress related to the communicated risk estimate. Enhanced coping may be psychologically beneficial, but the associated risk minimization could be detrimental if it undermines positive health behaviors that the individual might have otherwise enacted.
This study has several limitations. As in most clinical trials, the sample was predominantly composed of individuals with high levels of education. In addition, educational materials and clinician reminders that emphasized the limitations of risk estimates may have given credence to participants' notions that their actual risk differed from their communicated risk. Future studies should consider assessing participants' perceptions of the precision and accuracy of the communicated risk and exploring reasons for discordance. It is also noteworthy that although the disclosure of AD risk estimates and their limitations was standardized across providers and study sites, participants were free to ask their clinician clarifying questions and engage in further conversation. We are unable to systematically evaluate or adjust for the content of such additional conversations, which could have had an effect on how the participant recalled or perceived their AD risk estimate. Finally, although the relatively high number of African American participants is strength of the study, the small number of African Americans in the discordant-high group limited this particular analysis.
CONCLUSIONS
This study examined the perceived AD risk of individuals who accurately recalled their communicated AD risk. Among those who accurately recalled their communicated risk, nearly one half did not fully adjust their perceived personal risk of AD to match their provided objective AD risk estimate. Clinicians and researchers should not assume that accurate patient recall of communicated disease risk means that the patient has internalized the communicated risk. Clinicians should consider asking their patients how they view the objective risk estimate and why they do or do not feel that the objective risk fully applies to them. By engaging in this type of discussion, clinicians have an opportunity to address some of the cognitive and psychosocial reasons why some patients do not fully adjust their perceived personal risk to match their objective disease risk. Through these conversations, clinicians may be able to reduce barriers to future clinician-patient communication, improve compliance with disease prevention recommendations, and encourage positive health behavior change. Given that genetic susceptibility testing is likely to become an increasingly used tool in health care, it will be important to continue to investigate risk communication dynamics in this context to enhance patient and clinician education.
References
Evans D, Burnell L, Hopwood P, Howell A . Perception of risk in women with a family history of breast cancer. Br J Cancer 1993; 67: 612–614.
Lipkus IM, Rimer BK, Strigo TS . Relationships among objective and subjective risk for breast cancer and mammography stages of change. Cancer Epidemiol Biomarkers Prev 1996; 5: 1005–1011.
Schwartz LM, Woloshin S, Black WC, Welch HG . The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med 1997; 127: 966–972.
Woloshin S, Schwartz LM, Black WC, Welch HG . Women's perceptions of breast cancer risk: how you ask matters. Med Decis Making 1999; 19: 221–229.
Cull A, Anderson ED, Campbell S, Mackay J, Smyth E, Steel M . The impact of genetic counselling about breast cancer risk on women's risk perceptions and levels of distress. Br J Cancer 1999; 79: 501–508.
Cull A, Miller H, Porterfield T, et al. The use of videotaped information in cancer genetic counselling: a randomized evaluation study. Br J Cancer 1998; 77: 830–837.
Evans DG, Blair V, Greenhalgh R, Hopwood P, Howell A . The impact of genetic counselling on risk perception in women with a family history of breast cancer. Br J Cancer 1994; 70: 934–938.
Hopwood P . Genetic risk counselling for breast cancer families. Eur J Cancer 1998; 34: 1477–1479.
Hopwood P, Howell A, Lalloo F, Evans G . Do women understand the odds? Risk perceptions and recall of risk information in women with a family history of breast cancer. Community Genet 2003; 6: 214–223.
Hopwood P, Shenton A, Lalloo F, Evans DG, Howell A . Risk perception and cancer worry: an exploratory study of the impact of genetic risk counselling in women with a family history of breast cancer. J Med Genet 2001; 38: 139.
Lerman C, Lustbader E, Rimer B, et al. Effects of individualized breast cancer risk counseling: a randomized trial. J Natl Cancer Inst 1995; 87: 286–292.
Liden A, Berglund G, Hansson MG, Rosenquist R, Sjoden PO, Nordin K . Genetic counselling for cancer and risk perception. Acta Oncol 2003; 42: 726–734.
Meiser B, Butow PN, Barratt AL, et al. Long-term outcomes of genetic counseling in women at increased risk of developing hereditary breast cancer. Patient Educ Couns 2001; 44: 215–225.
Nordin K, Liden A, Hansson M, Rosenquist R, Berglund G . Coping style, psychological distress, risk perception, and satisfaction in subjects attending genetic counselling for hereditary cancer. J Med Genet 2002; 39: 689–694.
Watson M, Lloyd S, Davidson J, et al. The impact of genetic counselling on risk perception and mental health in women with a family history of breast cancer. Br J Cancer 1999; 79: 868–874.
Lipkus IM, Crawford Y, Fenn K, et al. Testing different formats for communicating colorectal cancer risk. J Health Commun 1999; 4: 311–324.
Shiloh S . Illness representations, self-regulation, and genetic counseling: a theoretical review. J Genet Couns 2006; 15: 325–337.
Smerecnik CM, Mesters I, Verweij E, de Vries NK, de Vries H . A systematic review of the impact of genetic counseling on risk perception accuracy. J Genet Couns 2009; 18: 217–228.
Sivell S, Elwyn G, Gaff CL, et al. How risk is perceived, constructed and interpreted by clients in clinical genetics, and the effects on decision making: systematic review. J Genet Couns 2008; 17: 30–63.
d'Agincourt-Canning L . The effect of experiential knowledge on construction of risk perception in hereditary breast/ovarian cancer. J Genet Couns 2005; 14: 55–69.
Huiart L, Eisinger F, Stoppa-Lyonnet D, et al. Effects of genetic consultation on perception of a family risk of breast/ovarian cancer and determinants of inaccurate perception after the consultation. J Clin Epidemiol 2002; 55: 665–675.
Kelly K, Leventhal H, Andrykowski M, et al. Using the common sense model to understand perceived cancer risk in individuals testing for BRCA1/2 mutations. Psychooncology 2005; 14: 34–48.
Madlensky L, Flatt SW, Bardwell WA, Rock CL, Pierce JP . Is family history related to preventive health behaviors and medical management in breast cancer patients?. Breast Cancer Res Treat 2005; 90: 47–54.
McBride CM, Alford SH, Reid RJ, Larson EB, Baxevanis AD, Brody LC . Putting science over supposition in the arena of personalized genomics. Nat Genet 2008; 40: 939–942.
O'Neill SC, White DB, Sanderson SC, et al. The feasibility of online genetic testing for lung cancer susceptibility: uptake of a web-based protocol and decision outcomes. Genet Med 2008; 10: 121–130.
Robin NH, Tabereaux PB, Benza R, Korf BR . Genetic testing in cardiovascular disease. J Am Coll Cardiol 2007; 50: 727–737.
Eckert S, Katzen H, Roberts J, et al. Recall of disclosed apolipoprotein E genotype and lifetime risk estimate for Alzheimer's disease: the REVEAL Study. Genet Med 2006; 8: 746–751.
Gurmankin AD, Domchek S, Stopfer J, Fels C, Armstrong K . Patients' resistance to risk information in genetic counseling for BRCA1/2. Arch Intern Med 2005; 165: 523–529.
Weinstein ND, Atwood K, Puleo E, Fletcher R, Colditz G, Emmons KM . Colon cancer: risk perceptions and risk communication. J Health Commun 2004; 9: 53–65.
Cupples LA, Farrer LA, Sadovnick AD, Relkin N, Whitehouse P, Green RC . Estimating risk curves for first-degree relatives of patients with Alzheimer's disease: the REVEAL study. Genet Med 2004; 6: 192–196.
Green RC, Roberts JS, Cupples LA, et al. Disclosure of APOE Genotype for Risk of Alzheimer's Disease. N Engl J Med 2009; 361: 245–254.
LaRusse S, Roberts J, Marteau T, et al. Genetic susceptibility testing versus family history-based risk assessment: Impact on perceived risk of Alzheimer disease. Genet Med 2005; 7: 48–53.
Marteau TM, Roberts S, LaRusse S, Green RC . Predictive genetic testing for Alzheimer's disease: impact upon risk perception. Risk Anal 2005; 25: 397–404.
Christensen KD, Roberts JS, Royal CDM, et al. Incorporating ethnicity into genetic risk assessment for Alzheimer's disease: the REVEAL Study experience. Genet Med 2008; 10: 207–214.
Katapodi MC, Lee KA, Facione NC, Dodd MJ . Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med 2004; 38: 388–402.
Roberts J, Connell C, Cisewski D, Hipps Y, Demissie S, Green R . Differences between African Americans and whites in their perceptions of Alzheimer disease. Alzheimer Dis Assoc Disord 2003; 17: 19–26.
Roberts JS, Connell CM . Illness representations among first-degree relatives of people with Alzheimer disease. Alzheimer Dis Assoc Disord 2000; 14: 129–136.
Beck AT, Steer RA . Beck anxiety inventory manual. San Antonio, TX, Psychological Corporation 1993.
Roberts RE, Vernon SW . The Center for Epidemiological Studies-Depression Scale: its use in a community sample. Am J Psychiatry 1983; 140: 41–46.
Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE . A definition and operational framework for health numeracy. Am J Prev Med 2005; 29: 375–376.
Lipkus IM, Samsa G, Rimer BK . General performance on a numeracy scale among highly educated samples. Med Decis Making 2001; 21: 37–44.
Etchegary H, Perrier C . Information processing in the context of genetic risk: implications for genetic-risk communication. J Genet Couns 2007; 16: 419–432.
Rothman AJ, Kiviniemi MT . Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monogr 1999; 44–51.
SPSS for Windows [computer program]. Version 14.0. Chicago, IL, SPSS Inc 2005.
Senay I, Kaphingst KA . Anchoring-and-adjustment bias in communication of disease risk. Med Decis Making 2009; 29: 193–201.
Gooding H, Linnenbringer E, Burack J, Roberts J, Green R, Biesecker B . Genetic susceptibility testing for Alzheimer disease: motivation to obtain information and control as precursors to coping with increased risk. Patient Educ Couns 2006; 64: 259–267.
Acknowledgements
This work was supported by NIH Grants RO1-HG/AG02213 (REVEAL Study), P50-AG13846 (Boston University Alzheimer's Disease Center), K24-AG027841, RO1-AG09029 (The MIRAGE Study), and M01-RR00533 (Boston University General Clinical Research Center).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Linnenbringer, E., Roberts, J., Hiraki, S. et al. “I know what you told me, but this is what I think:” Perceived risk of Alzheimer disease among individuals who accurately recall their genetics-based risk estimate. Genet Med 12, 219–227 (2010). https://doi.org/10.1097/GIM.0b013e3181cef9e1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181cef9e1
Keywords
This article is cited by
-
Clinical implications of APOE genotyping for late-onset Alzheimer’s disease (LOAD) risk estimation: a review of the literature
Journal of Neural Transmission (2019)
-
Amnestic MCI patients’ experiences after disclosure of their amyloid PET result in a research context
Alzheimer's Research & Therapy (2017)
-
Uninformed consent in nutrigenomic research
European Journal of Human Genetics (2017)
-
Choosing not to undergo predictive genetic testing for hereditary colorectal cancer syndromes: expanding our understanding of decliners and declining
Journal of Behavioral Medicine (2017)
-
Effect of Public Deliberation on Attitudes toward Return of Secondary Results in Genomic Sequencing
Journal of Genetic Counseling (2017)