Abstract
Purpose: Racial and ethnic disparities in health are evident among a range of diseases and health care services. New genetic technologies are likely to increase these disparities as access to expensive genetic tests further widens the gap.
Methods: Our analysis used data from a national representative sample collected in 2000. The total sample size for our analysis was 1724 men and women (consisting of 946 non-Hispanic whites, 392 Latinos, and 386 blacks) aged 18 to 91 years. Ordered logistic regression and binary logistic regression analysis were applied to investigate differences by race/ethnicity.
Results: Results showed significant differences by racial/ethnic groups in knowledge and concerns about the potential misuse of genetic testing. A significant difference was also found between the types of health insurance coverage by race/ethnicity as well as significantly higher levels of mistrust in a physician and the medical system.
Conclusion: Our findings raise concern about several barriers among minorities and calls for a development of educational and communication strategies that facilitate in narrowing the gap between racial and ethnic groups.
Similar content being viewed by others
Main
Using national representative sample data, this article examines racial and ethnic differences in the following barriers to genetic testing: (a) knowledge about genetic testing; (b) type of health insurance coverage; (c) concerns about the potential misuse of genetic testing; and (d) lack of trust in a medical doctor to keep their medical information private. It uses a national representative sample and ordered and binary logistic regression analyses building on previous works by Singer et al.1,2
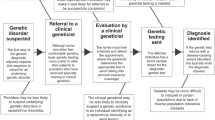
Genetic testing for predisposition of certain diseases is becoming common because scientific discoveries in the field of genetics and their implementation are enabling people to get speedy diagnosis of disease and treatments that are individually tailored with minimum side effects. These predictive genetic tests will allow individuals who wish to know information about their individual disease susceptibilities to take steps to reduce those risks.3
Access to expensive genetic tests is likely to further widen the gap between those who already receive the best care and those who do not.4 Racial and ethnic disparities in health continue to be evident among a range of diseases and health care services. Hence, genetic testing raises a number of issues pertinent to the provision of health care and the formulation of public policy.5 Genomic revelations propose to define human nature and alter the natural history of disease.6 However, caution must be taken about these expectations when social determinants of health are still significant factors globally affecting medicine in the 21st century.
Persistent inequities in access to health care could be intensified by advances in genetic knowledge.1,7 From past experience, those who will benefit most from these advances will probably be those who can afford to do so. Even the Healthy People 2010 revolves around low-cost solutions to public health issues such as increasing women's folic acid intake to prevent neural tube defects. But nowhere in this lengthy document does it push for access by the general population of women to costly genetic innovations such as genetic screening for breast or ovarian cancer.8 Genetics plays a role in approximately half of the 10 leading health indicators selected as public health issues in the Healthy People 2010 document.9 But of the total 467 objectives, only one deals specifically with genetics (newborn screening).
Genetic research has given us a greater understanding of the contribution of genes to health disparities.10 However, discussions regarding the implications or applications of genomic medicine have not included the perspectives of racial or ethnic groups.11 The socioecological model provides a useful framework for understanding the factors and barriers that influence racial and ethnic disparities in the use of genetic testing. An ecological model examines factors and behaviors from a multilevel perspective such as intrapersonal (knowledge, attitudes, beliefs), interpersonal (social norms and cultural acceptance), institutional and community (identification of resources and equal access to services), and policy (laws regarding confidentiality and discrimination).12,13 Each level is manipulated and reinforced by factors and behaviors from the other levels of influence.14
From an ecological perspective, interactions at all levels can provide opportunities or constraints15 in the utilization of genetic testing. For example, previous studies have found that African Americans and Hispanics are less likely to know about the availability of genetic testing for disease risk1,16–18 and African Americans are less likely to have confidence in the potential benefits of genetic testing than whites.16–18 Others found African American and Latino populations to be more likely to view genetic testing as interfering with “God's Will.”19,20 Other cultural issues such as discussing cancer risks with family members may also arise during genetic counseling and testing among minority populations.21 Thompson et al.19 showed evidence that African American women who declined BRCA1/2 counseling believed genetic testing to be just another attempt to stigmatize African Americans.
Apprehension about possible privacy breaches, stigmatization, and discrimination may cause physicians and consumers alike to avoid genetic-related services and participation in research.4 Historically, in the United States and in Europe, explanatory causes of particular diseases or social problems have been viewed as arising out of genetic material. For example, the eugenics movement in the United States in the early 1900 proposed solutions to social problems such as poverty by encouraging fertility among the upper and middle classes and discouraging childbearing among the lower socioeconomic groups. Another example is the period during which Nazi war criminals of the 1930 and 1940 singled out Jewish, gypsies, and homosexuals on the grounds that they were genetically inferior.11 More recently, the National Sickle Cell Anemia Control Act of 1972, which was intended to increase the availability of services for this trait, resulted in insurance and job discrimination against individuals carrying this trait.19
Although physicians are deluged with new genetic discoveries and ethical dilemmas, many lack the basic knowledge and skills necessary to incorporate genetic testing and genetic counseling into their practice.22,23 Many primary care practitioners lack information about genetic services and options available to patients.24 Not knowing which choices are available decreases their confidence to assess, counsel, and refer patients to services offered by genetic clinics. Lack of or poor knowledge of clinical cancer genetics lessens the chance that a high-risk patient will be referred to a genetic counselor for potential familial cancer inheritance.4
The characteristics of the primary care physicians of African American and non-Hispanic white women may reflect the differences in the use of primary prevention genetics such as BRCA1/2 counseling.17 Primary care physicians seen by African Americans experience more difficulty delivering specialized care than primary care physicians visited by non-Hispanic whites.25 Additionally, physicians treating black patients are less likely to be board certified. Shields et al.26 found that minority-serving physicians were less likely to order genetic testing and less likely to refer a patient to a genetic specialist or genetic counselor.
The discovery of genetic predisposition to chronic and inherited disease has set up the potential for discrimination in everything from who is marriageable to who is insurable. And if insurers are allowed to use genetic information in adjusting premiums, the burden of paying large if not impossible sums to obtain health care coverage will afflict numerous Americans who never thought of this as their problem.27 Patients who are employed in low-paying jobs with little or no health care benefits are more likely to experience barriers to genetic services for financial reasons. African Americans are less likely than non-Hispanic white Americans to have private or employment-based health insurance and more likely to be covered by Medicaid or other publicly funded insurance.5
Hypotheses
The purpose of this article is to examine racial and ethnic differences in barriers to genetic testing: (a) knowledge about genetic testing; (b) type of health insurance coverage; (c) concerns about the potential misuse of genetic testing; and (d) lack of trust in a medical doctor to keep their medical information private. The study posits the four null hypotheses stated below.
-
Hypothesis 1: There is no difference in knowledge about genetic testing by race/ethnicity.
-
Hypothesis 2: There is no variation in concerns about the misuse of genetic testing by race/ethnicity.
-
Hypothesis 3: There is no difference in the type of health insurance coverage among respondents by race/ethnicity.
-
Hypothesis 4: There is no difference in lack of trust in one's physician to keep medical information private by race/ethnicity.
MATERIALS AND METHODS
To achieve our aims and test the above hypotheses, a national representative sample of data collected in the year 2000 by the University of Maryland College Park Survey Research Center was used to investigate racial and ethnic disparities in knowledge and concerns about genetic testing. The specific barriers to genetic testing that are examined include knowledge, health insurance, concerns about misuse of testing, privacy and confidentiality concerns, and distrust in their medical doctor.
We conducted a power analysis for logistic regression with several predictor variables using the software PASS (Power Analysis and Sample Size) to determine the adequate sample size needed for our study. To achieve a power of 0.90 and medium effect size of 0.5 at a 0.05 significance level corresponding to an odds ratio (OR) of 1.50, a sample size between 1345 and 1794 was required depending on the value of R2 assumed. The total sample size for our analysis was 1724 men and women aged between 18 and 91 years. There were 946 non-Hispanic whites, 386 Latinos, and 351 blacks. For detailed information about study design, sample size, and other information see Ref. 1.
Four dependent variables were analyzed in detail: knowledge index about genetic testing, types of health insurance coverage, index regarding concerns about misuse of genetic testing, and mistrust in physicians. Following Singer et al.1 the knowledge index about genetic testing was constructed from seven questions (Cronbach's alpha = 0.65) by adding the number of correct answers given by each participant. Respondents who answered six or seven questions right were combined together. The constructed knowledge index variable is an ordinal variable and has six categories with a range of one to six. An index about respondent's concerns about misuse of genetic testing was created from eight questions (Cronbach's alpha = 0.71). This index is also an ordinal variable having three categories: 1, 2, and 3 where 1 shows the lowest concern and 3 shows the highest concern about the potential misuse of genetic testing. The questions used to create both indices are listed in the Appendix, Supplemental Digital Content, http://links.lww.com/A1431.
The third dependent variable investigated in this study is the respondents' type of health insurance: Medicare, Medicaid, private insurance, or any insurance (all analyzed separately). The type of health insurance variable had only two categories (yes or no). The last dependent variable examined is whether or not the respondent trusts his/her physician to keep medical information private. The question asks “How much do you trust your doctor to keep medical information about you private? (1) a great deal, (2) somewhat, (3) only a little, (4) hardly at all, (8) Don't know, (9) Refusal.” Those who answered (8) and (9) were small and were excluded from the final analysis. This variable is also an ordinal variable. In addition to race/ethnicity, the list of covariates used to predict each dependent variable outlined above include age, gender, marital status, education, employment, number of adults in the household, religiosity, whether the respondent knows anyone having a child born with a genetic defect, and region of residence.
Descriptive statistics were used to examine distribution of responses; χ2 tests were used to assess associations between race/ethnicity and all other predictor variables used in this study. Ordered logistic regression was applied for the ordinal dependent variables: knowledge index, concerns about potential misuse of genetic testing, and lack of trust in a medical doctor. Binary logistic regression was used for type of health insurance. All analyses used Statistical Analysis System (SAS, Version 9.1.3, Cary, NC). We presented the likelihood ratio χ2 test to assess our models goodness of fit. Additionally, McFadden's pseudo-R2 was used to indicate how useful the predictor variables were in predicting the dependent variable. Pseudo-R2 in logistic regression is analogous to the coefficient of determination (R2) used in linear regression.28,29 However, it does not have the same variance interpretation. Therefore, pseudo-R2 values should not be compared across datasets. Pseudo-R2 values between 0.2 and 0.4 are considered very satisfactory.29 The OR, also a measure of effect size in logistic regression,28 and its corresponding 95% confidence interval (CI), which measures the precision of the OR are also reported.
RESULTS
Table 1 shows the percentage distribution of respondents by race/ethnicity and all the predictor variables used in this study. It also presents a χ2 statistic together with its corresponding P value as a measure of association between each predictor variable and race/ethnicity. More than 70% of the respondents were 35 years or older. Fifty-nine percent of the respondents were females and 41% were males. More than half of the respondents were currently married or living with a partner, more than 85% have high school education or more, and about 70% were working either full time or part time. About 64% of respondents live in households where there are at least two adults and 39% of respondents attend religious services at least once a week. Overall, about 56% of respondents know someone having a child born with a genetic defect (63.5% for non-Hispanic whites, 43.8% for blacks, and 48.7% for Latinos). A test of association between the predictor variables considered in this analysis and race/ethnicity using a χ2 analysis show there is a significant difference at α = 0.05 level of significance except for employment status (α = 0.075).
Non-Hispanic white respondents tended to be older than both blacks and Latinos and blacks were less likely to be currently married (30.4%) than non-Hispanic whites (58.7%) and Latinos (53.8%). There was also a significant difference in the educational level of respondents by race. Latinos (31.3%) had the highest percentage of respondents with less than high school education and non-Hispanic whites (30.9%) had the highest percentage of respondents with college degree or higher education. Living arrangement measured by the number of adults in the household also varied considerably by race. Although about 52% of black respondents live in a household where there are two or more adults, about 68% of both non-Hispanic whites and Latinos live in a household where there are two or more adults. There was a significant variation in respondents' “attendance of religious services at least once a week” among non-Hispanic whites (35.9%), blacks (46.5%), and Latinos (37.1%). There was also substantial variation in knowing someone having a child born with a genetic defect by race/ethnicity. Although 63.5% of non-Hispanic whites reported that they know someone having a child born with a genetic defect, only 43.8% of blacks and 48.7% of Latinos answered affirmatively for the same question.
Table 2 presents OR from an ordered logistic regression model predicting knowledge about genetic testing. The likelihood ratio χ2 value (197.6, df 23, P < 0.001) shows the presented model fits the data well. The pseudo-R2 value (0.37) indicates that the model is highly satisfactory in predicting knowledge about genetic testing. After adjusting for all the variables included in the regression model, there was a strong association between race/ethnicity and knowledge about genetic testing. Both blacks and Latinos had significantly lower knowledge compared with non-Hispanic whites. Given that all other variables in the model are held constant, the odds of having adequate knowledge among blacks and Latinos compared with non-Hispanic whites was lower by 28% and 52%, respectively. Marital status was also significantly associated with respondent's knowledge about genetic testing. Comparing single versus currently married or living with a partner, the odds of higher knowledge about genetic testing was 1.63 times greater among singles than among currently married, given that all other variables in the model remain constant. As one would expect, education also played an important role in knowledge about genetic testing. Although having a less than high school education was negatively associated with knowledge (OR = 0.70, 95% CI 0.52–0.94) compared with high school education, having some college education (OR = 1.39, 95% CI 1.10–1.75) and college or more than college education (OR = 2.13, 95% CI 1.66–2.73) was positively associated. Being the only adult in a household was negatively associated with high knowledge score. Furthermore, knowing anyone having a child born with a genetic defect significantly increased knowledge score by 29% (OR = 1.29, 95% CI 1.07–1.57). The variables religiosity (measured by the frequency of religious services attendance), employment, and region of residence had no significant effect on knowledge about genetic testing.
Results of OR obtained from a logistic regression model by types of health insurance coverage found significant differences in the type of health insurance coverage by race/ethnicity. Compared with non-Hispanic whites, blacks were more likely to have Medicare (OR = 1.68) and/or Medicaid (OR = 2.51) and less likely to have private insurance (OR = 0.55). Latinos were less likely to have private insurance (OR = 0.49) or no insurance at all (OR = 0.60) compared with non-Hispanic whites. As expected (results are not shown), older respondents (aged 65 and older) were more likely to have Medicare and those 45 years old above had higher odds of having a private insurance compared with the 35 to 44 age group. Compared with women, men were more likely to have Medicare and Medicaid. Although single and previously married had higher odds of having Medicare and Medicaid, they were less likely to have private insurance. Education had also a significant effect on type of health insurance. On one hand, less than high school education was positively associated with Medicaid, but negatively associated with having private health insurance or having any other insurance at all. On the other hand, college education was negatively related with Medicare and Medicaid and positively related with having a private insurance or any insurance. In addition, being unemployed or working part time was positively associated with Medicare and Medicaid, but negatively associated with having a private insurance or any insurance.
Respondents were asked the extent they agree or disagree with the single statement “Information from genetic tests is likely to be misused.” Although 20% of non-Hispanic whites agree or strongly agree with the statement, more than one third of blacks (34%) and 28% of Latinos agree or strongly agree with the statement. This indicates there is substantial variability in concerns about the misuse of results from genetic testing by race/ethnicity with minorities expressing more concern than non-Hispanic whites.
Results from an ordered logistic regression model predicting more concerns about misuse of genetic testing are presented in Table 3. The overall model fit was good (χ2 = 76.2, df 23, P < 0.001) and the pseudo-R2 value (0.393) shows the usefulness of the model in predicting respondent's concerns about the misuse of genetic testing. The odds of blacks (OR = 1.66, 95% CI 1.28–2.15) and Latinos (OR = 1.58, 95% CI 1.21–2.07) being more concerned about the potential misuse of genetic testing versus non-Hispanic whites was higher by 66% and 58%, respectively. Gender was associated with concerns about the potential use of genetic testing. Men were 21% less likely to be concerned about the misuse of genetic testing than women. College-educated respondents were 37% less likely to be more concerned about the misuse of genetic testing compared with those with a high school degree. Religiosity was also significantly and positively associated with more concerns about the misuse of genetic testing. Age, marital status, employment, number of adults in the household, knowledge of someone having a child born with a genetic defect, and region were not associated with concerns about misuse of genetic testing.
Finally, Table 4 presents results from an ordered logistic regression model predicting respondent's lack of trust in their medical doctor in keeping information about them private. The overall model fit was good (χ2 = 58.7, df 23, P < 0.001) and the pseudo-R2 value (0.19) confirmed that the model was satisfactory in predicting lack of trust in a physician. Again, controlling for the effects of all the variables in the model, there was a significant difference in lack of trust in a physician by race/ethnicity. Compared with non-Hispanic whites, blacks and Latinos were more likely to distrust their medical doctor in keeping their medical information private by 48% and 64%, respectively. In addition, after taking into account the effects of all other covariates in the model, the odds of having a higher level of distrust were 1.39 times higher for men than for women. Except for race/ethnicity and gender, all other variables included in the model were not significant in predicting distrust in a medical doctor.
In summary, we posited four null hypotheses that stated there is no racial/ethnic difference in knowledge about genetic testing, concerns about the potential misuse of genetic testing, type of health insurance, and mistrust in a medical doctor. The results presented in this study strongly rejected these null hypotheses and provide strong evidence that there are significant differences in these barriers to genetic testing.
Limitations
The data used in the analyses were based on self-reports and social desirability response bias could be a potential problem. Additionally, although our findings may reflect true differences by race and ethnicity in genetic testing, the significant associations between race/ethnicity and the predictor variables used in this analysis may create a potential for confounding effects.
DISCUSSION
Ecological analyses suggest that individuals are influenced by circumstances in their day-to-day sociocultural and physical environments. Racial and ethnic disparities in genetic testing are reinforced by factors and behaviors on multiple levels: intrapersonal (knowledge and beliefs), interpersonal (social norms and cultural acceptance), institutional (identification of resources and equal access to services), and policy (laws regarding confidentiality and discrimination).
Blacks and Latinos are less likely to use genetic testing than non-Hispanic whites because of challenges and barriers they face including lack of knowledge or lack of adequate information provided by their physicians about genetic testing. Our analysis points to the need of educating minority populations about genetic testing so they will be able to make informed decisions about their own health and the health of their family members. Furthermore, education and counseling should be tailored to the educational level and socioeconomic status of the individual.30,31 As Hall and Olopade4 so aptly pointed out, the true power of knowledge is to be familiar with your own genetic risk or family history, which will enable you to ask your physician whether or not you should be tested.
There is a significant difference in health insurance coverage by race and ethnicity, which in turn may reflect the disparities in access to genetic testing. Although blacks are significantly more likely to be covered by Medicaid or Medicare than non-Hispanic whites, they have less private insurance coverage. For Latinos, they are less likely to be covered via a private health insurance. For both blacks and Latinos, the disparity in private health insurance coverage means less access to expensive genetic testing.
Distrust in the medical system has been determined to be higher among African Americans than non-Hispanic whites and may serve as a barrier to health care.19,32,33 Given the racial focus of the eugenics movement in the past, and historical experiences like the Tuskegee experiment, racial differences in attitudes about genetic testing in the general population are particularly important.16 Health care professionals who identify and address these cultural issues may increase the number of high-risk minorities who inquire about genetic counseling and are referred for risk-appropriate genetic services.34,35 In addition, information campaigns about the benefits of genetic testing that focus on minorities and promoting minority participation in genetic research are of paramount importance. Advancing the role that racial and ethnic minorities play in shaping and enhancing genetic research will further encourage the development of critical policies that address the ethical, social, and legal aspects of genomic medicine.
REFERENCES
Singer E, Antonucci T, Van Hoewyk J . Racial and ethnic variations in knowledge and attitudes about genetic testing. Genet Test 2004; 8: 31–43.
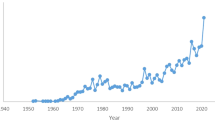
Singer E, Antonucci T, Van Hoewyk J . Attitudes toward genetic testing, 1990–2000. Int J Public Opin Res 2005; 17: 113–125.
Collins FS, McKusick VA . Implications of the human genome project for medical science. JAMA 2001; 285: 540–544.
Hall M, Olopade OI . Confronting genetic testing disparities. JAMA 2005;
Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C.: The National Academies Press, 2003.
Spellman MW . The human genome: cause to remember our humanity. Genet Med 2002; 4: 66s–67s.
Khoury MJ, Gwinn M, Yoon PW, Dowling N, Moore CA, Bradley L . The continuum of translation research in genomic medicine: how can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention?. Genet Med 2007; 9: 665–674.
Evans WJ, Britt DW . The genomic revolution and the obstetrician/gynaecologist: from societal trends to patient sessions. Best Pract Res Clin Obstet Gynaecol 2002; 16: 729–744.
Noonan AS . Key roles of government in genomics and proteomics: a public health perspective. Genet Med 2002; 4: 72S–76S.
Whitfield KE, Wiggins A, Brandon DT . Genetics and health disparities: fears and realities. J Natl Med Assoc 2003; 95: 539–543.
Schulz A, Caldwell C, Foster S . “What are they going to do with the information?” Latino/Latina and African American perspectives on the Human Genome Project. Health Educ Behav 2003; 3: 151–169.
Sallis JF, Owen N, Fisher EB . Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass, 2008: 465–485.
McLeroy KR, Bibeau D, Steckler A, Glanz K . An ecological perspective on health promotion programs. Health Educ Q 1988; 15: 351–377.
Hovell MF, Wahlgren DR, Gehrman CA . The behavioral ecological model: integrating public health and behavioral science. In: DeClemente RJ, Crosby RA, Kegler, editors. Emerging theories in health promotion practice and research: strategies for improving public health. San Francisco: Jossey-Bass, 2002: 362–370.
Glass TA, McAtee MJ . Behavioral science at the crossroads in pubic health: extending horizons, envisioning the future. Soc Sci Med 2006; 62: 1650–1671.
Peters N, Rose A, Armstrong K . The association between race and attitudes about predictive genetic testing. Cancer Epidemiol Biomarkers Prev 2004; 13: 361–365.
Armstrong K, Micco E, Carney A, Stopfer J, Putt M . Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA 2005; 293: 1729–1736.
Case AP, Ramadhani TA, Canfield MA, Wicklund CA . Awareness and attitudes regarding prenatal testing among Texas women of childbearing age. J Genet Couns 2007; 16: 655–661.
Thompson HS, Valdimarsdottir HB, Jandorf L, Red W . Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns 2003; 51: 217–227.
Phillips JM, Cohen MZ, Moses G . Breast cancer screening and African American women: fear, fatalism, and silence. Oncol Nurs Forum 1999; 26: 561–571.
Matthews AK, Cummings S, Thompson S, Wohl V, List M, Olopade OI . Genetic testing of African Americans for susceptibility to inherited cancers. J Psychosoc Oncol 2000; 18: 1–19.
Pagon RA, Pinsky L . The helix and health: applying genetics to primary care. West J Med 2001; 174: 304.
Suther S, Goodson P . Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genet Med 2003; 5: 70–76.
Watson E, Clements A, Yudkin P, et al. Evaluation of the impact of two educational interventions on GP management of familial breast/ovarian cancer cases: a cluster randomized controlled trial. Br J Gen Pract 2001; 51: 817–821.
Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL . Primary care physicians who treat blacks and whites. N Engl J Med 2004; 351: 575–584.
Shields AE, Burke W, Levy DE . Differential use of available genetic tests among primary care physicians in the United States: results of a national survey. Genet Med 2008; 10: 404–414.
Cunningham GC . The genetics revolution. Postgrad Med 2000; 108: 193–202.
Thompson B . Foundations of behavioral statistics: an insight-based approach. New York: The Guilford Press, 2003.
Tabachnick BG, Fidell LS . Using multivariate statistics, 4th ed. Boston: Allyn & Bacon, 2001.
Kinney AY, Croyle RT, Dudley WN, Bailey CA, Pelias MK, Neuhausen SL . Knowledge, attitudes, and interest in breast-ovarian cancer gene testing: a survey of a large African-American kindred with a BRCA1 mutation. Prev Med 2001; 33: 543–551.
Bao Y, Fox SA, Escarce JJ . Socioeconomic and racial/ethnic differences in the discussion of cancer screening: “between-” versus “within-” physician differences. Health Serv Res 2007; 42: 950–970.
Eiser AR, Ellis G . Cultural competence and the African American experience with health care: the case for specific content in cross-cultural education. Acad Med 2007; 82: 176–183.
Zimmerman RK, Tabbarah M, Nowalk MP, et al. Racial differences in beliefs about genetic screening among patients at inner-city neighborhood health centers. J Natl Med Assoc 2006; 98: 370–377.
Browner CH, Preloran HM, Casado MC, Bass HN, Walker AP . Genetic counseling gone awry: miscommunication between prenatal genetic service providers and Mexican-origin clients. Soc Sci Med 2003; 56: 1933–1946.
Hughes C, Fasaye GA, LaSalle VH, Finch C . Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns 2003; 51: 107–114.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.geneticsinmedicine.org).
Rights and permissions
About this article
Cite this article
Suther, S., Kiros, GE. Barriers to the use of genetic testing: A study of racial and ethnic disparities. Genet Med 11, 655–662 (2009). https://doi.org/10.1097/GIM.0b013e3181ab22aa
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181ab22aa
Keywords
This article is cited by
-
The post-diagnostics world: charting a path for pediatric genomic medicine in the twenty-first century
Pediatric Research (2023)
-
Role of genomic medicine and implementing equitable access for critically ill infants in neonatal intensive care units
Journal of Perinatology (2023)
-
Communicating risk and the landscape of cancer prevention — an exploratory study that examines perceptions of cancer-related genetic counseling and testing among African Americans and Latinos in the Midwest
Journal of Community Genetics (2023)
-
Racial and ethnic disparities in genetic testing for hearing loss: a systematic review and synthesis
Human Genetics (2022)
-
Comprehension of skin cancer genetic risk feedback in primary care patients
Journal of Community Genetics (2022)