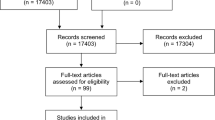
Abstract
Aims
To investigate a cluster of microsporidial keratoconjunctivitis in 33 eyes of 25 previously healthy paediatric and teenage individuals after a rugby match.
Methods
An observational case series was reported. Analysis of medical record of patients with microsporidial keratoconjunctivitis, who presented within May 2012, was performed. All patients were treated by a single ophthalmologist with a standardized topical regime, including a fluoroquinolone (moxifloxacin) and an antiseptic (Brolene or Desomedine). Five eyes received corneal scrapings.
Results
The mean age was 13.36 years (range 5–16). All patients have participated in a rugby match on 21–22 April 2012. The onset of symptoms ranged from 10 to 30 days post exposure. All eyes had multiple superficial coarse punctate keratitis. Four (12%) eyes presented with keratic precipitates. One (3%) eye had intraocular pressure of 27 mm Hg. Microscopic examination of corneal scrapings with modified trichrome or calcofluor white (CFW) fluorescent staining was unremarkable but subsequent PCR test was positive for the small subunit rRNA gene of Vittaforma corneae in three out of five eyes. Sequencing of the PCR product of 1150 bp showed 96–100% identity with the Indian or Singaporean strains of V. corneae. After treatment, all eyes healed without sequel.
Conclusions
The first outbreak of microsporidial keratoconjunctivitis in paediatric and teenage individuals with a rugby match is reported. A standardized topical regime, including a fluoroquinolone (moxifloxacin) and an antiseptic (Brolene or Desomedine), seems to be safe and effective, and requires validation in future treatment trials.
Similar content being viewed by others
Introduction
Microsporidia belong to a group of obligate intracellular parasite, which transmits via air or water by infective spores.1, 2 Three species of microsporidia are believed to cause most cases of the infection, namely Enterocytozoon bieneusi, Septata intestinalis and Encephalitozoon hellem.3 They infect the enterocytes of the small intestine and are associated with chronic diarrhoea.4 In human eyes, microsporidia are pathogens initially reported to cause opportunistic infection. It was first described in 1990, when three patients with acquired immunodeficiency syndrome presented with bilateral superficial epithelial keratitis.5 Two distinct clinical entities have emerged over the years: multifocal and superficial punctate epithelial keratopathy in immunocompromised patients such as AIDS,6, 7, 8, 9, 10, 11 and deep stromal corneal infection in immunocompetent patients.12, 13, 14, 15 Patients may develop other complications such as uveitis, corneal neovascularisation, necrosis, and perforation.
Risk factors for microsporidial keratoconjunctivitis include a history of contact-lens wearing, LASIK surgery, previous use of topical corticosteroid, trauma, or exposure to contaminated water or soil.14, 16, 17 The diagnosis can be made by detecting microsporidia in the corneal scraping using CFW, modified trichrome, or modified acid-fast stain.18 Electron microscopy is useful for definitive diagnosis. In addition, PCR is a sensitive way for organism detection, and subsequent sequencing of PCR products is used to identify particular microsporidial species.19, 20 The use of drugs namely albendazole, fumagillin, itraconazole, and propamidine isethionate has been associated with remission of microsporidial keratoconjunctivitis. However, it has been demonstrated to be less effective in stromal keratitis, in which corneal transplantation is usually required. Corticosteroids appear to be ineffective and may even worsen the disease.21, 22
In this case series, we report an outbreak of 33 eyes of 25 immunocompetent paediatric and teenage individuals who played rugby sport in Singapore. They all had the history of contact sport with soil exposure. The diagnosis has been confirmed by PCR for V. corneae. The possible associations of soil exposure with corneal microsporidial infection will be further discussed.
Materials and methods
This non-comparative observational case series was carried out in Hong Kong Sanatorium and Hospital. This study was reviewed and approved by the Institutional Review Board of the hospital. All the patients were treated and followed by one of the authors (AKHK). Patients with suspected microsporidial infection were evaluated based on medical history, symptoms, risk factors including exposure to contaminated water or soil, contact-lens wear, and steroid treatment before presentation. The clinical data such as age, sex, any injury during the rugby game, and the duration between exposures to the onset of symptoms were also obtained. Corneal scrapings were obtained from five patients and used for detection of microsporidia. Before attending our institution, treatment was non-standardized because they were previously treated by general practitioners, paediatricians or other eye specialists (Table 1). It included topical ciprofloxacin (Ciloxan), fusidic acid (Fucithalmic), chloramphenicol, tobramycin and dexamethsaone (Tobradex), moxifloxacin (Vigamox), ofloxacin (Tarivid), sofradex, evofloxacin and oral itraconazole (Sporanox), and mebendazole (Vermox). After evaluation in our hospital, all patients were started on topical moxifloxacin hydrochloride 0.5% (Vigamox) Q1H (day time), topical Brolene (propamidine isethionate 0.1%) or Desomedine (hexamidine isethionate 0.1%) Q1H (day time), and Tarivid ointment (ofloxacin 0.3%) nocte. The eye drops were instilled every 30 min alternating with each other. Oral albendazole 400 mg BD was continued for 2 weeks in two patients as requested by parents. This treatment regime was continued for 3 weeks and then gradually tapered according to individual patients’ response.
Laboratory diagnosis
Corneal scrapings were obtained from five patients after parental consent for the detection of microsporidia. After instillation of topical anaesthesia (0.5% proparacaine hydrochloride), superficial corneal scraping was done using sterile Kimura spatula with central cornea avoided under the slit lamp. Smearing and inoculation of various media was performed immediately at the eye clinic. The slides and media were then sent directly to the laboratory. The scraping was smeared on two glass slides and subjected to direct microscopic examination after staining with 10% potassium hydroxide with CFW (fluorescence microscopy), Gram, modified trichrome, and modified Ziehl Neelsen (1% H2SO4) stain. One scraping was plated on either blood or chocolate agar that was incubated at 37 °C for 2 weeks.
Nucleic acid extraction
DNA was extracted using EZ1 mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. The DNA was eluted in 60 μl of elution buffer and was used as the template for PCR.
PCR and DNA sequencing
Primer sequences23 used in this study are listed in Table 2.
The PCR mixture (25 μl) contained DNA, PCR buffer (10 mM Tris-HCl (pH 8.3), 50 mM KCl, 3 mM MgCl2, and 0.01% gelatin), 200 μM each deoxynucleoside triphosphates, and 1.0 U Taq polymerase (Applied Biosystems, Foster City, CA, USA). The mixtures were amplified in 60 cycles of 94 °C for 1 min, 55 °C for 1 min, and 72 °C for 1 min and a final extension at 72 °C for 10 min in an automated thermal cycler (Applied Biosystems). Standard precautions were taken to avoid PCR contamination, and no false-positive results were observed in negative controls. The PCR products were gel purified using the QIAquick gel extraction kit (Qiagen). Both strands of the PCR products were sequenced twice with an ABI Prism 3700 DNA analyzer (Applied Biosystems), using the PCR primers. The sequences of the PCR products were compared with known sequences by BLAST analysis against the NCBI database. PCR for adenovirus and enterovirus was performed.
Phylogenetic characterization
Phylogenetic tree was constructed by the neighbour-joining method using Kimura’s two-parameter correction with ClustalX 1.83. The 522 bp of amplicon from the small subunit rRNA (SSU rRNA) of V. corneae from the positive samples were included in the analysis using Trichodorus primitivus as the out-group.
Nucleotide sequence accession numbers
Nucleotide sequences of SSU rRNA gene obtained in this study have been lodged within the GenBank sequence database under accession numbers JX123131–JX123133.
Results
The rugby team played the game in Singapore, and the onset of symptoms ranged from 10 to 30 days post exposure. Twenty-five of them were seen in our hospital. They were referred either from general practitioners, paediatrician, other eye specialists, or self-referred. All were male and their age ranged from 5 to 16 years (mean age was 13.36 years). Initial symptoms included tearing (n=8; 32%), redness (n=22; 88%), grittiness (n=4; 16%), itchiness (n=6; 24%), blurring of vision (n=2; 8%), discharge (n=5; 20%), photophobia (n=2; 8%), and pain (n=3; 12%). Their past health was good, except five out of them had a history of either asthma or allergic rhinitis. None of them had concomitant symptoms of chronic diarrhoea. Predisposing factors related to trauma and the use of topical steroid was identified in 1 (4%) and 9 (36%) patients, respectively. Before tertiary referral, all (100%) and 9 (36%) patients were using topical antibiotics and oral anti-fungal/parasitic drug, respectively. The treatment before visiting our institution was not standardized owing to diverse referral source. There were four treatment regimens: (1) topical fluoroquinolone monotherapy (n=7; 28%) with ciprofloxacin 0.3%, levofloxacin 0.5%, or moxifloxacin 0.5%; (2) combinational therapy of topical fluoroquinolone together with topical steroid (n=4, 16%); (3) combinational therapy of oral itraconazole or mebendazole and topical fluoroquinolone (n=8; 32%); and (4) miscellaneous, including fuscidic acid, chloramphenicol, or tobramycin (n=7; 28%).
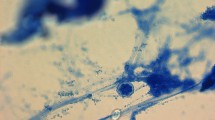
Eight (32%) patients had bilateral involvement. Nine (36%) and eight (32%) patients had involvements of the right and left eyes, respectively. Six (17%) eyes had lid swelling. Visual acuity at presentation ranged from 20/15− to 20/80. Six (17%) eyes had vision worse than 20/30−. All such eyes had central or diffuse corneal lesions. Slit-lamp biomicroscopy showed mild to severe non-purulent conjunctivitis in all patients. They were all mixed follicular and papillary in nature. The typical corneal patterns of multiple, coarse, small, punctate epithelial lesions, varying in number and locations, were noted (Figures 1a and b) in all eyes. In early stage, they presented with discrete white dots, which took up fluorescence stain in most, but not in all lesions. The patterns of corneal lesions were diffuse, central, and peripheral. Each group was present in 11 (33%) eyes. There were four (12%) eyes presented with small-to–medium-size non-pigmented keratic precipitates located over central-to-inferior cornea that subsided gradually after treatment. No topical steroid was given. No anterior chamber cell was observed. All eyes had normal intraocular pressure (IOP), except one (3%) that had initial IOP of 27 mm Hg, which was controlled with topical anti-glaucomatous drops that was discontinued after 2 weeks. No pre-auricular or cervical lymphadenopathy was found.
After treatment, the epithelial lesions gradually resolved with some evolving into a subepithelial nummular pattern with negative staining. Three (10%) patients developed increased bulbar conjunctival congestion, whereas one (3%) patient developed ciliary flush with limbitis 1 week after treatment. All subsided gradually after treatment. No topical steroid was given. All eyes gradually had finally vision of 20/20 or more. None of the patient required surgical intervention for complication.
Corneal scrapping had been performed in 5 (20%) out of 25 patients, depending on the consent of the patient and their parents. No bacteria or fungi were observed in all the smears and microbiological culture. The specimens of these five cases were subjected to specific microsporidial PCR tests for Encephalitozoon cuniculi, E. hellem, Encephalitozoon intestinalis, and E. bieneusi. They were all negative. However, specific PCR test for a 280-bp fragment of the SSU rRNA gene of V. corneae (a species of microsporidia) was positive in three out of five patients. A longer fragment of 1150 bp of this gene was amplified and sequenced (Figures 2a and b). Phylogenetic analysis of the sequences of the two different gene fragments confirmed that the three strains are V. corneae, which are 100% identical to the Indian strains of V. corneae for one fragment and 96–98% identical to the Singaporean strains for the other fragment (Figures 3a and b). Specific PCR for adenovirus and enterovirus was negative for all of our specimens.
(a) Photo of the gel electrophoresis showing the result of PCR assay for SSU rRNA of V. corneae with primer LPW20469 and LPW20470, giving a 1150-bp amplicon on three of the five corneal scrapings. Lanes: 1–3, patient 1–3: show positivity for V. corneae DNA; Lanes 4–5, patient 4 and 5: negative, showing no amplicon; Lane M, 100-bp plus marker; Lane NC, negative control. (b) Photo of the gel electrophoresis showing the result of PCR assay for SSU rRNA of V. corneae with primer LPW20475 and LPW20476 giving a 280-bp amplicon on three of the five corneal scrapings. Lanes: 1–3, patient 1–3: show positivity for V. corneae DNA; Lanes 4–5, patient 4 and 5: negative, showing no amplicon; Lane M, 100-bp plus marker; Lane NC, negative control.
(a) Phylogenetic tree of the 522-bp fragment of the SSU rRNA of V. corneae (only available fragment information in Indian strains) showing 100% nucleotide identity. (b) Phylogenetic tree of the 284-bp fragment of the SSU rRNA of V. corneae (only available fragment information in Singapore strains) showing 96–98% nucleotide identity.
Discussion
Microsporidial keratoconjunctivitis was first described in 1990, when three patients with acquired immunodeficiency syndrome presented with bilateral superficial epithelial keratitis.5 The reported prevalence of microsporidial keratitis was 0.4%, and it was considered to be a rare disease at that time.20 Since then, there has been an increasing awareness of such ocular infection both in immunocompromised and in immunocompetent patients.20 Recent report in Taiwan had suggested nine patients contracting the disease through in hot spring baths.17 In Singapore, Loh et al16 reported 124 cases of microsporidial keratitis. He found a strong correlation of soil/mud exposure in 62 cases (50%) from outdoor activities, including soccer, golf, and trail biking, especially after rainfall. Our case series is the first to report a cluster infection in rugby game.
Strong predisposition towards disease onset during the monsoon (70% of the case) has been reported.23, 24 Singapore, being situated in Southeast Asia, was generally hot with relative humidity in the range of 70–80%. It was affected by two main monsoon seasons: Northeast Monsoon Season (December–March) and the Southwest Monsoon Season (June–September). As the common environmental source of microsporidia included ditch water and other stagnant water bodies, three common species of microsporidia that infect humans have been detected in the water samples. 1, 2, 25 The cluster infection in our cases may be attributed to exposure to contaminated soil during the contact sport in this season. Although the outbreak of our cases occurs in April (not the usual peak season), there is evidence that there is higher than usual rainfall in April this year (2012) in Singapore (http://www.weather.gov.sg/wip/web/ASMC/Regional_Weather/Regional_Rainfall/Peninsular_Malaysia_Singapore). The relative superficial location of conjunctiva and corneal tissues suggested the direct inoculation of pathogens onto the eyes.21 We found out that other teams from Singapore, Malaysia, and so on also reported similar infections in their ruby players who played in the same field. In addition, all those infected did not stay in the same hotel. This highly suggested that the playing field was the source of infection.
None of the five corneal epithelial scrapings were positive for microsporidia by modified trichrome or CFW fluorescent staining. The possible explanations for the relatively low microbial load include the limited amount of specimen from corneal scrapping in the epithelial form of disease. Moreover, there is a significant lapse in time between the onsets of symptom to the taking of the corneal scrapings as many of them were initially dismissed as viral or bacterial illness. In addition, all cases were being partially treated with topical fluoroquinolone by general practitioner or other doctors elsewhere. In addition, the young age of the patients with tearing and strong light sensitivity did not allow a thorough corneal scrapping process. Nonetheless, PCR allowed the identification of microsporidia in the subspecies level.19, 26 Recently a study showed that 11.4% of patients with microsporidial keratoconjunctivitis have concomitant adenoviral infection.27 Specific PCR for adenovirus and enterovirus is negative for all of our specimens.
Currently, there are no defined guidelines for the treatment of ocular microsporidial infections. Epithelial debridement alone therapeutically debulked the infective organism from the corneal epithelium, but may increase the risk of penetration of pathogens into the deep stromal layers, further exacerbating the infection. Anecdotal reports of specific drug treatment included itraconazole, albendazole, benzimidazole, and fumagillin, but it lacked standardization of treatment. One of the problems might be the heterogeneous stage of the disease, with some patients with epithelial and others with stromal keratitis. The strength of our study includes all eyes with epithelial disease of similar stage, as well as all eyes were treated by a single eye specialist with a standardized topical regime, which included a fluoroquinolone (moxifloxacin) and an antiseptic (Brolene or Desomedine). This treatment regime seems to be safe and effective, and requires validation in future randomized, controlled treatment trials.
In our series, four patients (16%) received prior steroid prescribed by general practitioner or eye specialist, with no or a short period of improvement in symptoms. The steroid treatment may contribute to worsening of conditions and persistence of infection. Fortunately, we do not observe any adverse outcome in these four patients, probably related to the short duration of steroid use, as well as our prompt effective anti-parasitic treatment. Steroid treatment can also create a localized immunosuppressed state, similar to that proposed by Chan et al.22 He previously reported spontaneous resolution of keratitis within 2 weeks upon discontinuation of topical steroid, suggesting that immunocompetent host regained the local immune system to fight against the infection. However, it is unethical to observe the natural course of infection without treatment in this potentially blinding disease. It is therefore prudent to perform future study, to compare the efficacy of various treatment regimens against the one proposed by us.
In our series, there were four (12%) eyes presented with small-to-medium-size non-pigmented keratic precipitates located over central-to-inferior cornea that subsided gradually after treatment. No topical steroid was given. Three (10%) patients developed increased bulbar conjunctival congestion, whereas one (3%) patient developed ciliary flush with limbitis 1 week after treatment. Similarly, all subsided gradually after treatment with no topical steroid given. We suggest that these phenomenon are related to host immune response in fighting against the parasite and do not lead to adverse outcome. Although steroid eye drop may help to alleviate these signs and symptoms, it may lead to persistence of infection and worsening of conditions in the long run. We are reluctant to treat these eyes with topical steroid, especially in the early stage; however, other group treated such with topical steroid with no sequel reported.16
In summary, this study reports a series of microsporidial keratoconjunctivitis in paediatric and teenage healthy individuals with cluster infection, after mud exposure in ruby game. A standardized topical regime that included a fluoroquinolone (moxifloxacin) and an antiseptic (Brolene or Desomedine) seems to be safe and effective, and requires validation in future treatment trials.

References
Dowd SE, Gerba CP, Pepper IL . Confirmation of the human-pathogenic microsporidia Enterocytozoon bieneusi, Encephalitozoon intestinalis, and Vittaforma corneae in water. Appl Environ Microbiol 1998; 64 (9)p 3332–3335.
Sparfel JM, Sarfati C, Liguory O, Caroff B, Dumoutier N, Gueglio B et al. Detection of microsporidia and identification of Enterocytozoon bieneusi in surface water by filtration followed by specific PCR. J Eukaryot Microbiol 1997; 44 (6): 78S.
Curry A, Canning EU . Human microsporidiosis. J Infect 1993; 27 (3): 229–236.
Dascomb K, Clark R, Aberg J, Pulvirenti J, Hewitt RG, Kissinger P et al. Natural history of intestinal microsporidiosis among patients infected with human immunodeficiency virus. J Clin Microbiol 1999; 37 (10): 3421–3422.
Friedberg DN, Stenson SM, Orenstein JM, Tierno PM, Charles NC . Microsporidial keratoconjunctivitis in acquired immunodeficiency syndrome. Arch Ophthalmol 1990; 108 (4): 504–508.
Kersten A, Althaus C, Seitz HM, Pfahl HG, Sundmacher R . Bilateral microsporidial keratitis in an HIV-positive patient with AIDS stage infection. Klin Monbl Augenheilkd 1998; 212 (6): 476–479.
Martins SA, Muccioli C, Belfort R Jr, Castelo A . Resolution of microsporidial keratoconjunctivitis in an AIDS patient treated with highly active antiretroviral therapy. Am J Ophthalmol 2001; 131 (3): 378–379.
Garvey MJ, Ambrose PG, Ulmer JL . Topical fumagillin in the treatment of microsporidial keratoconjunctivitis in AIDS. Ann Pharmacother 1995; 29 (9): 872–874.
Rosberger DF, Serdarevic ON, Erlandson RA, Bryan RT, Schwartz DA, Visvesvara GS et al. Successful treatment of microsporidial keratoconjunctivitis with topical fumagillin in a patient with AIDS. Cornea 1993; 12 (3): 261–265.
McCluskey PJ, Goonan PV, Marriott DJ, Field AS . Microsporidial keratoconjunctivitis in AIDS. Eye (Lond) 1993; 7 (Pt 1): 80–83.
Metcalfe TW, Doran RM, Rowlands PL, Curry A, Lacey CJ . Microsporidial keratoconjunctivitis in a patient with AIDS. Br J Ophthalmol 1992; 76 (3): 177–178.
Weber R, Bryan RT . Microsporidial infections in immunodeficient and immunocompetent patients. Clin Infect Dis 1994; 19 (3): 517–521.
Curry A . Human microsporidial infection and possible animal sources. Curr Opin Infect Dis 1999; 12 (5): 473–480.
Theng J, Chan C, Ling ML, Tan D . Microsporidial keratoconjunctivitis in a healthy contact lens wearer without human immunodeficiency virus infection. Ophthalmology 2001; 108 (5): 976–978.
Silverstein BE, Cunningham ET Jr, Margolis TP, Cevallos V, Wong IG . Microsporidial keratoconjunctivitis in a patient without human immunodeficiency virus infection. Am J Ophthalmol 1997; 124 (3): 395–396.
Loh RS, Chan CM, Ti SE, Lim L, Chan KS, Tan DT . Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and management. Ophthalmology 2009; 116 (12): 2348–2353.
Fan NW, Wu CC, Chen TL, Yu WK, Chen CP, Lee SM et al. Microsporidial keratitis in patients with hot springs exposure. J Clin Microbiol 2012; 50 (2): 414–418.
Didier ES, Orenstein JM, Aldras A, Bertucci D, Rogers LB, Janney FA . Comparison of three staining methods for detecting microsporidia in fluids. J Clin Microbiol 1995; 33 (12): 3138–3145.
Joseph J, Sharma S, Murthy SI, Krishna PV, Garg P, Nutheti R et al. Microsporidial keratitis in India: 16S rRNA gene-based PCR assay for diagnosis and species identification of microsporidia in clinical samples. Invest Ophthalmol Vis Sci 2006; 47 (10): 4468–4473.
Joseph J, Sridhar MS, Murthy S, Sharma S . Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Ophthalmology 2006; 113 (4): 531–537.
Joseph J, Vemuganti GK, Sharma S . Microsporidia: emerging ocular pathogens. Indian J Med Microbiol 2005; 23 (2): 80–91.
Chan CM, Theng JT, Li L, Tan DT . Microsporidial keratoconjunctivitis in healthy individuals: a case series. Ophthalmology 2003; 110 (7): 1420–1425.
Raynaud L, Delbac F, Broussolle V, Rabodonirina M, Girault V, Wallon M et al. Identification of Encephalitozoon intestinalis in travelers with chronic diarrhea by specific PCR amplification. J Clin Microbiol 1998; 36: 37–40.
Reddy AK, Balne PK, Garg P, Krishnaiah S . Is microsporidial keratitis a seasonal infection in India? Clin Microbiol Infect 2011; 17 (7): 1114–1116.
Sironi M, Bandi C, Novati S, Scaglia M . A PCR-RFLP method for the detection and species identification of human microsporidia. Parassitologia 1997; 39 (4): 437–439.
Didier ES, Rogers LB, Brush AD, Wong S, Traina-Dorge V, Bertucci D . Diagnosis of disseminated microsporidian Encephalitozoon hellem infection by PCR-Southern analysis and successful treatment with albendazole and fumagillin. J Clin Microbiol 1996; 34 (4): 947–952.
Das S, Sharma S, Sahu SK, Nayak SS, Kar S . Diagnosis, clinical features and treatment outcome of microsporidial keratoconjunctivitis. Br J Ophthalmol 2012; 96 (6): 793–795.
Acknowledgements
This work was partly supported by the Hugh Guy Chan Education Fund of the Hong Kong Sanatorium and Hospital, as well as the Hui Ming and Hui Hoi sequencing platform, the Carol Yu Centre for Infection and the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Disease for Department of Health of the Hong Kong Special Administrative Region of China. We thank the clinical and technical staff of the Department of Microbiology, especially Dr. Rosanna Poon, at the Queen Mary Hospital for their kind support. Special thanks to Dr. Au Eong Kah Guan, Singapore, for the sharing of knowledge of microsporidiasis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kwok, A., Tong, J., Tang, B. et al. Outbreak of microsporidial keratoconjunctivitis with rugby sport due to soil exposure. Eye 27, 747–754 (2013). https://doi.org/10.1038/eye.2013.55
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.55
Keywords
This article is cited by
-
Microsporidial keratoconjunctivitis – first outbreak in Japan
BMC Infectious Diseases (2023)
-
A Narrative Review of Microsporidial Infections of the Cornea
Ophthalmology and Therapy (2020)
-
Microsporidial keratitis retrospectively diagnosed by ultrastructural study of formalin-fixed paraffin-embedded corneal tissue: a case report
Annals of Clinical Microbiology and Antimicrobials (2019)