Abstract
Purpose
To investigate the effect of head tilt on keratometric measurement using the IOLMaster.
Methods
Twenty-seven right eyes of 27 volunteers were examined using a manual keratometer (MK), automated keratometer (AK), and an IOLMaster. MK and AK measurements were performed in the upright head position, whereas IOLMaster measurements were performed in five different head positions (upright, 5° or 15° clockwise head tilt, and 5° or 15° counter-clockwise head tilt). The repeatability of IOLMaster was compared with MK and AK. The keratometric measurements (mean keratometric power, magnitude of astigmatism, and steep meridian) in different head positions were compared.
Results
The IOLMaster showed good repeatability of keratometric measurement comparable to MK or AK. 15° and 5° clockwise head tilt resulted in 12.09±9.51 (mean±SD) (P<0.001 vs upright) and 5.51±5.97 (mean±SD) degrees (P<0.001) of clockwise rotation of steep meridian, respectively. 15° and 5° counter-clockwise head tilt resulted in 12.49±7.07 (mean±SD) (P<0.001) and 6.08±5.09 (mean±SD) degrees (P<0.001) of counter-clockwise rotation of steep meridian, respectively.
Conclusions
The patient’s head tilt (5° or 15°, clockwise or counter-clockwise) significantly changed the steep meridian of astigmatism measured using IOLMaster and the steep meridian generally shifted to the direction of head tilt. The importance of maintaining the upright head posture during IOLMaster measurement is demonstrated.
Similar content being viewed by others
Introduction
The recent popularity of toric intraocular lenses (IOLs) heightens concerns about the accuracy of preoperative astigmatism measurement. The accuracy of keratometry is very important in planning astigmatism correction.1 Misalignment of toric IOLs can induce unexpected refractive outcomes after surgery.2, 3, 4 It is well known that eyes undergo cyclotorsional movement when changing from the sitting to the lying positions.5, 6, 7 The surgical procedure of astigmatism correction often begins with alignment and axis marking of eyes while sitting at the slit lamp. Various preoperative marking and surgical techniques8, 9, 10 have been introduced for precise positioning of toric IOLs, and a new intra-operative technology placing an angular scale display within the surgical microscope has recently been introduced to the market (SMI Surgery Guidance, SensorMotoric Instruments, Teltow, Germany). Manual keratometry, automated keratometry, and partial coherence interferometry are the most common instruments being used to measure keratometric values before cataract surgery. All of these instruments emphasize correct upright right head position during the measurement by supplying two marking points to level the right and left lateral canthi. However, a small misalignment is always possible even in experienced hands and head movement during the measurement can contribute further error. Torsional ocular movement usually compensates small head tilts, but not always.
In this study, we intentionally induced head tilts (5° and 15°) in clockwise and counter-clockwise directions during keratometric measurement by partial coherence interferometry, IOLMaster (Carl Zeiss Meditec, Oberkochen, Germany). We compared the obtained keratometric values (steep K, flat K, and the meridian of steep K) between the tilted and upright head positions.
Materials and methods
This study analyzed the measurement of right eyes of 27 volunteers (medical students of Dongguk University). This study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board of Dongguk University, Ilsan Hospital.
Measurement device
Manual keratometry (Ker 200, Rodenstock, Dusseldorf, Germany), automated keratometry (Full Auto Ref-keratometer RK-F1, Canon, Tokyo, Japan), and IOLMaster were used for this study.
Determining head posture and measurement
Measurements began with the manual keratometer (MK). The examinee was instructed to place their chin on the chin rest and appose their forehead to the forehead rest of the MK. Next, the lateral canthi of both eyes were aligned to the instrument’s eye level markers. Three points (nose tip, dorsum of the nose, and mid-glabella) were marked with a marking pen. A straight line was drawn on transparent commercial tape (Scotch, 3M, St Paul, MN, USA) and attached to the face between the marked points. After measuring with MK, automated keratometer (AK), and IOLMaster at zero-degree rotation, the examinee was asked to tilt the head. A protractor and thread and pendulum bob attached to the forehead rest were used to determine rotation angle with respect to the marked face midline. IOLMaster measurements were performed at four head tilt positions (5° and 15°, clockwise and counter-clockwise). All measurements with MK, AK, and IOLMaster were performed in triplicate.
Analysis of astigmatism change with head tilt
The magnitude of measured astigmatism was compared in each head position. The meridian of astigmatism was analyzed as follows; if the change of meridian was in the same direction as head tilt, the change of meridian had positive value in degrees; if the change of meridian was in the opposite direction of head tilt, then the change of meridian had negative value in degrees.
Statistical analysis
Statistical analysis was performed using SPSS software (version 20.0, SPSS Inc., Seoul, South Korea). Normality of data was assessed by the Shapiro–Wilk test. Paired T test was used to compare two related samples. P-values less than 0.05 were considered to be significant.
To determine the repeatability of measurement by each device, intraclass correlation coefficient (ICC) was calculated for the three repeated measurements. ICC valued greater than 0.90 signify high repeatability.
Results
All 27 subjects (22 male and 5 female) completed the measurement with good compliance. The age of subjects was 26.48±3.24 (mean±SD) (range 22–34).
MK, AK, and IOLMaster all showed good repeatability in measurement of keratometric powers (mean keratometric power and magnitude and meridian of corneal astigmatism) (Table 1).
Mean keratometric values measured higher with IOLMaster (43.33±0.91D, mean±SD) than with AK (42.82±0.99D) (P<0.001). However, mean keratometric values measured with MK (42.89±0.90D) showed no difference compared with IOLMaster or AK (Table 2). The magnitude of astigmatism measured higher with AK (1.97±1.10D) than with MK (1.80±1.08D) (P=0.002) and IOLMaster (1.83±1.05D) (P=0.005). However, the meridian of astigmatism showed no significant difference between the different measurement instruments.
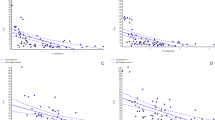
Head tilt either clockwise or counter-clockwise affected the meridian of astigmatism significantly (Table 2). Head tilt changed the meridian of astigmatism in the same direction of head tilt; 15° and 5° clockwise tilt resulted in 12.09±9.51° (range −15.33–24.67) (P<0.001 vs upright) and 5.51±5.97° (−3.66–17.67) (P<0.001 vs upright) clockwise rotation of meridian, respectively; 15° and 5° counter-clockwise tilt resulted in 12.49±7.07° (−11.33–22.66) (P<0.001 vs upright) and 6.08±5.09° (−5.67–18.66) (P<0.001 vs upright) counter-clockwise rotation of astigmatism meridian, respectively (Figures 1 and 2). Personal variation existed as evidenced by some outliers in Figures 1 and 2.
Bland–Altman plots show differences in astigmatism meridian between upright head position and clockwise head tilt. (a) Clockwise head tilt, 15°. (b) Clockwise head tilt, 5°. Mean difference and 95% limit of agreement (mean±2 SD of the difference) are represented by the three horizontal solid lines. If the change of meridian is in the same direction as that of the head tilt, the change of meridian has positive value and vice versa.
Bland–Altman plots show differences in astigmatism meridian between upright head position and counter-clockwise head tilt. (a) Counter-clockwise head tilt, 15°. (b) Counter-clockwise head tilt, 5°. Mean difference and 95% limit of agreement (mean±2 SD of the difference) are represented by the three horizontal solid lines. If the change of meridian is in the same direction as that of the head tilt, the change of meridian has positive value and vice versa.
However, the mean keratometric power and magnitude of astigmatism were not affected by head tilt on either clockwise or counter-clockwise direction (Table 2).
Discussion
In this study, MK, AK, and IOLMaster showed overall good repeatability of keratometric measurement (magnitude and meridian). The mean keratometric power was measured higher with IOLMaster than with MK or AK. The astigmatic power was measured higher with AK than with MK or IOLMaster. However, the meridian of astigmatism was not significantly different between instruments. Head tilt when measuring IOLMaster either in clockwise or counter-clockwise direction resulted in the rotation of astigmatic meridian in the same direction.
The precision in measurement of axial length by partial coherence interferometry technology, integrated automated keratometry function, and ease of operation are stated advantages of IOLMaster for standard biometry before cataract surgery.11, 12, 13, 14, 15 The astigmatism measurement (meridian and power) by IOLMaster was not different from measurement using MK in our and others’ studies.16 However, the higher measurement of mean keratometric power with IOLMaster than with AK has previously raised concerns.17 Therefore, it is always necessary to optimize IOLMaster calculating formulae by reviewing first series of surgical outcomes, because IOL power calculation output by the IOLMaster is based on its measurement.18
It is interesting that head tilt during IOLMaster measurement significantly changed the astigmatic meridian but had little effect in keratometric power (mean and astigmatism). The possible effect of head tilt on keratometric axis measurement is anticipated. However, torsional eye movements may or may not have sufficiently compensated the head tilt. No previous reports about the effect of head tilt on keratometry measurement by IOLMaster have been reported to our knowledge. Our results indicated that the compensatory effect was insufficient and this resulted in significant changes of astigmatic meridian in most eyes in our study. It is probable that the fixation target of the IOLMaster is not strong enough to induce complete compensatory torsional eye movement. It is also noteworthy that head tilt had little effect on mean keratometric power measurement, and hence, the IOL power calculation for non-toric IOLs.
An increasingly common clinical implication of incorrect astigmatic meridian measurement is incorrect toric IOL implantation. Theoretical analysis predicts a steady loss of astigmatism correction as a toric IOL rotates more and more off axis. The relationship is fairly linear from 0° to 30°, where the correction drops to essentially zero.19 The misaligned toric IOL not only causes reduction of astigmatism correction but also results in both rotation of the astigmatic meridian and change of the refractive spherical equivalent.4 Optical quality is also compromised and modulation transfer function decays to ∼50% due to increased aberration when a toric IOL rotates from 0° to 5°.2
A limitation of our study was the relatively small number of cases (27 eyes); however, considering the good repeatability of keratometric measurement by IOLMaster and the low P-values, we believe our study is sufficient to demonstrate the effect of head tilt on astigmatism meridian measurements by IOLMaster.
In summary, our study found a significant effect of head tilt on astigmatism meridian measurement using IOLMaster. Based on our results, we recommend that a cautious approach is necessary to avoid inadvertent head tilt when measuring preoperative keratometric data by IOLMaster, especially for toric IOL implantation. In cases of patients who have asymmetric lateral canthi or severe dermatochalasis obscuring the lateral canthal areas, more attention may be necessary to maintain upright head alignment.

References
Visser N, Berendschot TT, Bauer NJ, Jurich J, Kersting O, Nuijts RM . Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg 2011; 37: 1394–1402.
Felipe A, Artigas JM, Diez-Ajenjo A, Garcia-Domene C, Peris C . Modulation transfer function of a toric intraocular lens: evaluation of the changes produced by rotation and tilt. J Refract Surg 2012; 28: 335–340.
Forseto AS, Nose RM, Nose W . Toric intraocular lens misalignment inducing astigmatism after refractive surgery. J Refract Surg 2011; 27: 691–693.
Jin H, Limberger IJ, Ehmer A, Guo H, Auffarth GU . Impact of axis misalignment of toric intraocular lenses on refractive outcomes after cataract surgery. J Cataract Refract Surg 2010; 36: 2061–2072.
Ciccio AE, Durrie DS, Stahl JE, Schwendeman F . Ocular cyclotorsion during customized laser ablation. J Refract Surg 2005; 21: S772–S774.
Kim H, Joo CK . Ocular cyclotorsion according to body position and flap creation before laser in situ keratomileusis. J Cataract Refract Surg 2008; 34: 557–561.
Chang J . Cyclotorsion during laser in situ keratomileusis. J Cataract Refract Surg 2008; 34: 1720–1726.
Cha D, Kang SY, Kim SH, Song JS, Kim HM . New axis-marking method for a toric intraocular lens: mapping method. J Refract Surg 2011; 27: 375–379.
Watanabe K, Negishi K, Torii H, Saiki M, Dogru M, Tsubota K . Simple and accurate alignment of toric intraocular lenses and evaluation of their rotation errors using anterior segment optical coherence tomography. Jpn J Ophthalmol 2012; 56: 31–37.
Ma JJ, Tseng SS . Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg 2008; 34: 1631–1636.
Bhatt AB, Schefler AC, Feuer WJ, Yoo SH, Murray TG . Comparison of predictions made by the intraocular lens master and ultrasound biometry. Arch Ophthalmol 2008; 126: 929–933.
Packer M, Fine IH, Hoffman RS, Coffman PG, Brown LK . Immersion A-scan compared with partial coherence interferometry: outcomes analysis. J Cataract Refract Surg 2002; 28: 239–242.
Yong Park C, Do JR, Chuck RS . Predicting postoperative astigmatism using scheimpflug keratometry (Pentacam) and automated keratometry (IOLMaster). Curr Eye Res 2012; 37 (12): 1091–1098.
Whang WJ, Jung BJ, Oh TH, Byun YS, Joo CK . Comparison of postoperative refractive outcomes: IOLMaster((R)) versus immersion ultrasound. Ophthalmic Surg Lasers Imaging 2012; 2: 1–4.
Shammas HJ, Chan S . Precision of biometry, keratometry, and refractive measurements with a partial coherence interferometry-keratometry device. J Cataract Refract Surg 2010; 36: 1474–1478.
Lee H, Chung JL, Kim EK, Sgrignoli B, Kim TI . Univariate and bivariate polar value analysis of corneal astigmatism measurements obtained with 6 instruments. J Cataract Refract Surg 2012; 38: 1608–1615.
Elbaz U, Barkana Y, Gerber Y, Avni I, Zadok D . Comparison of different techniques of anterior chamber depth and keratometric measurements. Am J Ophthalmol 2007; 143: 48–53.
Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL . Intraocular lens formula constant optimization and partial coherence interferometry biometry: refractive outcomes in 8108 eyes after cataract surgery. J Cataract Refract Surg 2011; 37: 50–62.
Till JS, Yoder PR Jr., Wilcox TK, Spielman JL . Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg 2002; 28: 295–301.
Acknowledgements
This work was supported partially by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF 2010-0002532) and a core grant from Research to Prevent Blindness (Albert Einstein College of Medicine).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, C., Do, J., Kim, S. et al. The effect of head tilt on keratometric measurement using the IOLMaster. Eye 27, 1411–1417 (2013). https://doi.org/10.1038/eye.2013.209
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.209