Abstract
Background
To investigate the changes in inner foveal contour after surgery for macular hole (MH) and its clinical implications.
Methods
This retrospective observational case series included 66 eyes from 66 patients who underwent surgery for MH. Notching of tissue was defined as an abrupt alteration in the inner contour of the parafoveal tissue based on postoperative optical coherence tomography (OCT) image. The distance between the parafoveal edges of the outer plexiform layer (OPL) was defined as the inter-OPL distance. The inter-OPL distance was divided into nasal, temporal, superior, and inferior lengths. The difference in the lengths of each direction between the early and late postoperative period was compared between directions with and without notching.
Results
The early and late postoperative examination was performed at 4.6±2.9 weeks and 6.2±0.6 months, respectively. Notching of tissue was noted in 54 eyes (81.8%). In 53 eyes with a measurable inter-OPL distance, the notching of tissue was noted in 45 eyes (84.9%) regardless of preoperative MH size. The mean amount of foveal tissue elongation that occurred during the designated period was 104.6±68.8 and 78.4±72.9 μm in the directions with and without the notching of tissue (P<0.001), respectively.
Conclusions
The changes in the inner foveal contour, including notching of tissue and elongation of foveal tissue, were noted in the majority of eyes after MH surgery. Notching of tissue on OCT image could be a clinical marker for the development of foveal tissue elongation after MH surgery.
Similar content being viewed by others
Introduction
With the advent of spectral domain optical coherence tomography (SD-OCT),which allows analysis of each retinal layer, the detailed recovery process of foveal microstructure after macular hole (MH) surgery has been elucidated. In addition to the well-known phenomenon, such as restoration of the external limiting membrane and the photoreceptor layer,1, 2, 3, 4, 5, 6 the elongation of foveal tissue has recently been reported.7 The degree of asymmetric elongation of foveal tissue after MH surgery was closely associated with metamorphopsia and found to have a negative influence on the recovery of postoperative visual function.7
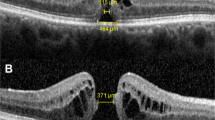
When analyzing postoperative OCT images after MH surgery, we often observed an abrupt alteration in the inner contour of the foveal tissue and a definite elongation of the foveal tissue in the direction that this phenomenon was noted (Figure 1, top). We termed this peculiar phenomenon as ‘notching’ of foveal tissue. We hypothesize that the notching of tissue is due to the re-distribution of parafoveal retinal tissue associated with the elongation of foveal tissue after MH surgery.
Optical coherence tomography images after macular hole surgery. Top: notching of tissue was defined as an abrupt alteration in the inner contour of the foveal tissue (arrow). When compared with the opposite direction, definite elongation of the ONL in the direction of notching was observed (top, arrowheads). The notching was usually observed between the OPL and the ONL. Upper middle: the distance between the edges of the OPL was defined as the inter-OPL distance. In this vertical section, inferior length (I) and superior length (S) indicate the distance from the inferior edge of the OPL to the center of the outer foveolar defect and the distance from superior edge of OPL to the outer foveolar defect, respectively. Lower middle: the angle of foveal tissue (α) was defined as the angle between an imaginary line parallel to the external limiting membrane (closed arrowhead) and a line connecting the innermost retinal region of the foveal center and the edge of OPL (open arrowhead). Bottom: the inner OPL area (A) was defined as the inner retinal area above the OPL within 500 μm of the edge of the OPL. The outer OPL area (B) was defined as the outer retinal area below the OPL to the level of the external limiting membrane with the same distance base.
The purpose of the present study was to investigate the changes in the inner foveal contour after MH surgery.
Materials and methods
This retrospective case series was performed at a single center and adhered to the tenets of the Declaration of Helsinki. The study was approved by the Institutional Review Board (IRB No.: 2011-12-072).
Medical records of consecutive patients who underwent surgery from September 2009 through March 2012 were reviewed. If a patient had a MH in both eyes, only one eye with prior surgery was included in this study. Patients with any of the following conditions in the studied eye were excluded: <6 months of follow-up, traumatic MH, evidence of ocular inflammation, diabetic retinopathy, hypertensive retinopathy, retinal vasculitis, media opacity that would influence visual acuity or preclude acquisition of clear SD-OCT images, −6.0 diopters or more of spherical equivalent, presence of staphyloma, history of intraocular surgery other than uncomplicated cataract surgery, or other ocular diseases that might influence macular microstructure or visual function.
Each patient underwent a complete preoperative evaluation, including an examination for best-corrected visual acuity (BCVA) either Snellen or ETDRS (Early Treatment Diabetic Retinopathy Study) score scale, anterior segment examination, and dilated fundus examination with a 90-diopter lens. Horizontal and vertical OCT scans through the fovea were performed with a combined confocal scanning laser ophthalmoscope and SD-OCT (Spectralis HRA+OCT, Heidelberg Engineering, Heidelberg, Germany). Snellen visual acuities were converted into ETDRS score using the previously recommended method7 for analysis.
A three-port standard pars plana vitrectomy was performed by a single surgeon (SWK) using either the Associate (Dutch Ophthalmic Research Center Inc., Zuidland, the Netherlands) or Accurus (Alcon Laboratories Inc., Fort Worth, TX, USA) 23-gauge vitrectomy system. The peeling of the internal limiting membrane (ILM), approximately 2-disc diameter area centered at the center of the MH, was conducted with or without the assistance of indocyanine green dye. This was followed by a complete fluid–gas exchange using 25% sulfur hexafluoride gas or 14% perfluoropropane gas. Perfluoropropane gas was usually used in case of large MH. Combined cataract surgery was performed in patients with visually significant cataracts or with incipient cataracts in subjects older than 60 years.
The first postoperative OCT scan was conducted at 1–3 weeks according to the intraocular gas status. Further, OCT scans were then conducted every 2–12 weeks based on the status of the eye until 6–8 months postoperatively.
The analyses of OCT images were conducted using the contained Heidelberg Eye Explorer software (version 1.5.12.0, Heidelberg Engineering). The MH size was calculated as the mean horizontal and vertical diameter. The distance between the edges of the outer plexiform layer (OPL) was measured and defined as the inter-OPL distance (Figure 1, upper middle). All the measurements for inter-OPL distance were performed by a single examiner (JHK).Notching of tissue was defined as an abrupt alteration in the inner contour of parafoveal tissue (Figure 1, top). The presence of notching of tissue was determined by an independent examiner (EJL) based on 1 : 1 pixel OCT images that were taken at 6–8 months postoperatively. The measurement of the inter-OPL distance was performed by another masked examiner (JHK) based on the 1 : 1 micron OCT images as conducted in our previous study.7 The retinal layers in which the notching of tissue was observed were determined on the basis of OCT images with 400–600% magnification by agreement of the two examiners (EJL and JHK).
Quantitative analysis included the eyes in which the inter-OPL distance was measurable from the early postoperative period. The inter-OPL distance at the first postoperative OCT scanning was compared with the inter-OPL distance at 6–8 months after surgery. The inter-OPL distance was divided into two sections on the basis of the center of the outer foveolar defect,8 which is usually present during the first few months in sealed MHs. If there was no outer foveolar defect, the thinnest foveal location was considered as the dividing point. The distance from the dividing point to the edge of the OPL was defined as the nasal length, temporal length, superior length, or inferior length according to the direction (Figure 1, upper middle). The difference in length between the first postoperative OCT and the OCT taken at postoperative 6-month follow-up was defined as Δ length. All the directions were divided into two groups according to the presence or absence of notching of tissue. The Δ length was compared between the directions in which the notching was noted and the directions in which the notching was not noted. To evaluate a possible association of notching or tissue elongation with the temporal thinning of the macula, the difference in postoperative (mean 6.2 months after surgery) thickness of the inner temporal or outer temporal ETDRS region between the eyes with and without temporal notching was measured. In addition, the correlation of Δ lengths to the temporal direction with the thickness of the inner or outer temporal regions was estimated.
Additional analysis was performed to determine the origin of notching of tissue. First, the angle of foveal tissue (α) was measured on the basis of the OCT images taken 6–8 months postoperatively. The angle between an imaginary line parallel to the external limiting membrane and a line connecting the innermost retinal region of the foveal center and the edge of the OPL was defined as the angle of foveal tissue (Figure 1, lower middle). The angle was compared between the directions with and without notching of tissue. The correlation between the angle and the Δ length was also estimated. Second, changes in the retinal area above and below the level of the edge of the OPL were estimated. The horizontal and vertical SD-OCT images were imported to Image J (National Institute of Health, Bethesda, MD, USA) software for analysis. The inner and outer OPL areas were defined as follows (Figure 1, bottom). The inner OPL area was defined as the inner retinal area at the level of the edge of the OPL, based on a horizontal distance of 500 μm, from the edge of the OPL. The outer OPL area was defined as the retinal area between the level of the edge of the OPL and the level of the external limiting membrane with the same horizontal base. The extents of the areas were measured using the polygon selection tool provided by the software. The difference in the area between the first postoperative OCT in which the inter-OPL distance was measurable, and the OCTs taken at the postoperative 6-month follow-up were compared within each group. In addition, the difference in area was compared between the directions with and without notching. Eyes were divided into two groups according to the presence or absence of notching. The difference in postoperative BCVA and postoperative change in BCVA were compared between the two groups.
Eyes in which the inter-OPL distance was not measurable due to an indistinct OPL edge in the OCT images taken before postoperative 6–8 months were included in the qualitative analysis group. In these eyes, the proportion of eyes and directions that exhibited notching of tissue was reported. In eyes with MHs >400 μm, analysis of serial postoperative OCT images was performed to elucidate the characteristics of the foveal microstructure with regard to notching of tissue.
The intra-observer repeatability and inter-observer variability for the measurement of horizontal inter-OPL distance, nasal length, inner OPL area, outer OPL area, and angle of foveal tissue were analyzed using an intraclass correlation coefficient (ICC). This analysis was based on the OCT images taken 6–7 months postoperatively. The ICC values for inner OPL area, outer OPL area, and the angle of foveal tissue in the nasal direction were analyzed.
Statistical analyses were performed using a commercially available software package (SPSS ver. 18.0 for Windows; SPSS Sciences, Chicago, IL, USA). Baseline characteristics of the qualitative and the quantitative analysis groups were compared using the independent sample t-test, the Mann–Whitney U-test, and Fisher’s exact test. Comparisons of visual acuity between eyes with and without notching were performed using independent sample t-test. Comparisons between the directions with and without notching of tissue were performed using the independent sample t-test. A comparison of the angle of foveal tissue between the directions with and without notching was performed using the independent sample t-test. The correlation between the angle and Δ length was analyzed using Pearson’s correlation analysis. Comparisons of numeric values within eyes were performed using paired t-tests. Comparison of the thickness of inner temporal or outer temporal region between the eyes with and without notching was performed using independent sample t-tests with a Bonferroni’s correction. The correlation of Δ lengths to the temporal direction with thickness of the inner or temporal region was estimated using Pearson’s correlation analysis with a Bonferroni’s correction. A P-value <0.05 was considered significant.
Results
A total of 87 consecutive eyes (58 eyes with MHs <400 μm and 29 eyes with MHs >400 μm) underwent MH surgery between the aforementioned periods. Among them, 66 eyes of 66 patients (44 eyes with MHs <400 μm and 22 eyes with MHs >400 μm) were ultimately included in the study (Table 1). Twenty-one eyes were excluded for the following reasons: follow-up period <6 months (17 eyes), unsealed hole after initial operation (3 eyes), and the development of postoperative retinal detachment (1 eye). During peeling of ILM, the borderline between the attached and the peeled ILM was carefully monitored, and a relatively accurate estimation of the extent of ILM peeling could be given in almost all the cases. The indocyanine green dye was used as surgical adjunctive in two eyes (3.0%) in which corneal edema developed during the surgery.
In all, 53 eyes (44 eyes (100%) with MHs <400 μm and 9 eyes (40.9%) with MHs >400 μm) were included in the quantitative analysis group. In these eyes, the mean age at the time of surgery was 63.2±6.2 years (mean±SD). The inter-OPL distance was compared between OCT images taken at mean times of 4.6±2.9 weeks and 6.2±0.6 months after surgery. The mean preoperative MH diameter was 308.7±149.0 μm with a horizontal diameter of 315.0±153.8 μm and a vertical diameter of 302.5±147.1 μm. The mean preoperative and postoperative BCVAs were 51.9±11.9 and 66.4±9.1 ETDRS letters, respectively. The remaining 13 eyes were included in the qualitative analysis group. In these eyes, the mean age at the time of surgery was 64.3±5.1 years. The mean preoperative MH diameter was 568.5±116.7 μm with a horizontal diameter of 584.5±116.7 μm and a vertical diameter of 552.2±117.9 μm. The mean preoperative and postoperative BCVAs were 42.3±11.9 and 57.7±11.4 ETDRS letters, respectively.
Notching of tissue was observed in 54 of 66 eyes (81.8%) and 121 of 264 directions (45.8%); the nasal direction in 42 eyes (63.6%), the temporal direction in 21 eyes (31.8%), the superior direction in 28 eyes (42.4%), and the inferior direction in 30 eyes (45.5%). The notching was first noted at a mean of 2.2±0.8 months (range, 1–4 months) after the surgery. Mean diameter of MH was 338.9±160.5 μm in eyes with notching and 437.4±213.5 μm in eyes without notching (P=0.063). The postoperative BCVA in the eyes with and without notching was 65.8±9.7 and 60.6±11.0 ETDRS letters, respectively (P=0.123). The change in BCVA in the eyes with and without notching was 15.9±9.3 and 15.0±8.9 letters, respectively (P=0.742).
In the quantitative analysis group, the horizontal and vertical inter-OPL distance at a mean of 4.6 weeks was 465.6±132.4 and 406.4±127.4 μm, respectively. The horizontal and vertical inter-OPL distances at a mean of 6.2 months were 578.0±123.8 and 492.2±113.1 μm, respectively. Elongation of the horizontal and vertical inter-OPL distance between the two time points was observed in 47 eyes (88.7%) and 49 eyes (92.4%), respectively. Both the horizontal and vertical inter-OPL distances were significantly greater in the measurements at a mean of 6.2 months than in the measurements at a mean of 4.6 weeks (P<0.001 and P<0.001, respectively). In the subgroup analysis of nine eyes with MHs >400 μm (mean MH size=567.1±123.8 μm), the horizontal and vertical inter-OPL distances at a mean 9.4±4.5 weeks were 553.4±161.4 and 481.4±538.6 μm, respectively. The horizontal and vertical inter-OPL distances at a mean 6.8±0.9 months after surgery were 639.0±159.2 and 538.6±130.7 μm, respectively. Elongation of the horizontal and vertical inter-OPL distance between the two time points was observed in seven eyes (77.8%) and eight eyes (88.9%), respectively. The vertical inter-OPL distance was significantly greater in the measurements at 6.8 months than in measurements at 9.4 weeks (P=0.042), whereas the horizontal inter-OPL distance between the two time points was not different (P=0.076).
The mean Δ lengths were 108.7±87.7, 77.9±75.8, 82.2±67.3, and 73.9±74.9 μm in the nasal, temporal, superior, and inferior directions, respectively. In this quantitative analysis group, the notching of tissue was observed in 45 of 53 eyes (84.9%) and 100 of 212 directions (47.2%); the nasal direction in 34 eyes (64.2%), the temporal direction in 18 eyes (33.9%), the superior direction in 23 eyes (43.4%), and the inferior direction in 25 eyes (47.2%). Notching of tissue was found to occur between the OPL and the outer nuclear layer (ONL). The mean Δ length was 104.6±68.8 and 78.4±72.9 μm in the directions with and without notching (Figure 2), respectively. The amount of elongation was significantly greater in the directions with notching than in the directions without notching (P=0.001). The mean angle of foveal tissue (α) was 10.8±3.1° and 13.9±4.8° in the directions with and without notching of tissue, respectively. The angle was significantly smaller in the directions with notching than in the directions without notching (P<0.001). In addition, there was a significant negative correlation between the angle and the Δ length (P<0.001, r=−294). An increase in the inner OPL area was noted in 163 (76.9%) directions, whereas a decrease in the inner OPL area was noted in 49 (23.1%) directions. An increase in the outer OPL area was noted in 104 (49.1%) directions, whereas a decrease in the outer OPL area was noted in 108 (50.9%) directions. In directions with notching of tissue, the inner and outer OPL areas were 0.044 and 0.062 mm2 on the first postoperative OCT, respectively. On the last postoperative OCT, the values were 0.053 and 0.062 mm2, respectively. The inner OPL area was significantly greater in the last postoperative OCT (P<0.001), whereas there was no difference in the outer OPL area (P=0.817). In the directions without notching of tissue, the inner and outer OPL areas were 0.041 and 0.060 mm2 on the first postoperative OCT, respectively. On the last postoperative OCT, the values were 0.047 and 0.061 mm2, respectively. The inner OPL area was significantly greater in the last postoperative OCT (P<0.001), whereas there was no difference in the outer OPL area (P=0.608). The increase in inner OPL area between 4.6 weeks and 6.2 months was significantly greater in directions with notching than in directions without notching (P=0.002), whereas there was no difference in the change of the outer OPL area between directions with and without notching (P=0.164).
A boxplot comparing the changes in the OPL distance from the foveal center(Δ length, top left), inner OPL area (Δ inner OPL area, bottom left), and outer OPL area(Δ outer OPL area, bottom right) in each direction between a mean of 4.6±2.9 weeks postoperatively and a mean of 6.2±0.6 months postoperatively. The angle of foveal tissue at a mean of 6.2±0.6 months postoperatively (top right) according to the presence of notching of tissue. Notching of the tissue was observed in 121 of 264 directions (45.8%). Positive values indicate increased length (postoperative elongation of foveal tissue), whereas negative values indicate decreased length. The central bars indicate median values, boxes indicate interquartile ranges, whiskers extend to the highest and lowest values, and excluded values extend beyond 3/2 of the interquartile range from the edge of the box. Open circles indicate values beyond this point.
In eyes with temporal notching, the thickness of the inner and the outer temporal regions were 317.2±15.9 and 285.9±13.7 μm, respectively. The values were 315.8±15.9 and 284.8±13.9 μm, respectively, in the eyes without temporal notching. There was no significant difference in the thickness of either the inner (P=1.000) or the outer (P=1.000) temporal region between the eyes with and without temporal notching. In addition, Δ lengths in the temporal direction were not correlated with the thickness of either the inner (P=0.884) or the outer (P=1.000) temporal region.
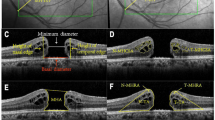
In the qualitative analysis group, notching of tissue was observed in 9 of 13 eyes (69.2%) and 21 of 52 directions (40.4%): the nasal direction in 8 eyes (69.2%), the temporal direction in 3 eyes (23.1%), the superior direction in 5 eyes (38.5%), and the inferior direction in 5 eyes (38.5%). All notching was also found to occur between the OPL and the ONL. Notching was not noted in directions in which the inner retinal layers were broadly stuck to the newly formed glial tissue (Figure 3).
Serial optical coherence tomography images showing the development of notching of tissue following macular hole surgery in eyes with a relatively large macular hole, with hole diameter of 751 μm (left column) and 606 μm (right column). Left column: the inner retinal layers in both directions are broadly connected to the newly formed glial tissue until 2 months postoperatively. The notching of tissue (arrow) was noted in the nasal direction at 6 months postoperatively. Right column: at postoperative 3 months, elongation of the foveal tissue was noted in the nasal direction (arrowheads) accompanied by early formation of notching of tissue (arrow). However, the inner retinal layers in the temporal directions are broadly connected to the newly formed glial tissue. At postoperative 6 months, definite elongation of the ONL and notching of tissue were observed in the nasal direction. Note that the notching developed between the outer plexiform layer and the ONL in both eyes.
Intra-observer and inter-observer ICC values of each measurement are as follows. Intra-observer repeatability: inter-OPL distance=0.963, nasal length=0.952, inner OPL area=0.917, outer OPL area=0.948, angle of foveal tissue=0.931. Inter-observer variability: inter-OPL distance=0.950, nasal length=0.938, inner OPL area=0.892, outer OPL area=0.916, angle of foveal tissue=0.883.
Discussion
In the present study, we revealed the changes in inner foveal contour after MH surgery in the majority eyes, including notching of tissue and elongation of foveal tissue. Methods of quantitative image analyses used in the present study showed relatively good intra-observer and inter-observer correlation. A greater amount of foveal tissue elongation occurred in the directions in which notching of tissue was noted than the directions in which the notching of tissue was not noted. This finding indicates that notching of tissue is a potential sign of foveal tissue elongation after MH surgery. Although the elongation of foveal tissue after MH surgery has been demonstrated, this result was derived from an analysis based on MHs <400 μm.7 In this study, we revealed that a similar phenomenon also occurs, at least in the vertical directions, in larger MHs. In a subgroup analysis of nine eyes with MHs >400 μm in which the elongation of the inter-OPL distance could be quantified, significant elongation of foveal tissue was noted after the surgery. Although quantitative analysis could not be performed in the remaining 13 eyes with large MHs, notching of tissue was found in the majority of these eyes. This suggests that postoperative elongation of foveal tissue is a universal phenomenon after surgery for MH, regardless of MH size. The horizontal elongation of inter-OPL distance was not verified in nine eyes with MHs >400 μm in the quantitative analysis group. However, this may be a result of the small sample size. Thus, this result requires confirmation by further studies with a larger study population.
Notching of tissue was observed between the OPL and the ONL. To elucidate the origin of notching of tissue, we analyzed the changes in the inner and outer retinal tissue configuration from the level of the notching. We found that the angle of foveal tissue was smaller in the directions with notching than in the directions without notching. This suggests that this relatively flat inner retinal contour close to the fovea emphasizes the abrupt alteration of the inner retinal contour at the location of the notching. One interesting finding was that the angle of foveal tissue had a negative association with Δ length. The angle was smaller in directions with greater postoperative foveal tissue elongation, suggesting that the elongation of foveal tissue accompanies the flattening of the central foveal tissue. In addition, we found a significant increase in the inner OPL area. This is probably caused by the thickening of the inner retinal layers after MH surgery. The amount of increase in the inner OPL area was almost 40% greater in directions with notching than in directions without notching. This suggests that the prominent postoperative increase in the area of the inner retinal layer and foveal tissue elongation are the causes of notching of tissue. In summary, both postoperative flattening of the inner retinal contour from the fovea to the edge of the OPL and thickening of the inner retinal layers to the edge of OPL may induce notching of tissue, which is characterized by the abrupt alteration of the inner retinal contour between the OPL and the ONL. Figure 4 illustrates the postulated mechanism for the development of notching of tissue.
An illustration showing the temporal change in the foveal contour after macular hole surgery, based on the results of the current study. Early postoperative (black line: mean 4.6 weeks after operation) and late postoperative (red line: mean 6.2 months after operation) retinal cross-sectional images are showing the difference in the postoperative changes of the inner retinal contour between directions with and without notching of tissue (red arrow). Although both postoperative elongation of foveal tissue (horizontal black arrow) and thickening of the inner retinal layer (vertical black arrow) were noted in both directions, the changes are more prominent in the direction with notching than in the direction without notching. Arrowheads indicate the edge of the OPL and the asterisk indicates the outer foveolar defect.
The fundamental cause for the phenomena that may lead to notching of tissue remains to be elucidated. We postulate that peeling of the ILM may be one of the possible causes. Although peeling of the ILM has been postulated to facilitate the closure of the MH by removing a possible source of contractile force,9, 10, 11 possible negative influence of ILM peeling has also been suggested.12, 13, 14 Alterations in the retinal microstructure and structural stability due to ILM peeling have been postulated as a reason for nasal displacement of retina after MH surgery with ILM peeling.15, 16, 17, 18 The changes in retinal microstructure found in our study may also be partially caused by an alteration in structural stability due to ILM peeling. The frequency of the notching of tissue as well as the amount of foveal tissue elongation were relatively greater in the nasal direction, suggesting these phenomena may have some association with nasal displacement of the retina, as was reported in previous studies. To confirm our hypothesis, further studies evaluating the association between postoperative retinal displacement with tissue notching in eyes with and without ILM peeling are required.
In a previous study, it was reported that the degree of asymmetric elongation of foveal tissue after MH surgery was closely associated with metamorphopsia.7 Because examination for metamorphopsia and BCVA was not routinely performed in the current retrospective analysis, the influence of the two origins of notching of tissue, flattening of the central foveal tissue and thickening of the parafoveal inner retinal layer, on visual function was not estimated. However, we postulate that tissue re-distribution due to these phenomena may have some negative influence on visual function. In particular, this may impede the recovery of visual function during the first several months after MH surgery and may be responsible for the limited recovery of visual function during the early postoperative period.19, 20, 21 In addition, we also postulate that this re-distribution of foveal tissue or attenuation of the central foveal tissue accompanied by the elongation of foveal tissue may have a negative effect on the anatomic stability of sealed MHs. This could be a potential cause of late re-opening of MH. Investigating the exact origin of postoperative elongation of foveal tissue or developing the methodology to prevent it is beyond the scope of the current study. Recently, an interesting phenomenon of macular migration toward the optic disc after ILM peeling for diabetic macular edema has been reported.6 Our results also indicate that the incidence of notching and elongation was highest in the nasal direction. A certain degree of change in macular topography after ILM peeling is suspected.
Previous studies have shown asymmetrical thickness in parafoveal retina after MH surgery with ILM peeling. In particular, thinning of the temporal retina is a characteristic finding.22, 23, 24, 25 Although previous studies did not clearly address the mechanism of this characteristic asymmetry, this finding is not noted in MH surgery without ILM peeling23 suggesting that ILM peeling has a role in this phenomenon. In the present study, the possible association of postoperative notching of tissue or foveal tissue elongation with temporal retinal thinning was evaluated. However, any significant association was not identified.
This study has several limitations. This study was a retrospective one. Thus, both the time of OCT examination and tamponade period after surgery were not controlled. Some of the conclusions were based on the qualitative analysis of OCT images. The horizontal elongation of inter-OPL distance was not significant in the nine eyes with MHs larger than 400 μm. However, this result may be due to the small sample size. Thus, this result requires confirmation by further studies with a larger study population. Although the notching of tissue was noted at a mean of 2.2±0.8 months after the surgery, results of this retrospective analysis may not accurately show the time at which the notching develops. Further studies with more frequent OCT examination will be needed to provide more information. Finally, this study was based on OCT images that were taken within 6–8 months after MH surgery suggesting that our findings may not reflect the long-term outcome.
In conclusion, changes in the inner foveal contour, including notching of tissue and elongation of foveal tissue were noted after MH surgery. Notching of tissue was found to be associated with foveal tissue elongation after MH surgery. Flattening of the inner retinal contour from the fovea to the location of the notching and thickening of the inner retinal layers outside the location of notching was postulated as the reason for notching. The presence of notching in the majority of eyes with large MHs suggests that postoperative elongation of foveal tissue occurs in both large and small MHs.

References
Bottoni F, De Angelis S, Luccarelli S, Cigada M, Staurenghi G . The dynamic healing process of idiopathic macular holes after surgical repair: a spectral-domain optical coherence tomography study. Invest Ophthalmol Vis Sci 2011; 52: 4439–4446.
Christensen UC, Kroyer K, Sander B, Larsen M, la Cour M . Prognostic significance of delayed structural recovery after macular hole surgery. Ophthalmology 2009; 116: 2430–2436.
Itoh Y, Inoue M, Rii T, Hiraoka T, Hirakata A . Significant correlation between visual acuity and recovery of foveal cone microstructures after macular hole surgery. Am J Ophthalmol 2012; 153: 111–119 e1.
Oh J, Smiddy WE, Flynn HW Jr, Gregori G, Lujan B . Photoreceptor inner/outer segment defect imaging by spectral domain OCT and visual prognosis after macular hole surgery. Invest Ophthalmol Vis Sci 2010; 51: 1651–1658.
Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y . Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 2010; 117: 1815–1824.
Landa G, Gentile RC, Garcia PM, Muldoon TO, Rosen RB . External limiting membrane and visual outcome in macular hole repair: spectral domain OCT analysis. Eye (Lond) 2012; 26: 61–69.
Kim JH, Kang SW, Park DY, Kim SJ, Ha HS . Asymmetric elongation of foveal tissue after macular hole surgery and its impact on metamorphopsia. Ophthalmology 2012; 119: 2133–2140.
Kang SW, Lim JW, Chung SE, Yi CH . Outer foveolar defect after surgery for idiopathic macular hole. Am J Ophthalmol 2010; 150: 551–557.
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J . Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology 1999; 106: 1392–1397.
Brooks HL Jr . Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 2000; 107: 1939–1948.
Lochhead J, Jones E, Chui D, Lake S, Karia N, Patel CK et al. Outcome of ICG-assisted ILM peel in macular hole surgery. Eye (Lond) 2004; 18: 804–808.
Smiddy WE, Feuer W, Cordahi G . Internal limiting membrane peeling in macular hole surgery. Ophthalmology 2001; 108: 1471–1476.
Ito Y, Terasaki H, Takahashi A, Yamakoshi T, Kondo M, Nakamura M . Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology 2005; 112: 1415–1420.
Baba T, Yamamoto S, Kimoto R, Oshitari T, Sato E . Reduction of thickness of ganglion cell complex after internal limiting membrane peeling during vitrectomy for idiopathic macular hole. Eye (Lond) 2012; 26: 1173–1180.
Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y . Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol 2014; 157: 971–977.
Kawano K, Ito Y, Kondo M, Ishikawa K, Kachi S, Ueno S et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye (Lond) 2013; 27: 871–877.
Nakagomi T, Goto T, Tateno Y, Oshiro T, Iijima H . Macular slippage after macular hole surgery with internal limiting membrane peeling. Curr Eye Res 2013; 38: 1255–1260.
Itoh Y, Inoue M, Rii T, Ando Y, Hirakata A . Asymmetrical recovery of cone outer segment tips line and foveal displacement after successful macular hole surgery. Invest Ophthalmol Vis Sci 2014; 55: 3003–3011.
Kumagai K, Furukawa M, Ogino N, Larson E, Uemura A . Long-term outcomes of macular hole surgery with triamcinolone acetonide-assisted internal limiting membrane peeling. Retina 2007; 27: 1249–1254.
Leonard RE 2nd, Smiddy WE, Flynn HW Jr, Feuer W . Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology 1997; 104: 1648–1652.
Baba T, Hagiwara A, Sato E, Arai M, Oshitari T, Yamamoto S . Comparison of vitrectomy with brilliant blue g or indocyanine green on retinal microstructure and function of eyes with macular hole. Ophthalmology 2012; 119: 2609–2615.
Kumagai K, Hangai M, Larson E, Ogino N . Progressive changes of regional macular thickness after macular hole surgery with internal limiting membrane peeling. Invest Ophthalmol Vis Sci 2013; 54: 4491–4497.
Kumagai K, Ogino N, Furukawa M, Hangai M, Kazama S, Nishigaki S et al. Retinal thickness after vitrectomy and internal limiting membrane peeling for macular hole and epiretinal membrane. Clin Ophthalmol 2012; 6: 679–688.
Ohta K, Sato A, Fukui E . Retinal thickness in eyes with idiopathic macular hole after vitrectomy with internal limiting membrane peeling. Graefes Arch Clin Exp Ophthalmol 2013; 251: 1273–1279.
Ohta K, Sato A, Fukui E . Asymmetrical thickness of parafoveal retina around surgically closed macular hole. Br J Ophthalmol 2010; 94: 1545–1546.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented at the Annual Meeting of the Association for Research in Vision and Ophthalmology, May 2013, Seattle, WA, USA.
Rights and permissions
About this article
Cite this article
Kim, J., Kang, S., Lee, E. et al. Temporal changes in foveal contour after macular hole surgery. Eye 28, 1355–1363 (2014). https://doi.org/10.1038/eye.2014.217
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.217
This article is cited by
-
Asymmetrical steepening of the foveal contour after macular hole surgery with internal limiting membrane peeling
Japanese Journal of Ophthalmology (2016)