Abstract
Several human leukocyte antigen (HLA) class I alleles are associated with the susceptibility to human immunodeficiency virus-1 (HIV-1) infection and/or AIDS progression. Of these, the HLA-B alleles are considered the strongest genetic determinant of disease outcome. We evaluated the influence of the HLA-B alleles on AIDS progression among HIV-1-positive individuals from Rio de Janeiro, Brazil, who were categorized as rapid progressors (RPs), typical progressors (TPs) or long-term non-progressors (LTNPs). In this study, significant differences in HLA-B allele frequencies were observed among the three progression groups for the B*48, B*49 and B*52 alleles. After controlling for other factors associated with AIDS progression, the presence of the B*52 allele was shown to be a significant protective factor (hazard ratio (HR) 0.49 (95% confidence interval (CI) 0.27–0.90) P<0.03). Although no direct association was observed between the presence of the B*27 or B*57 allele and the LTNP profile compared with the TP or RP groups, the adjusted model confirmed that these alleles are protective factors against AIDS progression (HR 0.62 (95% CI 0.38–0.99) P<0.05), as previously described. These data corroborate the existence of significant differences in HLA-B allele frequencies among the distinct AIDS progression profiles and further elucidate the role of HLA alleles in the outcome of HIV infections in diverse populations.
Similar content being viewed by others
Introduction
The natural clinical course of human immunodeficiency virus-1 (HIV-1) infection is extremely variable, ranging from the development of AIDS in less than a year to no evidence of progression in >10 years.1 The majority of HIV-infected individuals (70–80%) present with a typical course of infection that progresses to disease within 10 years. Approximately 10–15% of HIV-1-infected individuals progress to AIDS within 3 years of seroconversion, and these individuals are known as rapid progressors (RPs). A smaller proportion of individuals (5–10%) remains asymptomatic and presents CD4+ T-cell counts >500 cells mm−3 for >10 years; these patients are termed long-term non-progressors (LTNPs). To help explain the high variability among AIDS progression profiles, several studies have examined the roles of viral factors,2, 3, 4, 5, 6 the innate and adaptive immune responses7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 and host genetic factors20, 21, 22, 23, 24, 25, 26 in disease progression.
Host genetic variation is presently estimated to account for about one-fourth of the observed variation in HIV control.27 Among the genetic factors involved in the immune response to HIV, the human leukocyte antigens (HLAs) exert the strongest influence on viral control, immune escape and disease progression.28, 29, 30, 31 Several HLA class I alleles are associated with the susceptibility to HIV-1 infection and/or AIDS progression. The HLA-B alleles in particular impose substantially greater selection pressure on HIV-1 and are considered the strongest genetic determinant of disease outcome.21, 32, 33 Some associations are well characterized; for example, the impact of HLA-B*27 and B*57 alleles in slower progression to AIDS and long-term control of HIV-1 replication,24, 34, 35, 36, 37, 38 whereas the B*35 and B*53 alleles lead to faster progression.33, 39, 40
Based on this background, this study aimed to evaluate the impact of host genetics on AIDS progression based on the distribution of HLA-B class I alleles among HIV-1-infected individuals classified as RPs, typical progressors (TPs) or LTNPs.
Results
Clinical epidemiological characteristics
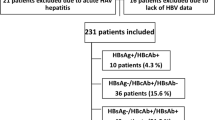
Of the 3809 HIV-1-seropositive individuals included in this cohort, 496 fulfilled the criteria for the disease progression classification (see Materials and methods section) and were categorized as 182 RPs (36.7%); 289 TPs (58.3%) and 25 LTNPs (5.0%). From this group, a subset of 218 individuals (86 RPs, 39.4%; 115 TPs, 52.8% and 17 LTNPs, 7.8%) had their HLA-B alleles genotyped.
In order to check the representativeness of this subset of 218 individuals, we compared the sociodemographic data of the 3313 unclassified individuals with data from individuals who had their HLA-B alleles genotyped (n=218) and those whose alleles could not be determined (n=278; Table 1). No difference regarding ethnicity, which could have influence on the HLA-B allele distribution, was observed from these comparisons, indicating that the subgroup of 218 individuals matches the 3313 group in this aspect. Similar results were observed when the sociodemographic data were compared considering the different groups of AIDS progression (Supplementary Table S1, Supplementary Material).
HLA-B alleles
Of the 218 HIV-positive individuals genotyped for their HLA-B alleles, roughly 29 HLA-B allelic groups were identified. The most frequent HLA-B alleles were B*15, B*35, B*44 and B*14 at 11.2%, 11.0%, 9.9% and 7.1% prevalence, respectively. These four common alleles accounted for 39.2% of the overall HLA-B allele frequency. Another 12 alleles presented moderate frequencies ranging from 2 to 7% and accounted for 48.3% of the overall allele frequency. The remaining 12 alleles had frequencies <2% and accounted for 12.5% of the overall allele frequency. Overall, deviation from Hardy–Weinberg equilibrium was not observed in the distribution of HLA-B genotypes in this population (P>0.05).
Given the miscegenation of the Brazilian population, we first analyzed the difference in frequencies of each HLA-B allele between Caucasian and non-Caucasian (Mulattoes and Black) individuals (Supplementary Table S2, Supplementary Material). Except for HLA-B*42 (0.4% vs 3.8%, respectively, P<0.02), no statistically significant differences were evident. Therefore, the following analysis of the HLA-B allele frequencies across the three AIDS progression groups were performed without accounting for the ethnic background of the individuals studied (Table 2). In our study, the frequency of the B*49 allele was higher in the TP group (4.0%) than in the RP group (0.6%, P<0.05, odds ratio (OR)=0.14). On the other hand, the frequency of the B*48 allele was higher in the LTNP group (5.9%) compared with the RP group (0%, P<0.03, OR=0.00). Notably, the B*52 allele frequency was higher in the LTNP group (11.8%) than in either the RP group (2.9%, P<0.05, OR=0.22) or the TP group (2.6%, P<0.05, OR=0.27; Table 2). The HIV-1-positive individuals in our study had quite diverse HLA-B genotypes, resulting from the combination of the four more common alleles cited above: B*15, B*35, B*44 and B*14. Each one of genotypes B*15:B*44 and B*14:B*15 were found in five individuals; followed by B*35:B*44 and B*14:B*44, with four occurrences each one and B*14:B*35, presented by three individuals. Only 13 individuals (6.0%) presented with a homozygous genotype (data not shown).
The comparison of the three HLA-B alleles significantly associated to disease progression profiles (Table 2) with their respective frequencies reported for the Brazilian general population (REDOME data set) is presented in Table 3. From this analysis, no statistically significant difference was verified in the overall comparison or stratified by ethnicity (white, black and mulattoes) showing that our studied population matched the HLA-B allelic distribution of the Brazilian population.
Survival analysis
In general, the median time between the diagnosis of HIV-1 infection and AIDS development for the 218 evaluated patients was 1816 days (95% confidence interval (CI): 1624–2004 days). The sociodemographic variables identified as having significant differences in the time to AIDS progression were gender (P<0.02), age at date of positive serology (P<0.05) and exposure category (P<0.02). The time until progression to AIDS was significantly different for the clinical variables presence of the B*48 allele (P<0.05, median 4470 vs 1792 days) and presence of the B*52 allele (P<0.02, median 2618 vs 1775 days), indicating a possible association of these factors with non-progression to AIDS (Figures 1a and b).
In the multivariate analysis, in addition to the variables significantly associated with the risk of progression to AIDS, described above, we also evaluated the variables schooling, presence of the rapid progression allele (B*35) and presence of the slow progression allele (B*27/B*57; Table 4). From this analysis, the variables independently associated with AIDS progression were gender, age at date of positive serology, presence of the slow progression allele (B*27/B*57) and presence of the allele B*52. Although the variable presence of the B*48 allele was not significantly associated with AIDS progression (P<0.08) in the multivariate model, this variable was included in the analysis because it added explanatory power. Controlling for these factors, the risk of developing AIDS was significantly higher among the male patients (hazard ratio (HR) 1.45 (95% CI 1.06–1.97) P<0.03) who were diagnosed with HIV-1 at a later age (HR 1.02 (95% CI 1.00–1.03) P<0.04). Although no direct association was observed between the B*27 or B*57 alleles and the LTNP profile (Table 2), in the adjusted model these alleles were confirmed as protective factors against AIDS progression (HR 0.62 (95% CI 0.38–0.99) P<0.05). The B*52 allele was found to be a protective factor against AIDS in both the bivariate (HR 0.49 (95% CI 0.27–0.90) P<0.03) and multivariate models (HR 0.48 (95% CI 0.26–0.89) P<0.03).
When selecting the variables to be evaluated in the multivariate model, the variable presence of the rapid progression allele (B*35) was included although the P-value (0.26) was >0.20 in the bivariate analysis. However, no association between this allele and the time to AIDS progression was found using the multivariate model (Table 4). By contrast, the variable exposure category, which was considered significant using the bivariate model, was not evaluated in the adjusted model because it would exclude 12 patients, including 2 from the LTNP group. The final model fit the data properly and was in accordance with the assumptions of Cox model.
Discussion
Host genetic factors have been consistently linked to variations in both susceptibility and resistance to HIV-1 infection and disease progression.1, 41, 42, 43 In a previous study, we tried to assess the possible association of CCR5 genotypes and HLA-B alleles with the susceptibility or resistance to HIV-1 infection in injecting drug users from Rio de Janeiro, Brazil, but no association was evident.44 Here we focused on AIDS progression, evaluating the influence of the HLA-B alleles on disease outcome.
The classification of HIV-1-positive individuals based on their AIDS progression profile is not consistent across the studies, mainly because of the different clinical criteria used to distinguish the RP, TP and LTNP groups. Here we defined these three groups of AIDS progressors based on the time from the estimated date of infection to the occurrence of the first AIDS-defining event. AIDS-defining events included a CD4+ T-lymphocyte count below 350 cells mm−3, AIDS-defining illness, the initiation of antiretroviral therapy or AIDS-related death. The need to apply a standardized and accepted set of clinical definitions for the purpose of disease stratification has already been emphasized.45 As a result of the strict inclusion criteria adopted in this study to classify the HIV-positive patients across the three AIDS progression profiles, a high proportion of the individuals included in our databank could not be classified. The major obstacle to classification was the late HIV diagnosis, which is common in our country, as in many other regions.46, 47, 48, 49 This factor impeded the classification of a large number of individuals with a potential TP profile. Similarly, the lack of information about the last negative HIV serology limited the classification of possible RPs in our databank.
The HLA class I locus has been characterized as the main factor influencing the outcome of HIV infection.21, 27 This study presents the first evidence of a significant association between HLA-B*52 and slower progression to AIDS. This observation contradicts a previous study in which this allele was not associated with either slower or faster AIDS progression.50 The association of the B52 antigen with resistance to HIV was first described in 1992 by Fabio et al.,51 but since then there has been no other study corroborating this finding. Recently, HLA-B*52 was linked to a strong effect on viral load during early time points but had no significant effect on the long-term control of HIV-1.38 This allele has also been described as a protective factor for pulmonary tuberculosis.52
We also detected other HLA-B alleles associated with slower progression or non-progression to AIDS that were less striking than that observed for the B*52 allele. In fact, a possible association between the B*48 allele and non-progression to AIDS was initially observed in this study but was not confirmed by the multivariate model results. For the HLA-B*27 and B*57 alleles, we did not find a direct association with non-progression to AIDS, but a correlation was observed based on the higher frequencies of these alleles in the LTNP group (Table 2) and the confirmation of the protective role of these alleles by the multivariate analysis (Table 4). Thus, we may have lacked the statistical power to detect this association because of the low number of individuals with an LTNP profile in our databank. The protective effect of these alleles on the different aspects of HIV-1 infection has been extensively documented in the literature,21, 24, 27, 36, 37, 50 including the potent antiviral immunity conferred by the B*27 and B*57 alleles through limiting central memory T-cell infection in LTNP individuals.53 On the other hand, the previously reported deleterious effect of the HLA-B*35 allele on disease progression33, 40 was not observed in this study despite the higher frequency of this allele in the RP group (13.4% vs 10.0% in the TP group vs 5.9% in the LTNP group). Unlike our findings for the B*27 and B*57 alleles, the multivariate analysis did not confirm the B*35 allele as a risk factor for AIDS in our study group.
Given the high genetic diversity of the Brazilian population, which is characterized by an elevated degree of miscegenation, it is important to compare the allelic frequencies between Caucasians and non-Caucasians. With the exception of the HLA-B*42 allele, which was overrepresented in non-Caucasian individuals (P<0.02), all other HLA-B alleles were equally distributed across different ethnicities within the study group. The predominance of HLA-B*42 in non-Caucasians is consistent with the literature54 and ethnicity information in the REDOME data set and in the Allele Frequency Net Database.55
In conclusion, despite the limitations in the classification of the HIV-1-positive individuals because of unavailable data, this study corroborates the importance of the HLA-B alleles in determining the outcome of HIV-1 infection. Here we have described for the first time the protective role of the B*52 allele in disease progression and confirmed the association of the B*27 and B*57 alleles with the LTNP profile. These results reinforce the hypothesis that HLA class I alleles are key determinants of the host immune response against HIV-1 infection and expand our knowledge of the distribution and effects of these alleles in the Brazilian population, where additional studies examining host genetic characterization in the context of infectious diseases are still needed.
Materials and methods
Study group
This retrospective study included HIV-1-seropositive individuals who were undergoing clinical follow-up at Evandro Chagas Clinical Research Institute (IPEC/FIOCRUZ), Rio de Janeiro, Brazil, from 1986 to 2011 (n=4015) and were registered in the IPEC database. The inclusion criteria for further classification according to the progression profiles were as follows: (1) the patient had been clinically followed up for at least 60 days, (2) HIV-1 infection was diagnosed before 2010 and (3) the patient was >13 years old. Clinical and laboratory data from a total of 3809 individuals that fulfilled these criteria were considered for the stratification of the HIV-1-infected individuals into the three clinical progression profiles: RP (AIDS progression within 3 years of seroconversion; ⩾1 CD4 T-cell measurement available; time between the negative serological test and the positive serological test <3 years), TP (AIDS progression >4 years after seroconversion; ⩾2 CD4 T-cell measurements >350 cells mm−3 before AIDS event) and LTNP (asymptomatic HIV-1 infection for >10 year after seroconversion; all CD4 T-cell measurements >500 cells mm−3). Biological material was available in the laboratory biorepository for 218 individuals. These samples were used for genetic characterization and subsequent statistical analyses.
For the RP group, the dates of the last seronegative test and the first seropositive test were used to calculate the estimated date of infection (defined as the midpoint of these two dates with a maximum interval of 36 months). For the other groups, when the date of the last seronegative test was not available, the estimated date of infection was calculated as 6 months before the date of the first seropositive test. Time to disease progression was defined as the time elapsed (in days, after conversion to years) between the estimated date of infection and the first AIDS-defining event. An AIDS-defining event included any one of the following: CD4+ T-lymphocyte count below 350 cells mm−3, AIDS-defining illness (according to the Brazilian Ministry of Health Guidelines),56 initiation of antiretroviral therapy or AIDS-related death.
Based on the criteria used to estimate the seroconversion date, we were not able to precisely classify individuals who progressed to AIDS within 3 to 4 years of infection because these individuals were in the threshold between the RP and TP groups after applying the estimated seroconversion criteria. The present work was approved by the FIOCRUZ Ethical Research Committee as an anonymous unlinked study (Ethics Committee CAE: 0002.0.009.000-08).
DNA extraction
DNA was extracted from whole blood using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. All DNA samples were stored at −20 °C until the genomic analyses.
HLA-B typing
The HLA-B typing was performed using a combination of two commercial kits: the INNO LiPA HLA-B Multiplex Plus kit and the INNO LiPA HLA-B Update Plus kit (INNOGENETICS, Ghent, Belgium). The first kit was used to PCR amplify a fragment between the second and fourth exons of the HLA-B locus according to the manufacturer’s protocol. After this step, the PCR products were submitted to a hybridization assay using the second kit, which is based on the line probe assay methodology. The identification of the HLA-B alleles was performed using the LiRAS interpretation software, LiPA HLA v6.00 (INNOGENETICS).
Statistical analyses
Sociodemographic characteristics of the subgroups of individuals were tested by the χ2 test, Fisher’s exact test or Mann–Whitney test (the most appropriated in each situation). The HLA-B allele frequencies and genotypes were estimated using the PyPop package.57 Deviations from Hardy–Weinberg equilibrium were calculated using the method of Guo and Thompson,58 which was also performed using PyPop. The frequencies of each HLA-B allele were compared (1) among the three clinical progression groups and (2) between HIV-1-positive individuals and the genomic profile from the Brazilian National Registry of Bone Marrow Donors (REDOME) released in March 2013, which represents a reliable and representative sample of the Brazilian population, with almost 3 million registered donors (www.imunogenetica.org). For all comparisons, a χ2 test or Fisher’s exact test was performed using the statistics program Epi Info Version 6.59
The Kaplan–Meier method and Cox proportional hazards models were used to evaluate the elapsed time from the first HIV-1-positive serology to the progression to AIDS for individuals who could be categorized into one of the three progression groups and for whom HLA-B data were available. Survival curves were described by the Kaplan–Meier estimator, and the categories of each analyzed variable were compared through a log-rank test. For the evaluation of the factors associated with AIDS progression, variables with a significant effect on the HR and an occurrence of the event <20% (based on the Wald test) were evaluated in the model. The models were compared using the likelihood ratio rest (analysis of variance). The assumptions of the Cox models and the quality of the adjustment were made, respectively, based on the residuals and coefficient of determination, as well as the likelihood of agreement, to evaluate the discriminatory power and predictive accuracy of the model. All tests were considered significant if the P-value was <0.05. R software version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria) with the Survival library was used to run these analyses.60
References
Sharma G, Kaur G, Mehra N . Genetic correlates influencing immunopathogenesis of HIV infection. Indian J Med Res 2011; 134: 749–768.
Alexander L, Weiskopf E, Greenough TC, Gaddis NC, Auerbach MR, Malim MH et al. Unusual polymorphisms in human immunodeficiency virus type 1 associated with nonprogressive infection. J Virol 2000; 74: 4361–4376.
Mariani R, Kirchhoff F, Greenough TC, Sullivan JL, Desrosiers RC, Skowronski J . High frequency of defective nef alleles in a long-term survivor with nonprogressive human immunodeficiency virus type 1 infection. J Virol 1996; 70: 7752–7764.
Michael NL, Chang G, d'Arcy LA, Ehrenberg PK, Mariani R, Busch MP et al. Defective accessory genes in a human immunodeficiency virus type 1-infected long-term survivor lacking recoverable virus. J Virol 1995; 69: 4228–4236.
Brumme ZL, Li C, Miura T, Sela J, Rosato PC, Brumme CJ et al. Reduced replication capacity of NL4-3 recombinant viruses encoding reverse transcriptase-integrase sequences from HIV-1 elite controllers. J Acquir Immune Defic Syndr 2011; 56: 100–108.
Deacon NJ, Tsykin A, Solomon A, Smith K, Ludford-Menting M, Hooker DJ et al. Genomic structure of an attenuated quasi species of HIV-1 from a blood transfusion donor and recipients. Science 1995; 270: 988–991.
Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, Abraham J et al. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 2006; 107: 4781–4789.
Ferre AL, Hunt PW, Critchfield JW, Young DH, Morris MM, Garcia JC et al. Mucosal immune responses to HIV-1 in elite controllers: a potential correlate of immune control. Blood 2009; 113: 3978–3989.
Migueles SA, Laborico AC, Shupert WL, Sabbaghian MS, Rabin R, Hallahan CW et al. HIV-specific CD8+ T cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nat Immunol 2002; 3: 1061–1068.
Migueles SA, Osborne CM, Royce C, Compton AA, Joshi RP, Weeks KA et al. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity 2008; 29: 1009–1021.
Ndhlovu ZM, Proudfoot J, Cesa K, Alvino DM, McMullen A, Vine S et al. Elite controllers with low to absent effector CD8+ T cell responses maintain highly functional, broadly directed central memory responses. J Virol 2012; 86: 6959–6969.
Saez-Cirion A, Lacabaratz C, Lambotte O, Versmisse P, Urrutia A, Boufassa F et al. HIV controllers exhibit potent CD8 T cell capacity to suppress HIV infection ex vivo and peculiar cytotoxic T lymphocyte activation phenotype. Proc Natl Acad Sci USA 2007; 104: 6776–6781.
Saez-Cirion A, Sinet M, Shin SY, Urrutia A, Versmisse P, Lacabaratz C et al. Heterogeneity in HIV suppression by CD8 T cells from HIV controllers: association with Gag-specific CD8 T cell responses. J Immunol 2009; 182: 7828–7837.
Chevalier MF, Julg B, Pyo A, Flanders M, Ranasinghe S, Soghoian DZ et al. HIV-1-specific interleukin-21+ CD4+ T cell responses contribute to durable viral control through the modulation of HIV-specific CD8+ T cell function. J Virol 2011; 85: 733–741.
Lambotte O, Ferrari G, Moog C, Yates NL, Liao HX, Parks RJ et al. Heterogeneous neutralizing antibody and antibody-dependent cell cytotoxicity responses in HIV-1 elite controllers. AIDS 2009; 23: 897–906.
Barblu L, Machmach K, Gras C, Delfraissy JF, Boufassa F, Leal M et al. Plasmacytoid dendritic cells (pDCs) from HIV controllers produce interferon-alpha and differentiate into functional killer pDCs under HIV activation. J Infect Dis 2012; 206: 790–801.
Machmach K, Leal M, Gras C, Viciana P, Genebat M, Franco E et al. Plasmacytoid dendritic cells reduce HIV production in elite controllers. J Virol 2012; 86: 4245–4252.
Saez-Cirion A, Hamimi C, Bergamaschi A, David A, Versmisse P, Melard A et al. Restriction of HIV-1 replication in macrophages and CD4+ T cells from HIV controllers. Blood 2011; 118: 955–964.
Vieillard V, Fausther-Bovendo H, Samri A, Debre P . Specific phenotypic and functional features of natural killer cells from HIV-infected long-term nonprogressors and HIV controllers. J Acquir Immune Defic Syndr 2010; 53: 564–573.
Pereyra F, Jia X, McLaren PJ, Telenti A, de Bakker PI, Walker BD et al. The major genetic determinants of HIV-1 control affect HLA class I peptide presentation. Science 2010; 330: 1551–1557.
Fellay J, Shianna KV, Ge D, Colombo S, Ledergerber B, Weale M et al. A whole-genome association study of major determinants for host control of HIV-1. Science 2007; 317: 944–947.
Bailey JR, Williams TM, Siliciano RF, Blankson JN . Maintenance of viral suppression in HIV-1-infected HLA-B*57+ elite suppressors despite CTL escape mutations. J Exp Med 2006; 203: 1357–1369.
Lambotte O, Boufassa F, Madec Y, Nguyen A, Goujard C, Meyer L et al. HIV controllers: a homogeneous group of HIV-1-infected patients with spontaneous control of viral replication. Clin Infect Dis 2005; 41: 1053–1056.
Migueles SA, Sabbaghian MS, Shupert WL, Bettinotti MP, Marincola FM, Martino L et al. HLA B*5701 is highly associated with restriction of virus replication in a subgroup of HIV-infected long term nonprogressors. Proc Natl Acad Sci USA 2000; 97: 2709–2714.
Dean M, Carrington M, Winkler C, Huttley GA, Smith MW, Allikmets R et al. Genetic restriction of HIV-1 infection and progression to AIDS by a deletion allele of the CKR5 structural gene. Hemophilia Growth and Development Study, Multicenter AIDS Cohort Study, Multicenter Hemophilia Cohort Study, San Francisco City Cohort, ALIVE Study. Science 1996; 273: 1856–1862.
Limou S, Le Clerc S, Coulonges C, Carpentier W, Dina C, Delaneau O et al. Genomewide association study of an AIDS-nonprogression cohort emphasizes the role played by HLA genes (ANRS Genomewide Association Study 02). J Infect Dis 2009; 199: 419–426.
Carrington M, Walker BD . Immunogenetics of spontaneous control of HIV. Annu Rev Med 2012; 63: 131–145.
Trachtenberg E, Korber B, Sollars C, Kepler TB, Hraber PT, Hayes E et al. Advantage of rare HLA supertype in HIV disease progression. Nat Med 2003; 9: 928–935.
O'Brien SJ, Nelson GW . Human genes that limit AIDS. Nat Genet 2004; 36: 565–574.
Altfeld M, Kalife ET, Qi Y, Streeck H, Lichterfeld M, Johnston MN et al. HLA Alleles Associated with Delayed Progression to AIDS Contribute Strongly to the Initial CD8(+) T Cell Response against HIV-1. PLoS Med 2006; 3: e403.
Huang X, Ling H, Mao W, Ding X, Zhou Q, Han M et al. Association of HLA-A, B, DRB1 alleles and haplotypes with HIV-1 infection in Chongqing, China. BMC Infect Dis 2009; 9: 201.
Kiepiela P, Leslie AJ, Honeyborne I, Ramduth D, Thobakgale C, Chetty S et al. Dominant influence of HLA-B in mediating the potential co-evolution of HIV and HLA. Nature 2004; 432: 769–775.
Gao X, O'Brien TR, Welzel TM, Marti D, Qi Y, Goedert JJ et al. HLA-B alleles associate consistently with HIV heterosexual transmission, viral load, and progression to AIDS, but not susceptibility to infection. AIDS 2010; 24: 1835–1840.
Kaslow RA, Carrington M, Apple R, Park L, Muñoz A, Saah AJ et al. Influence of combinations of human major histocompatibility complex genes on the course of HIV-1 infection. Nat Med 1996; 2: 405–411.
Hendel H, Caillat-Zucman S, Lebuanec H, Carrington M, O'Brien S, Andrieu JM et al. New class I and II HLA alleles strongly associated with opposite patterns of progression to AIDS. J Immunol 1999; 162: 6942–6946.
Altfeld M, Addo MM, Rosenberg ES, Hecht FM, Lee PK, Vogel M et al. Influence of HLA-B57 on clinical presentation and viral control during acute HIV-1 infection. AIDS 2003; 17: 2581–2591.
Catano G, Kulkarni H, He W, Marconi VC, Agan BK, Landrum M et al. HIV-1 disease-influencing effects associated with ZNRD1, HCP5 and HLA-C alleles are attributable mainly to either HLA-A10 or HLA-B*57 alleles. PLoS ONE 2008; 3: e3636.
Antoni G, Guergnon J, Meaudre C, Samri A, Boufassa F, Goujard C et al. MHC-driven HIV-1 control on the long run is not systematically determined at early times post-HIV-1 infection. AIDS 2013; 27: 1707–1716.
Klein MR, Keet IP, D'Amaro J, Bende RJ, Hekman A, Mesman B et al. Associations between HLA frequencies and pathogenic features of human immunodeficiency virus type 1 infection in seroconverters from the Amsterdam cohort of homosexual men. J Infect Dis 1994; 169: 1244–1249.
Gao X, Nelson GW, Karacki P, Martin MP, Phair J, Kaslow R et al. Effect of a single amino acid change in MHC class I molecules on the rate of progression to AIDS. N Engl J Med 2001; 344: 1668–1675.
Liu R, Paxton WA, Choe S, Ceradini D, Martin SR, Horuk R et al. Homozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infection. Cell 1996; 86: 367–377.
Samson M, Libert F, Doranz BJ, Rucker J, Liesnard C, Farber CM et al. Resistance to HIV-1 infection in caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor gene. Nature 1996; 382: 722–725.
Matthews PC, Listgarten J, Carlson JM, Payne R, Huang KH, Frater J et al. Co-operative additive effects between HLA alleles in control of HIV-1. PLoS ONE 2012; 7: e47799.
Teixeira SL, Bastos FI, Hacker MA, Morgado MG . Distribution of CCR5 genotypes and HLA Class I B alleles in HIV-1 infected and uninfected injecting drug users from Rio de Janeiro, Brazil. Infect Genet Evol 2009; 9: 638–642.
Casado C, Colombo S, Rauch A, Martínez R, Günthard HF, Garcia S et al. Host and viral genetic correlates of clinical definitions of HIV-1 disease progression. PLoS ONE 2010; 5: e11079.
Girardi E, Aloisi MS, Arici C, Pezzotti P, Serraino D, Balzano R et al. Delayed presentation and late testing for HIV: demographic and behavioral risk factors in a multicenter study in Italy. J Acquir Immune Defic Syndr 2004; 36: 951–959.
Grangeiro A, Escuder MM, Menezes PR, Alencar R, Ayres de Castilho E . Late entry into HIV care: estimated impact on AIDS mortality rates in Brazil, 2003-2006. PLoS ONE 2011; 6: e14585.
Kerr LRFS, Mota RS, Kendall C, Dourado I . HIV infection and late diagnosis among MSM in Brazil. In: XIX International AIDS Conference 2012. Washington DC, USA, 2012, (abstract MOPE280).
Ramos NA Jr, Matida LH, Alencar CH, Hearst N, Heukelbach J . Late-stage diagnosis of HIV infection in Brazilian children: evidence from two national cohort studies. Cadernos de Saúde Pública 2013; 29: 10.
Kaur G, Mehra N . Genetic determinants of HIV-1 infection and progression to AIDS: immune response genes. Tissue Antigens 2009; 74: 373–385.
Fabio G, Scorza R, Lazzarin A, Marchini M, Zarantonello M, D'Arminio A et al. HLA-associated susceptibility to HIV-1 infection. Clin Exp Immunol 1992; 87: 20–23.
Vijaya LV, Rakh SS, Anu RB, Hari SPV, Pantula V, Jasti S et al. Role of HLA-B51 and HLA-B52 in susceptibility to pulmonary tuberculosis. Infect Genet Evol 2006; 6: 436–439.
Descours B, Avettand-Fenoel V, Blanc C, Samri A, Mélard A, Supervie V et al. Immune responses driven by protective human leukocyte antigen alleles from long-term nonprogressors are associated with low HIV reservoir in central memory CD4 T cells. Clin Infect Dis 2012; 54: 1495–1503.
Paximadis M, Mathebula TY, Gentle NL, Vardas E, Colvin M, Gray CM et al. Human leukocyte antigen class I (A, B, C) and II (DRB1) diversity in the black and Caucasian South African population. Hum Immunol 2012; 73: 80–92.
Gonzalez-Galarza FF, Christmas S, Middleton D, Jones AR . Allele frequency net: a database and online repository for immune gene frequencies in worldwide populations. Nucleic Acids Res 2011; 39: D913–D919.
Brazilian Ministry of Health: Criteria for definition of AIDS cases in adults and children [Portuguese]. DST and AIDS National Program. Brasília, Brazil, 2004.
Lancaster A, Nelson MP, Meyer D, Thomson G, Single RM . PyPop: a software framework for population genomics: analyzing large-scale multi-locus genotype data. Pac Symp Biocomput 2003: 514–525. Available at: http://psb.stanford.edu/psb-online/proceedings/psb03/lancaster.pdf.
Guo SW, Thompson EA . Performing the exact test of Hardy-Weinberg proportion for multiple alleles. Biometrics 1992; 48: 361–372.
Dean AG, Dean JA, Coulombier D, Brendel KA, Smith DC, Burton AH et al. Epi Info Version 6: A Word Processing, Database, and Statistics Program for Epidemiology on Microcomputers 6 edn. Centers for Disease Control and Prevention: Atlanta, GA, USA, 1995.
Carvalho MS, Andreozzi VL, Codeço CT, Campos DP, Barbosa MTS, Shimakura SE . Análise de Sobrevivência: Teoria e Aplicações em Saúde 2a edn, vol. 1. Editora FIOCRUZ: Rio de Janeiro, Brasil, 2011.
Acknowledgements
This work was partially supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico—CNPq (grant number 305592/2010-6) and Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro—FAPERJ (grant number E26/110.517/2012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Genes and Immunity website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Teixeira, S., de Sá, N., Campos, D. et al. Association of the HLA-B*52 allele with non-progression to AIDS in Brazilian HIV-1-infected individuals. Genes Immun 15, 256–262 (2014). https://doi.org/10.1038/gene.2014.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gene.2014.14
This article is cited by
-
The immunogenetics of COVID-19
Immunogenetics (2023)
-
Clinical and genetic markers associated with tuberculosis, HIV-1 infection, and TB/HIV-immune reconstitution inflammatory syndrome outcomes
BMC Infectious Diseases (2020)
-
Next-generation sequencing analyses of the emergence and maintenance of mutations in CTL epitopes in HIV controllers with differential viremia control
Retrovirology (2018)
-
Host genotype and time dependent antigen presentation of viral peptides: predictions from theory
Scientific Reports (2017)