Abstract
Purpose
To investigate the role of protein oxidative damage and antioxidant defense in relationship to hyperglycemia measured as fasting plasma glucose (FPG), glycated hemoglobin (A1C), and duration of disease in type 2 diabetes mellitus (DM) and diabetic retinopathy (DR).
Methods
This study recruited 23 non-diabetic subjects, 16 DM patients without any complications and 18 DR patients. The serum ischemia modified albumin (IMA) and glutathione (GSH) levels were measured. The IMA results were corrected for serum albumin. Between-group differences were studied by analysis of variance and between-variable associations were studied by Spearman’s and partial correlations.
Results
IMA and cIMA values were elevated, whereas GSH was decreased in both patient groups vs controls (P<0.05), and the increase in IMA formation is not related to serum albumin changes. DR patients have much severe oxidative stress (OS) status with high IMA and cIMA, and low GSH than in the DM group (P<0.05). Both FPG and A1C levels were positively associated with IMA in DM group, while in the DR group, duration of disease too had a positive association with IMA. The antioxidant GSH had negative correlations with FPG (r=−0.52, P=0.02) and IMA (r=−0.49, P=0.03) in the DR group. Partial correlation analyses predicted mutual or independent associations among parameters.
Conclusions
Severe OS in DR has been associated with increased FPG, A1C, and disease duration. Both hyperglycemia and elevated oxidative damage detected as IMA are collectively associated with depleted GSH status. Our study unravels the need for monitoring of OS in addition to standard glycemic management in DR.
Similar content being viewed by others
Introduction
Highly reactive free radicals (FRs) are kept in equilibrium, and their deleterious oxidative activities are counteracted by various antioxidant defense systems, maintaining health in vivo. Dyshomeostasis between FRs and antioxidants results in oxidative stress (OS) where excess FR production overwhelms the antioxidant defense systems. OS can target and cause oxidative damages to important biomolecules such as lipids, DNA and proteins, resulting in several disease states. OS has been implicated in the pathogenesis of over 100 human diseases, including endocrine disorders.1, 2 Diabetes is the most prevalent, leading endocrine disorder worldwide. Type 2 diabetes mellitus (DM) has been described as a global epidemic with the estimates of 171 million diabetics in 2000, expected an increase to 366–440 million by 2030.3 According to the World Health Organization (WHO), the developing countries presented a rise of about 25% in diabetes rates since 1995.4 With every fifth diabetic in the world in India, it has been described as a diabetic capital of the world.5
The major complications associated with DM include cardiovascular disease, atherosclerosis, neuropathy, nephropathy, and retinopathy.6The key feature that is central to the development of complications is OS, resulting in tissue damage due to elevated FRs and depleted antioxidant defense.7 Globally, DM is the leading cause of blindness, especially in developing countries.8, 9 Hyperglycemia, glycation of hemoglobin, and duration of diabetes disease are among multiple factors involved in the development of diabetic retinopathy (DR).9, 10 In addition, retinal ischemia and OS are important processes in developing DR. Of much importance, it has been reported that hyperglycemia per se lead to increased generation of FRs and OS.11, 12
The status of OS in health and disease is determined by an array of oxidative damage markers and antioxidant defense systems. Research interest concerning OS in diabetes has been in focus in recent times. Although multiple reports13, 14, 15 including ours12 showed increased lipid peroxidation and impaired antioxidant status in diabetes and DR, little published data on protein markers of OS in both diabetes and DR patients are available.11, 16 Although ischemia modified albumin (IMA) has been demonstrated as a novel marker of ischemia, OS and endothelial dysfunction in diabetes17, 18, 19 studies on IMA in DR patients are very scarce. To the best of our knowledge, there is only one study in the literature on IMA levels in human DR patients.11 Among several antioxidant defense systems, reduced glutathione (GSH) is a tripeptide, which is ubiquitous and most abundant in humans. Although decreased levels of GSH were reported in diabetes, the cause of GSH deficiency is still unclear.20, 21 Moreover, to the best of our knowledge, there are no reports that have evaluated IMA and GSH in relation to hyperglycemia, glycated hemoglobin (A1C), and disease duration in both diabetes and DR (literature was mined by PubMed search using MeSH terms diabetes, diabetic retinopathy, free radicals, reactive oxygen species, oxidative stress, albumin, ischemia modified albumin, and glutathione).
Hence, there is a need to have a comprehensive understanding of OS by evaluating protein markers in diabetic and DR patients. With this aim, this study was carried out to determine IMA and GSH levels in both DM and DR patients compared with non-diabetic controls. We also evaluated associations of hyperglycemia, A1C, and disease duration with OS indices.
Material and methods
Study sample
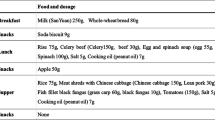
This study prospectively recruits a total of 57 subjects, of which 16 were DM patients (63.6±8.1 years; 7 males), 18 were DR patients (56.9±10.5 years; 11 males), and the remaining 23 were healthy non-diabetic controls (30.5±6.0 years; 13 males). Patients attending the outpatient clinics of ophthalmology, BPS Government Medical College, Sonepat, Haryana, India, were prospectively enrolled. We clearly defined our study sample by means of diagnostic criteria, locality, smoking, alcoholic, and dietary habits. All the participating members were vegetarians, non-smokers, non-alcoholics with similar socioeconomic status and belong to the Sonepat district of Haryana, India. Further, samples drawn were segregated into three groups by highly experienced clinicians. Diabetic patients were grouped into diabetic group without retinopathy and diabetic group with retinopathy and are matched for age and BMI. The control group included non-diabetic hospital controls and is BMI-matched for either of the patient groups. Information on disease duration was obtained from the patient records and the same has been confirmed with the individual patient. Any participant who did not reply at all and any suspected response to hide the facts about habits such as smoking, alcohol consumption, and non-vegetarian diet were excluded from participating in the study. Detailed information about occupation and lifestyle has not been obtained through questionnaires.
The DM patients were diagnosed based on their fasting plasma glucose (FPG) >126 mg/dl and/or or A1C >6.5% according to American diabetes association criteria.22 Patients with DR were diagnosed according to the previously defined criteria.23, 24 All the cases in the DR group had non-proliferative DR. The control group consisted of healthy subjects without any previous history and current evidence of diabetic disease. Exclusion criteria include; smokers, alcoholics, subjects with chronic or acute illness, hypertension, hepatic and renal diseases, inflammatory diseases, pregnancy, obesity, and endocrine diseases other than DM and DR. Informed consent was obtained from the study participants and the institutional ethical committee approved the study protocol.
Biochemical analysis
After 12-h overnight fasting, venous blood samples were drawn into sodium fluoride plus EDTA-treated and additive-free vacutainer tubes (BD Diagnostics, Plymouth, UK). Blood specimens were centrifuged for 15 min at 3000 r.p.m., and aliquots of plasma and serum were used immediately for biochemical analysis or stored at −20 °C until analysis was carried out. Plasma was used for the estimations of FPG by enzymatic glucose-oxidase-peroxidase method using kits provided by Autopak, Siemens Ltd, Gujarat, India on Roche/Hitachi Modular P-800 analyzer (Hitachi High-Technologies Corporation, Tokyo, Japan). The A1C levels were estimated from whole blood collected in EDTA vacutainer by immunoturbidimetry method using tetradecyltrimethylammonium bromide (TTAB method) using commercial kits from Roche Diagnostics (Roche Diagnostics GmbH, Mannheim, Germany), Germany on Roche/Hitachi Modular P-800 analyzer. Serum was used for the estimations of albumin, IMA, and GSH.
The IMA level was analyzed colorimetrically by an albumin cobalt binding assay developed by Bar-Or et al,25 which involves the binding capacity of albumin for Co(II) metal ion. The IMA value was determined by adding fixed amounts of Co(II) to a serum sample and measuring the unbound, free Co(II) with dithiothreitol as the chromogen. A direct relationship exists between IMA concentration and the intensity of the color formation measured at 470 nm. The IMA results were presented in absorbance units (ABSU). The IMA values obtained were corrected for serum albumin concentrations. Corrected IMA (cIMA) was calculated as a ratio of IMA/albumin ((IMA in ABSU/albumin (g/l)) × 1000).26 Serum GSH level was estimated by 5, 5’-dithiobis (2-nitrobenzoic acid), as previously described by Ellman.27
Statistical analysis
All data were expressed as mean±SD. The differences between groups were tested by analysis of variance test. Correlations between the variables were assessed by Spearman and partial correlation analysis. Receiver operating characteristic curve analyses were performed in individual patient groups and all diabetic patients as a whole (DM and DR) vs non-diabetic controls to analyze the difference between IMA and cIMA as a marker of oxidative damage. Statistical analysis was carried out on SPSS software for Windows 11.5 program (SPSS Inc., Chicago, IL, USA) and MEDCALC 12.2.1 version (Broekstraat, Mariakerke, Belgium). Statistical significance was considered at a P value less than 0.05.
Results
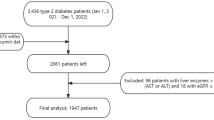
The mean±SD of the parameters studied are presented in Table 1. FPG and A1C were significantly higher in DM and DR groups compared with controls (P<0.05), with no significant difference between DM and DR groups. Although age was significantly higher in the patient groups than in controls, there was no significant difference between patient groups. Compared with the controls, there was an increase in serum IMA among DM and DR patients. There was also an increase in the IMA level between DM and DR groups being higher in the DR group (P<0.05). As serum albumin levels were decreased in our patient groups, the IMA results obtained were corrected for albumin concentrations. The cIMA levels significantly differed (P<0.05) across non-diabetic controls, and DM and DR patient groups with a higher value in the latter group. Levels of antioxidant marker GSH were decreased in both DM and DR patients compared with the non-diabetic controls. Patients with DR had significantly lowered GSH levels than in DM patients (P<0.05).
Results of Spearman’s correlation analysis were shown in Table 2. There were no correlations of age and albumin with any of the study variables in the DM and DR groups. In DM patients, significant positive correlations were found between FPG, A1C, and IMA. Disease duration showed a significant positive association with A1C. IMA was found to be negatively associated with GSH. In the DR group, disease duration showed significant associations with FPG, A1C, IMA, and cIMA. FPG was positively associated with A1C, IMA, and cIMA. GSH showed negative correlations with FPG, IMA, and cIMA. There were no significant associations of albumin with IMA in either of the patient groups.
In both DM and DR groups, the associations of FPG and A1C with IMA were retained when corrected for albumin and age (Table 3). As we found both FPG and A1C correlated significantly with IMA in both patient groups, we statistically nullified the effect of FPG on the relation between A1C and IMA. Likewise, we also nullified the effect of A1C on the correlation between FPG and IMA. In the DM group, the associations were lost when corrected for one of the factors, whereas they remained significant in the DR group (Table 3). When the effect of disease duration was controlled, the significance of associations of FPG and A1C with IMA were retained in both patient groups (Table 3). In both patient groups, the associations of IMA with GSH were lost when corrected for FPG (Table 4).
In the DM group, the receiver operating characteristic curve analysis yielded statistically significant (P<0.01) area under curve (AUC) values of 0.724 and 0.766 for IMA and cIMA, respectively. In DR patients, the significant (P<0.0001) AUC values for IMA and cIMA are 0.901 and 0.937, respectively. In a whole patient group (DM+DR), the significant (P<0.0001) AUC values for IMA and cIMA are 0.818 and 0.857, respectively. By comparing AUC values of IMA and cIMA, we found no significant difference in the DM group (P=0.12), the marginal difference in the DR group (0.07), and significant difference in a whole patient (DM+DR) group (P=0.03). In all comparisons, either in individual patient groups or in both patient groups together, cIMA showed better AUC values than that of IMA (Figure 1).
Discussion
Our results demonstrate OS with increased IMA and decreased GSH levels in both DM and DR patients vs non-diabetic controls and these changes were more marked in the DR group than in the DM group.Our findings are in accordance with previous studies in DM17, 18, 19, 20, 21 and DR patients.11 However, we could not find reports on both IMA and GSH simultaneously in DM and DR patients. Moreover, in a previous report on IMA in DR, the IMA values have not been corrected for serum albumin changes.11 Because of the dependence of IMA values on albumin level, it would be important to report albumin levels and IMA values corrected for albumin interference as previously suggested by us28, 29 and others.26 Therefore, for the first time, we report significantly increased cIMA values in both patient groups than in controls and there were higher levels of cIMA in DR patients than in the DM group. It is clear from this observation that IMA formation is significantly increased in our patients, irrespective of serum albumin concentrations.
Although the mechanism of IMA formation is not known precisely, excess FR formation and OS may cause molecular changes on metal binding sites of albumin producing a structural variant, IMA.18, 19 IMA has been well accepted in the literature as a marker of OS, and its elevation has been associated with endothelial dysfunction, inflammation, and hyperglycemia in different types of diabetes with and without complications.17, 18, 19, 30, 31, 32, 33, 34
Hyperglycemia in DM is linked to OS, and retinal exposure to hyperglycemia activates multiple enzymes/pathways accelerating OS and development of DR.9, 10, 11, 35 Hyperglycemia promotes increased IMA formation probably owing to mechanisms of hypoxia and OS.17, 18, 19 Interestingly, it was reported that increased glycosylation of hemoglobin increases its affinity for oxygen, therefore, preventing its release at the tissue inducing hypoxia and OS.25, 36 Positive associations of IMA with FPG and A1C in our patient groups (Table 2) may be owing to the role of hyperglycemia and A1C as an OS inducer.
As we found a significant change in serum albumin and age, we statistically controlled for these changes on the associations of IMA with FPG and A1C. By this, we tested whether significant changes in albumin and age affect the association between glycemic status and OS. This is important in view of evidence on age-associated increase in OS and decline in glucose metabolism.37 After controlling for one factor at a time, the significant correlations were retained in both patient groups (Table 3). These suggest that the positive associations of FPG and A1C with IMA are independent of age and albumin changes.
Further, it is also known that hyperglycemia increases hemoglobin glycosylation as is evident in this study by a positive association between FPG and A1C. Goodarzi et al38 reported a significant relationship of A1C with OS in diabetes. Thus, we speculate that higher A1C levels may per se be associated with a higher level of IMA. To test this, we statistically controlled for A1C on the positive association between FPG and IMA. Similarly, we also controlled for FPG on the association between A1C and IMA in both patient groups. By this, it was found that the significance of correlations was lost in DM patients, indicating that both elevated FPG and A1C levels are intimate factors that were collectively associated with increased IMA levels. However, the significant associations had been retained in the DR group (Table 3). This clearly suggests that both high FPG and A1C levels were independently associated with increased IMA levels, possibly contributing to the severe OS in the DR group. This is despite of no significant difference in FPG and A1C levels between DM and DR groups.
Why do patients with DR show high amounts of oxidative damage? Were associations of FPG and A1C levels adequately explaining this? Could there be any other contributing factor? Of importance, disease duration was significantly higher in DR patients vs the DM group, and it showed positive associations with FPG, A1C, and IMA. Therefore, we statistically nullified for disease duration on the positive associations of FPG and A1C with IMA. By this, we answered whether or not disease duration significantly affects these positive associations. After nullification, it was found that the significance of associations of FPG and A1C with IMA had been retained in both the patient groups (Table 3). This suggests a multifactorial interplay in the development of FR-mediated oxidative damage resulting in elevated IMA levels. It appears that higher levels of IMA in the DR group than in the DM group may be due to high disease duration in the former group. It is further supported by significant positive associations of disease duration with IMA and cIMA in DR patients (Table 2).
The ability of a cell to resist oxidant damage is determined by a balance between free radicals and antioxidants. GSH (ϒ-glutamyl-cysteinyl-glycine) is the most abundant antioxidant that has a central role in antioxidant defenses. Several studies reported a decline in GSH concentrations in diabetes.20, 21 The mechanisms underlying decreased GSH in diabetes are hyperglycemia-associated metabolic disturbances, abnormal protein balance, and inadequate GSH synthesis leading to OS.7, 20 In line with this, we observed a negative association between FPG and GSH, as hyperglycemia could per se influence oxidant-antioxidant homeostasis.12
Moreover, GSH may be utilized as an antioxidant to neutralize excess FR generated in diabetes. Although GSH deficiency has been reported in diabetes,21 no previous study has reported its relationship to IMA in both DM and DR patients. Could the lower levels of GSH be a result of elevated IMA values, with a greater utilization of GSH as an antioxidant? To answer this question, we studied the associations of GSH with IMA (Table 2). The negative association found between GSH and IMA may be because of the role of GSH as a defensive antioxidant against increased IMA. Because hyperglycemia is associated with lower levels of GSH, we also studied the associations of GSH with IMA controlling for FPG, and found that the significance of the association between GSH and IMA was lost in both patient groups (Table 4). This indicates that both hyperglycemia and elevated oxidative damage are mutually associated with the depleted GSH status. Therefore, hyperglycemia and increased OS reflected in elevated FPG and IMA levels might have a role in lowering GSH status.
Because of the known interference from serum albumin changes on IMA results, we studied the performance of IMA as such (before correcting for serum albumin) and cIMA (after correcting for serum albumin) by evaluating AUC for IMA and cIMA through receiver operating characteristic analysis (Figure 1). Comparison of AUC values of IMA and cIMA showed no significant difference (P=0.12) in DM and marginally significant (P=0.07) difference in DR groups (Figures 1a and b, respectively). However, using a combination of DM and DR groups as a whole yielded a significantly (P=0.03) better AUC for cIMA than that of IMA (Figure 1c). Considering the interference of serum albumin changes on IMA measurement and better AUC values for cIMA than IMA in DM (0.766 vs 0.724), DR (0.937 vs 0.901), and whole patient group (0.857 vs 0.818), we propose the importance of cIMA over IMA for evaluating OS.
In conclusion, OS is evidenced as accelerated oxidative damage (IMA formation) and antioxidant deficiency (GSH depletion) in DM and DR with a much severe OS in DR group. On the basis of our observations in accordance with previous studies, it has been postulated that hyperglycemia, high A1C level, and disease duration are multiple factors associated with OS. The positive associations between FPG, A1C, and IMA could be because of the role of hyperglycemia and higher A1C in promoting excess FR production and OS. Duration of disease appears to be an important factor. Depleted GSH level and its negative association with FPG and IMA may be because of the role of GSH as a defensive antioxidant. Furthermore, cIMA values should be preferred over IMA as a measure of oxidative damage owing to its better AUC values and known interference of serum albumin changes on IMA values. Recent evidence suggests that increasing GSH levels with oral precursor supplementation is a viable antioxidant intervention to target diabetic OS directly and could constitute a novel, safe, and inexpensive form of nutritional treatment.21 Diabetes remained to be a leading cause of blindness, and OS is an important mechanism whereby diabetes attributes to associated complications like DR. Therefore, in addition to standard glycemic management, IMA and GSH might be considered for evaluation in monitoring OS injury in diabetes and DR.
Limitations
The main limitation of our study is its limited sample size. However, we ensured enough statistical power. Another limitation is that possible interpretation of these results deals with an incomplete adjustment for confounding. Only a non-diabetic control group was not age-matched. However, both patient groups were matched for age and BMI. We reported associations between parameters by correlation analyses performed on cross-sectional data. It is therefore not possible to establish a causal relationship in our present study. Nevertheless, this study is the first to examine the levels of IMA, cIMA, and GSH markers across the non-diabetic, DM, and DR groups. It is also worth noting that confounding is a broad spectrum, and because case–control and cross-sectional study designs have inherent limitations, we cannot completely exclude the possibility of bias. Therefore, our study results could be considered preliminary and that it would encourage further studies with precise methodology and a large sample size.
Power analysis
As the size/number in the sample depends on the purpose/objective, the objective of the present study was to study OS (IMA, cIMA, and GSH) across the non-diabetic, diabetic group without retinopathy, and DR groups. We performed a power analysis using G*Power version 3.1. To calculate the achieved power when the differences across groups were tested, we first determined the effect size of means using mean values of IMA, cIMA, and GSH in all the three groups, highest standard deviations, the sample size in each group, and total sample size. Then, at a given α value of 0.05, the achieved power was computed. It was found that with a total sample size of 57 in three groups of this study, the achieved power was 0.98 or 98% for IMA, 0.99 or 99% for cIMA, and 0.99 or 99% for GSH. Therefore, the current study sample size, though small, is not underpowered. We also performed a power analysis for FPG and A1C and found that with a total sample size of 57 in three groups of this study, the achieved power was 91% for FPG and 98% for A1C. The results of power analysis along with protocol inputs and output graphs were provided as a Supplementary File.

References
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J . Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 2007; 39: 44–84.
Reddy VS, Gouroju S, Suchitra MM, Suresh V, Sachan A, Srinivasa Rao PV et al. Antioxidant defense in overt and subclinical hypothyroidism. Horm Metab Res 2013; 45: 754–758.
Dooley KE, Chaisson RE . Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis 2009; 9: 737–746.
Wild S, Roglic G, Green A, Sicree R, King H . Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–1053.
Joshi SR, Parikh RM . India—diabetes capital of the world: now heading towards hypertension. J Assoc Physicians India 2007; 55: 323–324.
Reusch JE . Diabetes, microvascular complications, and cardiovascular complications: what is it about glucose? J Clin Invest 2003; 112: 986–988.
Brownlee M . Biochemistry and molecular cell biology of diabetic complications. Nature 2001; 414: 813–820.
Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V . Prevalence of diabetic retinopathy in urban India: the Chennai Urban Rural Epidemiology Study (CURES) eye study, I. Invest Ophthalmol Vis Sci 2005; 46: 2328–2333.
Madsen-Bouterse SA, Kowluru RA . Oxidative stress and diabetic retinopathy: pathophysiological mechanisms and treatment perspectives. Rev Endocr Metab Disord 2008; 9: 315–327.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL . Glycosylated hemoglobin predicts the incidence and progression of diabetic retinopathy. JAMA 1988; 260: 2864–2871.
Turk A, Nuhoglu I, Mentese A, Karahan SC, Erdol H, Erem C . The relationship between diabetic retinopathy and serum levels of ischemia-modified albumin and malondialdehyde. Retina 2011; 31: 602–608.
Manohar SM, Vaikasuvu SR, Deepthi K, Sachan A, Narasimha SR . An association of hyperglycemia with plasma malondialdehyde and atherogenic lipid risk factors in newly diagnosed type 2 diabetic patients. J Res Med Sci 2013; 18 (2): 89–93.
Davì G, Falco A, Patrono C . Lipid peroxidation in diabetes mellitus. Antioxid Redox Signal 2005; 7: 256–268.
Srivatsan R, Das S, Gadde R, Manoj-Kumar K, Taduri S, Rao N et al. Antioxidants and lipid peroxidation status in diabetic patients with and without complications. Arch Iran Med 2009; 12: 121–127.
Gupta MM, Chari S . Lipid peroxidation and antioxidant status in patients with diabetic retinopathy. Indian J Physiol Pharmacol 2005; 49: 187–192.
Gürler B, Vural H, Yilmaz N, Oguz H, Satici A, Aksoy N . The role of oxidative stress in diabetic retinopathy. Eye (Lond) 2000; 14: 730–735.
Ukinc K, Eminagaoglu S, Ersoz HO, Erem C, Karahan C, Hacihasanoglu AB et al. A novel indicator of widespread endothelial damage and ischemia in diabetic patients: ischemia-modified albumin. Endocrine 2009; 36: 425–432.
Kaefer M, Piva SJ, De Carvalho JA, Da Silva DB, Becker AM, Coelho AC et al. Association between ischemia modified albumin, inflammation and hyperglycemia in type 2 diabetes mellitus. Clin Biochem 2010; 43: 450–454.
Piwowar A, Knapik-Kordecka M, Warwas M . Ischemia-modified albumin level in type 2 diabetes mellitus-Preliminary report. Dis Markers 2008; 24: 311–317.
Whiting PH, Kalansooriya A, Holbrook I, Haddad F, Jennings PE . The relationship between chronic glycaemic control and oxidative stress in type 2 diabetes mellitus. Br J Biomed Sci 2008; 65: 71–74.
Sekhar RV, McKay SV, Patel SG, Guthikonda AP, Reddy VT, Balasubramanyam A et al. Glutathione synthesis is diminished in patients with uncontrolled diabetes and restored by dietary supplementation with cysteine and glycine. Diabetes Care 2011; 34: 162–167.
American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care 2014; 37 Suppl 1: s14–s80.
Wu L, Fernandez-Loaiza P, Sauma J, Hernandez-Bogantes E, Masis M . Classification of diabetic retinopathy and diabetic macular edema. World J Diabetes 2013; 4: 290–294.
Wilkinson CP, Ferris FL, Klein RE, Lee PP, Agardh CD, Davis M et alGlobal Diabetic Retinopathy Project Group. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003; 110: 1677–1682.
Bar-Or D, Lau E, Winkler JV . A novel assay for cobalt-albumin binding and its potential as a marker for myocardial ischemia-a preliminary report. J Emerg Med 2000; 19: 311–315.
Seneş M, Kazan N, Coşkun O, Zengi O, Inan L, Yücel D . Oxidative and nitrosative stress in acute ischaemic stroke. Ann Clin Biochem 2007; 44(Pt 1): 43–47.
Ellman GL . Tissue sulfhydryl groups. Arch Biochem Biophys 1959; 82: 70–77.
Reddy VS, Rao PV, Suchitra MM, Garg R . Serum ischaemic-modified albumin levels might not be a marker of oxidative stress in patients with hypothyroidism. Endocrine 2014; 46: 169–170.
Reddy VS, Pasupuleti P, Srinivasa Rao PV, Garg R, Haribabu A . Ischemia-modified albumin in patients with hyperthyroidism and hypothyroidism. Eur J Intern Med 2014; 25: e42–e43.
Ma SG, Jin Y, Hu W, Bai F, Xu W, Yu WN . Evaluation of ischemia-modified albumin and C-reactive protein in type 2 diabetics with and without ketosis. Biomark Insights 2012; 7: 19–26.
Ma SG, Yu WN, Jin Y, Hong B, Hu W . Evaluation of serum ischemia-modified albumin levels in pregnant women with and without gestational diabetes mellitus. Gynecol Endocrinol 2012; 28: 837–840.
Ma SG, Jin Y, Xu W, Hu W, Bai F, Wu XJ . Increased serum levels of ischemia-modified albumin and C-reactive protein in type 1 diabetes patients with ketoacidosis. Endocrine 2012; 42: 570–576.
Ma SG, Wei CL, Hong B, Yu WN . Ischemia-modified albumin in type 2 diabetic patients with and without peripheral arterial disease. Clinics (Sao Paulo) 2011; 66: 1677–1680.
Ma SG, Xu W, Wei CL, Wu XJ, Hong B, Wang ZJ et al. Role of ischemia-modified albumin and total homocysteine in estimating symptomatic lacunar infarction in type 2 diabetic patients. Clin Biochem 2011; 44: 1299–1303.
Kowluru RA, Abbas SN . Diabetes-induced mitochondrial dysfunction in the retina. Invest Ophthalmol Vis Sci 2003; 44: 5327–5334.
Madsen H, Ditzel J . Blood-oxygen transport in first trimester of diabetic pregnancy. Acta Obstet Gynecol Scand 1984; 63: 317–320.
Salmon AB . Oxidative stress in the etiology of age-associated decline in glucose metabolism. Longev Healthspan 2012; 1: 7.
Goodarzi MT, Varmaziar L, Navidi AA, Parivar K . Study of oxidative stress in type 2 diabetic patients and its relationship with glycated hemoglobin. Saudi Med J 2008; 29: 503–506.
Acknowledgements
We would wish to acknowledge and thank Dr Kuldeep (Demonstrator) and Mr Ravi (Lab attendant) for their valuable help in sample collection and biochemical analysis. We especially thank Smt KJ Padmavathi (Assistant Professor-Communication English) for English corrections and Dr N Suresh Babu (Assistant Professor-Statistics) for his expert statistical consultations for this manuscript. Dr VS Reddy specially thank Professor RC Siwach (Director, BPS Govt. Medical College) for his constant and continuous support, encouragement and motivation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr VS Reddy presented this study in abstract form as an e-poster on 14th November 2014 at the endocrine society of India conference (ESICON-2014) in India. All other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Rights and permissions
About this article
Cite this article
Reddy, V., Agrawal, P., Sethi, S. et al. Associations of FPG, A1C and disease duration with protein markers of oxidative damage and antioxidative defense in type 2 diabetes and diabetic retinopathy. Eye 29, 1585–1593 (2015). https://doi.org/10.1038/eye.2015.177
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.177
This article is cited by
-
Diagnostic values of ischemia modified albumin in diabetes-related complications: a narrative review
Journal of Diabetes & Metabolic Disorders (2022)
-
Obstructive sleep apnea and the effect of CPAP treatment on ischemia-modified albumin levels: a multi effect size meta-analysis with diagnostic test accuracy
Sleep and Breathing (2019)
-
Effect of variable antidiabetic treatments strategy on oxidative stress markers in obese patients with T2DM
Diabetology & Metabolic Syndrome (2017)