Abstract
Numerous systemically used drugs are involved in drug-induced glaucoma. Most reported cases of non-steroidal drug-induced glaucoma are closed-angle glaucoma (CAG). Indeed, many routinely used drugs that have sympathomimetic or parasympatholytic properties can cause pupillary block CAG in individuals with narrow iridocorneal angle. The resulting acute glaucoma occurs much more commonly unilaterally and only rarely bilaterally. CAG secondary to sulfa drugs is a bilateral non-pupillary block type and is due to forward movement of iris–lens diaphragm, which occurs in individuals with narrow or open iridocorneal angle. A few agents, including antineoplastics, may induce open-angle glaucoma. In conclusion, the majority of cases with glaucoma secondary to non-steroidal medications are of the pupillary block closed-angle type and preventable if the at-risk patients are recognized and treated prophylactically.
Similar content being viewed by others
Introduction
Glaucoma is a form of optic neuropathy with specific visual field loss. It is usually associated with raised intraocular pressure (IOP) and may be divided into primary and secondary forms.1, 2 All types of glaucoma are categorized as open angle or closed angle based on the status of iridocorneal angle. If the cause of glaucoma can be identified, then the closed-angle glaucoma (CAG) or open-angle glaucoma is secondary.
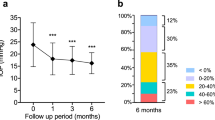
Glaucoma can occur as a consequence of some medications administered directly to the eye or systemically within the body. Untreated drug-induced glaucoma can lead to loss of vision. The majority of drugs listed as contraindicated in glaucoma are concerned with CAG. These medications may incite an attack in those individuals with narrow iridocorneal angle.3 At least one-third of acute closed-angle glaucoma (ACAG) cases are related to an over-the-counter or prescription drug.1 Prevalence of narrow angles in whites from the Framingham study was 3.8%. Narrow angles are more common in the Asian population. A study of a Vietnamese population estimated a prevalence of occludable angles at 8.5%.4 The reported prevalence of elevated IOP months to years after controlling ACAG with laser iridotomy ranges from 24 to 72%.5, 6 Additionally, a significant decrease in retinal nerve fiber layer thickness and an increase in the cup/disc ratio occurs after ACAG, which mandates lifelong care even when iridotomy has apparently alleviated the glaucoma attack.7, 8, 9, 10 Although drug-induced ACAG is relatively uncommon, it is a serious adverse reaction which, if not recognized in a timely manner, may result in severe morbidity and even permanent visual loss.
Medications have a direct or secondary effect, either to stimulate sympathetic or inhibit parasympathetic activation causing pupillary dilation, which can precipitate ACAG in predisposed patients (pupillary block CAG). In eyes predisposed to angle closure by their characteristic biometric features (short axial length and small anterior chamber), choroidal volume expansion also is considered as a contributing factor in inducing angle closure by slight forward movement of the lens and then narrowing and increasing resistance in the iris–lens channel.11 The other mechanism for CAG is thickening and forward movement of lens, ciliary body rotation, and choroidal effusion, which occur in patients with open or narrow iridocorneal angle (non-pupillary block CAG). This process seems to be an idiosyncratic reaction to certain systemic medications.
Most attacks of drug-induced pupillary block CAG occur in individuals that are unaware that they have narrow iridocorneal angles. Physicians using these drugs cannot practically send each and every patient to an ophthalmologist for gonioscopy, but they should be informed that patients wearing thick hyperopic glasses are at risk. They can perform the lateral penlight test to estimate anterior chamber depth and send the suspicious patients to an ophthalmologist for gonioscopy.12 The at-risk patients who are going to use the CAG inciting drugs should be offered a prophylactic iridotomy to prevent acute attacks. These patients need to be followed for any possible synechia formation and chronic CAG as long as they use the drugs.13
Numerous systemic medications have been implicated in the cause of drug-induced glaucoma and the most common medications that induce glaucoma are corticosteroids. In our previous review,14 all drugs causing glaucoma, including steroids, have been discussed; the present review is more comprehensive with recent references and discusses the treatments in detail. This review will discuss the non-steroidal medications that are involved with glaucoma induction.
Ocular agents
Antiglaucoma drugs
Cholinergic agents, topical anticholinesterase, pilocarpine, and intraocular acetylcholine and carbachol are commonly used cholinergic agents in ophthalmic practice. These agents can, however, induce ACAG due to anterior movement of the iris–lens diaphragm.3 In addition to narrow angle, the eyes with zonular weakness or exfoliation syndrome seem to be particularly prone to developing miotic-induced CAG.15 Surprisingly, pilocarpine may also precipitate ACAG by inducing mydriasis. This is due to an impurity of the stereoisomer of pilocarpine, jaborine, an atropine-like drug that even today, with improved manufacturing, occasionally is reported.16 Additionally, these agents can induce non-pupillary block CAG with inducing aqueous misdirection (malignant glaucoma).17
Sympathomimetics, especially those with α-1agonistic activity, cause mydriasis and can precipitate ACAG in predisposed individuals. Topical phenylephrine and its prodrugs dipivefrin and apraclonidine have been documented to induce ACAG.3, 18, 19, 20
Latanoprost has been associated with ACAG in two cases.21 Sakai et al22 had reported about ciliochoroidal effusion induced by latanoprost in a patient with Sturge–Weber syndrome. Enhanced uveoscleral outflow is the mechanism of latanoprost IOP reduction. Yalvac et al21 speculated that the increased flow through the ciliary muscles caused swelling of the ciliary body and pushed the iris–lens diaphragm anteriorly, initiating an ACAG.
Acetazolamide, an oral carbonic anhydrase inhibitor, can induce non-pupillary block CAG similar to other sulfa agents.23
Mydriatics
Topical anticholinergic/cycloplegics agents used for pupillary dilation for fundus examination should be used with caution in the susceptible patients. It has been shown that the iris volume increases after pupil dilation in narrow-angle eyes even in those with open iridotomies, which augments the possibility of CAG.24 Pandit and Taylor25 in a systematic review stated that the risk of inducing ACAG following mydriasis with tropicamide alone is close to zero and no case being identified. The risk with long-acting or combined agents was between 1 in 3380 and 1 in 20 000. However, Mapstone26 reported sever IOP elevation, which necessitated antihypertensive treatment in 19 out of 58 patients with narrow iridocorneal angle who underwent tropicamide pupil dilation.
Topical cycloplegics have been shown to cause significant IOP elevation in 2% of the apparently normal population, increasing to 23% of patients with known primary open-angle glaucoma.27, 28 It is recommended that the IOP be rechecked after dilation in glaucoma patients with significantly damaged optic nerve heads. The rise in IOP may be related to decreased aqueous outflow, resulting from decreased pull on the trabecular meshwork due to ciliary muscle paralysis.29 Valle30 reported an increase in aqueous inflow in patients who experienced a rise in IOP following pupillary dilation and also suggested a decrease in aqueous outflow in the same patients.
Ointments
Ointments are commonly used after ophthalmic surgery. Intraocular penetration may cause inflammation and open-angle glaucoma. One of the reported complications of intraocular ointments is toxic anterior segment shock syndrome that may lead to glaucoma due to trabeculitis and fibrin membranes.31 In 1972, Sugar and Airala32 proposed that ointments should be avoided on the first day or so postoperatively.
Botulinum toxin
Botulinum neurotoxins act primarily at peripheral cholinergic synapses, including the skeletal muscle neuromuscular junction, causing transient muscle paresis by inhibiting the release of acetylcholine. However, botulinum toxins could cause pupillary dilation when injected periocularly. It diffuses toward the ciliary ganglion and blocks its activity or acts at the pupillary sphincter muscle of the iris. Corridan et al33 reported a case of ACAG after receiving a series of botulinum toxin injections for blepharospasm.
Silicone oil
One of the reported complications of silicone oil is secondary open-angle glaucoma that can occur at any time in the postoperative period.34 The IOP elevation may range from mild and transient to severe and sustained. The early IOP spikes may be due to pupillary block, mechanical-angle obstruction by oil, or inflammation and the late-onset spikes are proposed to be due to synechial-angle closure, rubeosis iridis, oil droplet emulsification, and migration of silicone oil into the anterior chamber and clogging the outflow. Presence of silicone oil in the anterior chamber may induce a chronic inflammation and trabecular meshwork fibrosis. Treatments of elevated IOP include silicone oil removal, medical therapy, and laser or incisional surgeries.35, 36, 37
Viscoelastic materials
These agents have been associated with an elevated IOP and open angle in the early postoperative period.38 The IOP rise seems to be due to obstruction of the trabecular meshwork outflow channels and is usually seen within the first postoperative day.39 Kocak-Altintas et al40 also reported a higher incidence of postoperative IOP increases associated with the use of viscoelastic agents with higher viscosity. If these agents are carefully washed out of the eye at the end of surgery, the risk of an IOP spike will be significantly reduced.38, 39
Antibiotics
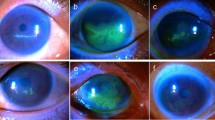
Sulfa drugs have been reported to induce ACAG without pupillary block. Mechanisms in this type of angle closure include lenticular swelling, retinal edema, choroidal effusion, and secondary shallowing of the anterior chamber associated with elevated IOP.41, 42, 43 The lens thickening has been confirmed with A-scan ultrasound in acute attacks.44 The increase in the anteroposterior lens thickness may be due to marked zonular relaxation secondary to swelling of ciliary body. Moreover, the mechanism may involve anterior rotation of the ciliary body, choroidal expansion secondary to accumulation of serous fluid in the extravascular choroidal space.43 This type of CAG has been reported with the following drugs: topiramate, hydrochlorthiazide, acetazolamide, quinine, and tetracycline.23, 45, 46, 47 Table 1 shows the list of medications containing sulfa component in their formulations.
The typical presentation is a bilateral ACAG that occurs within the first several doses of the sulfonamide-containing medication. There are cases reported after a single dose in patients who had taken the medication weeks or months previously without notable visual side effects. The most common presenting symptom is blurred vision. It is due to forward movement of the lens and increased lens thickness, which produces myopia. The forward position of the lens could explain about half of the myopic shift.48 Fan et al23 reported a case of ACAG in an individual who took oral acetazolamide and subsequently developed myopia in both the phakic and pseudophakic eyes. The induced myopia was attributed to forward movement of intraocular lens.
It has been documented that human immunodeficiency virus-infected individuals have a high risk for hypersensitivity reactions to sulfamethoxazol.49 A 49-year-old man with acquired immunodeficiency syndrome who started pneumocystis carini prophylaxis with sulfamethoxazole trimethoprim (cotrimoxazole) developed bilateral ACAG and 360 degree choroidal effusions in both eyes after just 4 days of drug use. Although the medication was stopped, the patient developed bilateral cataracts and phthisis bulbi in 2 months.42
In order to treat these patients, the sulfa-containing drug should be discontinued and IOP should be controlled by antihypertensive medicines. Topical steroid, cycloplegic agents, and aqueous suppressants are effective in treating this condition. Although cross-reactivity between sulfa drugs is rare, treatment with topical or systemic carbonic anhydrase inhibitors is contraindicated to control IOP in these patients.50, 51 Rhee et al52 reported the beneficial effect of intravenous methylprednisolone and mannitol in controlling the acute glaucoma induced by topiramate within 4 h in one patient. Topical miotics should be avoided as they may precipitate a relative pupillary block. Laser iridotomies or peripheral iridectomy would alleviate the CAG only if a pupillary block component is present, but otherwise are of no benefit.48 In those who do not respond to medical therapy, the possibility of supracilliary fluid accumulation should be taken into account.53 Parikh et al54 reported the successful outcome for ciliochoroidal effusion drainage in a case of bilateral ACAG with topiramate. After choroidal drainage, the anterior chamber deepened, corneal edema resolved, and IOP was controlled without medication.
Gentamicine has been reported to induce mydriasis after topical use in a patient, which theoretically can cause ACAG in individuals with narrow iridocorneal angle.55 However, no case of gentamicine-induced glaucoma has been reported yet.
Central nervous system agents
Antidepressants
Antidepressants are used in the treatment of psychoneurotic anxiety or depressive reactions. Selective serotonin reuptake inhibitors (SSRI) are increasingly the first line choice of antidepressant because of their tolerable side-effect profile and low rate of lethality, if taken in an overdose. They act by producing a gradual increase in postsynaptic levels of serotonin. The patho-physiological mechanism of SSRI-induced ACAG remains unclear; although anticholinergic effects or increased levels of serotonin, which cause partial pupillary dilatation, and increased aqueous production secondary to increased ciliary body blood flow have been implicated.56, 57 The cause of ACAG in other groups of antidepressants is induced mydriasis by anticholinergic action of these medications in patients with narrow iridocorneal angle. Of tricyclic agents, amitryptiline (the most commonly reported agent) and imipramine58 and of the non-tricyclic drugs, mianserin hydrochloride,59 paroxetine,57, 60 fluoxetine,61 maprotiline,62, 63 fluvoxamine,64 venlafaxine,65, 66 citalopram,67 and escitalopram68 have been documented to be associated with ACAG attacks. Ritch et al58 reported development of ACAG in four patients with occludable angles who received routinely prescribed doses of imipramine.
Monoamine oxidase inhibitors, another group of antidepressant agents, have weak anticholinergic effect. Phenelzine sulfate and tranylcypromine sulfate have been reported to produce CAG.69
Antipsychotics
Compared with tricyclic antidepressants, antipsychotics have a relatively weaker anticholinergic action and lower possibility of inducing CAG.70 Among the available antipsychotic agents, perphenazine, trifluperazine, and fluphenazine have been reported to induce ACAG.37, 69, 71 The anticholinergic effects—blurred vision, mydriasis, and decreased accommodation are more likely to occur with concomitant use of anti-Parkinsonian's agents and care in the use of this drug combination should be taken in patients with narrow angles.16
Benzodiazepines
The benzodiazepines are a group of compounds with related chemical structure that exert a therapeutic effect via binding to a site on the γ-aminobutyric acid (GABA) receptor complex and enhancing the inhibition that occurs when GABA binds to its receptor.72 They are effective in the management of psychoneurotic states manifested by anxiety, tension, or agitation. They are also used as adjunctive therapy in the relief of skeletal muscle spasms and as preoperative medications. Theoretically, these agents can induce ACAG, because they induce relaxation of the sphincter muscle of the iris and have a mild anticholinergic effect.73 Diazepam was suspected as having caused ACAG in a case report, also clotiazepam and alprazolam in another case, but there is no other report of glaucoma induction by these agents.63, 74
Anti-Parkinsonians
Cabergoline, a dopamine D2 receptor agonist, is also prescribed in prolactin producing pituitary gland tumors, and dysfunctions associated with hyperprolactinemia has been reported to induce non-pupillary block ACAG associated with choroidal effusion 5 h after ingestion of a single tablet.75
Orphenadrine citrate, an anticholinergic agent used also for the treatment of muscle spasm, has been documented to precipitate ACAG.37
Trihexyphenidyl, also known as benzhexol, is an antimuscarinic, which has peripheral and central anticholineric activity. It has been shown to precipitate CAG in patients with occludable angles.76 Trihexyphenidyl has a mydriatic effect, which is about one-third as strong as that of an equal dose of atropine systemically. In addition to precipitating an ACAG attack, its prolonged cumulative effect may cause chronic CAG in susceptible individuals. Owing to cognitive deficits in some patients with Parkinson's disease, the diagnosis of the glaucoma may be delayed. Friedman and Neumann13 reported total blindness of one eye in two patients and legal blindness with tubular vision in one eye of a third patient that occurred as a result of CAG due to long-term treatment with trihexyphenidyl. It is, therefore, advisable to have gonioscopic evaluation in all patients who are to be put on trihexyphenidyl.13
Anticonvulsants
Topiramate, a sulfamate-substituted monosaccharide antiseizure medication, is also used in the management of migraine, depression, and neuropathic pain. It is also used off-label as a weight-reduction medication. More than 114 cases of topiramate-induced CAG have been reported in the literature. These usually occur within the first 2 weeks after starting topiramate therapy. In some cases, attacks develop within hours after doubling the dosage. Almost all cases are bilateral ACAG. In only three patients, attacks have been reported as unilateral. Glaucoma occurred between days 1 and 49, after drug initiation, with an average of 7 days. In a pilot study by Leung et al,77 it was shown that short-term use of topiramate did not induce asymptomatic angle narrowing. Therefore, it was suggested that topiramate-induced secondary CAG may be an all-or-none phenomenon. The most prevalent presenting symptom was blurred vision due to myopia. Acute myopia up to 6–8.5 diopters may occur in a matter of hours after starting this drug; however, it may take a number of weeks to resolve once the drug is discontinued. Seven patients sustained permanent vision loss.48, 49, 78, 79
Ecstasy (3, 4-methylenedioxymethamphetamine)
Ecstasy, a synthetic amphetamine derivate, and marijuana was implicated as the cause of recurrent bilateral ACAG in a 29-year-old woman.80 Ecstasy increases the release of monoamine neurotransmitters and inhibits the uptake of serotonin from the synaptic gap that can lead to mydriasis and ACAG in predisposed persons.
Respiratory system agents
Epinephrine used for asthmatics with severe symptoms, for epistaxis, and in cold remedies may cause mydriasis and precipitate CAG in predisposed individuals.20, 81, 82, 83
Ipratropium bromide, an anticholineric agent used to relive bronchoconstriction causes mydriasis and might precipitate an ACAG attack in susceptible individuals.3, 84, 85, 86 Three of five patients who developed ACAG after receiving ipratropium and salbutamol experienced bilateral ocular involvement.84
Tiotropium bromide, another anticholinergic agent, has weaker anticholinergic activity, but has been reported to induce ACAG.87 Ipratropium and tiotropium can be absorbed through the cornea and the conjunctiva in the nebulized form when the mask is not fitted properly.
The β-2 agonists relieve reversible bronchospasm in patients with asthma or chronic obstructive pulmonary disease by relaxing the smooth muscles of the bronchi. The β-2 adnergics can compound the problem of CAG secondary to anticholigergic agents’ mydriasis by increasing the production of aqueous humor.
Cocaine has indirect sympathomimetic activity and causes mydriasis. ACAG has been reported following therapeutic or abuse intranasal application of cocaine.88, 89
Cardiac agents
Disopyramide, an anticholinergic agent, is indicated for suppression and prevention of recurrence of cardiac arrhythmias. Owing to its anticholinergic activity, it may induce ACAG up to 3 weeks after the patient starts taking the medication.90, 91
Calcium channel blockers, though may be regarded as a neuroprotective and IOP reducing agent, have been reported to have incremental effect on the IOP.92, 93
Hematologic agents
Anticoagulants have been described as inducing massive spontaneous choroidal hemorrhages. This is an extremely rare event that cause ACAG in older patients (65–87 years old) receiving anticoagulants or thrombolytic agents. Systemic hypertension and generalized atherosclerosis are additional risk factors. In addition to overtreatment with anticoagulants, some ocular issues such as age-related macular degeneration with neovascularization and nanophthalmos are risk factors for this uncommon complication.94, 95, 96, 97, 98 Four patients with age-related macular degeneration who were on phenprocomoun or heparin developed unilateral ACAG after massive intraocular bleeding. Three of the four eyes were blind within a few months even with surgical evacuation of blood.99 Chandra et al98 reported a patient with history of atrophic age-related macular degeneration that was on warfarin with a therapeutic international normalized ratio and presented with CAG due to spontaneous suprachoroidal hemorrhage.
To manage increased IOP, anticoagulative agents should be discontinued (if the patient's medical condition allows) and treatment of CAG started. Consultation with patient's physician for alternative anticoagulative medicine may be necessary.100 Peripheral iridotomy is not effective because the mechanism is non-pupillary block CAG. Surgery may be needed to drain the choroidal effusion or evacuate the hemorrhage.97, 98 Evacuative sclerotomies may have value in the relief of pain and elevated IOP, but has not been shown to be beneficial in visual and anatomic outcomes.100, 101
Docetaxel and paclitaxel belong to a generation of anticancer agents used in the treatment of a variety of neoplastic diseases, primarily in the advanced stages. There is a report of a patient with breast cancer and diffuse bone metastasis who developed IOP elevation with docetaxel.102 She received docetaxel every 21 days. Before each cycle, she received premedication with 50 mg prednisolone 3 and 12 h before docetaxel. After the first cycle, she developed fluid retention and after the fifth cycle, she complained about loss of vision. She had an IOP of 44 mm Hg, but without any glaucomatous optic nerve or visual field abnormality. The mechanism of this IOP elevation is not determined. Although the authors stated that fluid retention could have been responsible for IOP elevation, the possibility of steroid-induced IOP elevation cannot be ruled out.
Imatinib mesylate is a selective inhibitor of the bcr-abl, c-kit, and platelet-derived growth factor receptor tryrosine kinases. This drug is an effective targeted therapy for patients with chronic myelogenous leukemia and gastrointestinal stromal tumors. In a case series on 104 patients, only one patient developed IOP elevation.103
Gastrointestinal agents
Spasmolytics, anticholinergic agents, are effective in the management of gastrointestinal tract spasticity and peptic ulcers. Although no case of CAG has been reported with these agents, dicyclomine and propantheline have been reported to increase the IOP in patients with open-angle glaucoma. The mechanism for this is not understood.104
Antihemmorhoidal suppositories may contain epinephrine compounds, which can precipitate ACAG in patients with narrow iridocorneal angle.3, 37
Scopolamine, an anticholinergic drug, used for treatment of intestinal cramping and its time-release discs dermatologic application for the treatment of motion sickness should be prescribed with caution in the susceptible patients.105, 106 In a double-masked randomized, placebo-controlled study on 40 patients with open angle who were on treatment regimens that included or excluded pilocarpine, transdermal scopolamine patches were prescribed. No statistically significant differences in IOP were detected for either group.107
Cimetidine and ranitidine, H2-blocker agents, have weak anticholinergic adverse effects, which may induce CAG in susceptible individuals. These have been documented to raise the IOP in one patient with glaucoma being treated for a duodenal ulcer.108 However, Cohen et al109 documented no effect on the IOP in any of four medically controlled glaucoma patients treated with intravenous infusion of cimetidine compared with the effect of a control infusion of normal saline.
Immune system agents
Antiallergic agents
Promethazine, an H1-blocker agent, has been shown to produce an idiopathic swelling of the lens that can induce ACAG.110 Although the possibility of inducing CAG with these agents is low because of their miniscule anticholinergic activity, they should be used with caution in at-risk patients.
Diphenhyramine used in the intravenous form has been regarded as a causative agent for ACAG and fexofenadine has been suggested as an alternative in patients at risk of CAG.111
Antiinflammatory agents
Mefenamic acid, a non-steroidal antiinflammatory agent, has been documented to induce secondary non-pupillary block CAG and −9.00 diopter myopia in a 30-year-old patient. This is the same clinical picture that occurs with sulfa drugs.112
Anesthetic agents
The majority of drugs used for general anesthesia cause a decrease in IOP.113 However, the induction of general anesthesia may be associated with an elevated IOP from laryngeal spasm and coughing associated with endotracheal intubation.114 Additionally, succinylcholine115 and ketamine116 have been documented to elevate IOP. This effect seems to be due to increased extraocular muscle tone from these drugs. The IOP elevation is temporary and has no harmful effect on the eye except in patients with ruptured globe. Avoidance of using these agents in this condition is the best preventive method.
Postoperative ACAG after non-ocular surgery has been reported after various procedures, including abdominal, orthopedic, facial, gynecologic, and endoscopic surgery.117, 118, 119, 120, 121 Several factors are likely to induce postoperative ACAG in predisposed individuals such as the use of anticholinergics (atropine, scopolamine, and muscle relaxants) and adrenergics (ephedrine and epinephrine). Moreover, the perioperative period carries the risk of psychological stress and darkness-induced mydriasis may increase the risk of glaucoma attacks.3, 118, 122 Owing to the patient's systemic early postoperative condition, the classic signs of ACAG may not be detected and the diagnosis can be delayed.
Conclusion
There are numerous reports of drug-induced glaucoma; however, controlled, comparison trials of agents involved in this subject are virtually non-existent and most data are obtained from case reports and case series. Although the results from these types of studies may be useful in developing instructions for the optimal use of these agents, controlled trials are required for establishing standard treatment instructions.
Drug-induced glaucoma is an issue that is preventable in many cases. The main mechanism is pupillary block CAG caused by the anticholinergic or adrenergic activity of systemic or topical drugs in patients with narrow iridocorneal angle. For this mechanism, prophylactic laser iridotomy in high-risk individuals offers protection against drug-induced glaucoma. The other mechanism is non-pupillary block CAG that occurs because of ciliary or suprachoroidal effusion, or even vitreous hemorrhage with forward movement of the iris–lens diaphragm. In contrast to the first mechanism where laser iridotomy is curative, in the latter group laser iridotomy is ineffective.
In the case of ACAG, the problem is to know which eye is at risk as the patients are unaware that they have narrow iridocorneal angles and the practitioner prescribing systemic medication are not able to detect at-risk patients. It is wise to send high-risk patients (hyperopic, having family history of glaucoma, being from a high-risk ethnicity such as Asian) for ophthalmic examination before commencing agents that have potential of inducing CAG. All in all, systemic and local drug effects may lead to open or more commonly CAG. Prompt recognition and appropriate treatment may help protect the vision of these susceptible patients and the clinician must be watchful of the potential to cause glaucoma associated with systemic medications that are necessary in the treatment of various systemic diseases.
References
Boland MV, Quigley HA . Risk factors and open-angle glaucoma: classification and application. J Glaucoma 2007; 16 (4): 406–418.
Tello C, Tran HV, Liebmann J, Ritch R . Angle closure: classification, concepts, and the role of ultrasound biomicroscopy in diagnosis and treatment. Semin Ophthalmol 2002; 17 (2): 69–78.
Lachkar Y, Bouassida W . Drug-induced acute angle closure glaucoma. Curr Opin Ophthalmol 2007; 18 (2): 129–133.
Nguyen N, Mora JS, Gaffney MM, Ma AS, Wong PC, Iwach AG et al. A high prevalence of occludable angles in a Vietnamese population. Ophthalmology 1996; 103 (9): 1426–1431.
Lowe RF . Primary angle-closure glaucoma. A review 5 years after bilateral surgery. Br J Ophthalmol 1973; 57 (7): 457–463.
Krupin T, Mitchell KB, Johnson MF, Becker B . The long-term effects of iridectomy for primary acute angle-closure glaucoma. Am J Ophthalmol 1978; 86 (4): 506–509.
Chew SS, Vasudevan S, Patel HY, Gurria LU, Kerr NM, Gamble G et al. Acute primary angle closure attack does not cause an increased cup-to-disc ratio. Ophthalmology 2011; 118 (2): 254–259.
Shen SY, Baskaran M, Fong AC, Chan YH, Lim LS, Husain R et al. Changes in the optic disc after acute primary angle closure. Ophthalmology 2006; 113 (6): 924–929.
Wong IY, Yuen NS, Chan CW . Retinal nerve fiber layer thickness after a single attack of primary acute angle-closure glaucoma measured with optical coherence tomography. Ophthalmic Surg Lasers Imaging 2010; 41 (1): 96–99.
Fang AW, Qu J, Li LP, Ji BL . Measurement of retinal nerve fiber layer in primary acute angle closure glaucoma by optical coherence tomography. J Glaucoma 2007; 16 (2): 178–184.
Quigley HA . Angle-closure glaucoma-simpler answers to complex mechanisms: LXVI Edward Jackson Memorial Lecture. Am J Ophthalmol 2009; 148 (5): 657–669 e651.
Bruno CA, Alward WL . Gonioscopy in primary angle closure glaucoma. Semin Ophthalmol 2002; 17 (2): 59–68.
Friedman Z, Neumann E . Benzhexol-induced blindness in Parkinson's disease. Br Med J 1972; 1 (5800): 605.
Razeghinejad MR, Myers JS, Katz LJ . Iatrogenic glaucoma secondary to medications. Am J Med 2011; 124 (1): 20–25.
Ritch R, Lowe R . Angle-closure glaucoma: clinical types. In: Ritch R, Shields M, Krupin T (eds). The Glaucomas. Mosby: St Louis, 1996, pp 829–830.
Fraunfelder FT, Fraunfelder FW, Chambers WA . Clinical Ocular Toxicology, 1st ed. Saunders Elsevier: China, 2008.
Rieser JC, Schwartz B . Miotic-induced malignant glaucoma. Arch Ophthalmol 1972; 87 (6): 706–712.
Wolfs RC, Grobbee DE, Hofman A, de Jong PT . Risk of acute angle-closure glaucoma after diagnostic mydriasis in nonselected subjects: the Rotterdam Study. Invest Ophthalmol Vis Sci 1997; 38 (12): 2683–2687.
Patel KH, Javitt JC, Tielsch JM, Street DA, Katz J, Quigley HA et al. Incidence of acute angle-closure glaucoma after pharmacologic mydriasis. Am J Ophthalmol 1995; 120 (6): 709–717.
Zenzen CT, Eliott D, Balok EM, Watnick RL, German P . Acute angle-closure glaucoma associated with intranasal phenylephrine to treat epistaxis. Arch Ophthalmol 2004; 122 (4): 655–656.
Yalvac IS, Tamcelik N, Duman S . Acute angle-closure glaucoma associated with latanoprost. Jpn J Ophthalmol 2003; 47 (5): 530–531.
Sakai H, Sakima N, Nakamura Y, Hayakawa K, Sawaguchi S . Ciliochoroidal effusion induced by topical latanoprost in a patient with sturge-weber syndrome. Jpn J Ophthalmol 2002; 46 (5): 553–555.
Fan JT, Johnson DH, Burk RR . Transient myopia, angle-closure glaucoma, and choroidal detachment after oral acetazolamide. Am J Ophthalmol 1993; 115 (6): 813–814.
Aptel F, Denis P . Optical coherence tomography quantitative analysis of iris volume changes after pharmacologic mydriasis. Ophthalmology 2010; 117 (1): 3–10.
Pandit RJ, Taylor R . Mydriasis and glaucoma: exploding the myth. A systematic review. Diabet Med 2000; 17 (10): 693–699.
Mapstone R . Dilating dangerous pupils. Br J Ophthalmol 1977; 61 (8): 517–524.
Portney GL, Purcell TW . The influence of tropicamide on intraocular pressure. Ann Ophthalmol 1975; 7 (1): 31–34.
Harris LS . Cycloplegic-induced intraocular pressure elevations a study of normal and open-angle glaucomatous eyes. Arch Ophthalmol 1968; 79 (3): 242–246.
Velasco Cabrera J, Eiroa Mozos P, Garcia Sanchez J, Bermudez Rodriguez F . Changes in intraocular pressure due to cycloplegia. CLAO J 1998; 24 (2): 111–114.
Valle O . The cyclopentolate provocative test in suspected or untreated open-angle glaucoma. I. Effect on intraocular pressure. Acta Ophthalmol (Copenh) 1976; 54 (4): 456–472.
Holland SP, Morck DW, Lee TL . Update on toxic anterior segment syndrome. Curr Opin Ophthalmol 2007; 18 (1): 4–8.
Sugar HS, Airala MA . Introduction of some ophthalmic atropine ointments into the anterior chamber. Ann Ophthalmol 1972; 4 (5): 367–374.
Corridan P, Nightingale S, Mashoudi N, Williams AC . Acute angle-closure glaucoma following botulinum toxin injection for blepharospasm. Br J Ophthalmol 1990; 74 (5): 309–310.
Ichhpujani P, Jindal A, Jay Katz L . Silicone oil induced glaucoma: a review. Graefes Arch Clin Exp Ophthalmol 2009; 247 (12): 1585–1593.
Honavar SG, Goyal M, Majji AB, Sen PK, Naduvilath T, Dandona L . Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology 1999; 106 (1): 169–176; discussion 177.
Moisseiev J, Barak A, Manaim T, Treister G . Removal of silicone oil in the management of glaucoma in eyes with emulsified silicone. Retina 1993; 13 (4): 290–295.
Mandelkorn RM . Drug-induced glaucoma. In: Zimmerman TJ, Kooner KS (eds). Clinical Pathways in Glaucoma, 1st edn. Thieme: New York, 2001, pp 333–350.
Bissen-Miyajima H . Ophthalmic viscosurgical devices. Curr Opin Ophthalmol 2008; 19 (1): 50–54.
Waseem M, Rustam N, Qamar ul I . Intraocular pressure after phacoemulsification using hydroxypropyl methylcellulose and sodium hyaluronate as viscoelastics. J Ayub Med Coll Abbottabad 2007; 19 (1): 42–45.
Kocak-Altintas AG, Anayol MA, Cakmak HB, Simsek S . Effects of topical dorzolamide on IOP after phacoemulsification with different types of ophthalmic viscosurgical devices. Eur J Ophthalmol 2007; 17 (1): 38–44.
Maddalena MA . Transient myopia associated with acute glaucoma and retinal edema following vaginal administration of sulfanilamide. Arch Ophthalmol 1968; 80 (2): 186–188.
Spadoni VS, Pizzol MM, Muniz CH, Melamed J, Fortes Filho JB . [Bilateral angle-closure glaucoma induced by trimetoprim and sulfamethoxazole combination: case report]. Arq Bras Oftalmol 2007; 70 (3): 517–520.
Sankar PS, Pasquale LR, Grosskreutz CL . Uveal effusion and secondary angle-closure glaucoma associated with topiramate use. Arch Ophthalmol 2001; 119 (8): 1210–1211.
Hook SR, Holladay JT, Prager TC, Goosey JD . Transient myopia induced by sulfonamides. Am J Ophthalmol 1986; 101 (4): 495–496.
Beasley FJ . Transient myopia and retinal edema during hydrochlorothiazide (hydrodiuril) therapy. Arch Ophthalmol 1961; 65: 212–213.
Segal A, Aisemberg A, Ducasse A . Quinine, transient myopia and angle-closure glaucoma. Bull Soc Ophtalmol Fr 1983; 83 (2): 247–249.
Edwards TS . Transient myopia due to tetracycline. JAMA 1963; 186: 69–70.
Fraunfelder FW, Fraunfelder FT . Adverse ocular drug reactions recently identified by the National Registry of Drug-Induced Ocular Side Effects. Ophthalmology 2004; 111 (7): 1275–1279.
Slatore CG, Tilles SA . Sulfonamide hypersensitivity. Immunol Allergy Clin North Am 2004; 24 (3): 477–490.
Rauscher FM, Parrish II RK . Atypical angle closures. Curr Opin Ophthalmol 2008; 19 (2): 107–114.
Ponka D . Approach to managing patients with sulfa allergy: use of antibiotic and nonantibiotic sulfonamides. Can Fam Physician 2006; 52 (11): 1434–1438.
Rhee DJ, Ramos-Esteban JC, Nipper KS . Rapid resolution of topiramate-induced angle-closure glaucoma with methylprednisolone and mannitol. Am J Ophthalmol 2006; 141 (6): 1133–1134.
Postel EA, Assalian A, Epstein DL . Drug-induced transient myopia and angle-closure glaucoma associated with supraciliary choroidal effusion. Am J Ophthalmol 1996; 122 (1): 110–112.
Parikh R, Parikh S, Das S, Thomas R . Choroidal drainage in the management of acute angle closure after topiramate toxicity. J Glaucoma 2007; 16 (8): 691–693.
Awan KJ . Mydriasis and conjunctival paresthesia from local gentamicin. Am J Ophthalmol 1985; 99 (6): 723–724.
Tripathi RC, Tripathi BJ, Haggerty C . Drug-induced glaucomas: mechanism and management. Drug Saf 2003; 26 (11): 749–767.
Costagliola C, Parmeggiani F, Sebastiani A . SSRIs and intraocular pressure modifications: evidence, therapeutic implications and possible mechanisms. CNS Drugs 2004; 18 (8): 475–484.
Ritch R, Krupin T, Henry C, Kurata F . Oral imipramine and acute angle closure glaucoma. Arch Ophthalmol 1994; 112 (1): 67–68.
Kinek M . Glaucoma following the antidepressant mianserin. Harefuah 1990; 118 (12): 699–700.
Lewis CF, DeQuardo JR, DuBose C, Tandon R . Acute angle-closure glaucoma and paroxetine [2]. J Clin Psychiatry 1997; 58 (3): 123–124.
Ahmad S . Fluoxetine and glaucoma. DICP 1991; 25 (4): 436.
Kadoi C, Hayasaka S, Tsukamoto E, Matsumoto M, Hayasaka Y, Nagaki Y . Bilateral angle closure glaucoma and visual loss precipitated by antidepressant and antianxiety agents in a patient with depression. Ophthalmologica 2000; 214 (5): 360–361.
Kadoi C, Hayasaka S, Tsukamoto E, Matsumoto M, Hayasaka Y, Nagaki Y . Bilateral angle closure glaucoma and visual loss precipitated by antidepressant and antianxiety agents in a patient with depression. Ophthalmologica 2000; 214 (5): 360–361.
Jimenez-Jimenez FJ, Orti-Pareja M, Zurdo JM . Aggravation of glaucoma with fluvoxamine. Ann Pharmacother 2001; 35 (12): 1565–1566.
Aragona M, Inghilleri M . Increased ocular pressure in two patients with narrow angle glaucoma treated with venlafaxine. Clin Neuropharmacol 1998; 21 (2): 130–131.
de Guzman MH, Thiagalingam S, Ong PY, Goldberg I . Bilateral acute angle closure caused by supraciliary effusions associated with venlafaxine intake. Med J Aust 2005; 182 (3): 121–123.
Croos R, Thirumalai S, Hassan S, Davis Jda R . Citalopram associated with acute angle-closure glaucoma: case report. BMC Ophthalmol 2005; 5: 23.
Zelefsky JR, Fine HF, Rubinstein VJ, Hsu IS, Finger PT . Escitalopram-induced uveal effusions and bilateral angle closure glaucoma. Am J Ophthalmol 2006; 141 (6): 1144–1147.
Davidson SI . Reports of ocular adverse reactions. Trans Ophthalmol Soc UK 1973; 93 (0): 495–510.
Oshika T . Ocular adverse effects of neuropsychiatric agents. Incidence and management. Drug Saf 1995; 12 (4): 256–263.
Fornaro M, Venuti S, Pompei F, Gabrielli F, Fornaro P . Ophthalmological side effects of antipsychotic agents. Minerva Psichiatr 2006; 47 (2): 129–142.
Krystal AD . A compendium of placebo-controlled trials of the risks/benefits of pharmacological treatments for insomnia: the empirical basis for U.S. clinical practice. Sleep Med Rev 2009; 13 (4): 265–274.
Malone Jr DA, Camara EG, Krug Jr JH . Ophthalmologic effects of psychotropic medications. Psychosomatics 1992; 33 (3): 271–277.
Hyams SW, Keroub C . Glaucoma due to diazepam. Am J Psychiatry 1977; 134 (4): 447–448.
Razmjoo H, Rezaei L, Dehghani A, Peyman A, Akhlaghi M . Bilateral angle-closure glaucoma in a young female receiving cabergoline: a case report. Case Report Ophthalmol 2011; 2 (1): 30–33.
Edwards CE, O’Doherty DS . Anti-Parkinson drugs and their relationship to glaucoma. Bull Georgetown Univ Med Cent 1958; 12 (1): 15–16.
Leung DY, Leung H, Baig N, Kwan P, Kwong YY, Wong KS et al. Topiramate and asymptomatic ocular angle narrowing: a prospective pilot study. Eye (Lond) 2009; 23 (11): 2079–2081.
Thambi L, Kapcala LP, Chambers W, Nourjah P, Beitz J, Chen M et al. Topiramate-associated secondary angle-closure glaucoma: a case series. Arch Ophthalmol 2002; 120 (8): 1108.
Richa S, Yazbek JC . Ocular adverse effects of common psychotropic agents: a review. CNS Drugs 2010; 24 (6): 501–526.
Trittibach P, Frueh BE, Goldblum D . Bilateral angle-closure glaucoma after combined consumption of ‘ecstasy’ and marijuana. Am J Emerg Med 2005; 23 (6): 813–814.
Sharma R, Waldock A . Bilateral acute angle closure glaucoma following administration of oral pseudoephedrine for sinusitis. Asian J Ophthalmol 2007; 9 (2): 87–88.
Khan MA, Watt LL, Hugkulstone CE . Bilateral acute angle-closure glaucoma after use of Fenox nasal drops. Eye (Lond) 2002; 16 (5): 662–663.
Rudkin AK, Gray TL, Awadalla M, Craig JE . Bilateral simultaneous acute angle closure glaucoma precipitated by non-prescription cold and flu medication. Emerg Med Australas 2010; 22 (5): 477–479.
Shah P, Dhurjon L, Metcalfe T, Gibson JM . Acute angle closure glaucoma associated with nebulised ipratropium bromide and salbutamol. BMJ 1992; 304 (6818): 40–41.
Cox AR, Gilmartin B . Drug-induced ophthalmic adverse reactions. Adverse Drug React Bull 2006; (241): 923–926.
Ortiz Rambla J, Hidalgo Mora JJ, Gascón Ramón G, Navarro Arambudo B . Acute angle-closure glaucoma and ipratropium bromide [1]. Med Clin 2005; 124 (20): 795.
Oksuz H, Tamer C, Akoglu S, Duru M . Acute angle-closure glaucoma precipitated by local tiotropium absorption. Pulm Pharmacol Ther 2007; 20 (6): 627–628.
Hari CK, Roblin DG, Clayton MI, Nair RG . Acute angle closure glaucoma precipitated by intranasal application of cocaine. J Laryngol Otol 1999; 113 (3): 250–251.
Mitchell JD, Schwartz AL . Acute angle-closure glaucoma associated with intranasal cocaine abuse. Am J Ophthalmol 1996; 122 (3): 425–426.
Ahmad S . Disopyramide: pulmonary complications and glaucoma. Mayo Clin Proc 1990; 65 (7): 1030–1031.
Trope GE, Hind VM . Closed-angle glaucoma in patient on disopyramide. Lancet 1978; 1 (8059): 329.
Monica ML, Hesse RJ, Messerli FH . The effect of a calcium-channel blocking agent on intraocular pressure. Am J Ophthalmol 1983; 96 (6): 814.
Beatty JF, Krupin T, Nichols PF, Becker B . Elevation of intraocular pressure by calcium channel blockers. Arch Ophthalmol 1984; 102 (7): 1072–1076.
Asensio Sanchez VM, Perez Flandez FJ, Carlos Bejarano J, Merino Nunez F . Suprachoroidal haemorrhage and acute glaucoma associated with systemic fibrinolysis. Arch Soc Esp Oftalmol 2002; 77 (8): 459–461.
Chorich LJ, Derick RJ, Chambers RB, Cahill KV, Quartetti EJ, Fry JA et al. Hemorrhagic ocular complications associated with the use of systemic thrombolytic agents. Ophthalmology 1998; 105 (3): 428–431.
Khawly JA, Ferrone PJ, Holck DE . Choroidal hemorrhage associated with systemic tissue plasminogen activator. Am J Ophthalmol 1996; 121 (5): 577–578.
Caronia RM, Sturm RT, Fastenberg DM, Berke SJ, Weintraub J . Bilateral secondary angle-closure glaucoma as a complication of anticoagulation in a nanophthalmic patient. Am J Ophthalmol 1998; 126 (2): 307–309.
Chandra A, Barsam A, Hugkulstone C . A spontaneous suprachoroidal haemorrhage: a case report. Cases J 2009; 2: 185.
Schlote T, Freudenthaler N, Gelisken F . Anticoagulative therapy in patients with exudative age-related macular degeneration: acute angle closure glaucoma after massive intraocular hemorrhage. Ophthalmologe 2005; 102 (11): 1090–1096.
Pesin SR, Katz LJ, Augsburger JJ, Chien AM, Eagle Jr RC . Acute angle-closure glaucoma from spontaneous massive hemorrhagic retinal or choroidal detachment. An updated diagnostic and therapeutic approach. Ophthalmology 1990; 97 (1): 76–84.
De Marco R, Aurilia P, Mele A . Massive spontaneous choroidal hemorrhage in a patient with chronic renal failure and coronary artery disease treated with Plavix. Eur J Ophthalmol 2009; 19 (5): 883–886.
Fabre-Guillevin E, Tchen N, Anibali-Charpiat MF, Calluaud L, Ravaud A . Taxane-induced glaucoma. Lancet 1999; 354 (9185): 1181–1182.
Fraunfelder FW, Solomon J, Druker BJ, Esmaeli B, Kuyl J . Ocular side-effects associated with imatinib mesylate (Gleevec®). J Ocul Pharmacol Ther 2003; 19 (4): 371–375.
Mody MV, Keeney AH . Propantheline (pro-banthine) bromide in relation to normal and gluacomatous eyes; effects on intraocular tension and pupillary size. J Am Med Assoc 1955; 159 (11): 1113–1114.
Hamill MB, Suelflow JA, Smith JA . Transdermal scopolamine delivery system (TRANSDERM-V) and acute angle-closure glaucoma. Ann Ophthalmol 1983; 15 (11): 1011–1012.
Fraunfelder FT . Transdermal scopolamine precipitating narrow-angle glaucoma. N Engl J Med 1982; 307 (17): 1079.
Maus TL, Larsson LI, Brubaker RF . Ocular effects of scopolamine dermal patch in open-angle glaucoma. J Glaucoma 1994; 3 (3): 190.
Dobrilla G, Felder M, Chilovi F, de Pretis G . Exacerbation of glaucoma associated with both cimetidine and ranitidine. Lancet 1982; 1 (8280): 1078.
Cohen MM, Feldman F, Clark L, Hudy D . Effect of cimetidine on intraocular pressure in patients with glaucoma. Can J Ophthalmol 1984; 19 (5): 212–214.
Bard LA . Transient myopia associated with promethazine (phenegan) therapy: report of a case. Am J Ophthalmol 1964; 58: 682–686.
Komatsubara K, Miyoshi K, Kogure Y, Matsuhisa T, Eguchi H . Administration of premedication with fexofenadine for paclitaxel-induced hypersensitive reactions in breast cancer patients complicated with closed-angle glaucoma. Gan To Kagaku Ryoho 2010; 37 (1): 107–110.
Vishwakarma P, Raman GV, Sathyan P . Mefenamic acid-induced bilateral transient myopia, secondary angle closure glaucoma and choroidal detachment. Indian J Ophthalmol 2009; 57 (5): 398–400.
Murphy DF . Anesthesia and intraocular pressure. Anesth Analg 1985; 64 (5): 520–530.
Duncalf D . Anesthesia and intraocular pressure. Bull N Y Acad Med 1975; 51 (3): 374–381.
Khosravi MB, Lahsaee M, Azemati S, Eghbal MH . Intraocular pressure changes after succinylcholine and endotracheal intubation: a comparison of thiopental and propofol on IOP. Indian J Ophthalmol 2007; 55 (2): 164.
Nagdeve NG, Yaddanapudi S, Pandav SS . The effect of different doses of ketamine on intraocular pressure in anesthetized children. J Pediatr Ophthalmol Strabismus 2006; 43 (4): 219–223.
Rosenberg M . Ocular injuries during general anesthesia. J Oral Surg 1981; 39 (12): 945–947.
Fazio DT, Bateman JB, Christensen RE . Acute angle-closure glaucoma associated with surgical anesthesia. Arch Ophthalmol 1985; 103 (3): 360–362.
Ujino H, Morimoto O, Yukioka H, Fujimori M . [Acute angle-closure glaucoma after total hip replacement surgery]. Masui 1997; 46 (6): 823–826.
Eldor J, Admoni M . Acute glaucoma following nonophthalmic surgery. Isr J Med Sci 1989; 25 (11): 652–654.
Garcia MP, Gomez ME, Carrion JM, Huertas FR . Acute closed-angle glaucoma after gynecological surgery under general anesthesia. Rev Esp Anestesiol Reanim 2007; 54 (9): 572–573.
Lentschener C, Ghimouz A, Bonnichon P, Parc C, Ozier Y . Acute postoperative glaucoma after nonocular surgery remains a diagnostic challenge. Anesth Analg 2002; 94 (4): 1034–1035.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Razeghinejad, M., Pro, M. & Katz, L. Non-steroidal drug-induced glaucoma. Eye 25, 971–980 (2011). https://doi.org/10.1038/eye.2011.128
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.128
Keywords
This article is cited by
-
Bilateral exudative retinal detachments and associated choroidal detachments in a patient on dapsone: a case report
International Journal of Retina and Vitreous (2022)
-
Gene network analyses unveil possible molecular basis underlying drug-induced glaucoma
BMC Medical Genomics (2021)
-
Psychotropic Drug-Induced Glaucoma: A Practical Guide to Diagnosis and Management
CNS Drugs (2021)
-
Benzodiazepine Use and Risk of Acute Angle-Closure Glaucoma: A Population-Based Case-Crossover Study
Drug Safety (2020)
-
The change in intraocular pressure after pupillary dilation in eyes with pseudoexfoliation glaucoma, primary open angle glaucoma, and eyes of normal subjects
International Ophthalmology (2015)