Abstract
Purpose
To report the changing trend in the utilisation rate of donated corneas for keratoplasty and to examine the reasons for unutilised corneas in the North East of England.
Methods
Relevant data were retrospectively collected from a local eye retrieval database and the UK Transplant Registry for two separate years; namely, 2006 and 2010.
Results
The utilisation rate of donated corneas for keratoplasty improved from 57% (52/92) in 2006 to 71% (220/312) in 2010 (P=0.012). Over the same period, there was a marked reduction of failed serological test results from 24% (22/92) to 5% (14/312) (P<0.001). The leading reasons for unutilised corneas were failed serological test results (22/92, 24%) in 2006 and inadequate tissue quality (23/312, 7%) in 2010. The rate of tissue contamination remained similar between 2006 (4%) and 2010 (6%) (P=0.80). Eleven (4%) corneas were not transplanted due to recipient-related factors in 2010. Donor corneas of inadequate tissue quality were associated with older age (P=0.04) but not with gender, donation site, consent method, death-to-enucleation interval, death-to-processing interval, and storage time in the eye bank.
Conclusion
There was a substantial improvement in the utilisation rate of corneas donated in the North East of England between 2006 and 2010. The principal reason was a reduction in failed serological test results. High donor age was associated with increased chance of corneas not being used. Utilisation rate of corneas can be further improved if potential modifiable factors are addressed, such as recipient-related factors and microbial contamination.
Similar content being viewed by others
Introduction
Shortage of eye donors remains a problem in corneal transplantation in many countries, including the UK1 (http://nhsbtmediaservices.blob.core.windows.net/organ-donation-assets/pdfs/cornea.pdf). In 2007, the Newcastle Eye Retrieval Scheme, which serves as one of the 10 eye retrieval schemes funded by National Health Service Blood and Transplant (NHSBT) in the UK, introduced telephone consent with the aim of overcoming barriers of face-to-face consenting and consequently improving the eye donation rate in the North East of England, predominantly the Northumberland, Tyne and Wear regions (NTW). We recently reported the success of this initiative, which demonstrated an 88% increase in eye donation when telephone consent was used in addition to the conventional face-to-face interview.2
Nonetheless, merely increasing the eye donation rate is not sufficient. A successful corneal transplant relies on a series of well-defined steps in the donation–transplantation pathway, starting with identification and referral of potential donors, approaching the relatives of these potential donors to obtain consent for eye donation, eye retrieval, transport of the eyes to the eye bank for processing and corneal storage, donor testing for markers of transmissible disease, and investigation of the donor’s medical history to exclude corneas from donors with medical contraindications to transplantation, quality assessment (eg, based on endothelial cell density) of corneas, and ultimately transplanting the donated corneas. Any break in this chain will prevent transplantation and reduce the utilisation of potentially suitable corneas.
So far, there have been no published studies examining the utilisation rate of corneas donated in the North East of England and the reasons for not using corneas. The aims of our paper are threefold: first, to report the changes in the utilisation rate of the donated corneas for keratoplasty from NTW between 2006 and 2010; second, to examine the reasons for not using corneas; and third, to identify areas for potential improvement in the utilisation rate of the corneas.
Materials and methods
The Newcastle Eye Retrieval Service covers a major part of the North East of England, including Newcastle upon Tyne, Gateshead, Sunderland, Northumberland, Tyneside, County Durham, and North Cumbria. For descriptive and analytic purposes we only included eye donation sites that fall within NTW, which was coded as UKC2 under the Eurostat Nomenclature of Territorial Units for Statistics.3 All the hospitals, the hospices, and the funeral directors were included in the study. The population of NTW is estimated to be 1.4 million4 (http://www.twri.org.uk/sites/default/files/twri/twri_Bulletin_Population_TW_2010.pdf).
Data pertaining to donors’ demographic factors, eye donation sites, consent method, death-to-enucleation interval (DEI), death-to-processing interval (DPI), suitability of donated eyes for transplantation, and storage time in the Manchester eye bank in 2006 and 2010 were retrospectively collected from our local eye retrieval database (Royal Victoria Infirmary, Newcastle Upon Tyne, UK) and the NHSBT UK Transplant Registry. Our study did not require any ethical approval, but was conducted according to the tenets of Declaration of Helsinki.
Eye donation sites
In view of the variation of the eye donation and eye retrieval processes, all the hospitals in NTW were divided into two categories: (1) within Newcastle upon Tyne and (2) outside Newcastle upon Tyne. Hospices and funeral directors were classified as ‘others’ under the ‘outside Newcastle upon Tyne’ group.
Process of eye donation and retrieval
Hospitals within Newcastle upon Tyne
The process of eye donation and retrieval in our region has been described previously.2 Briefly, all deaths in hospitals within Newcastle upon Tyne were identified by two full-time eye donation specialist nurses (JP and TL). They were trained by the NHSBT to identify potential eye donors, to examine medical records for medical contraindications, to approach and obtain consent for eye donation from relatives, and to retrieve eyes from suitable donors. Cases where the death-to-enucleation interval exceeded 24 h were excluded under NHSBT guidelines.
In 2006, before the introduction of telephone consent, families of all suitable cases were approached via face-to-face interview. In 2010, if face-to-face interview was not possible, telephone consent would then be attempted through a standardised and validated procedure in accordance with the Human Tissue Act (2004). Following consent, eyes were retrieved, and sent for processing in the Manchester eye bank, which is part of the national Corneal Transplant Service of NHSBT.
Hospitals outside Newcastle upon Tyne
The referral system for donors outside Newcastle upon Tyne was slightly different because there were no dedicated eye donation nurses available at these hospital sites. Therefore, relatives of the deceased were either initially approached by the hospital’s bereavement officer, or staff in critical care units, emergency departments, and general wards to discuss eye donation. In all above circumstances, the potential donors were referred to the NHSBT National Referral Centre based in Liverpool who then telephoned the relatives of the deceased to obtain consent for eye donation. Eye donation nurses (JP and TL) would subsequently be contacted to complete the donation process and carry out the eye retrieval.
Eye retrieval time intervals
Time taken from a donor’s death to eye retrieval (by enucleation) was defined as ‘DEI’. The entire process of eye retrieval from a donor’s time of death to the time of processing of the eyes (corneoscleral disc excision and organ culture storage) in the eye bank was termed ‘DPI’.
Utilisation rate of the donated corneas
Utilisation rate of the donated corneas refers to the proportion of corneas from the retrieved eyes that were actually used for transplantation. Reasons for non-use of donated corneas were classified into six main groups, including failed serology (ie, confirmed positive, repeatedly reactive samples, poor blood sample quality, or missing serological test results), other medical contraindications, microbial contamination during organ culture storage of corneas, poor tissue quality (eg, endothelial cell density <2200 cells per mm2, central corneal opacity), recipient factors (eg, a cornea issued for a transplant but the patient was unfit, unavailable, or no longer required transplant), and others. Factors likely to influence the quality of donated corneas, including donor age, gender, cause of death, eye donation site, consent method, DEI, DPI, and storage time in the eye bank, were also analysed.
Statistical analysis
The study included eyes donated during January to December 2006 (period 1) and January to December 2010 (period 2) as representative of periods before and after the introduction of telephone consent in 2007. Means were compared by unpaired t-tests. Chi-squared tests or, where one or more counts were <5, Fisher’s exact test were used to examine the difference in frequencies of categorical variables. The level of significance was set at 5%.
Results
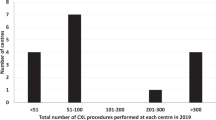
There was a threefold increase in eye donation in NTW from 48 donors (96 eyes) in 2006 to 157 donors (312 eyes) in 2010. This represented an increase in eye donors per million population (p.m.p.) from 34.3 to 112.1 p.m.p. The proportion of eye donors from hospitals within Newcastle upon Tyne remained similar between 2006 (67%) and 2010 (70%; Table 1).
Process of eye retrieval
The DEI in 2006 was 18.4 h (SD 5.2), which was similar to the DEI of 16.7 h (SD 5.7) in 2010 (P=0.15). Similarly, little difference was observed in DPI between 2006 and 2010, which were, respectively, 37.2 h (SD 6.5) and 35.3 h (SD 6.8; P=0.30).
Utilisation rate of donated corneas
Utilisation rate of the donated corneas for keratoplasty increased from 57% (52/92 eyes) in 2006 to 71% (220/312 eyes) in 2010 (P=0.012). Four eyes in 2006 were excluded from the analysis because they were donated for research-use only. The leading reasons for unutilised corneas in 2006 and 2010 were, respectively, failed serology (24%) and inadequate corneal tissue quality (7%), respectively (Table 2). There was a reduction of failed serology from 2006 (24%) to 2010 (5%) (P<0.001). The microbial contamination during organ culture was similar in 2006 (4%) and 2010 (6%) (P=0.80). In 2010, recipient-related factors and other medical contraindications accounted for the non-use of, respectively, 4% and 5% of corneas.
Factors influencing the quality of donated corneas
In 2006 and 2010, a total of 404 corneas were donated: 272 (67%) donated corneas were utilised, whereas 28 (7%) donated corneas were excluded owing to inadequate tissue quality. To avoid the potential lack of independence between corneas from the same patient, only one cornea from each of these patients was included in the analysis. This resulted in 163 corneas being included for analysis, of which 17 were non-used corneas (Table 3). Non-use of corneas was associated with older donor age (P=0.04), but not with gender, donation site, consent method, DEI, DPI, and storage time in the eye bank.
Discussion
The Newcastle Eye Retrieval Service is one of the 10 NHSBT funded eye retrieval services in the UK. It serves the North East of England, predominantly the NTW region. To the best of our knowledge, our study represents the first detailed report examining the utilisation rate of the corneas donated in the North East of England and the reasons for non-use of corneas.
Utilisation rate of donated corneas
Our study demonstrated a marked increase in utilisation of donated corneas from 2006 (57%) to 2010 (71%; P=0.012). This was primarily attributed to a reduction in the failed serology test results from 2006 (24%) to 2010 (5%; P<0.001). Failed serology included samples where tests could not be carried out owing to poor quality (eg, haemolysis) or samples that were repeatedly reactive for serological tests for markers of transmissible disease. Donors had to be excluded on the basis of repeat reactive tests, even if subsequent confirmatory testing showed the samples to be negative. This was a particular problem with human T-lymphotrophic virus (HTLV) testing.5 However, changes to the testing protocols at the NHSBT National Transfusion Microbiology Reference Laboratory (Colindale, London) reduced the loss of donors for serological reasons and, provided confirmatory testing shows the reactivity to be non-specific, the UK Blood Services guidelines (www.transfusionguidelines.org.uk) no longer exclude tissue donors with repeatedly reactive test samples (personal communication, W. John Armitage, 2015).
The utilisation rate of 71% observed in our study in 2010 was comparable to the rates reported in US (66%) in 2013 and UK in 1999–2005 (70%) and 2014–2015 (64%)6, 7 (http://nhsbtmediaservices.blob.core.windows.net/organ-donation-assets/pdfs/cornea.pdf). However, it was lower than the rate reported in New Zealand National Eye Bank (NZNEB) study (88%),8 suggesting potentials for further improvement in the future. Our data showed that 4% of corneas judged to be suitable for transplantation were not used in 2010 owing to recipient-related factors, including recipients who were unfit or unavailable or no longer requiring transplantation. This problem could be addressed by confirming the recipients’ availability and their fitness and need for surgery one week prior to the corneal transplantation. Five per cent of corneas were excluded owing to other medical contraindications. Whether these could have been identified before eye retrieval needs to be investigated. Also, we observed a tissue contamination rate of 5.8% in 2010, which was similar to the nationwide data of the UK in 1999–2005 (contamination rate of 5.7%)6 but higher than the rate reported in 2014–2015 (3%),7 demonstrating that there had been an improvement in the processing and preservation of the retrieved corneas in UK eye banks over the recent years. However, these rates were slightly higher than the data reported by the NZNEB study (1%).8 The difference in the contamination rate might be owing to various factors, including the cause of death, enucleation process, cleaning protocol before corneoscleral disc excision, and choices of antibiotic and antimycotic used in the organ culture medium during storage in the eye bank.7 Therefore, future studies examining and analysing the protocols of different eye banks in relation to the contamination rate will be useful. If all potentially modifiable factors reported before (ie, recipient-related factors, other medical contraindication, and tissue contamination) are addressed in our study, the utilisation rate could potentially be improved from 71 to 84%, which will be similar to the rate reported by NZNEB (88%). Despite what has just been said, it is well known that the main way to improve donor corneas usability is to reduce donor age; however, although that may increase suitable corneas it may reduce the absolute number of corneas available for transplantation.7, 8, 9
In 2010, inadequate tissue quality was the leading reason for non-use of corneas, representing 7% of all the retrieved corneas. Eye banks in the USA similarly reported that the main reason for unused corneas in 2013 was inadequate tissue quality, consisting of 11% of all the retrieved corneas.6 We observed that older age was negatively associated with the quality of the corneas (P=0.04), which is consistent with the data published by Armitage et al and NZNEB study.7, 8, 9 Furthermore, the Australian Corneal Graft Registry reported that increasing donor age negatively influences the long-term survival of grafts performed for all indications excluding keratoconus.10 At the time of our study, there was no upper age limit for eye donation in the UK. Since 2012, an upper age limit of 85 years old had been in place in the UK; however, the utilisation rate of the donated corneas did not increase (64% in the UK in 2014/2015; http://nhsbtmediaservices.blob.core.windows.net/organ-donation-assets/pdfs/cornea.pdf), suggesting that perhaps the upper age limit for eye donation needs to be set lower. Nonetheless, this may inevitably reduce the absolute numbers of suitable donated eyes for corneal transplant.
With the increasing uptake of the lamellar keratoplasty techniques in the recent years,11, 12, 13, 14 this may have a positive impact on the utilisation rate of the donated corneas in the future. For instance, donated corneas with stromal opacity can be potentially used for endothelial keratoplasty (eg, Descemet’s membrane endothelial keratoplasty) and those with poor endothelial cell counts can be used in anterior lamellar keratoplasty. Therefore, setting an upper age limit to improve the tissue quality of the donated corneas (ie, endothelial function) may not be relevant in the future.
One of the limitations in our study is that examination of the influencing factors on tissue quality of the donated corneas was limited to univariate analysis as there was insufficient sample size to allow for further multivariate analysis. However, our results paralleled the findings reported in other larger studies.7, 8, 9
In summary, our study highlights the changing trend in the utilisation rate of donated corneas for keratoplasty from the North East of England. We found a marked increase in utilisation rate between 2006 and 2010 as a result of improved protocols for donor serological testing for HTLV. Donor age had a major influence on suitability of corneas for transplantation. However, while reducing donor age may increase the utilisation rate this may result in a reduction in the absolute numbers of corneas available for transplantation.

References
Sundmacher R, Reinhard T . Meeting the demand for quality and safety checked corneal transplants. The role of corneal banks and health care organizations in Germany. Ophthalmologe 2001; 98: 277–284.
Ting DS, Potts J, Lawther T, Jones M, Armitage WJ, Figueiredo FC . Impact of telephone consent and potential for eye donation in the UK: the Newcastle Eye Centre Study. Eye (Lond) 2016; 30: 342–348.
http://ec.europa.eu/eurostat/web/nuts. (accessed on 28 July 2015).
http://www.northumberland.gov.uk/Default.aspx?page=16002. (accessed on 28 July 2015).
Thomas S, Klapper PE, Mutton KJ, Turner AJ, Tullo AB, Zambrano I et al. Lack of vision, loss of sight: consequences of mandatory HTLV screening in corneal transplantation. Transpl Infect Dis 2007; 9: 171–172.
Eye Bank Association of America 2013. Available at http://www.restoresight.org/wp-content/uploads/2014/04/2013_Statistical_Report-FINAL.pdf.
Armitage WJ, Jones MN, Zambrano I, Carley F, Tole DM ; NHSBT Ocular Tissue Advisory Group and Contributing Ophthalmologists OTAG Audit Study 12. The suitability of corneas stored by organ culture for penetrating keratoplasty and influence of donor and recipient factors on 5-year graft survival. Invest Ophthalmol Vis Sci 2014; 55: 784–791.
Cunningham WJ, Moffatt SL, Brookes NH, Twohill HC, Pendergrast DG, Stewart JM et alNHSBT Ocular Tissue Advisory Group and Contributing Ophthalmologists OTAG Audit Study 12. The New Zealand National Eye Bank study: trends in the acquisition and storage of corneal tissue over the decade 2000 to 2009. Cornea 2012; 31: 538–545.
Armitage WJ, Easty DL . Factors influencing the suitability of organ-cultured corneas for transplantation. Invest Ophthalmol Vis Sci 1997; 38: 16–24.
Williams KA, Lowe MT, Keane MC, Jones VJ, Loh RS, Coster DJ . The Australian Corneal Graft Registry 2012 Report. Available at http://dspace.flinders.edu.au/xmlui/handle/2328/25860 (accessed on 28 July 2015).
Park CY, Lee JK, Gore PK, Lim CY, Chuck RS . Keratoplasty in the United States: A 10-year review from 2005 through 2014. Ophthalmology 2015; 122: 2432–2442.
Tan JC, Holland SP, Dubord PJ, Moloney G, McCarthy M, Yeung SN . Evolving indications for and trends in keratoplasty in British Columbia, Canada, from 2002 to 2011: a 10-year review. Cornea 2014; 33: 252–256.
Keenan TD, Jones MN, Rushton S, Carley FM . National Health Service Blood and Transplant Ocular Tissue Advisory Group and Contributing Ophthalmologists (Ocular Tissue Advisory Group Audit Study 8). Trends in the indications for corneal graft surgery in the United Kingdom: 1999 through 2009. Arch Ophthalmol 2012; 130: 621–628.
Ting DS, Sau CY, Srinivasan S, Ramaesh K, Mantry S, Roberts F . Changing trends in keratoplasty in the West of Scotland: a 10-year review. Br J Ophthalmol 2012; 96: 405–408.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ting, D., Potts, J., Jones, M. et al. Changing trend in the utilisation rate of donated corneas for keratoplasty in the UK: The North East England Study. Eye 30, 1475–1480 (2016). https://doi.org/10.1038/eye.2016.145
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.145