Abstract
Purpose
To assess the distribution of microorganisms isolated from patients with bacterial endophthalmitis and their antimicrobial susceptibility.
Methods
Retrospective analysis of medical and microbiological records of patients with suspected diagnosis of endophthalmitis. The following information was assessed: number of presumed and culture-positive endophthalmitis cases, source of infection, microbiological result (aqueous and/or vitreous culture and Gram staining), microbial characterization and distribution, and antimicrobial susceptibility.
Results
A total of 107 (46%) of 231 patients with bacterial endophthalmitis showed positive results by gram stain or culture. Of these, 97 (42%) patients were positive for culture only. Most of them (62%) were secondary to a surgical procedure (postoperative), 12% were posttraumatic and 26% were secondary to an unknown source or the data were unavailable. A total of 100 microorganisms were isolated (38 aqueous and 67 vitreous samples) from the 97 culture-positive cases (91% were gram-positive and 9% were gram-negative). Coagulase-negative Staphylococcus(CoNS) (48%) were the most frequently isolated, followed by Stretococcus viridans(18%), and Staphylococcus aureus(13%). The antimicrobial susceptibility for CoNS was as follows: amikacin—91.6%, cephalothin—97.9%, ceftriaxone—50%, ciprofloxacin—62.5%, chloramphenicol—91.8%, gatifloxacin—79.5%, gentamicin—72.9%, moxifloxacin—89.5%, ofloxacin—70.8%, oxacillin—58.3%, penicillin—33.3%, tobramycin—85.4%, and vancomycin—100%.
Conclusion
Gram-positive bacteria were the major causes of infectious endophthalmitis in this large series, usually following surgery. CoNS was the most common isolate. Of interest, susceptibility to oxacillin and fourth-generation quinolones was lower than previously published.
Similar content being viewed by others
Introduction
Infectious endophthalmitis following cataract surgery still is a devastating condition, despite major improvements in surgical techniques in the last decades. Most series report on an incidence rate ranging from 0.05 to 0.4% in different studies worldwide.1
Most cases are caused by microorganisms from the conjunctiva and the eyelid. They might be secondary to surgery (postoperative endophthalmitis) or to trauma (posttraumatic endophthalmitis). Other microorganisms reach the eye through hematogenic spread (endogenous endophthalmitis).1, 2, 3
Acute postoperative endophthalmitis is commonly caused by gram-positive bacteria, especially by coagulase-negative Staphylococcus (CoNS), Staphylococcus aureus, and Streptococcus viridans.3, 4, 5 Low virulence microorganisms, such as Propionibacterium acnes, some species of Streptococci, and fungi, are usually causatives of late postoperative endophthalmitis.6 ‘Posttraumatic endophthalmitis’ is caused by the same microorganisms as postoperative cases, as well as other environmental agents.7
Endogenous endophthalmitis accounts for 2–6% of all cases. Previously published causative organisms include Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus agalactiae, Clostridium perfringens, Moraxella spp., Neisseria meningitidis, Escherichia coli, Klebsiella spp., Serratia marcescens, and Candida albicans.3, 8
Its management requires a prompt intervention, such as vitreous tap or vitrectomy followed by intravitreal injection of antibiotics for postoperative and posttraumatic endophthalmitis.9 Endogenous endophthalmitis requires that the main cause be treated, usually meaning systemic therapy with antibiotics in additional to ocular therapy.
Taking this into account, this study aimed at assessing the distribution of microorganisms isolated from patients with bacterial endophthalmitis and their antimicrobial susceptibility from 2006 to 2009 and compare them with the data previously published by our group (2000–2005).3
Patients and methods
This was a retrospective study based on medical records from the Departments of Ophthalmology and Ocular Microbiology Laboratory at the Federal University of São Paulo, Brazil.
Data from all patients with presumed infectious endophthalmitis from 1 January 2006 to 31 October 2009 were analyzed. Presumption of endophthalmitis was based on a well-characterized clinical diagnosis.
The following information was assessed: number of presumed and culture-positive endophthalmitis cases, source of infection (postoperative, posttraumatic, endogenous, and unknown), microbiological result (aqueous and/or vitreous culture and gram staining), microbial characterization and distribution, and antimicrobial susceptibility testing of the positive cases for amikacin, cephalothin, ceftriaxone, ciprofloxacin, chloramphenicol, gatifloxacin, gentamicin, moxifloxacin, ofloxacin, oxacillin, penicillin, tobramycin, and vancomycin.
The patients were submitted either to vitreous/aqueous tap or vitrectomy followed by intravitreal injection of antibiotics. Intraocular specimens were collected and cultured on blood agar, chocolate agar, fastidious anaerobic thioglycolate broth, and Sabouraud agar for aerobic and anaerobic bacteria, and fungi. Gram stain and acid-fast stain tests were performed immediately. A positive culture was defined as either separate colonies of the same organism on two or more separate culture plates or confluent growth at the site of inoculation. Antimicrobial susceptibility testing was performed by the disc diffusion method. Current version of CLSI document M-100, published annually, was used for zone diameter interpretation.
Results
Aqueous and vitreous samples from 231 patients with presumed endophthalmitis of different origins were sent to our laboratory of ophthalmic microbiology throughout the period of this study. A total of 107 (46%) of 231 patients with bacterial endophthalmitis showed positive results by gram stain or culture. Of these, 97 (42%) patients were positive for culture only. Smears were positive for bacteria in 10 culture-negative and in 47 culture-positive cases. Culture was positive in 41 samples obtained from the aqueous humor, 34 from vitreous tap, and 33 from vitrectomy samples. There was overlap among them in 15 cases.
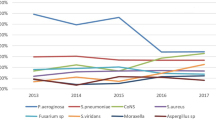
A total of 100 microorganisms were isolated (38 from aqueous and 67 from vitreous samples) from the 97 culture-positive cases (91% were gram positive and 9% were gram negative). Table 1 shows detailed microbial distribution. Coagulase-negative Staphylococcus (CoNS) (48%) were the most frequently isolated, followed by Streptococcus viridans (18%), and Staphylococcus aureus (13%). Three cases were diagnosed with two microorganisms. CoNS was identified in each of them. Contamination from the lid microbiota might have happened.
Most culture positive cases (62%) were secondary to a surgical procedure (postoperative), 12% were posttraumatic and 26% were secondary to an unknown source or the data were unavailable (Table 2). CoNS was the most common microorganism regardless the predisposing factor. Of note, the two cases caused by Bacillus sp. were secondary to trauma.
Antibiotic susceptibility for the five more prevalent groups of microorganisms is disclosed in Table 3. It should be pointed out that 33% of the cases of CoNS resistant to gatifloxacin were sensitive to oxacillin (methicillin-sensitive) and 67% were also resistant to oxacillin (methicillin-resistant). All CoNS moxifloxacin-resistant cases were also methicillin-resistant.
Discussion
To achieve effective prophylaxis and treatment of endophthalmitis, it is important to know the most common etiological agents involved and their response to the major classes of antibiotics routinely used.
The data in this are quite similar to those from our previous report (155 positive samples). From 2000 to 2005, CoNS (42%), Streptococcus viridans (14%) and Staphylococcus aureus (8%) prevailed. Postoperative infection was, as well as in this series, the most prevalent source (61%). Regarding antibiotic susceptibility, CoNS was 83%-sensitive to oxacillin and 100%-sensitive to the fourth-generation quinolones and vancomycin.3
In the present series of 231 infectious endophthalmitis cases, 46.3% were found to have a positive gram-stain or culture result. The remaining cases did not have a conclusive microbiological culture. The low sensitivity of this technique may be because of different factors, such as small amount of available microorganisms or previous use of antibiotics.10 Molecular biology techniques, especially PCR, disclose sensitivities from 90 to 100% in most studies.11, 12
Culture and gram-staining positivity were similarly distributed among aqueous, vitreous tap, and vitrectomy specimens. In all, 15% were simultaneously identified from two different sources (aqueous and vitreous tap or vitrectomy samples). These data were different from our previous study in which vitreous tap specimens made up 51% of all positive cases. As clinical data, such as visual acuity, were not available for this analysis, this difference could simply be explained by a different severity at presentation. Assuming this hypothesis, vitrectomy might have been more used in the present series because of more severe cases and, therefore, disclosed more positive cases than previously.
Gram-positive bacteria were responsible for 91% of culture-positive cases whereas gram negative caused 9% of them. Most published articles show a predominance of gram-positive microorganisms, ranging from 63 to 86%.13, 14, 15 In a previous report from our laboratory (2000–2005), gram-positive bacteria comprised 79% of the culture-proven endophthalmitis isolates.3 In our present and previous analyses, CoNS, Streptococcus viridans, and Staphylococcus aureus were the three most common bacteria in a descending order. This is in agreement with the most common microorganims in the conjunctival flora.16
As expected, most cases were secondary to a surgical procedure (62%) and to trauma (12%). The microorganisms profile in the postoperative and posttraumatic groups is that present in conjunctival flora in both and from the environment in the latter. It should be remarked that Bacillus sp. was only present in the posttraumatic group.
The most relevant information of this study refers to the antimicrobial susceptibility. In our previous report, comprising data from 2000 to 2005, all CoNS were susceptible to both moxifloxacin and gatifloxacin.3 From 2006 to 2009, 79.5 and 89.5% of CoNS were sensitive to gatifloxacin and moxifloxacin, respectively. Other studies in the literature have shown this rate to vary from 65 to 96%.17, 18 Additionally, most fourth-generation quinolone-resistant samples were also found to be methicillin resistant in our study. A recently published article showed that most methicillin-resistant samples from the conjunctiva were also quinolone resistant.19 Betanzos-Cabrera et al have just shown how this resistance mechanism occurs.20 All strains of CoNS resistant to quinolones (gatifloxacin and moxifloxacin) presented mutations at Ser84Phe for the gyrA gene, and Ser80Phe for the parC gene in their series.
As the fourth-generation quinolones are routinely used in the prophylaxis of many surgical procedures, this increasing trend of CoNS resistance is of concern. Besides that, because of their vitreous penetration above MIC, oral moxifloxacin is used in some settings as an additional treatment of endophthalmitis.
The fourth-generation quinolones showed good in vitro results against Staphylococcus aureus, Streptococci, and Pseudomonas. All gram-positive microorganisms were susceptible to vancomycin.
In summary, gram-positive bacteria were the major causes of infectious endophthalmitis in this large series, usually following surgery. CoNS was the most common isolate. Of interest, susceptibility to oxacillin and fourth-generation quinolones was lower than previously published.

References
Taban M, Behrens A, Newcomb RL, Nobe MY, Saedi G, Sweet PM et al. Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol 2005; 123 (5): 613–620.
Callegan MC, Engelbert M, Parke II DW, Jett BD, Gilmore MS . Bacterial endophthalmitis: epidemiology, therapeutics, and bacterium-host interactions. Clin Microbiol Rev 2002; 15 (1): 111–124.
Bispo PJ, Melo GB, d’Azevedo PA, Höfling-Lima AL, Yu MC, Pignatari AC . Culture proven bacterial endophthalmitis: a 6-year review. Arq Bras Oftalmol 2008; 71 (5): 617–622.
Han DP, Wisniewski SR, Wilson LA, Barza M, Vine AK, Doft BH et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol 1996; 122 (1): 1–17. Erratum in: Am J Ophthalmol 1996;122(6):920.
Kresloff MS, Castellarin AA, Zarbin MA . Endophthalmitis. Surv Ophthalmol 1998; 43 (3): 193–224.
Samson CM, Foster CS . Chronic postoperative endophthalmitis. Int Ophthalmol Clin 2000; 40 (1): 57–67.
Reynolds DS, Flynn Jr HW . Endophthalmitis after penetrating ocular trauma. Curr Opin Ophthalmol 1997; 8 (3): 32–38.
Smith SR, Kroll AJ, Lou PL, Ryan EA . Endogenous bacterial and fungal endophthalmitis. Int Ophthalmol Clin 2007; 47 (2): 173–183.
Kim JY, Ali R, Cremers SL, Henderson BA . Perioperative prophylaxis for postcataract extraction endophthalmitis. Int Ophthalmol Clin 2007; 47 (2): 1–14.
Okhravi N, Adamson P, Lightman S . Use of PCR in endophthalmitis. Ocul Immunol Inflamm 2000; 8 (3): 189–200.
Goldschmidt P, Degorge S, Benallaoua D, Basli E, Batellier L, Boutboul S et al. New test for the diagnosis of bacterial endophthalmitis. Br J Ophthalmol 2009; 93 (8): 1089–1095.
Okhravi N, Adamson P, Carroll N, Dunlop A, Matheson MM, Towler HM et al. PCR-based evidence of bacterial involvement in eyes with suspected intraocular infection. Invest Ophthalmol Vis Sci 2000; 41 (11): 3474–3479.
Ng JQ, Morlet N, Pearman JW, Constable IJ, McAllister IL, Kennedy CJ, et al. Team EPSWA. Management and outcomes of postoperative endophthalmitis since the endophthalmitis vitrectomy study: the Endophthalmitis Population Study of Western Australia (EPSWA)'s fifth report. Ophthalmology 2005; 112 (7): 1199–1206.
Benz MS, Scott IU, Flynn Jr HW, Unonius N, Miller D . Endophthalmitis isolates and antibiotic sensitivities: a 6-year review of culture-proven cases. Am J Ophtahlmol 2004; 137 (1): 38–42.
Kunimoto DY, Das T, Sharma S, Jalali S, Majji AB, Gopinathan U et al. Microbiologic spectrum and susceptibility of isolates: part I. Postoperative endophthalmitis. Endophthalmitis Research Group. Am J Ophthalmol 1999; 128 (2): 240–242.
Miño de Kaspar H, Koss MJ, He L, Blumenkranz MS, Ta CN . Antibiotic susceptibility of preoperative normal conjunctival bacteria. Am J Ophthalmol 2005; 139 (4): 730–733.
Miller D, Flynn PM, Scott IU, Alfonso EC, Flynn Jr HW . In vitro fluoroquinolone resistance in staphylococcal endophthalmitis isolates. Arch Ophthalmol 2006; 124 (4): 479–483.
Miller DM, Vedula AS, Flynn Jr HW, Miller D, Scott IU, Smiddy WE et al. Endophthalmitis caused by staphylococcus epidermidis: in vitro antibiotic susceptibilities and clinical outcomes. Ophthalmic Surg Lasers Imaging 2007; 38 (6): 446–451.
Hori Y, Nakazawa T, Maeda N, Sakamoto M, Yokokura S, Kubota A et al. Susceptibility comparisons of normal preoperative conjunctival bacteria to fluoroquinolones. J Cataract Refract Surg 2009; 35 (3): 475–479.
Betanzos-Cabrera G, Juárez-Verdayes MA, González-González G, Cancino-Díaz ME, Cancino-Díaz JC . Gatifloxacin, moxifloxacin, and balofloxacin resistance due to mutations in the gyrA and parC genes of Staphylococcus epidermidis strains isolated from patients with endophthalmitis, corneal ulcers and conjunctivitis. Ophthalmic Res 2009; 42 (1): 43–48.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Melo, G., Bispo, P., Yu, M. et al. Microbial profile and antibiotic susceptibility of culture-positive bacterial endophthalmitis. Eye 25, 382–388 (2011). https://doi.org/10.1038/eye.2010.236
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.236
Keywords
This article is cited by
-
Acute uveitis caused by abnormal glucose and lipid metabolism: a case report
BMC Ophthalmology (2023)
-
Diagnostic performance of blood culture bottles for vitreous culture compared to conventional microbiological cultures in patients with suspected endophthalmitis
European Journal of Clinical Microbiology & Infectious Diseases (2018)
-
Comparison of methods for identifying causative bacterial microorganisms in presumed acute endophthalmitis: conventional culture, blood culture, and PCR
BMC Infectious Diseases (2017)
-
Clinical outcomes and antibiotic susceptibilities of Staphylococcus aureus endophthalmitis
Graefe's Archive for Clinical and Experimental Ophthalmology (2017)