Abstract
Aim
The aim of this study is to determine the outcomes following referral for glaucoma from routine optometric practice and the positive predictive value (PPV).
Methods
A prospective study of 441 referrals for glaucoma in the Portsmouth area was performed over 6 months. A positive outcome was defined when the patient had the diagnosis of glaucoma made or if there was a high index of suspicion of glaucoma requiring follow-up. The PPV was determined from positive outcome number/referral number.
Results
The overall PPV was 0.37 (95% confidence interval 0.33–0.42). Open-angle glaucoma (OAG) was confirmed in 33 (7%) patients. A diagnosis of ocular hypertension was made in 49 (11%) patients and glaucoma suspect in 92 (21%) referrals. Two-thirds of optometrists recorded all 3 assessments: fields, intraocular pressure (IOP) and disc appearance, a figure representing 293 referrals (PPV 0.37). However the greatest referral accuracy was seen when only discs and IOPs were recorded (PPV 0.47). When all three tests were given as reasons for suspicion for glaucoma, the PPV was 0.71. The number of patients diagnosed with OAG from Portsea Island during the study period was 7, whereas the expected number of diagnosed patients was 29.
Conclusion
Wider use of perimetry by optometrists and increased reporting of all three tests has not led to an increase in PPV. There remain a considerable number of undiagnosed patients with glaucoma in the population.
Similar content being viewed by others
Introduction
Glaucomatous neuropathy is often an insidious disease with no symptoms until the advanced stages are reached.1 As the neuropathy is irreversible, early detection is important. Currently, this detection is through the community optometrists from whom almost all referrals to the hospital eye service in the United Kingdom originate.2 Although the National Health Service provides a free eye test to all those who are above the age of 60 years, many people do not visit their local optometrist. Far from being a screening process, the methods used can best be described as ‘opportunistic’ with a variable number of tests performed of differing accuracy. As a consequence, there is considerable potential for both the yield of false positives and for missing pathology: it is estimated that 50% of glaucoma cases in the community are undetected.3
The accuracy of optometrist referral has been examined by a number of studies.4, 5, 6, 7, 8 In 1999 Theodossiades and Murdoch4 found the positive predictive value (PPV) for glaucoma (the number of patients requiring follow-up with glaucoma or a high index of suspicion of glaucoma/number referred) of 0.43. Other studies have reported an increase in referral number with no change in accuracy after intensive training of optometrists, suggesting an increase in pick-up rate.9, 10
We aimed to determine the diagnostic accuracy of referrals for glaucoma from optometrists to our department over a 6-month period. The goal was to look at both the PPV and to compare the expected incidence of open-angle glaucoma (OAG) with the observed incidence.
Materials and methods
All referrals made for the suspicion of glaucoma over a 6-month period were assessed prospectively. Existing or previously diagnosed patients with glaucoma were excluded. Evaluation in the outpatient clinic included history, distance visual acuity, full threshold automated Humphrey visual field analysis, Goldmann applanation tonometry, central corneal thickness measurement, and assessment of the optic disc with slit lamp biomicroscopy through dilated pupils. Referral information with regard to the reasons for referral and the tests performed were recorded. The outcomes after the clinic visit were noted. A positive outcome was defined when the patient had the diagnosis of glaucoma made or if there was a high index of suspicion of glaucoma requiring follow-up. A negative outcome was defined when the patient was discharged or had a different diagnosis unrelated to glaucoma.
The diagnoses were classified as follows:
-
OAG—pathological optic disc changes, visual field loss, open angle on gonioscopy, no other secondary glaucoma findings.
-
Angle-closure glaucoma—closed or occludable angle on gonioscopy and glaucomatous optic neuropathy.
-
Ocular hypertension (OHT)—IOP >21 mm Hg on two separate occasions with normal discs and visual fields and an open angle on gonioscopy.
-
Glaucoma suspect—the patient did not fall clearly under any diagnostic category but the suspicion for glaucoma was high enough to warrant follow-up, for example, ‘glaucoma-like optic discs’.
-
Normal—no evidence of glaucoma and an IOP <22 mm Hg. Other—the patient received a diagnosis that was different from that mentioned above.
Patients diagnosed with OHT requiring follow-up or labelled as a glaucoma suspect were considered as positive outcomes as it was felt appropriate that these patients should be examined by an ophthalmologist.
To compare observed incidence of glaucoma with the expected incidence, the Tuck-Crick predictive equation was used,11 an equation that intended to relate only to ‘definite’ OAG. The Tuck-Crick predictive equation was applied to the demographic data of the population of Portsea Island (taken from the 2001 census) to derive the expected incidence.12, 13
Results
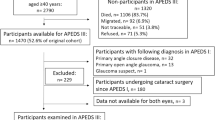
In total, 454 new referrals were collected over the 6-month period. The survey included all referrals for glaucoma in the Portsmouth area including Portsea Island. There were no glaucoma referrals through the private system during this period. Eleven patients did not attend for their outpatient appointment or were lost to follow-up. In two referrals by GPs, the optometrist's letter was not attached. These 13 were excluded from the study and analysis was performed on the remaining 441.
Age and sex of referrals
The patients’ ages ranged from 22 to 92 years. Most patients were in their 60s and 70s (105 of 441 and 115 of 441, respectively). The median age at referral was 64 years and 57% (252 of 441) were female. The median age of the 165 patients requiring follow-up was 67 years. Of those patients requiring follow-up, 93 of 165 (56%) were female.
Referral outcome
In all, 165 referrals (37%) resulted in a positive outcome and 276 (63%) resulted in a negative outcome. Out of all 441 referrals, 49 (11%) patients were diagnosed with OHT after their second visit. Of these, 19 (39%) had been discharged, 12 (24%) had been put on treatment, 14 (29%) were followed up without treatment, and 4 were lost to follow-up (8%). The diagnoses made after consultation are summarised in Table 1. The PPV following optometrist referral is 0.37 (165/441). With a 95% confidence interval, this value falls between 0.33 and 0.42.
Referral information
Of the 441 referral letters, 293 (66%) reported information on the triad of discs fields and IOP (Figure 1). Discs and pressures only were reported in 97 (22%) letters. Fields and IOP were reported in 23 (5%) letters. Discs and fields were reported in 3 (1%). Twenty-five (6%) referral letters reported IOP only. Those referrals containing information on the IOP and disc appearance resulted in the highest PPV (47%).
Reasons for referral
Altogether 71% (315 of 441) of the referrals were made on a single suspicious reason (Figure 2). A single finding of raised IOP was the commonest reason for referral, seen in 140 of 441 (32%) of referrals. The highest PPV was seen when all three test (IOP, disc appearance, and fields) were given as reasons for suspicion of glaucoma (71%). In all, 46 (10%) referrals also included a family history of glaucoma. Of these, 16 (35%) resulted in a positive outcome.
Observed and expected incidence of OAG
A total of 33 patients were diagnosed with OAG (7%). Of these, 10 lived on Portsea Island. With a population of 59 284 derived from the 2001 census figures, the expected incidence for OAG on Portsea Island was 29 new patients over the 6-month period.
Discussion
Glaucoma is an important disease to detect. It is the main cause of irreversible blindness in the world.14 However, with a prevalence of between 1 and 3% detection is tricky. Even tests with relatively high sensitivity and specificity will yield low PPVs if the prevalence is at this level.15 For example, if a test has a specificity of 98% and sensitivity of 98% the PPV with a prevalence of 2% will be 0.49. In our series, the PPV for glaucoma was 0.37. This number is less than recent those of previous studies performed over the past 10 years,2, 4, 5, 6, 8 but identical to the PPV found by Vernon examining a series in 1993.7
In total, 66% of referrals reported information on all the three tests: IOP, disc appearance, and fields. This number is considerably greater than those found by Theodossiades and Murdoch, in which only 15% of referrals reported all the three parameters.4 Logic suggests and studies report that more the information gathered the higher the PPV.4, 5 In our study in which optometrists gave all the three tests as reasons for referral, PPV was highest (71%). However, the act of performing and recording all the three test results did not lead to the highest PPV. On the contrary, the subset of referrals reporting on only discs and pressures had a higher PPV (47%) compared with the proportion reporting on the triad of tests (37%). Why should this be? Is it that those patients who had only the two tests performed had more advanced disease, or did the optometrists who performed all three tests have a lower threshold for referral? Vernon postulates a ‘two-hit’ hypothesis whereby a ‘positive’ test no matter how minor will influence the assessment of remaining tests resulting in a greater number of false positives.7 In our series, the proportion of referrals containing discs and pressures were diagnosed with a higher rate of OAG (11%) compared with those reporting the triad of tests (7%), but the numbers were too small for statistical testing.
An interesting and contentious issue is the role of perimetry in screening of glaucoma. As faster computerised perimeters have become available, field tests are increasingly used to screen for glaucoma.7 However, variability in the sensitivity and specificity between machines and inappropriate patient selection for testing can result in a high false-positive rate.16 Vernon has shown that routine field testing in a population of ⩾50 years of age results in the discovery of 10 patients with field defects from other causes for each patient with a glaucomatous defect.17 There have been attempts to improve field test accuracy by patient education before performing a field test; however, the results have been disappointing.18
Our results indicate that 72% of referrals have information on fields, a considerable difference from the 19% found by Theodossiades and Murdoch.4 One could therefore argue that it is no surprise that the PPV is one of the lowest reported value. To advocate that optometrists should not perform visual field testing, however, would result in missed diagnoses. For example, if the fields had not been performed in our series, the 19 positive referrals with abnormal fields given as a reason might not have been picked up.
Furthermore, the observed incidence of OAG from Portsea Island was less than half the expected, and although the numbers are small, this agrees with previous studies that 50% of glaucoma remains undetected. However, we do not know how many of the population of Portsea Island have visited their optometrists during the trial period and therefore cannot determine the false-negative rate for referrals.
To improve the false-positive rate while reducing the number of missed glaucoma patients in the community represents a major challenge. There is no single digital screening test, unlike, for example, the detection of diabetes mellitus using blood glucose measurements. Of those tests that are available, tonometry is the only digital test performed objectively; and on its own, tonometry is ineffective as a screening tool.19 Instead, we rely on optometrists to use their intuitive skills to interpret optic nerve appearance and field test results, in conjunction with tonometry.
Even then how these tests are performed can be variable. Dilated indirect ophthalmoscopy using slit lamp biomicroscopy is better at determining optic nerve head appearance than direct ophthalmoscopy through an undilated pupil, as it enables binocular assessment of depth.20 Applanation tonometry is the gold standard method of measuring IOP,21 and using an automated machine specifically designed for the detection of glaucomatous field defects reduces error.16 It is encouraging to see that in Scotland attempts at implementing these methods as part of the new GOS contract have had some positive effect on referral accuracy.8
Repetition of abnormal tests can improve referral accuracy.22 In this study, we do not know the number of times an abnormal test was repeated. It has been questioned whether repeat investigations can be funded within a single sight test. Indeed, cost-effectiveness of glaucoma screening remains difficult to ascertain.23 One possible alternative showing promise is the use of an intermediary specialist glaucoma optometrist to determine whether low-risk referrals warrant hospital referral.24
Certainly an area to be improved is communication, both between optometrist and ophthalmologist, and between ophthalmologist and optometrist. Scully et al25 found that 44% of referral letters for glaucoma were less than acceptable (defined as not including the referring practice details, the date of referral, patient details, visual acuity and refraction, optic disc evaluation, and IOP measurement). Whittaker et al26 found that ophthalmologists replied to optometrists in 16% (13/107) of referrals after patient consultation.
It is easy to forget that as clinicians we are exposed to patients with glaucoma every day, and that if there is a query about a patient, there is often another colleague to take advice from. In the optometry practices, many optometrists work alone and exposure to glaucoma is far less. Since this survey was undertaken in Portsmouth, we have started to encourage optometrists to spend time in the glaucoma clinic. Studies looking at whether intensive training improves referral accuracy have suggested that the referral rate increases but the PPV remains unchanged.9, 10 The authors suggest that more cases of glaucoma were detected, but the sample size was insufficient to provide a conclusive answer.
Areas of limitation in this study for which we do not have information include optometrist numbers, optometrist experience, and recorded information about patient ethnicity. It would also be interesting to investigate the PPV for specific diagnoses in future papers, for example, to determine diagnostic accuracy of referral for OHT.
Our study shows that the PPV for glaucoma remains unchanged over the past 10 years, whereas the number of optometrists performing perimetry has increased greatly. It will be difficult to drive the PPV higher in the face of low prevalence. Repetition of field tests and implementation of a contract similar to that in Scotland may help, but the question of funding will still arise.

References
Quigley HA . Open-angle glaucoma. N Engl J Med 1993; 328: 1097–1106.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR . An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol 1994; 1: 31–39.
Sheldrick JH, Sharp AJ . Glaucoma screening clinic in general practice: prevalence of occult disease, and resource implications. Br J Gen Prac 1994; 44: 561–565.
Theodossiades J, Murdoch I . Positive predictive value of optometrist-initiated referrals for glaucoma. Ophthal Physiol Opt 1999; 19 (1): 62–67.
Bell RWD, O’Brien C . The diagnostic outcome of new glaucoma referrals. Ophthal Physiol Opt 1997; 17 (1): 3–6.
Bowling B, Chen SDM, Salmon JF . Outcomes of referrals by community optometrists to a hospital glaucoma service. Br J Ophthalmol 2005; 89: 1102–1104.
Vernon SA . The changing pattern of glaucoma referrals by optometrists. Eye 1998; 12: 854–857.
Ang GS, Ng WS, Azuara-Blanco A . The influence of the new general services (GOS) contract in optometrist referrals for glaucoma and Scotland. Eye 2009; 123: 351–355.
Theodossiades J, Murdoch IE, Cousens S . Glaucoma case finding: a cluster-randomised intervention trial. Eye 2004; 18: 483–490.
Patel UDM, Murdoch IE, Theodossiades J . Glaucoma detection in the community: does ongoing training of optometrists have a lasting effect? Eye 2006; 20: 591–594.
Tuck MW, Crick RP . The projected increase in glaucoma due to an aging population. Ophthal Physiol Opt 2003; 23: 175–179.
The 2001 census (http://www.portsmouth.gov.uk/media/Age_and_gender_Portsmouth_and_Wards.pdf).
Leske C, Ederer F, Podgor M . Estimating incidence from age-specific prevalence in glaucoma. Am J Epidemdiol 1981; 113 (5): 606–613.
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82: 844–851.
Grimes DA, Schulz KF . Uses and abuses of screening tests. Lancet 2002; 359 (9309): 881–884.
Newman DK, Anwar S, Jordan K . Glaucoma screening by optometrists: positive predictive value of visual field testing. Eye 1998; 12: 921–924.
Vernon SA, Henry DJ, Cater L, Jones SJ . Screening for glaucoma in the community by non-ophthalmologically trained staff using semi-automated equipment. Eye 1990; 4: 88–97.
Manoj B, Rathod D, Austin MV . Does patient education result in more reliable initial visual fields? In: Henson DB, Wall M, eds. Perimetery Update 2002/03. Kugler: Amsterdam, 2003, pp 47–51.
Tielsch JM, Katz J, Singh K, Quigley H, Gottsch J, Javitt J et al. A population-based evaluation of glaucoma screening: the Baltimore eye study. Am J Epidemiol 1991; 134 (10): 1102–1110.
Kirwan JF, Gouws P, Linnell AE, Crowston J, Bunce C . Pharmacological mydriasis and optic disc examination. Br J Ophthalmol 2000; 84 (8): 894–898.
Kniestedt C, Punjabi O, Lin S, Stamper RL . Tonometry through the ages. Surv Ophthalmol 2008; 53 (6): 568–591.
Bell RWD, O’Brien C . Accuracy of referral to a glaucoma clinic. Ophthal Physiol Opt 1997; 17 (1): 7–11.
Hernandez R, Burr JM, Vale LD . Economic evaluation of screening for open-angle glaucoma. Int J Technol Assess Health Care 2008; 24 (2): 203–211.
Bourne RRA, French KA, Chang L, Borman AD, Hingorani M, Newsom WD . Can an optometrist-based referral refinement scheme reduce false-positive glaucoma hospital referrals without compromising quality of care? The community and hospital allied network glaucoma evaluation scheme (CHANGES). Eye 2009; 24 (5): 881–887.
Scully ND, Chu L, Siriwardena D, Wormald R, Kotecha A . The quality of optometrists’ referral letters for glaucoma. Ophthal Physiol Opt 2009; 29: 26–31.
Whittaker KW, Ikram K, Anderson DF . Non-communication between ophthalmologists and optometrists. J R Soc Med 1999; 92: 247–248.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lockwood, A., Kirwan, J. & Ashleigh, Z. Optometrists referrals for glaucoma assessment: a prospective survey of clinical data and outcomes. Eye 24, 1515–1519 (2010). https://doi.org/10.1038/eye.2010.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.77
Keywords
This article is cited by
-
Outcomes of newly referred patients with suspected angle closure: do we need to redefine the clinical pathways?
Eye (2024)
-
Positive predictive value of optic disc haemorrhages for open angle glaucoma
Eye (2020)
-
Systematic review of the appropriateness of eye care delivery in eye care practice
BMC Health Services Research (2019)
-
Evaluation of an AI system for the automated detection of glaucoma from stereoscopic optic disc photographs: the European Optic Disc Assessment Study
Eye (2019)
-
Portsmouth visual field database: an audit of glaucoma progression
Eye (2014)