Abstract
Objective
To evaluate the feasibility and safety of a revised technique of botulinum toxin type A (BTA) injections for the treatment of infantile esotropia.
Methods
Forty-seven patients with infantile esotropia were randomly divided into two groups. In group A, 23 cases were treated with a bilateral injection of 2.5–3.75 U BTA combined with sodium hyaluronate (SH) to the medial rectus muscle. In group B, 24 cases were treated with a bilateral injection of 2.5–3.75 U BTA solution alone to the medial rectus muscle. Electromyography was not used in the study. All patients received one injection and were evaluated 2 weeks, 3 months, and 6 months following injection.
Results
The measured changes between groups A and B included the frequencies of good alignment 6 months after injections (30.4% vs 37.5%), complicated ptosis (2.2% vs 20.8%), and vertical deviation (2.2% vs 2.1%).
Conclusion
BTA injections combined with or without SH in the absence of electromyography demonstrated effectiveness and feasibility in the treatment of infantile esotropia. A relative decrease in the frequency of complicated ptosis resulted from injections of BTA+SH.
Similar content being viewed by others
Introduction
Many studies supported the administration of botulinum toxin type A (BTA) as an efficacious therapeutic protocol for the treatment of infantile esotropia1, 2, 3, 4, 5, 6 and acquired esotropia.7 Typically, electromyography is used to ensure toxin injection into the correct area of the muscle belly of the extraocular muscles. With electromyography, a clear signal will be present where the neuromuscular junctions are densely distributed, which is about 25 mm posterior to the muscular insertion.8 However, with children under general anesthesia, signal identification is relatively difficult because of the absence of active muscular contractions. Moreover, injections performed with electromyographic assistance are not directly visualized and are more likely to be close to the retrobulbar area when administered within the small eyeballs of children. As a result, drug diffusion to neighboring muscles, as well as ptosis and vertical deviations, may occur. Based upon these considerations, it is quite evident that improvements in BTA injection procedures in children are warranted.
Another salient issue regarding improvements in this protocol involves the combination of BTA injections with sodium hyaluronate (SH). The addition of SH may decrease drug diffusion to other muscles, and thus decrease the potential for ptosis and vertical deviations. In fact, data from our animal studies indicate a high level of BTA bioactivity when combined with SH9 and the presence of high concentrations that remain within localized regions following BTA+SH injections.10 Therefore, a pilot study using a revised protocol for BTA injections in the treatment of infantile esotropia was performed to evaluate its feasibility and possible merits.
Subjects and methods
Subjects
The research protocol was approved by the ethics committee of the Zhongshan Ophthalmic Center. The patients had attended the Strabismic and Amblyopic Clinic of the Zhongshan Ophthalmic Center from Feb 2008 to May 2011. Patients with esotropia onset before 6 months of age whose guardians choose botulinum toxin injection as the first treatment were enrolled in the study. Before study enrollment, patients underwent cycloplegic refraction with 1% atropine ointment once daily for 3 days. The full refractive correction that had been prescribed for the patients was >+1.50 diopter spherical. Patients with the following conditions were excluded from the study: became orthotropic after the refraction was corrected, had previous surgery, a history of allergy to any drugs, or complications resulting from systemic diseases. For cases with monocular amblyopia, occlusion of the unamblyopic eye for 3–6 h daily (50% of waking hours) over a 1–3 month period was required before the injections. All patients’ guardians were provided with information on the surgery and botulinum toxin injection, and the risks and benefits about the treatment were explained. A signed informed consent was required for enrollment. If the alignment was not satisfactory 6 months after BTA injection, patients’ guardians were offered the option for reinjection or surgery.
Methods
Subjects were randomly divided into two groups. Patients in group A were treated with 0.05 ml bilateral injection of 2.5–3.75 U BTA (Lanzhou Institute of Biological Products, Lanzhou, China) combined with SH (Shandong C. P. Freda Pharmaceutical Company, Jinan, China) to the medial rectus muscle in the absence of electromyography (Table 1). Patients in group B were treated with 0.03 ml bilateral injection of 2.5–3.75 U BTA solution to the medial rectus muscle in the absence of electromyography (Table 1). A dose of 2.5 U of BTA per muscle was administered to patients with deviation <30 prism diopters, whereas 3.75 U was used for those with >30 prism diopters. The doses used were based upon those recommended by Scott et al.11 All patients received one injection. The combined BTA and SH injection was prepared by mixing the BTA solution with SH at a volume ratio of 1 : 3. These solutions were mixed within a relative negative pressure syringe (original syringe for SH) by pulling the plunger back for approximately 40 min at 4 °C to enable even dispersion. A homogenous dispersion and the concentrations of BTA in the preparations were indicated from our previous studies with 125Iodine labeling technique. All preparations were made by the same physician at the bedside in a sterile manner just before injections. Separate syringes containing the designated amount of BTA solution were prepared for each accurate injection. All injections were performed while patients were maintained under general anesthesia.
After the administration of eye drops containing a topical anesthetic and 0.1% epinephrine, a blepharostat was used to retract the eyelids. The nasal corneal limbus was then grasped with forceps and reflected laterally. A 27-gauge needle was passed through the insertion of the medial rectus muscle and introduced at a distance of 5–10 mm parallel to the sclera. BTA+SH (0.05 ml) or BTA solution alone (0.03 ml) with target dosages of the toxin was then injected. All procedures were performed by the same person.
The size of deviation, ocular movements and the development of a palpebral fissure, an anterior segment, fundus, or any other symptoms were assessed before treatment and at 2 weeks, 3 months, and 6 months following the injections. The deviation size was assessed using the prism and alternate cover tests or the Krimsky or Hirschberg estimate. A deviation of <10Δ in the primary position at 6 months following injection was defined as a good alignment. Ptosis complications were rated on a scale of 0–4. A 2-mm reduction in the height of the palpebral fissure following the injection was considered as no ptosis (P0), a 2–3-mm reduction was considered as mild ptosis (P1), a ≥3-millimeter reduction without vision impairment was considered as moderate ptosis (P2), an apparent reduction with vision impairment was considered as marked ptosis (P3), and a complete eyelid closure was considered as profound ptosis (P4).12 In the primary position, complications of vertical deviation were defined as follows: mild, 1–10Δ of hypertropia or hypotropia; moderate, 10.1–20Δ; and severe, >20Δ.
Statistical software of SPSS 19.0 was used for data analysis, and SAS 9.1.3 was used to assess power analysis for the Fisher’s exact test. Paired t-tests were performed to evaluate the difference in deviation size before and 2 weeks after injections. Independent sample t-tests were used to compare the age or the preinjection deviation between groups A and B. Fisher’s exact tests were used to compare the prevalence of good alignment or complications, or gender distribution between groups A and B. A P-value <0.05 was considered statistically significant.
Results
A total of 47 cases (22 males and 25 females) were included. Table 2 shows the baseline clinical characteristics between groups A and B. Of the 47 patients, 10 were associated with monocular amblyopia, 5 with inferior oblique overaction (IOOA), 3 with dissociated vertical deviation (DVD), and 1 with both IOOA and DVD. The children received the BTA injections between 12 and 81 months of age.
Early symptoms and general examinations
Subconjunctival hemorrhages occurred in both groups with one injection per group. There were no complaints of diplopia from the children nor did they display any abnormal behaviors after the injections. There were no changes in the anterior segment and fundus examinations. However, two cases in group B developed -1 underaction of bilateral medial rectus at 2 weeks after injections and regained action 3 months after injections. The patients with IOOA and/or DVD in groups A and B showed the same abnormal ocular movements after injection. Retrobulbar hemorrhages and ocular perforations were not observed.
Early efficacy and complications
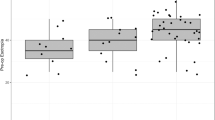
The measured changes (mean±SD) before and after injections between groups A and B, respectively, were as follows: the size of deviation before the injections (35.0±15.7Δ vs 33.9±16.7Δ), 2 weeks (14.2±13.1Δ vs −2.8±13.6Δ), 3 months (17.8±13.8Δ vs 10.2±8.2Δ), and 6 months (24.0±16.4Δ vs 15.9±13.5Δ) following injections and the frequencies of good alignment at 6 months after injections (30.4% vs 37.5%), complicated ptosis (2.2% vs 20.8%), and vertical deviation (2.2% vs 2.1%) (Table 3). The size of deviation was significantly reduced 2 weeks following the injections in both groups (group A: t=12.4, P≤0.0001, paired t-test; group B: t=11.3, P≤0.0001, paired t-test). Figure 1 shows a representative patient’s change of deviation before and after injections. The frequency of good alignment at 6 months after injections was not significantly different between groups A and B, but the rate of complicated ptosis was lower in group A. Of the 11 injections with complicated ptosis, 10 were associated with mild ptosis in group B, and only 1 injection with mild ptosis was observed in group A. In groups A and B, only one case developed a mild complicated vertical deviation. The rate of complicated vertical deviations did not differ significantly between groups A and B. Among the 16 cases without good alignments 6 months after injections in group A, 7 cases chose reinjection, 5 cases chose surgery, and 4 cases chose follow-up. In group B, 6 cases chose reinjection, 6 cases chose surgery, and 3 cases chose follow-up.
Discussion
Infantile esotropia represents one of the most common forms of strabismus. Because the onset occurs at the sensitive period for development of binocular vision, children with esotropia require early treatment to correct this condition and achieve better alignment and binocularity. However, complications associated with early treatment may jeopardize the outcome. Vertical deviation and ptosis are the most common complications that not only produce problems with appearance but also increase the risk of amblyopia in young children. Hence, safety is an especially important concern in the management of infantile esotropia at a very young age. Bilateral medial rectus injections of botulinum toxin has been shown to be an effective alternative to conventional surgery in the treatment of infantile esotropia.3, 4, 6 However, botulinum toxin injection for infantile esotropia is not without its own problems. Therefore, we revised the protocol of this classic technique to simplify the injection protocol and improve its safety.
The emphasis of this pilot study was to assess the feasibility and safety of a revised BTA injection technique in the treatment of infantile esotropia. A 6-month period after injection was selected for the final assessment in this pilot study, as it was reported that no variation in the angle of deviation was observed after 6 months following BTA injection.13 Our results indicated that a single bilateral medial rectus injection of botulinum toxin at 5–10 mm posterior to the muscular insertion without electromyography was effective for the treatment of infantile esotropia, with 30.4% of the patients showing a good alignment at 6 months after injections when treated with BTA+SH (group A), and 37.5% when treated with BTA alone (group B). The successful motor results in our study were similar to that reported by de Alba Campomanes,3 with 24.5% of their infantile esotropia patients showing long-term motor success in the first injection of BTA. Our results also indicated that BTA combined with SH did not prolong this effect, which may be because of a reduction in BTA bioactivity soon after injection as a result of a change in temperature. Only mild complicated ptosis and vertical deviation developed, and these conditions resolved spontaneously within 6 weeks. A rather low frequency of complications was observed following injections of BTA+SH. The rates of complicated ptosis and vertical deviation obtained in our study were no more than those reported previously, with values ranging from 24 to 55.54%.2, 5
The significance of our study is as follows: (1) the demonstration of BTA effectiveness in the absence of electromyography guidance; (2) the ability to target and inject at the medial rectus muscle 5–10 mm posterior to the muscular insertion; and (3) the possibility to reduce complications with injections of BTA+SH. These first two points were also supported by studies of de Alba Campomanes et al.3, 14 An additional note of significance of our report is the potential of this technique for the treatment of other types of strabismus. The underlying mechanisms of effectiveness may have involved toxin diffusion into posterior or shorter orbital fibers where BTA exerts the major action by the long or global fibers acting as a wick.15, 16 Although the same BTA dose was used in both groups, the lower rates of complications observed in group A may have resulted from a decrease of toxin diffusion to the neighboring muscles when the BTA injections were combined with SH. Such a decrease in toxin diffusion would reduce complications such as ptosis and vertical deviation.
In this pilot study, we describe a revised injection technique, consisting of BTA injections combined with or without SH in the absence of electromyography. Our results demonstrate the feasibility, simplificity, and potential safety of this protocol in the treatment of infantile esotropia. Further studies will be required to refine this technique and improve the efficacy of BTA injections while reducing adverse complications by adjusting the doses and/or the volume ratio of BTA and SH.

References
McNeer KW, Tucker MG, Spencer RF . Botulinum toxin management of essential infantile esotropia in children. Arch Ophthalmol 1997; 115: 1411–1418.
Rowe FJ, Noonan CP . Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev 2009; 15: CD006499.
de Alba Campomanes AG, Binenbaum G, Campomanes Eguiarte G . Comparison of botulinum toxin with surgery as primary treatment for infantile esotropia. J AAPOS 2010; 14: 111–116.
McNeer KW, Tucker MG, Guerry CH, Spencer RF . Incidence of stereopsis after treatment of infantile esotropia with botulinum toxinA. J Pediatr Ophthalmol Strabismus 2003; 40: 288–292.
McNeer KW, Spencer RF, Tucker MG . Observations on bilateral simultaneous botulinum toxin injection in infantile esotropia. J Pediatr Ophthalmol Strabismus 1994; 31: 214–219.
Baggesen K, Arnljot HM . Treatment of congenital esotropia with botulinum toxin type A. Acta Ophthalmol 2011; 89: 484–488.
Tejedor J, Rodríguez JM . Long-term outcome and predictor variables in the treatment of acquired esotropia with botulinum toxin. Invest Ophthalmol Vis Sci 2001; 42 (11): 2542–2546.
Scott AB . Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology 1980; 87 (10): 1044–1049.
Chen JC, Mai GH, Yu XP, Yu HY, Wu HP, Jiang FT . Qualitative analysis on the denervating action of botulinum toxin A in gel. Zhongguo Ying Yong Sheng Li Xue Za Zhi 2008; 24: 104–107.
Chen J, Mai G, Yu X, Yu H, Wu H, Lin X et al. Distribution of the toxin following medial rectus muscular injection of botulinum toxin gel in rabbits. Yan Ke Xue Bao 2005; 21: 52–55.
Scott AB, Magoon EH, McNeer KW, Stager DR . Botulinum treatment of childhood strabismus. Ophthalmology 1990; 97: 1434–1438.
Christine L, Burns CL, Gammon JA, GemmilL MC . Ptosis associated with botulinum toxin treatment of strabismus and blepharospasm. Ophthalmology 1986; 93: 1621–1627.
Campos EC, Schiavi C, Bellusci C . Critical age of botulinum toxin treatment in essential infantile esotropia. J Pediatr Ophthalmol Strabismus 2000; 37: 328–332.
Benabent EC, García Hermosa P, Arrazola MT, Alió y Sanz JL . Botulinum toxin injection without electromyographic assistance. J Pediatr Ophthalmol Strabismus 2002; 39: 231–234.
Spencer RF, McNeer KW . Botulinum toxin paralysis of adult monkey extraocular muscle. Structural alterations in orbital, singly innervated muscle fibers. Arch Ophthalmol 1987; 105: 1703–1711.
McNeer KW, Tucker MG, Spencer RF . Management of essential infantile esotropia with botulinum toxin A: review and recommendations. J Pediatr Ophthalmol Strabismus 2000; 37: 63–67.
Acknowledgements
This study was supported by a grant from the Guangdong Provincial Scientific Technological Research Fund (no. 2008B030301316).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, J., Deng, D., Zhong, H. et al. Botulinum toxin injections combined with or without sodium hyaluronate in the absence of electromyography for the treatment of infantile esotropia: a pilot study. Eye 27, 382–386 (2013). https://doi.org/10.1038/eye.2012.264
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.264