Abstract
Purpose
To identify factors associated with visual outcomes in patients with diabetic macular edema (DME) treated with ranibizumab (RBZ) in the Ranibizumab for Edema of the mAcula in Diabetes—Protocol 2 (READ-2) Study.
Patients and methods
Optical coherence tomography scans, fundus photographs, and fluorescein angiograms (FAs) were graded and along with baseline characteristics were correlated with month (M) 24 visual outcome of best-corrected visual acuity (BCVA) ≤20/100 (poor outcome) vs >20/100 (better outcome).
Results
Of 101 patients with a M20 visit or beyond, 27 (27%) had BCVA ≤20/100. Comparison of patients with or without poor outcome showed mean baseline BCVA of 16.8 letters (20/125) in the former compared with 30.4 letters (20/63; P<0.001). Mean change in BCVA between baseline and M24 was −2.6 letters in the poor outcome group compared with +9.8 letters (P<0.001). Foveal thickness (FTH) at M24 was 374.1 μm in the poor outcome group compared with 268.8 μm (P<0.01), a difference driven by 14 patients with mean FTH of 450.3 μm. Foveal atrophy occurred in 65% (11/17) in the poor outcome group compared with 17%(12/71, P=0.001). Persistent edema was noted in 52% (14/27) of patients with poor outcome. Laser scars near foveal center were significantly more common in patients with poor outcome who did not have edema vs those who did (78% (7/9) vs 23% (3/13) P=0.03).
Conclusion
Poor baseline BCVA (≤20/125) in DME patients predicts poor visual outcome (≤20/100) after 2 years of treatment with RBZ and/or focal/grid laser, often due to foveal atrophy and/or persistent edema.
Similar content being viewed by others
Introduction
Diabetic retinopathy is a prevalent cause of reduced vision, mostly due to diabetic macular edema (DME).1 Although the pathogenesis of DME is not completely understood, recent studies have demonstrated that vascular endothelial growth factor (VEGF) has a major role.2, 3 The first study to clearly implicate VEGF was the Ranibizumab for Edema of the mAcula in Diabetes (READ) trial, which demonstrated a mean improvement in best-corrected visual acuity (BCVA) of 12.3 letters in patients with chronic DME given five intraocular injections of 0.5 mg of ranibizumab (RBZ) over the course of 7 months.2 This led to the READ-2 study, in which patients with DME were randomized to receive intraocular injections of RBZ (RBZ group), focal/grid laser (laser group), or a combination of RBZ and focal/grid laser (RBZ+laser group). At the month (M) 6 primary end point, RBZ patients who were treated with intraocular injections of 0.5 mg of RBZ at baseline and months 1, 3, and 5 showed a mean improvement in BCVA of 7.2 letters compared with −0.4 letters in the laser group (P=0.01), whereas RBZ+laser patients had a mean improvement of 3.8 letters (P=0.08).3 After the primary end point, patients in the RBZ group were seen every 2 months and if foveal thickness (FTH, center subfield thickness) was 250 μm or greater, with time domain optical coherence tomography (OCT), they were treated with 0.5 mg RBZ. Patients in the laser group were seen every 2 months and if FTH was 250 μm or greater, they could be treated with laser or RBZ. Patients in RBZ+laser group were seen every 3 months and if FTH was 250 μm or greater, they could receive laser plus RBZ or RBZ alone. At M24, the mean improvement in BCVA letters was 7.7, 5.1, and 6.8 in RBZ, laser, and RBZ+laser groups.4 Some patients had an outstanding outcome, with 45, 44, and 35% of patients having a M24 BCVA ≥20/40, whereas others fared less well. In this study, we sought to determine why some patients in the READ-2 study had a suboptimal visual outcome.
Materials and methods
The design and protocol of the READ-2 study have been described in detail elsewhere3, 4 and are summarized here. After the primary end point at M6, patients and investigators had the option to switch to RBZ only treatment. Consequently, during the 18-month follow-up period, patients in all three groups were mostly treated with RBZ alone. Patients were divided based upon visual outcome at M24 into poor visual outcome (≤20/100) vs better visual outcome (>20/100). Patients in the poor visual outcome group were further divided into two groups based on presence (poor vision/edema) or absence (poor vision/no edema) of edema contributing to poor BCVA. Edema was judged to be contributing to poor vision if there was foveal thickening at M24, and during months 12–24 there was a correlation between reduced FTH and improved BCVA. Patients were included in the analysis if they had completed 20–24 months of the READ-2 study, and M24 data were used when available. If a patient did not have the M24 study visit, but had a study visit at M20 or beyond, the last observation was carried forward. If fundus photography and fluorescein angiography (FA) images from M24 were not available, images from M12 were used for analysis as long as no laser treatment was administered between months 12 and 24. Data regarding demographics, baseline characteristics, BCVA, presence of edema, FTH, treatment received during the study, and grading of fundus photographs and FA images were analyzed and compared among groups. Fundus photography and FAs were analyzed at the Wilmer Retinal Imaging Research and Reading Center (RIRRC) for the presence of the following characteristics: evidence of extensive laser treatment, foveal atrophy, laser within 1 mm of the fovea, pigment changes within 1 mm of the fovea, and severe macular ischemia. Information regarding duration of macular edema was obtained from patient charts in which macular edema was first documented as a finding on exam or ophthalmic imaging. FTH of the central 1 mm of the macula was measured using Stratus Optical Coherence Tomography, scans were reviewed at the RIRRC and the thickness values were used for analysis. Images were received electronically from all sites via a central database. Images acquired from different cameras were resized to have uniform dimensions across images, an ETDRS grid was overlaid, the area of the macula covered by laser scars was measured using the software Image J (National Institutes of Health, Bethesda, MD, USA; available at http://rsbweb.nih.gov) and expressed as a percentage of the total area covered by the ETDRS grid. Patients were considered to have evidence of extensive laser treatment if more than 20% of the macula had laser scars or if patients had a history of having received laser treatment with more than 200 burns before being enrolled in the study. Laser scars were further assessed to look for presence in the central 1 mm of the ETDRS grid to determine whether laser treatment closer to the fovea was associated with poor visual outcomes. Severe macular ischemia was considered to be present if there was closure of perifoveal capillaries for 360° extending at least 1 mm from the fovea. Foveal atrophy was judged from the presence of window defect on FA and retinal thinning on OCT images. If hyper- or hypopigmentary changes were identified on color FP in the central 1 mm of the macula, the patient was judged to have pigmentary changes.
Statistical Package for the Social Sciences version 19 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. For the purposes of analysis, fundus photo and FA characteristics that could not be graded were considered as missing values. The independent samples t-test was used for parametric variables, and the Wilcoxon Signed-Rank test was used for non-parametric variables. Differences in proportion among categorical variables were determined using Pearson’s χ2 and Fisher’s exact test. Variables that had a P-value of <0.05 upon univariate analysis were selected for the multivariate model. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
The M24 disposition, visual outcome, and anatomic outcome of patients in the READ-2 study have been previously published.4 Of the 126 patients originally enrolled in the study, 101 had a study visit at M20 or beyond and are included in the analysis. Two patients had reduced vision at M24 owing to disease processes unrelated to DME or its treatment: one had vitreous hemorrhage and the other had a retinal vein occlusion. Fundus photographs and FAs were available for 95 of the remaining 99 patients and were analyzed. At M24, 27 (27%) had BCVA ≤20/100 and were classified as having poor visual outcome. Of the patients who had a better visual outcome, 42 (57%) had BCVA≥20/40. The characteristics of patients with a poor visual outcome were compared with those of the 74 (73%) patients who had a better visual outcome.
Effect of baseline characteristics and original treatment assignment on visual outcome
The baseline characteristics of the groups are shown in Table 1. There were no significant differences in duration of DME, age, or race. The percentage of female patients was greater (P=0.03 by univariate analysis) in the poor visual outcome (59%) vs the better outcome group (35%). The mean BCVA at baseline was 16.8 letters (20/125) in the poor outcome group vs 30.4 letters (20/63) in the better outcome group (P<0.001 by univariate and 0.001 by multivariate analyses).
The major differences in treatment occurred in the first 6 months of the trial and at the M6 primary end point, improvement from baseline BCVA was significantly greater in the RBZ group compared with the focal/grid laser group.3 After M6, RBZ was available to all patients as frequently as every 2 months if FTH was 250 μm or greater, and at M24 there was no longer any difference in visual outcome among the three treatment groups.4
Effect of treatment on visual outcome and course throughout trial
The mean number of RBZ injections through M24 (6.9 vs 5.9, P=0.27) and the mean number of focal/grid laser treatments administered before and during the study (3.0 vs 2.7, P=0.59) were not significantly different in the poor vs better outcome group (Table 2). The peak BCVA recorded for all study visits provides an assessment of visual potential. The mean peak BCVA was 28.4 letters (20/63) in poor visual outcome group vs 44 letters (20/32) in the better outcome group (P<0.001). The difference between baseline and peak BCVA was not significantly different in the poor (11.7 letters) vs better outcome group 13.6 (P=0.28). Patients in the poor visual outcome group did not maintain BCVA at peak and on average lost 2.6 letters compared with a gain of 9.8 letters in the better outcome group (P<0.001). The average time point in the study at which maximum improvement in VA occurred was significantly earlier in the poor vs the better visual outcome group (12 vs 17 months; P=0.002).
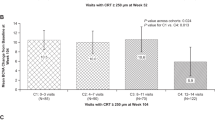
Mean FTH at M24 was 374.1 μm in the poor visual outcome group vs 268.8 μm in the better outcome group (P=0.005 by univariate and P=0.01 by multivariate analysis; Table 2).
Effect of cataract surgery or cataract progression on visual outcome
Between baseline and M24, 1 of 27 patients in the poor outcome group and 4/74 in the better outcome group underwent cataract surgery, and 3/27 patients in the poor outcome group and 10/74 in the better outcome group had progression of cataract that was not severe enough to consider cataract surgery. Neither of these differences was statistically significant (Table 2).
Differences in fluorescein angiographic and treatment characteristics between groups
Of the 95 sets of color and FA images available for analysis, the following could not be graded: two images for the presence of laser scars in the central 1 mm, seven for foveal atrophy, one for pigmentary changes in the fovea, and nine for the presence of severe macular ischemia. Table 3 summarizes the color photographic and FA characteristics between the groups. Foveal atrophy was identified in 65% (11/17) in the poor outcome group and 17% (12/71) in the better outcome group (P<0.001 by univariate and P=0.01 by multivariate analysis, Table 4). Pigmentary changes in the fovea were more frequent in patients in the poor outcome vs better outcome groups (70 vs 39%, P=0.01); however, this difference was not significant by multivariate analysis. Extensive macular laser treatment and laser within the central 1 mm were almost equivalent among groups: 58% (14/24) and 46% (10/22) in poor visual outcome vs 45% (32/71) and 52% (37/71) in the better outcome groups (P=0.26 and P=0.59). Severe macular ischemia was present in 4 of 17 (21%) in the poor visual outcome group and 7 of 67 (10%) in the better outcome group (P=0.25).
Further analysis of patients with poor VA outcome
Among the 27 patients in the poor visual outcome group, edema could not be ruled out as a cause of poor VA in 14, although 13 patients had little or no edema. Figure 1 shows images from a patient in which persistent/recurrent edema contributed to poor visual outcome, and Figure 2 shows images from a patient who had a poor visual outcome despite the absence of edema. Table 5 summarizes differences in characteristics between the two groups. There were no significant differences in gender, race, age, duration of disease, BCVA, or FTH at baseline. There was a higher percentage of patients in the RBZ group (50% (7/14) vs 7% (1/13), P=0.03) and a lower percentage in the RBZ+laser group (14% (2/14) vs 54% (7/13), P=0.04) who had edema at the M24 visit. The mean times to peak BCVA and the magnitude of peak BCVA gain were similar between groups (10.2 vs 13.6, P=0.2; 15.0 vs 8.1, P=0.35). However, patients in the edema group maintained BCVA between baseline and M24, whereas patients in the edema-free group lost on average 5.9 letters between baseline and M24. Patients with edema required a significantly higher number of injections (9.2 vs 4.3, P<0.001), and FTH at M24 was higher (450.3 μm vs 292.2 μm, P=0.004). The percentage of patients who received extensive laser treatments as well as total number of laser treatments was similar between groups (46% (6/13) vs 73% (8/11), P=0.24; 2.5 vs 3.4, P=0.29). However, laser in the central 1 mm was significantly more frequent in the edema-free group (78% (7/9) vs 23% (3/13), P=0.03). Owing to the small numbers, this sub-analysis was not adjusted for possible confounding variables.
Images at M24 of a patient with poor visual outcome in which recurrent macular edema contributed. Fundus photograph (a) and red-free photograph (b) show some pigmentary changes adjacent to the fovea, laser burns temporally, exudates inferiorly, and a few hemorrhages and microaneurysms. An early frame of a FA taken 43 s after dye injection (c) shows many microaneurysms and areas of capillary closure temporally and superiorly. A late frame of the FA taken 11 min and 3 s after dye injection (d) shows severe leakage with pooling of dye in the fovea in a petaloid pattern. A horizontal time domain OCT scan through the fovea (e) shows severe thickening and intraretinal fluid.
Images at M24 of a patient with poor visual outcome in which recurrent macular edema did not contribute. Fundus photograph (a) and red-free photograph (b) show some numerous laser scars surrounding the fovea (within 1 mm) and throughout the posterior pole. An early frame of a fluorescein angiogram (FA) taken 41 s after dye injection (c) shows hyper- and hypofluorescent spots in areas of laser burns and pigmentary changes and some microaneurysms between the disc and fovea. A late frame of the FA taken 10 min and 48 s after dye injection (d) shows mild leakage associated with the microaneursyms near the disc, but no leakage or pooling of dye near the fovea. A horizontal time domain optical coherence tomography scan through the fovea (e) shows no thickening or intraretinal fluid.
Discussion
Several studies have demonstrated that VEGF antagonists provide benefit in patients with DME.3, 4, 5, 6, 7, 8 These studies show that on average patients with DME experience reduction in retinal thickness and improvement in BCVA when treated with an anti-VEGF agent or with a combination of an anti-VEGF agent and focal/grid laser. However, although some patients improve to near-normal levels, others are left with substantial visual disability. In this study, we sought to determine why visual outcomes vary in patients with DME treated with RBZ. As the range of visual outcomes is large and the differences among patients are large, this sort of analysis is very complex. To reduce complexity, we performed a categorical analysis. Given new criteria for legal blindness when using ETDRS charts (http://www.lighthouse.org/about-low-vision-blindness/definition-legal-blindness/), patients with BCVA of 20/100 or worse were considered to have a poor visual outcome. Compared with patients who had a better visual outcome, those with a poor outcome had a significantly lower mean baseline BCVA. These two groups showed almost an equal peak improvement, but the change from baseline to M24 was −2.6 letters in the poor outcome group compared with +9.8 letters in the better outcome group. This suggests that both groups had potential for visual gain, but it was only achieved in one of them. Uncontrolled edema accounted for poor visual outcome in about half the patients in the poor visual outcome group and these patients could still have some improvement in vision with better control of edema. In fact, after M24, the protocol was amended and patients were evaluated every month and recurrent or persistent edema was treated with RBZ; this resulted in reduced FTH and visual improvement in many of the patients who had residual edema at M24.9 In the remaining half of the patients with poor visual outcome, there was no residual edema contributing to reduced vision.
In patients with poor visual outcome, foveal atrophy was significantly more frequent than in patients with better outcome. This suggests that photoreceptor damage is a major contributor to poor visual outcome. There are several possible causes for photoreceptor damage, including chronicity of edema, ischemia, or foveal damage from photocoagulation. Although this study has not provided definitive evidence that long-standing persistent and/or recurrent edema contributed to poor outcome, there are some hints that this may be the case. Poor vision at baseline correlated with a poor visual outcome and patients with more severe edema had poor vision at baseline. Patients with poor baseline vision still had some potential for visual improvement, because many of them showed substantial improvement from baseline BCVA at some point in the trial, but this improvement was gradually lost. Whether this loss could have been prevented by better control of edema is an important question that should be investigated in the future.
Macular ischemia has been suggested to be associated with poor visual outcomes in patients with DME.10, 11 We did not find a significant association between severe macular ischemia and poor visual outcome regardless of the presence or absence of residual edema. However, a limitation of our study is that it was a retrospective analysis of a clinical trial and may not have had sufficient power to detect all differences between groups that contribute to poor visual outcome. Therefore, we cannot conclude that our failure to identify differences in some of the parameters, such as severe macular ischemia, conclusively proves that they do not exist. Surprisingly, seven patients with a good visual outcome (≥20/40) were judged to have severe macular ischemia because of widespread closure of perifoveal capillaries involving 360° of capillaries bordering the foveal avascular zone. This could mean that macular ischemia does not contribute to poor visual outcome in patients with DME, or it may mean that closure of perifoveal capillaries is not a valid indicator of macular ischemia and that some patients may obtain sufficient oxygenation from the choroid to maintain foveal function. Thus, we conclude that dropout of perifoveal capillaries for 360° for at least 1 mm around the fovea is not strongly associated with a poor visual outcome, but as we do not know how well this anatomic finding correlates with macular ischemia, we cannot determine whether macular ischemia contributes to poor outcome. One might expect that patients with extensive macular laser are more likely to have had foveal damage or may have exceeded a threshold of loss of central retinal tissue that would lead to reduced vision. However, there was no association between patients with extensive macular laser photocoagulation and reduced visual outcome, which is consistent with results of a previous study.12 Closeness of photocoagulation burns to the fovea may be more important than total amount of macular laser. The percentage of patients with laser burns in the central 1 mm was significantly greater in patients with a poor visual outcome and no residual edema compared with patients who had a poor visual outcome due to residual edema. This raises the possibility that laser photocoagulation in close proximity to the fovea could contribute to poor visual outcome in patients treated with a combination of an anti-VEGF agent and focal laser, and it may be prudent to avoid it since we no longer have to rely solely on laser.
In conclusion, after 2 years of treatment of DME with RBZ no more frequently than every 2 months for recurrent edema, about 27% of patients have a poor visual outcome (BCVA≤20/100), with about half having some residual edema that could be contributing. More aggressive follow up and treatment with RBZ was able to improve vision in some of these patients.9 Foveal atrophy was substantially more common in patients with poor visual outcome than in patients with a better visual outcome suggesting that photoreceptor damage was an important contributor to reduced vision. Severity and/or chronicity of edema may have contributed because poor vision at baseline correlated with a poor visual outcome and, although many patients with poor vision at baseline showed substantial improvement from baseline BCVA at some point in the trial, this improvement was gradually lost. Focal laser within 1 mm of the center of the fovea was a significant factor associated with poor vision in patients who did not have persistent edema as a cause of poor vision. These data suggest that treatment with anti-VEGF agents should be initiated early in the disease process before vision is substantially reduced. Focal laser therapy is well-tolerated in most patients, but in view of the substantial efficacy of anti-VEGF agents, it is prudent to avoid laser photocoagulation in close proximity to the fovea.

References
Klein R, Klein B . Vision disorders in diabetes. In: Group NDD editor, Diabetes in America 2nd ed. National Institutes of Health: Washington, DC, USA, 1995 pp 293–330.
Nguyen QD, Tatlipinar S, Shah SM, Haller JA, Quinlan E, Sung J et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol 2006; 142: 961–969.
Nguyen QD, Shah SM, Heier JS, Do DV, Lim J, Boyer D et al. Primary end point (six months) results of the Ranibizumab for Edema of the mAcula in Diabetes (READ-2) Study. Ophthalmology 2009; 116: 2175–2181.
Nguyen QD, Shah SM, Khwaja AA, Channa R, Hatef E, Do DV et al. Two-year outcomes of the Ranibizumab for Edema of the mAcula in Diabetes (READ-2) study. Ophthalmology 2010; 117: 2146–2151.
The Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibzumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmolgy 2010; 117: 1064–1077.
Massin P, Bandello F, Hansen LL, Harding SP, Larsen M, Mitchell P et al. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study). Diabetes Care 2010; 33: 2399–2405.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Masin P, Schlingemann RO et al. The RESTORE Study. Ranibizumab monotherapy or combined with laser vs laser monotherapy for diabetic macular edema. Ophthalmology 2011; 118: 615–625.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L et al. Ranibizumab for diabetic macular edema. Results from 2 Phase III Randomized Trials: RISE and RIDE. Ophthalmology 2012; 119: 789–801.
Do DV, Nguyen QD, Khwaja AA, Channa R, Sepah YJ, Sophie R et al. Ranibizumab for edema of the macula in diabetes study: 3-year outcomes and the need for prolonged frequent treatment. JAMA Ophthalmol 2013; 131 (2): 139–145.
Chung EJ, Roh MI, Kwon OW, Koh HJ . Effects of macular ischemia on the outcome of intravitreal bevacizumab therapy for diabetic macular edema. Retina 2008; 28: 957–963.
Jonas JB, Martus P, Degenring RF, Kreissing I, Akkoyun I . Predictive factors for visual acuity after intravitreal triamcinolone treatment for diabetic macular edema. Arch Ophthalmol 2005; 123: 1338–1343.
Aiello LP, Edwards AR, Beck RW, Bressler NM, Davis MD, Ferris F et al. Factors associated with improvement and worsening of visual acuity 2 years after focal/grid photocoagulation for diabetic macular edema. Ophthalmology 2010; 117: 946–953.
Acknowledgements
Jiangxia Wang, MS, MA, assisted with the data analysis for this study. She is affiliated with the Biostatistics Center, Department of Biostatistics, Johns Hopkins Bloomberg School of Public Health; supported by Wilmer Biostatistics Core Grant EY01765. The study was supported by Genentech and by a grant from the Juvenile Diabetes Research Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Afsheen Khwaja was an employee of JHU during the conduct of the study, but is now an employee of Santen Inc. Diana V Do has the following potential conflicts of interest: consultant for ISTA and Johns Hopkins University has received payment for her consulting with Regeneron and Genentech. She has received an honorarium from Heidelberg. Johns Hopkins University, the previous employer of Dr Do receives research support from Genentech, Regeneron, Heidelberg, and Pfizer. Quan Dong Nguyen has the following potential conflicts of interest: consultant for Bausch and Lomb, and Santen. The Johns Hopkins University receives payment for his consulting with Genentech, Acucela, Pfizer, Regeneron, GlaxoSmithKline, and Heidelberg. Johns Hopkins University, the previous employer of Dr Nguyen, has received research support from Genentech, MacuSight, and Regeneron. Dr Nguyen chairs the Steering Committee for the RISE and RIDE studies. Peter A Campochiaro has the following potential conflicts of interest: consultant for Kala Pharmaceuticals and Applied Genetic Technologies Corporation and served as a consultant for Allergan within the past 2 years. Johns Hopkins University receives payment for his consultation with Genentech, Regeneron, and Aerpio. He receives research support from Genentech, Regeneron, Allergan, Aerpio, Genzyme, and Oxford BioMedica. These activities are being managed by the Conflict of Interest Committee of the Johns Hopkins University School of Medicine.
Additional information
Contributors Clinical Sites Black Hills Regional Eye Institute: Principal Investigator: Prema Abraham, MD Coordinator: Buffi Green, Kristi Livermont East Bay Retina Consultants Principal Investigator: Eugene S Lit, MD Investigators: Daniel A Brinton, MD, Scott S Lee, MD Coordinator: Scotty Renslow Eye Care Specialists Principal Investigator: Erik F Kruger, MD Coordinator: Patty Yuhas, COA Illinois Retina Associates Principal Investigator: John S Pollack, MD Investigators: Joseph M. Civantos, MD Coordinator: Barbara J Ciscato Johns Hopkins University/Wilmer Eye Institute Principal Investigator: Diana V Do, MD Investigators: Peter Campochiaro, MD, Daniel Finkelstein, MD, Morton F Goldberg, MD, James T Handa, MD, Quan Dong Nguyen, MD, MSc, Jennifer U Sung, MD, Howard Ying, MD, PhD, Ingrid Zimmer-Galler, MD Coordinators: Gulnar Hafiz, MD, MPH, Lisa Azzaro, COT, Lisa Greer, COT, MBA, Ovais Shaikh, MD, COT, Jennifer Simmons, COT Midwest Eye Institute Principal Investigator: Thomas Ciulla, MD Coordinator: Neelam Thukral Ophthalmic Consultants of Boston Principal Investigator: Jeffrey S Heier, MD Investigators: Janet J Chieh, MD, Tina S Cleary, MD, Gregory L Fenton, MD, David S Liao, MD, Trexler M Topping, MD, Torsten W Wiegand, MD, Grant P Janzen, MD, Sumit P Shah, MD, Jeffrey A Chang, MD Coordinator: Lindsey Williams Retina Consultants of Arizona Principal Investigator: Pravin U Dugel, MD Investigators: Jack Sipperley, MD, Donald W Park, MD, Judy Liu, MD, Derek Y Kunimoto, MD, Edward J Quinlan, MD, Arthur Mollen, DO, Jaime R Gaitan, MD Coordinator: Sarah G Mobley, CCRC Retina Consultants of Nevada—Las Vegas Principal Investigator: Allen Thach, MD Investigators: Roger Simon, MD, R Jeffrey Parker, MD, Rodney D Hollifield, MD, Roy H Loo, MD, MeherYepremyan, MD, Irene Voo, MD, Jason C Wickens, MD Coordinators: Janet Seybert, Cassondra Major, Mia Davis, Christy Browder, Melissa Rediker Retina Institute of California Principal Investigator: Thomas S Chang, MD Investigators: Michael A Samuel, MD, Anthony J Culotta, MD, Ednan Ahmed, MD Coordinator: Yvette Baghoomian, Coleman Ho Retina-Vitreous Associates Medical Group Principal Investigator: David Boyer, MD Investigators: Roger L Novack, MD, PhD, Thomas G Chu, MD, PhD, Firas M Rahhal, MD, Janet Jill Hopkins, MD, FRCSC, HomayounTabandeh, MD, MS, FRCP, FRCS, FRCOphth, Richard H. Roe, MD, MHS Coordinator: Tammy Gasparyan, Janet Kurokouchi, Charles Yoon University of New Mexico Principal Investigator: Arup Das, MD, PhD Investigators: Mark Schluter, MD Coordinator: Sheila Nemeth, COMT University of Southern California/Doheny Eye Institute Principal Investigator: Jennifer Lim, MD (year 1); Dean Eliott, MD (years 2 and 3) Coordinator: Margaret Padilla Steering Committee Peter A Campochiaro, MD Jeffrey S Heier, MD Quan Dong Nguyen, MD, MSc, Chair Data Safety and Monitoring Committee Brian P Conway, MD, University of Virginia David Wilson, MD, Oregon Health and Science University, Casey Eye Institute Reading Center The Retinal Imaging Research and Reading Center at Wilmer Roomasa Channa, MD Mohamed Ibrahim, MD Yasir Sepah, MD Syed Mahmood Shah, MBBS. Data Collection and Monitoring Center, Wilmer Eye Institute, Johns Hopkins University Afsheen Khwaja, MD John Putzke, PhD, MSPH Yasir Sepah, MD Coordinating Center, Wilmer Eye Institute, Johns Hopkins University Gulnar Hafiz, MD, MPH Velma Pack, BA Statistical Analyses Raafay Sophie, MD Afsheen Khwaja, MD Roomasa Channa, MD Yasir Sepah, MD
Rights and permissions
About this article
Cite this article
Channa, R., Sophie, R., Khwaja, A. et al. Factors affecting visual outcomes in patients with diabetic macular edema treated with ranibizumab. Eye 28, 269–278 (2014). https://doi.org/10.1038/eye.2013.245
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.245
Keywords
This article is cited by
-
Predictive factors for treatment outcomes with intravitreal anti-vascular endothelial growth factor injections in diabetic macular edema in clinical practice
International Journal of Retina and Vitreous (2023)
-
Angiographic biomarkers are significant predictors of treatment response to intravitreal aflibercept in diabetic macular edema
Scientific Reports (2023)
-
The effect of insulin on response to intravitreal anti-VEGF injection in diabetic macular edema in type 2 diabetes mellitus
BMC Ophthalmology (2022)
-
Optical coherence tomography angiography analysis of changes in the foveal avascular zone in eyes with diabetic macular edema treated with intravitreal anti-vascular endothelial growth factor
International Journal of Retina and Vitreous (2022)
-
Effect of age on response to anti-VEGF agents in patients with center involving diabetic macular edema in a tertiary hospital
International Journal of Retina and Vitreous (2022)