Abstract
Purpose
Although pediatric cataract surgery has become standardized and safe, further surgical interventions are not uncommon. The purpose of this study was to analyze the incidence of complications in children who required an intraocular intervention.
Methods
A retrospective review of medical records of children (<7 years) with cataract who underwent cataract surgery with or without primary posterior chamber intraocular lens (IOL) placement between January 2006 and December 2014 was carried out. Data were collected regarding visual axis opacification (VAO), glaucoma, IOL decentration, intraocular infections, and other indications that required a second intraocular surgery.
Results
Out of 814 (570 pseudophakic and 244 aphakic) eyes of 620 operated children, 45 eyes of 40 children (5.5%, 45/814) needed a second surgery. The most common indication being VAO (2.9%, 24/814), followed by glaucoma (0.73%, 6/814). Incidence of complications was higher in children <1 year (VAO 6.1%, 19/308 and glaucoma 6%, 6/308). Among all children, repeat interventions and VAO were slightly less frequent in pseudophakics (4.91%, 28/570) vs aphakics (6.91%, 17/244) (P=0.31). As VAO was more common in pseudophakic eyes in infants, glaucoma was equally common in both groups. Best-corrected visual acuity improved from 1.6±0.56 LogMAR preoperatively to 0.80±0.50 LogMAR postoperatively.
Conclusions
Our study suggests that overall incidence of second intraocular surgery is low after primary pediatric cataract surgery. VAO remains the most common indication followed by secondary glaucoma. Incidence of complications is higher in children <1 year of age at initial surgery.
Similar content being viewed by others
Introduction
Developments of new microsurgical techniques and amblyopia management have improved the safety and effectiveness of pediatric cataract treatment.1, 2 However, owing to the inherent nature of growing eyes, marked inflammatory responses in pediatric eyes and inherent risks involved in surgery, management of congenital cataract remains a challenge in terms of preventing and managing complications.3, 4 The most commonly reported complications after pediatric cataract surgery with or without an intraocular lens (IOL) implantation are visual axis opacification (VAO),5, 6 heightened inflammatory response,7 secondary membranes,7 IOL precipitates,8 pupillary capture,8 posterior synechiae,8 uveitis,9 iris prolapse, corectopia,10, 11 endothelial cell loss,12 pupillary block and aphakic/pseudophakic glaucoma,6, 13, 14 retinal detachment,15 and endophthalmitis.10, 16 Although some retrospective studies have reported prevalence of postoperative complications after pediatric cataract surgery, only a few studies have focused on complications that require intervention/reoperation.9, 10, 11 Wilson et al17 reported a 22% reoperation rate over a 3-year follow-up most commonly for pupillary membranes. Lambert et al18 reported a 72% reoperation rate for glaucoma, pupillary membranes, VAO, and corectopia. These studies however had a very small sample size with a short follow-up. In addition, most of these studies reported VAO and secondary glaucoma as the most common complications requiring intervention after pediatric cataract surgery.5, 8 There are only a few reports suggesting other complications needing surgical intervention,9, 10 and only a few studies that reported complications both in aphakia and pseudophakia.
The current study reports the incidence of all the complications following lens aspiration with and without IOL implantation in children <7 years that necessitated a second intraocular surgery over a 5-year follow-up.
Materials and methods
We conducted a retrospective chart review at our institute, after receiving institutional review board approval. A search of the pediatric cataract database and medical records of patients who underwent lens aspiration with/without primary IOL placement between January 2006 and December 2014 was performed. We reviewed records of all children aged <7 years who underwent lens aspiration with or without primary posterior capsulotomy, anterior vitrectomy, and primary posterior chamber IOL (LA±PPC±AV±PCIOL) implantation for congenital and developmental cataracts. We selected records of consecutive patients who underwent second intraocular procedure for complications (except secondary IOL implantation and strabismus surgery). Children with traumatic cataracts, complicated cataracts secondary to retinoblastoma, uveitis, and those who underwent extraocular surgery were excluded. All the selected patients underwent surgery using the standard surgical technique and postoperative medications were prescribed according to the regimen as described in the previous reports.19 Preoperatively, biometry was performed either by partial coherence interferometry (IOL master, Carl Zeiss Meditec, Dublin, CA, USA) or applanation technique under general anesthesia depending on the age and cooperation of the child. Intraocular pressure (IOP) was measured with a Perkins MK2 handheld applanation tonometer (Belrose Refracting Equipment Co. Inc., Skokie, IL, USA). Keratometry was performed using a Nidek KM 500 handheld autokeratometer (Nidek Inc., Fremont, CA, USA) and axial length was measured with contact A-scan with OcuScan RxP (Alcon Laboratories, Inc., Fort Worth, TX, USA) in cataract mode. Sanders–Retzlaff–Kraff II formula was used to calculate the IOL power. IOL power was chosen according to Enyedi’s rule of seven. The sutures were removed 4 weeks postoperatively. Retinoscopy readings after suture removal were taken into consideration for the purpose of analysis. A trained optometrist who was unaware of the amount of under correction performed the retinoscopy. Postoperative evaluation was carried out at intervals during examination under anesthesia or outpatient visits, depending on the age of the patient. The interval between surgeries in bilateral cases ranged from 1 to 4 weeks.
Data collection and analysis
Case records were analyzed and data were collected regarding the age at surgery, gender, cataract morphology, etiology, technique of biometry, and surgical technique. Postoperative data were used to look for the incidence of complications like corneal edema, increased postoperative inflammation, glaucoma, retinal detachment, secondary membrane formation, wound leak, strabismus, IOL decentration, and endophthalmitis, which if found, were duly noted.
VAO was defined as lens material regrowth extending across the pupil believed to be interfering with vision.
Glaucoma was defined as increase in the IOP (<22 mm Hg), with the presence of increased optic nerve cupping and/or myopic refractive shift.
IOL was recorded as decentered if the edge of the optic was seen in the pupillary area in undilated or dilated state.
Visual outcome was assessed by changes in best-corrected visual acuity (BCVA), which was measured with appropriate optical correction during each postoperative follow-up visit.
Outcome measures
-
1
Prevalence of all the complications that needed resurgery in eyes with or without IOLs.
-
2
Visual outcomes in the children with various indications for second surgery.
Statistical analysis
Statistical analysis was performed using the R-software 3.1.2 (R-foundation for statistical computing, Vienna, Austria). Shapiro–Wilk test was used to assess the normal distribution of the data.
Descriptive analysis was performed. In addition, univariate and multivariate analysis were carried out to study the effect of various factors such as age, type of IOL, and surgical technique (aphakia vs pseudophakia) on the incidence of the complications.
Results
During the period from 1 January 2006 to 31 December 2014, a total of 814 (570 pseudophakic with an IOL implantation and 244 aphakic) eyes of 620 children <7 years underwent cataract surgery.
Of these, 45 eyes of 40 patients (5 bilateral) needed a second surgical intervention over a mean follow-up of 4.8 years (median 3 years: IQR 2–5.5 years). Of all the 40 patients, 39 patients had >1-year follow-up and 1 patient with only a 6-month follow-up.
Table 1 summarizes the clinical features of children who needed a second intraoperative surgical intervention. Out of 45 (5.53%) eyes, 28 were pseudophakic and 17 were aphakic. Out of 40 children, 22 were boys and 18 were girls. Out of 45 eyes, 3 had preexisting posterior lenticonus and 5 had microcornea (2 along with persistent fetal vasculature (PFV) and 1 had only PFV).
Table 2 shows the distribution of the second surgery for all children. Overall incidence of the second intraocular surgery was 5.53% (45/814 eyes: 95% CI: 3.96–7.1%). Most common indications were VAO (2.9%, 24/814), followed by glaucoma (0.73%, 6/814). The incidence of repeat surgery was slightly less in pseudophakics (4.91%, 28/570) vs aphakics (6.91%, 17/244), though not statistically significant (P=0.31). The incidence of VAO was significantly less in pseudophakics (2.1%, 12/570) vs aphakics (4.9%, 12/244) (P=0.05). However, if we excluded eyes with microcornea and PHPV cases, incidence of repeat surgery and VAO in aphakic group lowers from 4.5% (12/244) to 2.86% (7/244), respectively. The overall prevalence of glaucoma was 3.4% (28 eyes of 24 patients). Most children were managed medically. The incidence of glaucoma necessitating surgery in pseudophakia was 0.35% (2/570) vs 1.6% (4/244) in aphakia (P=0.12, 1.2% (3/244) if microcornea and PFV are excluded).
Heightened postoperative acute inflammation was seen in 24 eyes (2.9%; 24/814: 2 aphakic, 22 pseudophakic), however, only 7 eyes had sequelae of inflammation (IOL deposits and posterior synechiae) and only 1 eye underwent IOL exchange.
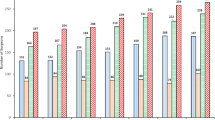
Out of 24 eyes with VAO, 18 eyes (75%) had their first surgery when they were <1 year old. The incidence of VAO was significantly higher in children <1 year of age. Out of 308 eyes operated at age <1 year, 19 had VAO (6.1%) vs 5/506 eyes (1%) in children operated at age >1 year (P=0.001). In addition, postoperative glaucoma developed exclusively in eyes operated at age <1 year, and of these, four eyes (66.6%) were operated at age <6 months (e-Supplementary Table 1). The incidence of postoperative uveitis was higher in pseudophakic infants 9.6% (10/104) vs 0.4% (1/204) aphakia, P=0.0001, however, only one eye needed repeat intervention. Data of individual complications were summarized in e-Supplementary Table 2 and the distribution of various surgeries at each follow-up year is summarized in e-Supplementary Table 3.
Table 3 shows that mean BCVA improved postoperatively at last follow-up in children who underwent a second surgical procedure from 1.16±0.56 LogMAR preoperatively to 0.80±0.50 LogMAR. BCVA data were available for patients before and after the surgery. A total of 17 patients had vision <20/200 at last follow-up, even after appropriate intervention. Poor compliance to spectacles and patching in cases with dense amblyopia accounted for poor vision in majority of these cases. One child had poor vision following the intervention for endophthalmitis, 4 due to coexisting glaucoma, 10 due to coexisting amblyopia and poor compliance to glasses and patching, and 2 patients were lost to follow-up after 1 year.
Discussion
In today’s world, although pediatric cataract surgery has become standardized and simplified with the advent of fine microsurgical techniques and instrumentation, incidence of postoperative complications still remain of concern to all pediatric ophthalmologists especially in the infants. The infant aphakia treatment study (IATS) showed that at 4.5-year follow-up, infants who underwent primary IOL implantation or were aphakic and treated with contact lenses (CL) had similar visual outcomes, whereas children who were pseudophakic had a greater incidence of complications and second interventions than CL group (CL, 56%; IOL, 81%; P = 0.02).10 Wilson et al17 (22%) and Lambert et al18 (72%) also reported a significantly high number of reoperations in infants.
As the mean age of the children in the current study was more than in IATS and other studies, it might not be directly possible to compare the results with the older studies. However, as this is the largest study that reports the incidence of various complications in children who underwent primary surgery at <7 years of age, we attempt to compare outcomes in infants and older children with reported literature. As reported in previous studies, majority of the complications occurred in the age group <1 year. However, as compared with the previous studies, the overall incidence of second surgical interventions was relatively low (only 5.5%). The overall incidence in children <1 year was 5.5% (28/308 eyes), which was, still less when compared with the IATS (72%) and other studies. This may be attributable to age difference, genetic differences, surgical technique, difference in the selection of cases at the time of surgery, more intensive postoperative regimes, and the effect of surgery being performed at a single center by a single experienced surgeon.
In addition, unlike previous studies, incidence of complications was not higher in children who had an IOL implantation as against children who were left aphakic. This may be attributable to more intensive postoperative medication regimes followed at our center that lowers the incidence of severe inflammatory response.
As reported in previous studies,5, 8, 10, 11, 15, 16 VAO requiring surgical intervention is the most frequent complication in our study as well (Table 3). Membranectomy constituted 53.3% (24/45) of all the secondary interventions. Five cases with IOL in our series also required Nd: YAG capsulotomy. However, the overall incidence was low as compared with the previous studies; even in infants alone, the incidence of VAO needing a second surgery was 6.1% (19/308). The incidence was 7.7% (8/104 eyes) in pseudophakic and 5.4% (11/204 eyes) in aphakic infants. In a study by Lambert et al6 in 2004, none of the 11 aphakic eyes required intervention for VAO and 70% (7/10) eyes with PCIOL required intervention for VAO. However, as compared with the previous reports, in our series, VAO was seen equally in both pseudophakic and aphakic eyes. This might be attributable to coexisting pathology in eyes left aphakic, such as microcornea and PHPV. If we excluded eyes with microcornea and PHPV cases, incidence of repeat surgery and VAO in aphakic group lowers to 4.5%.
As previously reported, relative risk of eyes needing secondary surgery for VAO is more, if surgery is performed before 6 months of age.18 Similarly, in our series, children who underwent membranectomy had initial cataract surgery at the age of 0.96±1.44 range (0.08–5 years), suggesting early age was a common risk factor for risk of VAO.
The reported incidence of secondary glaucoma after pediatric cataract surgery varies from 15 to 58%.14 The highest incidence is reported when the surgery is performed early (below the age of 2 months) and in children left aphakic.20, 21
In our study, the incidence of glaucoma was 3.4% (28/814) and glaucoma requiring surgical intervention was 0.73% (6/814) (13.3% of all the secondary interventions). As noted above, all our patients who developed glaucoma were operated at age <1 year. In this subgroup, the incidence of glaucoma was 6% (16/308) with a mean follow-up of 4.8±2.3 years. Average age of these children at the time of initial surgery was 0.31±0.29 (range 0.08–0.75) years. Average interval between primary cataract and glaucoma surgery was 1.94±2.4 years (range: 0.17–5 years). Unlike previous reports, the incidence of surgery for secondary glaucoma in these patients was similar in pseudophakic (1.9%, 2/104) and aphakic (2.0%, 4/2014) eyes. Out of these 6 cases, 3 cases had trabeculotomy and trabeculectomy, 2 had trabeculectomy with mitomycin-C, and 1 had transscleral cyclophotocoagulation.
Factors which have been reported to influence the risk of glaucoma in children include age at surgery, preexisting ocular abnormalities, type of cataract and the effect of lens particles, lens proteins, inflammatory cells, retained lens material, type of lensectomy, development of pupillary block, and duration of postoperative follow-up.21 Our results are similar to those suggested by Rabiah13 and Haargaard et al,22 who suggested that the risk of glaucoma was higher in children operated before 9 months of age.
In our series, four eyes had IOL exchange for varied reasons: two for significant pigments on IOL, one for lens dislocation into vitreous and one for anterior subluxation of the IOL. Three children in our series had a significant IOL decentration or dislocation necessitating IOL exchange or repositioning. One child had IOL exchange for IOL drop through posterior capsulotomy and underwent pars plana vitrectomy and IOL exchange within a week of primary surgery.
Another child had IOL exchange as superior haptic had subluxated into anterior chamber after 5 years of surgery. A third child required IOL repositioning for significant decentration. This might be attributable to capsular bag instability from radial tears or poor construction capsulotomies,23 vitreous prolapse, instability produced by a posterior capsulotomy, and significant growth of the eyes of younger children.24
A fourth child, operated at 4 months of age, with IOL in sulcus had significant deposits on IOL and underwent IOL exchange after 5 years. This might be seen secondary to fibrinoid uveitis in the early postoperative period or owing to the sulcus implantation of the IOL, and may result in the formation of posterior synechiae, pigment deposition on the IOL, pupil irregularity, and IOL decentration occasionally. Sharma et al8 have reported that sequelae of uveitis were present in 30.8% of eyes in their series. Use of intraoperative heparin in the irrigating fluid might reduce the incidence of fibrinoid uveitis.25 However, the incidence was reported less in our study (2.4%, 24/814 overall and 3.5%, 11/308 infants). In our opinion, atraumatic surgical techniques, in-the-bag fixation of IOLs, and intensive postoperative steroid treatment (prednisolone acetate 1% starting 12 times a day and slow taper over 6 weeks) are other contributing factors that help reduce inflammatory responses. It is mentioned that years after surgery, decentralization and iris chafing can occur with the single-piece AcrySof IOL (Alcon Laboratories, Inc.) implanted in the sulcus.22 One child with posterior lenticonus had to undergo vitrectomy for vitreous wick syndrome within a month.
Endophthalmitis is one of the most serious complications after intraocular surgery in children, with an incidence similar to that observed following adult cataract surgery.16 In our series, two children developed endophthalmitis after surgery via a scleral incision. The children underwent vitreous biopsy+intraocular antibiotic injection. However, biopsy showed inflammatory cells and no organisms were identified on culture. Even after surgery, BCVA did not improve significantly in these patients owing to possible macular damage.
In our series, we claim that low prevalence of complications leading to resurgery is owing to a thorough preoperative examination, good surgical technique with minimal intraoperative manipulation, optimal postoperative regimen, relatively older children, and long-term follow-up.26, 27
Our study is limited by its retrospective nature, occasional ciliary sulcus placement of IOL, different IOL models being used over time, and loss of patients to follow-up. However, our study does suggest that the incidence of second surgery after primary IOL implantation in children, especially VAO- and IOL-related complications, might be less frequent than previously reported. Further, the incidence of complications does not tend to be higher in pseudophakic children as compared with aphakic children. Our study however cautions that the incidence of glaucoma might be significantly higher especially in children operated at an early age.

References
Lundvall A, Kugelberg U . Outcome after treatment of congenital bilateral cataract. Acta Ophthalmol Scand 2002; 80 (6): 593–597.
Robb RM, Petersen RA . Outcome of treatment for bilateral congenital cataracts. Ophthalmic Surg 1992; 23 (10): 650–656.
Keech RV, Tongue AC, Scott WE . Complications after surgery for congenital and infantile cataracts. Am J Ophthalmol 1989; 108 (2): 136–141.
Lundvall A, Zetterström C . Complications after early surgery for congenital cataracts. Acta Ophthalmol Scand 1999; 77 (6): 677–680.
Parks MM . Posterior lens capsulectomy during primary cataract surgery in children. Ophthalmology 1983; 90 (4): 344–345.
Lambert SR, Lynn M, Drews-Botsch C, DuBois L, Plager DA, Medow NB et al. Optotype acuity and re-operation rate after unilateral cataract surgery during the first 6 months of life with or without IOL implantation. Br J Ophthalmol 2004; 88 (11): 1387–1390.
Plager DA, Yang S, Neely D, Sprunger D, Sondhi N . Complications in the first year following cataract surgery with and without IOL in infants and older children. J AAPOS 2002; 6 (1): 9–14.
Sharma N, Pushker N, Dada T, Vajpayee B, Dada V . Complications of pediatric cataract surgery and intraocular lens implantation. J Cataract Refract Surg 1999; 25 (12): 1585–1588.
Knight-Nanan D, O'Keefe M, Bowell R . Outcome and complications of intraocular lenses in children with cataract. J Cataract Refract Surg 1996; 22 (6): 730–736.
Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR . Complications, adverse events, and additional intraocular surgery 1 year after cataract surgery in the infant Aphakia Treatment Study. Ophthalmology 2011; 118 (12): 2330–2334.
Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR . Infant Aphakia Treatment Study Group. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol 2014; 158 (5):892–898.
Basti S, Aasuri MK, Reddy S, Reddy S, Rao GN . Prospective evaluation of corneal endothelial cell loss after pediatric cataract surgery. J Cataract Refract Surg 1998; 24 (11): 1469–1473.
Rabiah PK . Frequency and predictors of glaucoma after pediatric cataract surgery. Am J Ophthalmol 2004; 137 (1): 30–37.
Chen TC, Bhatia LS, Halpern EF, Walton DS . Risk factors for the development of aphakic glaucoma after congenital cataract surgery. Trans Am Ophthalmol Soc 2006; 104 (2): 241–251.
Chang W, Kim J, Moon S, Kim J . Retinal detachment following congenital cataract surgery. Invest Ophthalmol Vis Sci 2007; 48 (13): 5747–5748.
Wheeler DT, Stager DR, Weakley DR . Endophthalmitis following pediatric intraocular surgery for congenital cataracts and congenital glaucoma. J Pediatr Ophthalmol Strabismus 1992; 29 (3): 139–141.
Wilson ME, Peterseim MW, Englert JA, Lall-Trail JK, Elliott LA . Pseudophakia and polypseudophakia in the first year of life. J AAPOS 2001; 5 (4): 238–245.
Lambert SR, Lynn M, Drews-Botsch C, Loupe D, Plager DA, Medow NB et al. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. J AAPOS 2001; 5 (2): 70–75.
Kekunnaya R, Gupta A, Sachdeva V, Rao HL, Vaddavalli PK, Prakash VO . Accuracy of intraocular lens power calculation formulae in children less than two years. Am J Ophthalmol 2012; 154 (1): 13–19.e2.
Michaelides M, Bunce C, Adams GG . Glaucoma following congenital cataract surgery-the role of early surgery and posterior capsulotomy. BMC Ophthalmol 2007; 7: 13.
Mandal AK, Netland PA . Glaucoma in aphakia and pseudophakia after congenital cataract surgery. Indian J Ophthalmol 2004; 52 (3): 185–198.
Haargaard B, Ritz C, Oudin A, Wohlfahrt J, Thygesen J, Olsen T et al. Risk of glaucoma after pediatric cataract surgery. Invest Ophthalmol Vis Sci 2008; 49 (5): 1791–1796.
Lambert SR, Drack AV . Infantile cataracts. Surv Ophthalmol 1996; 40 (6): 427–458.
Astle WF, Ingram AD, Isaza GM, Echeverri P . Paediatric pseudophakia: analysis of intraocular lens power and myopic shift. Clin Experiment Ophthalmol 2007; 35 (3): 244–251.
Bayramlar H, Totan Y, Borazan M . Heparin in the intraocular irrigating solution in pediatric cataract surgery. J Cataract Refract Surg 2004; 30 (10): 2163–2169.
Trivedi RH, Wilson Jr ME, Bartholomew LR, Lal G, Peterseim MM . Opacification of the visual axis after cataract surgery and single acrylic intraocular lens implantation in the first year of life. J AAPOS 2004; 8 (2): 156–164.
Uy HS, Chan PS . Pigment release and secondary glaucoma after implantation of single-piece acrylic intraocular lenses in the ciliary sulcus. Am J Ophthalmol 2006; 142 (2): 330–332.
Acknowledgements
The work was supported by Hyderabad Eye Research Foundation (HERF). Dr Akhila Acharya helped with English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work was presented as an e-poster at the 42nd Annual Meeting of American Academy of Pediatric Ophthalmology and Strabismus, 7–10 April 2016, Vancouver, BC, Canada.
Supplementary Information accompanies this paper on Eye website
Rights and permissions
About this article
Cite this article
Sachdeva, V., Katukuri, S., Ali, M. et al. Second intraocular surgery after primary pediatric cataract surgery: indications and outcomes during long-term follow-up at a tertiary eye care center. Eye 30, 1260–1265 (2016). https://doi.org/10.1038/eye.2016.170
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.170