Abstract
Purpose
To determine whether there is a displacement of the fovea toward the optic disc after successful macular hole (MH) surgery with internal limiting membrane (ILM) peeling.
Methods
The medical records of 54 eyes of 53 patients that had undergone pars plana vitrectomy with ILM peeling and gas or air tamponade for an idiopathic MH were evaluated. Spectral-domain optical coherence tomography (OCT) had been performed before and >6 months after the surgery. The preoperative distances between the center of the MH and the optic disc (MH-OD), center of the MH and the bifurcation or crossing of retinal vessels (MH-RV) were measured in the OCT images. In addition, the postoperative distance between the center of the fovea and optic disc (F-OD) and the center of the fovea and the same bifurcation or crossing of retinal vessels (F-RV) were measured in the OCT images.
Results
The F-OD was 2.67±0.33 disc diameters (DD), which was significantly shorter than that of the MH-OD of 2.77±0.33 DD (P<0.001). The F-RV was also significantly shorter than the MH-RV on the inner nasal area (from 0.85±0.16DD to 0.79±0.15DD; P<0.001), the inner temporal area (from 0.82±0.15DD to 0.77±0.14DD; P<0.001), and outer nasal area (from 1.70±0.31DD to 1.65±0.32DD; P<0.001), but it was significantly longer than the MH-RV in the outer temporal area (from 1.65±0.29DD to 1.68±0.29DD; P<0.001).
Conclusion
Our results showed that successful closure of a MH by vitrectomy with ILM peeling and gas tamponade leads to a displacement of the center of the macula toward the optic disc.
Similar content being viewed by others
Introduction
An idiopathic macular hole (MH) can be successfully closed by vitrectomy,1, 2, 3, 4, 5, 6 and the success rate is improved if the internal limiting membrane (ILM) is peeled during the vitrectomy.2, 3, 4, 5, 6 Although the mechanism causing the MH has been essentially determined,7, 8, 9, 10, 11, 12 the mechanism for the MH closure has not been definitively determined.
Yanagita et al13 reported that after a closure of a MH by vitrectomy, the retinal blood vessels near the MH are displaced toward the center of the fovea in all cases. They suggested that the retina around the MH moved toward the foveal pit after vitrectomy. On the other hand, we have noted that in many cases the retinal vessels in the macular area appeared to move toward the optic disc after vitrectomy that successfully closed a MH.
Thus, the purpose of this study was to test the hypothesis that the center of the macular area moves nasally toward the optic disc after successful closure of a MH by vitrectomy with ILM peeling.
Materials and methods
Study population
We reviewed the medical charts of 54 eyes of 53 patients who underwent successful vitrectomy for an idiopathic MH at the Nagoya University Hospital between October 2008 and May 2012. There were 33 women and 20 men. The mean±SD of the age was 65.3±6.0 years with a range of 54–78 years. There were 25 stage-2 MHs (46%), 12 stage-3 MHs (22%), and 17 stage-4 MHs (31%).7 All MHs were closed after a single surgery.
Eyes excluded from the statistical analyses were those with a reopening of the MH, with high myopia, or with a retinal detachment combined with the MH. Eyes with other macular diseases, such as age-related macular degeneration, were also excluded.
We also reviewed the charts of five eyes of five patients who had an idiopathic MH that closed spontaneously. The measurements made on these five eyes were identical to that of eyes that underwent vitrectomy.
The protocol for this study was approved by the institutional review board of the Nagoya University School of Medicine, and the procedures used conformed to the tenets of the Declaration of Helsinki.
Surgical techniques
A three-port pars plana vitrectomy with ILM peeling was carried out with 23- or 25-gauge instruments in all cases. All of the patients underwent combined cataract surgery except one patient who was pseudophakic. Triamcinolone acetonide was used for staining the ILM in all 54 eyes. The area of ILM peeling was symmetrical around the fovea and was about four disc diameters (DD). Sulfur hexafluoride (0.5–1.0 ml) gas was used in 38 eyes, perfluoropropane (0.5–0.8 ml) gas in 15 eyes, and simple fluid gas exchange without any gas injection was used in one eye as a tamponade. The patients were instructed to maintain a face-down position as much as possible until the closure of MHs was confirmed by OCT.
Examination and measurement procedures
All patients underwent a complete ophthalmic examination, including measurements of the best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, fundus examination, and optical coherence tomography (OCT; Cirrus OCT; Carl Zeiss Meditec, Dublin, CA, USA) before and 1–2 weeks, 1–3 months, and >6 months after the vitrectomy. Axial length was measured in all eyes preoperatively (IOL master, Carl Zeiss Meditec). The fovea was scanned with the 200 × 200 Macular Cube protocol of the Cirrus HD-OCT. OCT images were excluded if the eye moved during the scans.
The distance across the fundus was measured in the Cirrus OCT images.14 The Cirrus OCT instrument allows a direct registration of the OCT projection maps onto the infrared line scanning ophthalmoscopic image. The location of the center of the MH or postoperative foveola was determined by realigning the vertical and horizontal OCT scans in the analysis window manually (Figures 1a). In cases where the postoperative foveal pit was irregular, center of fovea was considered to be the thinnest part in the OCT image. In cases where the postoperative foveal pit was flat, the center of the fovea was considered to be the center of foveal pit.
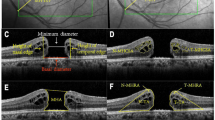
Diagrams of how the distances between center of MH or postoperative fovea and major landmarks are measured in the OCT images and infrared line scanning ophthalmoscope images. (a, b) Preoperative OCT images. (a) is an image obtained by a horizontal scan and (b) is a vertical scan in the raster map program of Cirrus OCT. Pink line in (a) indicates the location of the vertical scan (b). Blue line in (b) indicates the location of the horizontal scan (a). Center of MH can be easily identified by moving the location of scans (blue and pink lines) to the center of MH (white arrowheads). (c) Distance between the center of the macular hole and optic disc or bifurcation or crossing of retinal vessels were measured manually using the caliper function of the Cirrus OCT (yellow arrows). Vertical diameter of the optic disc was also measured similarly (blue arrow). The location of a bifurcation or crossing of retinal vessels were made in four areas of the macular area; inner nasal, inner temporal, outer nasal, and outer temporal area. The diameter of the ring is two and four DD (red circles). The vertical line running through fovea divided the retina into nasal and temporal halves (red vertical line). (d, e) Postoperative OCT images. (d) is an image obtained by a horizontal scan and (b) is a vertical scan in the raster map program of Cirrus OCT. Pink line in (d) indicates the location of the vertical scan (e). Blue line in (e) indicates the location of the horizontal scan (d). Center of fovea can be easily identified by moving the location of scans (blue and pink lines) to the center of fovea.
The preoperative distance between center of MH and optic disc (MH-OD) and the distance between center of the MH and a bifurcation or crossing of retina vessels (MH-RV) were measured in the Cirrus OCT images (Figure 1c). In the same way, the postoperative distance between the fovea and optic disc (F-OD), and the distance between the fovea and a bifurcation or crossing of retina vessels (F-RV) were measured in the Cirrus OCT images. Each distance was measured manually with the caliper function embedded in the OCT instrument. To compensate for variations in the magnification of each scan, each distance was divided by vertical diameter of the optic disc, and the distance was expressed in DD units.
The locations of the bifurcation or crossing of the retinal vessels were selected in four areas: the inner nasal area, the inner temporal area, the outer nasal area, and the outer temporal area (Figure 1c). The inner areas were within a circle of two DD centered on the fovea, and the outer area was between circles of two and four DDs centered on fovea. The margin between the nasal and temporal areas was a vertical line passing through the fovea. The movement of the macula in each area was analyzed separately.
Eyes with spontaneous closure of MH
The MHs of five eyes closed spontaneously, and both the pre-closure and post-closure OCT images were available. The measurements of the displacement were done identically to the eyes that underwent vitrectomy. The mean±SD age of these three women and two men was 65.6±6.7 years with a range of 56–73 years. There were two stage-2 MHs (40%) and three stage-3 MHs (60%).
Statistical analyses
The significance of the differences between the pre- and postoperative values was determined by paired t-tests, and single and stepwise regression analysis was used to determine the parameters that were significantly associated with the distance of movement of the fovea (PASW statistics version 18.0; SPSS Inc and IBM Company, Chicago, IL, USA). A P<0.05 was taken to be statistically significant.
Results
The pre- and postoperative OCT images of 36 eyes of 36 patients at 1–3 months and >6 months were of sufficient quality to be analyzed. The mean±SD preoperative MH-OD distance was 2.77±0.33 DD with a range of 2.08–3.47 DD. The mean postoperative F-OD distance was 2.67±0.32 DD with a range of 2.05–3.34 DD at 1–3 months, and 2.67±0.33 DD with a range of 2.03–3.37 DD at >6 months. The F-OD distance at 1–3 and >6 months after surgery were significantly shorter than the MH-OD by 3.3±2.0% and 3.6%±1.8%, respectively, (both P <0.001, paired t-tests).
The OCT images of 13 eyes that were recorded within 2 weeks after surgery and were good enough to be analyzed were available. In these 13 eyes, the average MH-OD distance was 2.61±0.16 DD, and the F-OD distance was 2.57±0.18 DD at 1–2 weeks, 2.54±0.16 DD at 1–3 months, and 2.53±0.16 DD at >6 months after the vitrectomy. The F-OD distance at 1–2 weeks, 1–3 months, and >6 months after surgery were significantly shorter than the MH-OD distance by 1.8%±1.5% (P=0.001, paired t-test), by 2.9±1.4% (P <0.001, paired t-test), and by 3.1%±1.5% (P <0.001, paired t-test; Figure 2a).
Graphs showing the degree of foveal movement toward optic disc. (a) Changes in the distance between the fovea and optic disc in eyes that had undergone surgery. The preoperative distance was between center of macular hole and optic disc. Postoperative distance was between fovea and optic disc. Macular retina moved significantly toward the optic disc after surgery. (b) Changes in the distance between the fovea and optic disc in eyes with a spontaneous closure. Distance was not significantly different, indicating that the macular retina did not move after the closure.
The mean±SD of the MH-RV distance in the inner nasal area for the 36 eyes was 0.85±0.16 DD preoperatively. The mean±SD of the F-RV distance in the inner nasal area was 0.80±0.16 DD at 1–3 months after surgery and 0.79±0.15 DD at >6 months after the vitrectomy. The F-RV distance in the inner nasal area were significantly shorter than the MH-RV distance by 6.6±4.4% (P<0.001, paired t-test) at 1–3 months and by 7.2%±4.1% (P<0.001, paired t-test) at 6 months after the vitrectomy (Figure 3).
Graphs showing the degree of movement of the macular retina. (a) Changes in the distance between the fovea and bifurcation or crossing of retinal vessels in the inner ring. Macular retina in inner ring moved significantly toward the fovea after surgery. (b) Changes in the distance between the fovea and bifurcation or crossing in the outer ring. The distance to the nasal outer areas decreased significantly after surgery. In contrast, the distance to the temporal outer area increased significantly after surgery. This is probably because fovea moved toward optic disc.
The mean±SD of the MH-RV distance in the inner temporal area was 0.82±0.15 DD preoperatively. The mean of the F-RV distance in the inner temporal area was 0.77±0.15 DD at 1–3 months after surgery and 0.77±0.14 DD at >6 months after the vitrectomy. The F-RV distance in the inner temporal area was significantly shorter than the MH-RV by 6.5±4.5% (P<0.001, paired t-test) at 1–3 months after surgery and by 6.5%±4.4% (P<0.001, paired t-test) at >6 months after surgery.
The mean±SD MH-RV distance in the outer nasal area was 1.70±0.31 DD preoperatively. The mean±SD F-RV distance in the outer nasal area was 1.65±0.31 DD at 1–3 months after surgery and 1.65±0.32 DD at >6 months after the vitrectomy. The R-RV distance in the outer nasal area were significantly shorter than the MH-RV distance by 2.8±2.9% (P<0.001, paired t-test) at 1–3 months and by 3.1±3.3% (P<0.001, paired t-test) at >6 months after the vitrectomy.
The mean±SD MH-RV distance in the outer temporal area was 1.65±0.29 DD preoperatively. The mean±SD F-RV distance in the outer temporal area was 1.67±0.29 DD at 1–3 months and 1.68±0.29 DD at >6 months after the vitrectomy. The F-RV in the outer temporal area was significantly longer than the MH-RV by 1.0±2.8% (P=0.006, paired t-test) at 1–3 months and by 1.8±3.0% (P<0.001, paired t-test) at >6 months after the vitrectomy.
The mean±SD diameter of the MHs was 693±318 μm with a range of 234–1778 μm or 0.42±0.20 DD with a range of 0.13–1.08 DD. The difference between the preoperative MH-OD and postoperative F-OD, that is, the movement of the fovea at >6 months after the vitrectomy, was greater than the radius of the MH in eight eyes (22.2%).
The mean BCVA was 0.68±0.23 logMAR units with a range of 0.3–1.2 logMAR units preoperatively and 0.29±0.24 logMAR units with a range of 0.0–1.0 logMAR units postoperatively.
Single and stepwise regression analysis showed that the diameter of the MHs, preoperative and postoperative BCVAs, improvements in the BCVA, age and axial length were not significantly associated with the difference between the MH-OD and F-OD distances (Table 1).
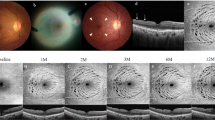
A representative case is shown in Figure 4. When the pre- and postoperative fundus images were overlapped, the movement of the retinal vessels in the center of macular area toward the optic disc could be clearly seen.
Representative case with a stage-2 MH in a 55-year-old man. This is a composite OCT image that was made by overlapping preoperative and postoperative images after changing to the gray scale. The black retinal vessels are the preoperative location of the retinal vessels, and white vessels are postoperative location. White ring shows the MH. White dot shows postoperative fovea. This image clearly shows that the macular retina has moved toward the optic disc.
Eyes with spontaneous closure
The mean±SD of the MH-OD distance while the MH was open was 3.05±0.37 DD, with a range of 2.71–3.64 DD. The mean±SD of the F-OD distance after a spontaneous closure of the MH was 3.04±0.41 DD, with a range of 2.69–3.70 DD at >6 months after the spontaneous closure (Figure 2b). The difference in the MH-OD and F-OD distances were not significant. The MH-RV and F-RV in the inner nasal area were 0.80±0.09 DD with a range of 0.66–0.90 DD and 0.81±0.10 DD with a range from 0.65 to −0.91 DD, respectively. MH-RV and F-RV distances in the inner temporal area were 0.72±0.10 DD with a range of 0.59–0.85 DD and 0.71±0.10 DD with a range of 0.58–0.84 DD, respectively. The MH-RV and F-RV distances in the outer nasal area were 1.72±0.17 DD with a range of 1.50–1.97 DD and 1.72±0.16 DD with a range of 1.52–0.96 DD, respectively. The MH-RV and F-RV distances in the outer temporal area were 1.63±0.23 DD with a range of 1.31–1.91 DD and 1.62±0.24 DD with a range of 1.31–1.93 DD, respectively. The differences in the MH-RV and F-RV distances were not significant in all four areas.
Discussion
Our results showed that the F-OD distance was significantly shorter than the MH-OD distance. This indicates that the center of the macular area moved toward the optic disc after vitrectomy with ILM peeling. There is a possibility that the MH closure caused this displacement. However, the MH-OD and F-OD distances were not different in eyes with a spontaneous closure of the MH. Therefore, the ILM peeling was most likely the cause of this movement. Under natural conditions, the traction of the ILM on the fovea from the temporal side may be stronger than that from nasal side because there is no ILM on the optic disc. We suggest that once the ILM is peeled, the balance may be altered, and the fovea is then displaced toward the optic disc. Further studies are needed to determine whether ILM peeling can cause the macular movement in other diseases after surgery with ILM peeling. A study analyzing eyes with diabetic macular edema treated by vitrectomy with ILM peeling is ongoing in our clinic.
There is a possibility that the MH may close asymmetrically around the center of the MH. However, the movement in eight eyes was larger than the radius of the MH. Therefore, the fovea most likely moved toward the optic disc after the surgery. This displacement of foveal area toward optic disc could be clearly seen in the images made by overlapping pre- and postoperative fundus images (Figure 4).
The average F-RV distance of the inner nasal and temporal area was significantly shorter than that of the MH-RV. This indicates that the retina around the MH moved toward the center of the MH after the MH was closed. In contrast, the F-RV distance in the outer temporal area was significantly greater than the MH-RF distance. The movement of the fovea toward the optic disc may cause this expansion.
A movement of the macular area was reported in eyes with an epiretinal membrane,14 in eyes after the removal of an epiretinal membrane,15 and in eyes after retinal detachment surgery.16 Macular translocation surgeries for myopic choroidal neovascularization and age-related macular degeneration have also been intentionally moved from the foveal area to other locations.17, 18, 19, 20, 21, 22, 23, 24 Thus, the macular retina is movable depending on the circumstances and can function on any retinal pigment epithelium.
Our single and stepwise regression analysis showed that the pre- and postoperative BCVAs and the improvements in the BCVA were not significantly associated with the degree of retinal movement. A significant relationship between the change in the position of the macular area and functional changes was not found in this study. In eyes with an epiretinal membrane, the extent of tractional foveal dystopia was found to be correlated with a decrease of the visual acuity.14 Further studies are needed to determine the relationship between the degree of displacement and any functional changes of the retina.
The nasal movement of the fovea may cause a pseudoesotropia. As we did not evaluate the eye position, we cannot state whether a change of eye position occurred. However, none of the patients complained of diplopia postoperatively, and none had an obvious pseudoesotropia. As the average distance of movements was 0.09 DD or about 0.4 degree or 0.7 prism diopters, it may be difficult to detect. Further studies are needed to determine whether changes in the eye position occurred postoperatively.
One of the limitations in this study is that cataract surgery may cause the change of the distance in the OCT image. However, we measured the distance with DD unit. Therefore, even if this change occurs, this change is compensated and the distance in the OCT image before and after the surgery can be compared.
In conclusion, we have shown that center of the macula is displaced toward the optic disc after vitrectomy for MH with ILM peeling. As all of the MHs were closed after the initial surgery, it is not known whether this movement contributes to the success of the surgery. Further studies are needed to investigate this phenomenon.

References
Kelly NE, Wendel RT . Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol 1991; 109: 654–659.
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J . Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology 1999; 106: 1392–1398.
Brooks HL Jr . Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 2000; 107: 1939–1949.
Kumagai K, Furukawa M, Ogino N, Uemura A, Demizu S, Larson E . Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina 2004; 24: 721–727.
Kadonosono K, Itoh N, Uchio E, Nakamura S, Ohno S . Staining of internal limiting membrane in macular hole surgery. Arch Ophthalmol 2000; 118: 1116–1118.
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T et al. Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling. Retina 2006; 26: 631–636.
Gass JD . Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol 1988; 106: 629–639.
Gass JD . Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 1995; 119: 752–759.
Gass JD . Müller cell cone, an overlooked part of the anatomy of the fovea centralis: hypotheses concerning its role in the pathogenesis of macular hole and foveomacualr retinoschisis. Arch Ophthalmol 1999; 117: 821–823.
Kishi S, Kamei Y, Shimizu K . Tractional elevation of Henle's fiber layer in idiopathic macular holes. Am J Ophthalmol 1995; 120: 486–496.
Kishi S, Hagimura N, Shimizu K . The role of the premacular liquefied pocket and premacular vitreous cortex in idiopathic macular hole development. Am J Ophthalmol 1996; 122: 622–628.
Ito Y, Terasaki H, Suzuki T, Kojima T, Mori M, Ishikawa K et al. Mapping posterior vitreous detachment by optical coherence tomography in eyes with idiopathic macular hole. Am J Ophthalmol 2003; 135: 351–355.
Yanagita T, Shimizu K, Fujimura F, Takano M . Fixation point after successful macular hole surgery with internal limiting membrane peeling. Ophthalmic Surg Lasers Imaging 2009; 40: 109–114.
Lo D, Heussen F, Ho HK, Narala R, Gasperini J, Bertoni B et al. Structural and functional implications of severe foveal dystopia in epiretinal membranes. Retina 2012; 32: 340–348.
Weinberger D, Stiebel-Kalish H, Priel E, Barash D, Axer-Siegel R, Yassur Y et al. Digital red-free photography for the evaluation of retinal blood vessel displacement in epiretinal membrane. Ophthalmology 1999; 106: 1380–1383.
Shiragami C, Shiraga F, Yamaji H, Fukuda K, Takagishi M, Morita M et al. Unintentional displacement of the retina after standard vitrectomy for rhegmatogenous retinal detachment. Ophthalmology 2010; 117: 86–92.
Machemer R, Steinhorst UH . Retinal separation, retinotomy, and macular relocation: I. experimental studies in the rabbit eye. Graefes Arch Clin Exp Ophthalmol 1993; 231: 629–634.
Machemer R, Steinhorst UH . Retinal separation, retinotomy, and macular relocation: II. a surgical approach for age-related macular degeneration? Graefes Arch Clin Exp Ophthalmol 1993; 231: 635–641.
Eckardt C, Eckardt U, Conrad HG . Macular rotation with and without counter-rotation of the globe in patients with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 1999; 237: 313–325.
Aisenbrey S, Lafaut BA, Szurman P, Grisanti S, Lüke C, Krott R et al. Macular translocation with 360 degree retinotomy for exudative age-related macular degeneration. Arch Ophthalmol 2002; 120: 451–459.
Terasaki H, Miyake Y, Suzuki T, Niwa T, Piao CH, Suzuki S et al. Change in full-field ERGs after macular translocation surgery with 360° retinotomy. Invest Ophthalmol Vis Sci 2002; 43: 452–457.
Terasaki H, Ishikawa K, Suzuki T, Nakamura M, Miyake K, Miyake Y et al. Morphologic and angiographic assessment of the macula after macular translocation surgery with 3601 retinotomy. Ophthalmology 2003; 110: 2403–2408.
Terasaki H, Ishikawa K, Niwa Y, Piao CH, Niwa T, Kondo M et al. Changes in focal macular ERGs after macular translocation surgery with 360 degrees retinotomy. Invest Ophthalmol Vis Sci 2004; 45: 567–573.
Takeuchi K, Kachi S, Iwata E, Ishikawa K, Terasaki H . Visual function 5 years or more after macular translocation surgery for myopic choroidal neovascularisation and age-related macular degeneration. Eye 2012; 26: 51–60.
Acknowledgements
This study was supported by the Grant-in Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (Dr Ito, C2159225).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Meeting Presentation: Parts of this study were presented at the Japanese Clinical Ophthalmological Society Meeting, October 2011, and the Japanese Ophthalmological Society Meeting, May 2012.
Rights and permissions
About this article
Cite this article
Kawano, K., Ito, Y., Kondo, M. et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye 27, 871–877 (2013). https://doi.org/10.1038/eye.2013.99
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.99
Keywords
This article is cited by
-
The impact of preoperative parameters on postoperative foveal displacement in idiopathic macular hole
Scientific Reports (2024)
-
Displacement of the retina and changes in the foveal avascular zone area after internal limiting membrane peeling for epiretinal membrane
Japanese Journal of Ophthalmology (2023)
-
Microstructural and hemodynamic changes in the fundus after pars plana vitrectomy for different vitreoretinal diseases
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Retinal displacement and intraretinal structural changes after idiopathic macular hole surgery
Japanese Journal of Ophthalmology (2022)
-
Ultrastructural study of closed macular hole- preliminary application of a novel high magnification module combining with OCT
BMC Ophthalmology (2021)