Abstract
Purpose: Fragile X syndrome is the most common form of hereditary intellectual disability. Detection of the fragile X phenotype in the prepubertal period is very difficult, and early detection might assist in early developmental intervention and reproductive counseling. A pilot study was conducted to establish the feasibility of newborn screening for fragile X syndrome.
Methods: A prospective study was done contacting mothers postdelivery in two hospitals in upstate South Carolina from 2005 to 2006. With their permission, blood samples were obtained from the male infants via heelstick and analyzed.
Results: A total of 1,459 newborns were tested, and 5 abnormal results were obtained. The results included one sex chromosome aneuploidy (47, XXY), two premutations, and two full mutations.
Conclusions: Our study establishes the potential feasibility of such a screening process. However, more complete studies assessing a larger population and risk-benefit analyses are necessary before any universal application of this test. Our detection rate for fragile X syndrome (1:730) was inexplicably greater than anticipated but likely represents a chance occurrence among the small number of infants tested.
Similar content being viewed by others
Main
In 1969, Lubs reported a family with four mentally retarded males who had an unusual constriction, or marker, on their X chromosome, and the clinical significance was confirmed in 1977.1,2 In 1991, it was discovered that the “constriction” was caused by an expanded trinucleotide repeat in affected males.3–6 Molecular testing most commonly shows affected individuals have a full mutation in the FMR1 gene of >200 trinucleotide repeats. An individual with a premutation has between 55 and 200 repeats. A premutation can expand to a full mutation when transmitted from generation to generation through females. Repeats sizes of <55 do not tend to expand to premutations or full mutations.7
Fragile X is the most common form of hereditary mental retardation. A Canadian study of over 10,000 women found a premutation prevalence of 1/259.8 Expansions of these premutations, which can occur on average 24% of the time,9 or transmission of full mutations lead to a fragile X population frequency of 1/3700 in Caucasian males and 1/2500 in African American males, based on a study performed in Atlanta, GA.10
Males affected with fragile X syndrome have moderate mental retardation, macroorchidism, and features including large ears, a prominent jaw, and a long face. Females with full mutations can have developmental disabilities or mild mental retardation. Premutations may place males and females at risk for late-onset cerebellar ataxia (Fragile X-associated tremor/ataxia syndrome [FXTAS]) and females at risk for early cessation of menses (premature ovarian failure [POF]). Fragile X syndrome was originally considered an unique disorder due to the change in the FMR1 gene but should now be considered a part of the family of FMR1 disorders, along with FXTAS and POF.7
Detection of the fragile X phenotype in the prepubertal period is very difficult. Various studies have shown that 50% of families with fragile X males have their second child before the diagnosis is established in the first child (the median age at diagnosis is 32 months).11–14 These authors also found that 24% of families visited a health care provider more than 10 times before fragile X testing was performed. The affected families noted that an early diagnosis would have affected their decisions about reproduction. After diagnosis, 73% reported that the diagnosis affected their decision to have another child. Forty-three percent of these families surveyed had a second child with fragile X. Early detection in the newborn period could allow for appropriate developmental intervention and reproductive counseling for the immediate and extended family.15
This pilot study was conducted to establish the feasibility of newborn screening for fragile X syndrome. We demonstrated such a project could be done but that considerable work is necessary before full-scale population-wide neonatal screening for fragile X syndrome can be undertaken. We also found a higher than anticipated incidence of fragile X syndrome among the small number of infants tested.
MATERIALS AND METHODS
Institutional review board approval was sought and obtained for the study from two hospitals in upstate South Carolina. On the basis of the availability of the project nurses, mothers were contacted postdelivery at the hospital by a project nurse. They were given printed information on fragile X and offered testing on a voluntary and research basis. If they agreed to join the study, they were asked to sign an institutional review board-approved consent enrolling their infant in the study.
Initially, this project aimed to identify a method capable of determining FMR1 CGG repeat status in both males and females. Two methods of quantitative polymerase chain reaction (PCR) analysis (Amplisensor and Abbott fluorescent PCR with internal control to measure relative range) used in the in-house validation process to determine the FMR1 repeat number in females failed to produce reliable and reproducible results, so the testing was limited to males for this initial pilot project.
Blood samples
Blood specimens were obtained via heel stick at the time of standard newborn metabolic screening and placed on a separate piece of Guthrie filter paper early in the project. Thereafter, samples were obtained from filter paper punches provided by the state laboratory (South Carolina Department of Health and Environmental Control Newborn Screening Laboratory) in charge of newborn screening for South Carolina. Cord blood samples were temporarily stored for enrolled patients, when possible. The flowchart shown in Figure 1 depicts the sequence of events in the analysis of the samples.
DNA isolation
Guthrie filter paper cards were punched with a BSD600 instrument (BSD Robotics, Australia) to obtain three spots for DNA isolation purposes using a standard procedure for the instrument. Punches from each individual enrolled in the study were collected in tubes rather than a 96-well plate to minimize possible contamination. DNA from these punches was extracted with a standard isolation protocol using a QiaAmp isolation kit (Qiagen, Valencia, CA). BSD robotics ensures that their technology has been thoroughly evaluated for potential contamination and sample carry-over issues. We performed internal assessments by routinely collecting spots from blank Guthrie cards and demonstrating lack of contamination for samples processed in identical fashion.
Polymerase chain reaction protocol/fragment analysis
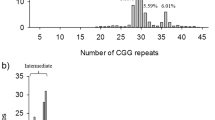
A PCR protocol based on conditions originally reported by Fu et al.16 for amplifying the FMR1 trinucleotide repeat was used with primers from Houdayer et al.17 to minimize the size of the amplicon generated. Briefly, DNA isolated from the blood spot punches was used as template and PCR was performed with the reverse primer fluorescently labeled. The PCR included dimethyl sulfoxide and betaine to assist in amplifying the GC-rich product. Amplicons were sized and analyzed on an ABI3100 with GeneScan software (Applied Biosystems, Foster City, CA). Most amplicons ranged between 116 bp (20 CGG repeats) and 176 bp (40 CGG repeats). To determine the CGG repeat size, the following calculation was used ([fragment size − 56]/3 = repeat number). It should be noted that DNA concentration was not routinely analyzed given the reproducibility of the assay to generate results from the original isolation. Only in the rare cases of PCR failure were samples quantified and quality assessed.
Follow-up testing
A more detailed analysis was pursued after a failed attempt to amplify the FMR1 trinucleotide repeat. This initially included quantitation of the DNA specimen to determine that the concentration was >10 ng/μL. If the concentration was below this threshold the isolation procedure was repeated. If the concentration was above the accepted threshold the amplification procedure was repeated. A second failure from either the first or secondary isolation was highly suggestive of an abnormal FMR1 CGG repeat size. To confirm this assumption, stored cord blood was requested and DNA was isolated using a standard automated protocol on an Autopure instrument (Gentra, Minneapolis, MN). The same PCR protocol used in the initial attempts was repeated on the DNA isolated from the cord blood. If PCR on the cord blood specimen failed, Southern blot analysis using our standard diagnostic protocol was performed.
For samples sized at >55 CGG repeats, the cord blood sample was also requested. DNA isolation, PCR, and Southern blot analysis were performed as previously outlined to confirm the presence of a premutation allele.
Reporting results
Final results (normal and abnormal) were reported to the project nurse, the family, and their primary doctor. Genetic evaluations and counseling were provided for the patients and families with abnormal results by the authors (RAS, RES, and GAS). Analyses comparing the observed and expected proportions of fragile X males were calculated using a one-sample z-test in Microsoft Excel (Redmond, OR).
RESULTS
From early 2005 to late 2006, a total of 1459 newborn males were studied after appropriate consent procedures—1286 from one hospital and 173 from another. This is 22% of the potential pool of newborn males during the time of the study (n = 6562). Of the 1844 mothers contacted in the newborn nursery for permission to enroll in the study, 79% elected to participate. Three hundred eighty-five mothers declined participation and their reasons were not ascertained.
Five abnormal results were obtained during the course of the study—one sex chromosome aneuploidy (47, XXY), two premutations, and two full mutations. The abnormal detection rate for these five results was 0.3% (5/1459). Racial data were not collected during this study, but it should be noted that all the positive results occurred in Caucasian families. Using a one-sample z-test, there is a significant difference (P value = 0.02) between the observed proportion of fragile X males (1/730) and the expected proportion (1/3300), given that South Carolina births in 2005 occurred in about twice as many Caucasians as African Americans.
The two premutations were 59 repeats and 68 repeats, respectively. The mother of the infant with 59 repeats had allele sizes of 20 and 57 repeats. The mother of the infant with 68 repeats had allele sizes of 19 and 64 repeats. After genetic counseling, both families were found to have unremarkable family histories.
The two full mutations were 600 and 800 repeats. The partial pedigree for the infant (IV-1) with 600 repeats is shown in Figure 2. His mother (III-3) had allele sizes of 32 and 85 repeats. His maternal grandfather (II-5) had an allele of 90 repeats and was an apparently unaffected carrier male. The brother of the maternal grandfather (II-1) was said to have autism and alcoholism and died at age 35. The sister of the maternal grandfather (II-2) suffered from infertility, reportedly secondary to endometriosis. This latter individual was not studied even though counseling and testing was offered through the family.
Partial pedigree for one infant detected by neonatal testing for fragile X. The infant (IV-1) had 600 repeats, his mother (III-3) had 85 and 32 repeats and the maternal grandfather (II-5) had 90 repeats. No additional history is available for the maternal great uncle (II-1) with “autism” and alcoholism or for the maternal great aunt (II-2) with severe “endometriosis” and infertility.
The partial pedigree for the infant (IV-2) with 800 repeats is shown in Figure 3. His mother (III-2) had allele sizes of 23 and 150 repeats. The maternal grandmother (II-2) had allele sizes of 30 and 77 repeats. Both the mother, maternal grandmother, and a distant relative (III-14) had “early” menopause by report. There was a distant male relative (III-15) with severe learning disability.
Partial pedigree for second infant detected by neonatal testing for fragile X. The infant (IV-2) had 800 repeats, his mother (III-2) had 150 and 23 repeats, and maternal grandmother (II-2) had 77 and 30 repeats. No additional history is available about “early menopause” in the mother (III-2), grandmother (II-2) and distant relative (III-14) or for the distant relative (III-15) with “severe” learning disability.
DISCUSSION
This study was designed as an initial pilot project to ascertain the feasibility of neonatal detection of fragile X syndrome. The strengths of the study include no selection bias (voluntary enrollment) and a prospective study over 2 years. The project advisory board had diverse interests (newborn screening officials, agency representatives, professional organizations, support groups, health professionals, parents) and had significant input during the project planning stages.
Numerous technical issues were successfully addressed during the course of this study including the feasibility of using filter paper spots provided by the state laboratory for screening purposes. The initial intent of the project was to identify a method capable of determining FMR1 CGG repeat status in both males and females. The testing was limited to males for this initial pilot project since the two methods used in the in-house validation process to determine the FMR1 repeat number in females failed to produce reliable and reproducible results.
As newborn screening for genetic disorders expands, a controversy exists whether screening should include conditions without a clear-cut mode of intervention. Until such time as specific therapies exist for fragile X syndrome, we are left with early diagnosis, access to developmental intervention and reproductive counseling as tangible benefits for neonatal detection of fragile X syndrome. Our experience with local fragile X support groups tells us that those benefits alone justify neonatal detection, but others have expressed significant concerns about the possible stigmatization of infants and their families.18
Neonatal detection allows for early diagnosis since phenotypic detection of fragile X syndrome in the prepubertal period is problematic. The median age of diagnosis tends to be between 2 and 3 years of age, and some families will have a second affected child before the first child is diagnosed.11–14 These families report that early detection would affect their decisions about reproduction. Early detection would avoid the long time to diagnosis and avoid the cost of other diagnostic tests. In addition, early detection in the newborn period could allow for appropriate developmental intervention. Detection will become increasingly important when specific therapeutic interventions become available.19–21 Counseling for potential adult complications in premutation carriers, such as POF and FXTAS, could also be offered to other family members.7
In an attempt to examine women's attitudes toward neonatal fragile X testing, Anido et al.22 interviewed women of children with and without fragile X syndrome in their families.22 The focus group analyses revealed that mothers of children with fragile X each have unique experiences that do not generalize to the group as a whole. These experiences affect their perception of the need for population-wide screening and suggest that individuals do not necessarily speak for the group as a whole. It was also noted that women's responses varied with respect to their life stage. The authors emphasized that formal population-wide education programs about FMR1-related disorders (fragile X syndrome, FXTAS, and POF) would be necessary before any population screening program should begin.
Screening for fragile X syndrome in the newborn period will potentially detect not just fragile X syndrome but other sex chromosome aneuploidies. Furthermore, this screening may determine whether the infant or family members are at risk for other FMR1-related disorders (FXTAS and POF). Newborn detection programs will need to consider the ramifications of this added requirement of appropriate informed consent in addition to the ethical issues involved. This type of screening program might detect asymptomatic conditions in the newborn period that can have significant consequences later in life in the individual tested or for other individuals in the family after genetic counseling.23–25 Similar concerns have been raised for other situations (such as hemochromatosis24 or Huntington disease25) where screening might have adverse consequences. By and large, testing is discouraged if there exists no clear and present benefit to the individual being tested. Newborn screening for FMR1-related disorders incurs the additional “burden” of potential detection of unanticipated conditions in immediate and/or more distant relatives. The detection of sex chromosome aneuploidy by the indirect method of molecular signals from X-linked genes also raises the possibility of stigmatization without substantial benefit to the patient. Consideration of these issues require further study before population studies are undertaken.
If new technology proves effective, it may allow for newborn detection in both sexes.26 This type of methodology would use high-throughput processing to detect full mutations and premutations in both males and females. Our study exclusively tested newborn males.
Because fragile X syndrome is the most common form of inherited mental retardation and early phenotypic detection is very difficult, there has been discussion regarding the need for potential neonatal detection allowing for early developmental intervention and appropriate counseling.13,14,18 Although significant benefits to the early detection of fragile X syndrome are evident, population-wide screening requires a more thorough analysis of the issues regarding detection of other FMR1-related disorders and sex chromosome aneuploidy.18 We would recommend a more broad-based pilot project (5,000–10,000 male newborns) using high-throughput technology with extensive education efforts regarding informed consent and appropriate genetic counseling. Cost analyses and risk-benefit analyses are critical to understanding whether this testing is truly beneficial. Potential therapeutic interventions will alter these conclusions and should be considered accordingly.
CONCLUSION
Over the course of 2 years, a total of 1459 newborn males were studied after appropriate consent procedures at two hospitals in upstate South Carolina. Five of the newborn males had abnormal results—two with full mutations for fragile X, two with premutations for fragile X, and one with sex chromosome aneuploidy (47, XXY). Our preliminary results show a significantly higher incidence of fragile X syndrome (1:730) than reported previously in population studies (1:3300). We conclude that the potential risks and benefits of newborn screening for fragile X syndrome should be studied in a larger population before the universal application of this test.
References
Lubs HA Jr . A marker X chromosome. Am J Hum Genet 1969; 21: 231–244.
Sutherland GR . Fragile sites on human chromosomes: demonstration of their dependence on the type of tissue culture medium. Science 1977; 197: 265
Yu S, Pritchard M, Kremer E, et al. Fragile X genotype characterized by an unstable region of DNA. Science 1991; 252: 1179–1181.
Oberlé I, Rousseau F, Heitz D, et al. Instability of a 550-base pair DNA segment and abnormal methylation in fragile X syndrome. Science 1991; 252: 1097–1102.
Verkerk AJ, Pieretti M, Sutcliffe JS, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell 1991; 65: 905–914.
Kremer EJ, Pritchard M, Lynch M, et al. Mapping of DNA instability at the fragile X to a trinucleotide repeat sequence p(CCG)n. Science 1991; 252: 1711–1714.
Saul RA, Tarleton JC . (updated December 2007) FMR1-Related Disorders in: Gene-Reviews at GeneTests: Medical Genetics Information Resource [database online]. Copyright, University of Washington, Seattle. 1997–2007. Available at: http://www.genetests.org. Accessed January 20, 2008.
Rousseau F, Rouillard P, Morel M-L, Khandjian EW, Morgan K . Prevalence of carriers of premutation-size alleles of the FMR1 gene and implications for the population genetics of the fragile X syndrome. Am J Hum Genet 1995; 57: 1006–1018.
Nolin SL, Brown WT, Glicksman A, et al. Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am J Hum Genet 2003; 72: 454–464.
Crawford DC, Meadows KL, Newman JL, et al. Prevalence of the fragile X syndrome in African-Americans. Am J Med Genet 2002; 110: 226–233.
Centers for Disease Control and Prevention Delayed diagnosis of fragile X syndrome—United States, 1990–1999. MMWR Morb Mortal Wkly Rep 2002; 51: 740–742.
Bailey DB Jr, Skinner D, Sparkman KL . Discovering fragile X syndrome: family experiences and perceptions. Pediatrics 2003; 111: 407–416.
Skinner D, Sparkman KL, Bailey DB Jr Screening for Fragile X Syndrome: parent attitudes and perspectives. Genet Med 2003; 5: 378–384.
Bailey DB, Jr. Newborn screening for fragile X syndrome. Ment Retard Dev Disabil Res Rev 2004; 10: 3–10.
Warren ST, Sherman SL . In: Scriver CR, Beaudet AL, Sly WS, Valle D, Vogelstein B, editors. The metabolic and molecular bases of inherited disease (OMMBID), Chapter 64. New York: McGraw-Hill. Available at: www.ommbid.com. Accessed December 19, 2007.
Fu YH, Kuhl DP, Pizzuti A, et al. Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell 1991; 67: 1047–1058.
Houdayer C, Lourdaux J, Billette de Villemeur T, et al. Simple fluorescent PCR assay for discriminating FRAXA fully mutated females from normal homozygotes. Genet Test 2002; 6: 135–139.
Bailey DB, Jr, Skinner D, Davis AM, Whitmarsh I, Powell C . Ethical, legal, and social concerns about expanded newborn screening: fragile X syndrome as a prototype for emerging issues. Pediatrics 2008; 121: e693–e704.
Nakamoto M, Nalavadi V, Epstein MP, Narayanan U, Bassell GJ, Warren ST . Fragile X mental retardation protein deficiency leads to excessive mGluR5-dependent internalization of AMPA receptors. Proc Natl Acad Sci U S A 2007; 104: 15537–15542.
Bear MF, Huber KM, Warren ST . The mGluR theory of fragile X mental retardation. Trends Neurosci 2004; 27: 370–377.
Dolen G, Bear MF . Role for metabotropic glumatate receptor 5 (mGluR5) in the pathogenesis of fragile X syndrome. J Physiol 2008; 586: 1503–1508.
Anido A, Carlson LM, Taft L, Sherman SL . Women's attitudes toward testing for fragile X carrier status: a qualitative analysis. J Genet Couns 2005; 14: 295–306.
Schmitt B, Golub RM, Green R . Screening primary care patients for hereditary hemochromatosis with transferrin saturation and serum ferritin level: systematic review for the American College of Physicians. Ann Intern Med 2005; 143: 522–536.
Qaseem A, Aronson M, Fitterman N, et al. Screening for hereditary hemochromatosis: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2005; 143: 517–521.
Robins Wahlin TB . To know or not to know: a review of behaviour and suicidal ideation in preclinical Huntington's disease. Patient Educ Couns 2007; 65: 279–287.
Strom CM, Crossley B, Redman JB, et al. Molecular testing for Fragile X Syndrome: lessons learned from 119,232 tests performed in a clinical laboratory. Genet Med 2007; 9: 46–51.
Acknowledgements
This study was completed through funding by the Maternal and Child Health Bureau of the Health Resources and Services Administration (Grant number 6H46MC00278) and institutional funding from the Greenwood Genetic Center.
We are grateful to our Advisory Board members, which included: Don Bailey (Frank Porter Graham Child Development Center), Robert Best (USC School of Medicine), Mary Beth Busby (parent), Katherine Clapp (FRAXA Research Foundation), Scott Grosse (Centers for Disease Control and Prevention), Thomas Hickey (SC Department of Health and Environmental Control), Robert Meyer (NC Birth Defects Monitoring Program), Robert Miller (National Fragile X Foundation), Cynthia Moore (Centers for Disease Control and Prevention), Susan Panny (MD Department of Health and Mental Hygiene), Carmen Quintero (SC Department of Health and Environmental Control), Paul Shewmaker (parent), and Jack Tarleton (Fullerton Genetics Center).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saul, R., Friez, M., Eaves, K. et al. Fragile X syndrome detection in newborns—pilot study. Genet Med 10, 714–719 (2008). https://doi.org/10.1097/GIM.0b013e3181862a76
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181862a76