Abstract
Purpose
Previous epidemiologic studies that focused on the association between open-angle glaucoma (OAG) and dementia showed inconsistent results. In the present study, we explored the association between OAG and dementia in an ethnic Chinese (ie, Taiwanese) population using a population-based data set.
Methods
We retrieved data on study subjects for this case-control study from the Longitudinal Health Insurance Database 2000. We identified 7770 patients who had a diagnosis of dementia as cases, and 7770 subjects matched in terms of sex and age, which were randomly extracted as controls. A conditional logistic regression conditioned on age group, sex, and index year was used to assess the association of dementia with previously diagnosed OAG among the sampled patients.
Results
Of 15 540 patients, 1.70% had prior OAG, including 2.02% of the dementia group and 1.38% of the controls. After adjusting for patient socioeconomic characteristics and comorbid medical disorders, dementia patients were more likely to have had prior OAG than controls (odds ratio (OR): 1.44; 95% confidence interval (CI): 1.12–1.85; P<0.01). In addition, female dementia patients were more likely to have had prior OAG than controls (OR: 1.93; 95% CI: 1.35–2.77; P<0.001), whereas no statistical difference in prior OAG between male dementia patients and controls was found.
Conclusions
Female dementia patients were associated with a higher proportion of prior OAG than were the controls.
Similar content being viewed by others
Introduction
As elderly populations have increased, dementia has become one of the major public health issues worldwide, and impacts of the illness will greatly expand in the future. Internationally, it is estimated that there were 36 million people with dementia in 2010 worldwide, and as the world population ages, the number is predicted to double every two decades.1 Dementia is usually caused by degenerative or vascular etiologies, and aging is recognized as one of the notable major risk factors.2, 3
Glaucoma is a progressive optic neuropathy pathologically characterized by the death of retinal ganglion cells and axon degeneration in the optic nerve, and clinically by abnormal optic disk cupping and visual field defects.4, 5, 6 Although elevated intraocular pressure (IOP) is recognized as one of the well-known risk factors for the development and progression of the disease,7 the pathogenesis of primary open-angle glaucoma (OAG) is still obscure and very intricate with interactions of age effects, genetic influences, and other risk factors.8, 9 Because of similarities between primary OAG and Alzheimer's disease (AD) in animal experimental and human immunohistochemical studies,10, 11 there is increasing evidence suggesting that OAG is a neurodegenerative disease of the eye.12
However, previous epidemiologic studies focusing on the association between OAG and dementia showed inconsistent results.13, 14, 15, 16, 17 There are only four nationwide or population-based studies in Western countries,15, 16, 17, 18 and, to the best of our knowledge, large epidemiologic investigations regarding the association between OAG and dementia are still lacking in Asian populations. Therefore, the aim of this study was to explore the association between OAG and dementia in an ethnic Chinese (ie, Taiwanese) population by means of a case-control design using a large, nationwide population-based data set in Taiwan.
Materials and methods
Database
We retrieved data on study subjects for this case-control study from the Longitudinal Health Insurance Database 2000 (LHID2000). The LHID2000 consists of claims data of 1 000 000 individuals randomly sampled from the 2000 Registry for Beneficiaries (n=23.72 million) of the Taiwan National Health Insurance (NHI) program, which was implemented in 1995 to provide comprehensive and easily accessible medical care for all residents in Taiwan. Some independent researchers have demonstrated the high validity of data derived from the Taiwanese NHI program.19, 20 The LHID2000 enables researchers in Taiwan to trace the medical services of these selected 1 000 000 individuals since the beginning of the Taiwan NHI program. This study was exempted from full review by the institutional review board (IRB) after consulting with the director of Taipei Medical University's IRB, as the LHID2000 consists of de-identified secondary data released to the public for research purposes.
Selection of cases and controls
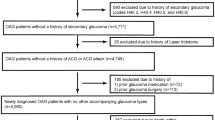
As for the selection of cases in this case-control study, we first selected 13 818 subjects who had received a first-time diagnosis of dementia (International Classification of Disease (ICD)-9-CM codes 290.0–290.3, 294.1, 331.0–331.2, or 331.82) during ambulatory care visits in January 2005 to December 2011. In addition, these selected 13 818 subjects all had received a diagnosis of dementia at least twice coded in their ambulatory care claims, with at least one diagnosis being made by a certified neurologist or psychiatrist, in order to increase the diagnosis validity of this administrative data set. We further excluded subjects aged under 45 years because of the low prevalence of dementia in this age group (n=250). We designated the date of receiving their first dementia diagnosis as the index date for cases. We also excluded those subjects who had ever received a diagnosis of major psychosis or a substance-related disorder (ICD-9-CM codes 291–299 or 303–305), stroke (ICD-9-CM codes 430–438), or traumatic brain injury (ICD-9-CM codes 801–804 or 850–854) before the index date (n=5798). Specifically, stroke cases were excluded as both OAG and dementia might share common vascular risk factors. As a result, we included 7770 subjects with dementia as cases in this study.
As for controls, we first excluded all beneficiaries of the LHID2000 who had ever received a diagnosis of dementia since the initiation of the NHI program in 1995. We then selected 7770 controls matched with the cases in terms of sex, age, and index year. For cases, the year of the index date was the year in which they received their first dementia diagnosis. For controls, the year of the index date was simply a matched year in which the controls had a medical utilization. In addition, we defined the date of their first use of ambulatory care occurring during that matched year as the index date for controls. We further ascertained that none of the selected controls had ever received a diagnosis of major psychosis, a substance-related disorder, stroke, or traumatic brain injury prior to their index date.
Exposure assessment
We identified OAG cases by the principal diagnosis of ICD-9-CM codes 365.1, 365.10, or 365.11 in a medical claim during ambulatory care visits. We only included those subjects who had been diagnosed with OAG at least twice prior to the index date. Furthermore, this study included OAG cases who received treatment with topical antiglaucoma medication only.
Statistical analysis
All statistical analyses were performed using SAS (SAS System for Windows, vers. 8.2, SAS Institute, Cary, NC, USA). A χ2-test was used to compare differences in the sociodemographic characteristics including monthly income, geographic location, and urbanization level of the patient’s residence as well as selected medical comorbidities between cases and controls. The medical comorbidities included hyperlipidemia, diabetes, hypertension, tobacco use disorder, and alcohol abuse. We used conditional logistic regression analyses (conditioned on sex, age, and index year) to explore the association of dementia with previously diagnosed OAG. Furthermore, as there may be surveillance bias as patients with OAG are more likely to have frequent outpatient clinic visits, which may lead to early detection of dementia, we examined the association between dementia and prior urinary calculi. We used the conventional P≤0.05 to assess statistical significance.
Results
The mean age was 76.8 years with a SD of 9.6 years for the study sample. After matching for sex and age group, Table 1 shows that there were no significant differences in the distributions of urbanization level (P=0.243), monthly income (P=0.077), or geographic region (P=0.541) between cases and controls. However, cases had a higher prevalence of comorbidities including hyperlipidemia, diabetes, hypertension, and alcohol abuse than controls.
Table 2 shows the prevalences, odds ratios (ORs), and 95% confidence intervals (CIs) of prior OAG between cases and controls. In total, 264 (1.70%) sampled subjects had been diagnosed with OAG before the index date. The χ2-test showed that there was a significant difference in the prevalence of prior OAG between cases and controls (2.02 vs 1.38%, P<0.001). Furthermore, the conditional logistic regression analysis (conditioned on sex, age, and index year) indicated that the OR of prior OAG for cases was 1.48 (95% CI: 1.15–1.89) compared with controls. Even after adjusting for subject’s hyperlipidemia, diabetes, hypertension, and alcohol abuse and the number of outpatient visits within 1 year prior to index date, the conditional logistic regression analysis still showed that the cases had a higher OR of previously diagnosed OAG than controls (OR: 1.44; 95% CI: 1.12–1.85).
We also examined the relationship between dementia and interaction term between OAG and sex and found that there existed a significant interaction (P<0.05). Therefore, we further presented the relationship between dementia and OAG according to sex in Table 3. Among female subjects, the OR of previously diagnosed OAG for cases was as high as 1.93 (95% CI: 1.35–2.77) compared with controls after adjusting for subject’s hyperlipidemia, diabetes, hypertension, and alcohol abuse, and the number of outpatient visits within 1 year prior to index date. However, among male subjects, we observed no increased odds of prior OAG for cases compared with controls (OR: 1.06, 95% CI: 0.74–1.52).
In addition, we examined the association between dementia and prior urinary calculi. We found that there was no significant relationship between dementia and prior urinary calculi (7.2% for cases and 6.5% for controls, P=0.362).
Discussion
Currently available large epidemiologic data regarding the association between OAG and dementia were all obtained from Western populations, and results are controversial.15, 16, 17 In a longitudinal study using nationwide case register data of patients who had been hospitalized in Denmark, Kessing et al15 found that OAG was not associated with an increased risk of subsequent AD. However, the cases and controls were not matched in terms of sociodemographic characteristics or medical comorbidities, and there may have been a selection bias for patients with more-severe OAG. Similarly, Ou et al,16 using US Medicare claims data, also showed no increased risk of developing dementia after a diagnosis of OAG in nationally representative longitudinal cohorts of elderly persons. Ekström18 further identified a null association between OAG and AD in a population survey in the municipality of Tierp, Sweden. On the contrary, in a population-based longitudinal study in a French city that actively screened for glaucoma and dementia in elderly adults, Helmer et al17 showed a positive association between OAG and subsequent dementia. However, the study population mainly consisted of well-educated subjects and therefore the results might not be applicable to less-educated populations. To our best knowledge, this study is the first population-based study to investigate an epidemiologic association between OAG and dementia, after adjusting for patient sociodemographic characteristics and comorbid medical disorders in an Asian population. Consistent with the findings of Helmer et al, we demonstrated that a statistically significant higher proportion of prior OAG was found among dementia patients compared with the controls, which supports a possible association between OAG and dementia.
The actual mechanisms contributing to the association between OAG and dementia are not fully understood. There is an ample evidence suggesting that vascular risk factors including hypertension, diabetes, and hyperlipidemia are associated with cognitive impairment and increase the risk of AD and vascular dementia.21, 22 Vascular risk factors contributing to vascular dysregulation and microvascular damage are also increasingly acknowledged as potential risk factors for the development and progression of OAG.23, 24 Thus, a possible explanation regarding the association between OAG and dementia is that both diseases share common vascular risk factors. Our analysis adjusted for hypertension, diabetes, hyperlipidemia, and other vascular risk factors such as tobacco and alcohol use. It was suggested that vascular risk factors are not the sole mechanism contributing to the association between OAG and dementia.
In experimental studies using rat models, neurotoxic amyloid-β (Aβ), the core element of amyloid plaques in the AD brain, exhibited abnormal aggregation in retinal ganglion cells of eyes affected by elevated IOP.10, 25 Activation of caspases, a group of proteases essential for apoptosis, that cleave amyloid precursor proteins into neurotoxic Aβ was also demonstrated in an ocular hypertensive model of rat glaucoma, implying a role of Aβ neurotoxicity in retinal ganglion cell death and the pathogenesis of glaucoma.12, 26 Furthermore, there is emerging evidence that abnormal hyperphosphorylation of the microtubule-associated tau protein, a crucial injury marker of neuronal integrity and axonal transport in neurodegenerative diseases such as AD, was found in the retina of human glaucoma patients with elevated IOP.27 The presence of neurotoxic Aβ and hyperphosphorylated tau, major hallmarks of AD, in experimental rat and human retinas with elevated IOP, respectively, underscores the similarities between these two age-related neurodegenerative diseases at the molecular level. In addition to elevated IOP, decreased cerebrospinal fluid pressure, observed in a substantial proportion of patients with AD,28 results in an abnormal high trans-lamina cribrosa pressure difference and contributes to the development of glaucomatous damage to the optic nerve,29 suggesting a potential link between AD and OAG.
Another possible mechanism that links OAG to dementia is the severe vision loss and blindness caused by OAG in the elderly. Serious visual impairment, deprivation of an important structure critical for sensory input, is associated with limitations of the activities of daily living, and handicaps in physical and mental leisure activities, which may be helpful in enhancing the complexity of neuronal synapses, improving cognitive reserves, and eventually bringing about or aggravating cognitive impairment or dementia in older people.30, 31 In addition, as the disease progresses, older people with visual impairment due to glaucoma are significantly afflicted by substantial psychological suffering, a poor quality of life, and depression, which are potential risk factors for AD and dementia.32, 33, 34 It is worth noting that female but not male dementia patients were more likely to have prior OAG than controls in our study. This observation can partially be explained by the gender effect in the progression of visual impairment due to glaucoma, and the lines of evidence show that older women are at greater risk for glaucoma vision loss.35 The mechanisms behind this may be a decline in female sex hormones after menopause, which may influence the IOP, increase vascular resistance, and hamper ocular blood flow to the optic nerve. As glaucoma more rapidly deteriorates in aged women, they are at a higher risk for dementia than men. As women exceed men in rapidly growing dementia populations, further research is needed to clarify the role of gender effects on the relationship between glaucoma and dementia.
A particular strength of this study is the use of a nationwide population-based data set that provided a sufficient sample size and statistical power to explore the association between OAG and dementia. However, the findings of this study need to be interpreted in the context of the following limitations. First, OAG and dementia diagnoses, which rely on administrative claims data and ICD codes, may be less precise than those made according to standardized diagnostic procedures including ophthalmologic and neuropsychological examinations. To avoid miscoding and increase the diagnostic accuracy, we selected patients who had at least two consensus diagnoses of OAG or dementia, and only dementia cases who were diagnosed by a certified neurologist or psychiatrist or only OAG cases who received prescriptions for topical antiglaucoma medication were included in the study. In order to address the appropriateness of using the applied coding approach, sensitivity analyses were performed using different definitions. We thus selected all subjects (n=17 292) who had received at least one diagnosis of dementia in their ambulatory care claims. We found that although the association magnitude decreased, there was still a significant association between dementia and OAG (adjusted OR=1.37 95% CI=1.28–1.46). In addition, to preclude inaccurate medical claims, the NHI Bureau of Taiwan randomly samples a fixed percentage of claims data with review and scrutiny of chart records from every hospital, followed by heavy penalties if outlier practice or malpractice is discovered. In addition, several previous studies determined that the NHI Research Database is of acceptable quality to provide reasonable estimates for epidemiological studies of OAG and dementia.36, 37 Second, the administrative data set did not provide individual information such as the severity of the disease, dietary habits, or body mass index, which might potentially modify the relationship between OAG and dementia. Educational level that might impact both the risk of dementia and the recourse to care was further unavailable in our administrative data set. However, we adjusted for patient monthly income, urbanization level, and geographic location in the study to minimize the effect of sociodemographic characteristics. Third, previous population-based studies showed that approximately half of persons with glaucoma were undiagnosed.6 Therefore, subjects with undiagnosed OAG would have been categorized as non-OAG, and hence there is a possibility that diagnostic misclassification may have led to a spurious association between dementia and OAG. Similarly, underdiagnosis of dementia should be a concern.38 However, potential underdiagnosis and selection bias should be partly justified as the prevalence of dementia (3.9%, 12 147/307 672) and OAG (1.46%, 4489/307 672) during the study period (2005–2011) on population aged ≥45 years in our administrative claims, data were consistent with previous literature on the prevalence of dementia39 and OAG.40
Fourth, there may be surveillance bias as patients with OAG are more likely to have frequent outpatient clinic visits, which may lead to early detection of dementia. However, we have adjusted for the number of outpatient visits within 1 year prior to index date. In addition, we examined the association between dementia and prior urinary calculi where a biological association is implausible. We found that there was no significant relationship between dementia and prior urinary calculi. Therefore, surveillance bias may not be a major reason contributing to the association found in the present study. Fifth, the study population mainly consisted of people of Chinese ethnicity, and it is unclear whether the results can be generalized to other ethnic populations. Finally, the data set only allowed us to trace the medical utilization of sampled patients back to 1996. Therefore, we could not ensure that cases and controls had no OAG or dementia prior to 1996, and this could have compromised our findings.
Despite these limitations, our nationwide population-based study found that female dementia patients were associated with a higher proportion of prior OAG than control among ethnic Chinese in Taiwan. Further studies are needed to confirm the association found in the present study and clarify the causal relationship.

References
Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP . The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement 2013; 9: 63–75.
Kalaria RN, Maestre GE, Arizaga R, Friedland RP, Galasko D, Hall K et al. Alzheimer's disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol 2008; 7: 812–826.
Blennow K, de Leon MJ, Zetterberg H . Alzheimer's disease. Lancet 2006; 368: 387–403.
Foster PJ, Buhrmann R, Quigley HA, Johnson GJ . The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002; 86: 238–242.
Quigley HA . Glaucoma. Lancet 2011; 377: 1367–1377.
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90: 262–267.
Boland MV, Quigley HA . Risk factors and open-angle glaucoma: concepts and applications. J Glaucoma 2007; 16: 406–418.
Leske MC, Connell AM . Risk factors for open-angle glaucoma: the Barbados Eye study. Arch Ophthalmol 1995; 113: 918–924.
Klein BE, Klein R, Lee KE . Heritability of risk factors for primary open-angle glaucoma: the Beaver Dam Eye study. Invest Ophthalmol Vis Sci 2004; 45: 59–62.
Kipfer-Kauer A, McKinnon SJ, Frueh BE, Goldblum D . Distribution of amyloid precursor protein and amyloid-beta in ocular hypertensive C57BL/6 mouse eyes. Curr Eye Res 2010; 35: 828–834.
Yoneda S, Hara H, Hirata A, Fukushima M, Inomata Y, Tanihara H . Vitreous fluid levels of beta-amyloid((1–42)) and tau in patients with retinal diseases. Jpn J Ophthalmol 2005; 49: 106–108.
McKinnon SJ . Glaucoma: ocular Alzheimer’s disease? Front Biosci 2003; 8: s1140–s1156.
Bayer AU, Ferrari F, Erb C . High occurrence rate of glaucoma among patients with Alzheimer’s disease. Eur Neurol 2002; 47: 165–168.
Tamura H, Kawakami H, Kanamoto T, Kato T, Yokoyama T, Sasaki K et al. High frequency of open-angle glaucoma in Japanese patients with Alzheimer’s disease. J Neurol Sci 2006; 246: 79–83.
Kessing LV, Lopez AG, Andersen PK, Kessing SV . No increased risk of developing Alzheimer disease in patients with glaucoma. J Glaucoma 2007; 16: 47–51.
Ou Y, Grossman DS, Lee PP, Sloan FA . Glaucoma, Alzheimer’s disease and other dementia: a longitudinal analysis. Ophthalmic Epidemiol 2012; 19: 285–292.
Helmer C, Malet F, Rougier MB, Schweitzer C, Colin J, Delyfer MN et al. Is there a link between open-angle glaucoma and dementia?: the Three-City–Alienor cohort. Ann Neurol 2013; 74: 171–179.
Ekström C, Kilander L . Pseudoexfoliation and Alzheimer's disease: a population-based 30-year follow-up study. Acta Ophthalmol 2014; 92 (4): 355–358.
Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML . Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 2011; 20: 236–242.
Hsieh C-Y, Chen C-H, Li C-Y, Lai M-L . Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc 2013; 114 (3): 254–259.
Kivipelto M, Helkala EL, Laakso MP, Hänninen T, Hallikainen M, Alhainen K et al. Midlife vascular risk factors and Alzheimer's disease in later life: longitudinal, population based study. BMJ 2001; 322: 1447–1451.
Gorelick PB . Risk factors for vascular dementia and Alzheimer disease. Stroke 2004; 35: 2620–2622.
Mitchell P, Lee AJ, Rochtchina E, Wang JJ . Open-angle glaucoma and systemic hypertension: The Blue Mountains Eye Study. J Glaucoma 2004; 13: 319–326.
Leske MC . Ocular perfusion pressure and glaucoma: clinical trial and epidemiologic findings. Curr Opin Ophthalmol 2009; 20: 73–78.
Guo L, Salt TE, Luong V, Wood N, Cheung W, Maass A et al. Targeting amyloid-β in glaucoma treatment. Proc Natl Acad Sci USA 2007; 104: 13444–13449.
McKinnon SJ, Lehman DM, Kerrigan-Baumrind LA, Merges CA, Pease ME, Kerrigan DF et al. Caspase activation and amyloid precursor protein cleavage in rat ocular hypertension. Invest Ophthalmol Vis Sci 2002; 43: 1077–1087.
Gupta N, Fong J, Ang LC, Yucel YH . Retinal tau pathology in human glaucomas. Can J Ophthalmol 2008; 43: 53–60.
Silverberg G, Mayo M, Saul T, Fellmann J, McGuire D . Elevated cerebrospinal fluid pressure in patients with Alzheimer’s disease. Cerebrospinal Fluid Res 2006; 3: 7.
Berdahl JP, Allingham RR, Johnson DH . Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma. Ophthalmology 2008; 115: 763–768.
Laurin D, Verreault R, Lindsay J, MacPherson K, Rockwood K . Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch Neurol 2001; 58: 498–504.
Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, Kuslansky G et al. Leisure activities and the risk of dementia in the elderly. N Engl J Med 2003; 348: 2508–2516.
Skalicky S, Goldberg I . Depression and quality of life in patients with glaucoma: a cross-sectional analysis using the Geriatric Depression Scale-15, assessment of function related to vision, and the Glaucoma Quality of Life-15. J Glaucoma 2008; 17: 546–551.
Varma R, Lee PP, Goldberg I, Kotak S . An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol 2011; 152: 515–522.
Saczynski JS, Beiser A, Seshadri S, Auerbach S, Wolf PA, Au R . Depressive symptoms and risk of dementia: the Framingham Heart Study. Neurology 2010; 75: 35–41.
Vajaranant TS, Nayak S, Wilensky JT, Joslin CE . Gender and glaucoma: what we know and what we need to know. Curr Opin Ophthalmol 2010; 21: 91–99.
Chung SD, Hu CC, Ho JD, Keller JJ, Wang TJ, Lin HC . Open-angle glaucoma and the risk of erectile dysfunction: a population-based case-control study. Ophthalmology 2012; 119: 289–293.
Wang HK, Lin SH, Sung PS, Wu MH, Hung KW, Wang LC et al. Population based study on patients with traumatic brain injury suggests increased risk of dementia. J Neurol Neurosurg Psychiatry 2012; 83: 1080–1085.
Connolly A, Gaehl E, Martin H, Morris J, Purandare N . Underdiagnosis of dementia in primary care: variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Health 2011; 15 (8): 978–984.
Zhang ZX, Zahner GE, Romn GC, Liu J, Hong Z, Qu QM et al. Dementia subtypes in China: prevalence in Beijing, Xian, Shanghai, and Chengdu. Arch Neurol 2005; 62: 447–453.
Xu L, Chen JH, Li JJ, Luo L, Yang H, Zhang RX et al. [The prevalence and its screening methods of primary open angle glaucoma in defined population-based study of rural and urban in Beijing]. Zhonghua Yan Ke Za Zhi 2004; 40: 726–732.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chung, SD., Ho, JD., Chen, CH. et al. Dementia is associated with open-angle glaucoma: a population-based study. Eye 29, 1340–1346 (2015). https://doi.org/10.1038/eye.2015.120
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.120
This article is cited by
-
Prevalence of visual impairment in older people living with dementia and its impact: a scoping review
BMC Geriatrics (2023)
-
Frequency of coexistent eye diseases and cognitive impairment or dementia: a systematic review and meta-analysis
Eye (2023)
-
Cognitive evaluation of patients with glaucoma and its comparison with individuals with Alzheimer’s disease
International Ophthalmology (2018)