Abstract
Purpose
To analyse the long-term visual acuity (VA) and intraocular pressure (IOP) outcomes in phacomorphic glaucoma.
Patients and methods
A retrospective analysis of 100 consecutive, acute phacomorphic glaucoma cases from January 2000 to April 2009 was conducted at The Caritas Medical Centre in Hong Kong. All cases underwent cataract extraction after IOP control with medication and/or laser.
Results
During a 3.1±2.6-year follow-up, the mean visual improvement was 1.1±0.9 LogMAR units with improvements in 81.7% of cases. A shorter duration from symptoms to cataract extraction resulted in greater visual improvement (r2=0.1, P=0.001). In all, 80.5% of the cases had IOP⩽21 mm Hg without any glaucoma treatment; 19.5% required 1.6±0.7 glaucoma eye drops; and 3.7% required additional laser iridotomy or trabeculectomy for IOP control at 1.8±2.3 years. The vertical cup–disc ratio (VCDR) of the index eye was 0.6±0.3. Gonioscopy revealed an averaged Shaffer grading of 3.0±1.0 and 99±90 degrees of peripheral anterior synechiae (PAS). The Humphrey automated perimetry mean deviation was 5.2±2.7 and the pattern standard deviation was −15.9±10.
Conclusion
Over 80% of phacomorphic patients had long-term visual improvements and normalization of IOP after cataract extraction. A shorter attack seemed to offer better VA. Post-operatively, most have open angles with some degree of PAS formation, and glaucomatous optic neuropathy is evident from enlarged VCDRs and visual field defects. At least 2 years of follow-up is useful to detect a 20% glaucoma progression possibly requiring additional glaucoma treatments.
Similar content being viewed by others
Introduction
Phacomorphic glaucoma is an important disease entity in developing Asian countries, especially in India, with reported incidences of 3.91% of all cataract extractions.1 Phacomorphic glaucoma is often associated with a population of lower social economical class with inadequate access to medical care.1 It is caused by a mature and swollen cataract compressing on and compromising the normal aqueous drainage pathways resulting in a secondary angle closure.2 The resulting prolonged elevated intraocular pressure (IOP) in turn leads to irreversible optic nerve damage and visual impairment.3, 4, 5 The definitive treatment is cataract extraction after initial control of intraocular pressure with medical or laser therapy (laser iridoplasty, LI and or laser iridotomy, ALPI) to prevent the risks of operating on an eye with corneal oedema and high IOP.
There is limited information in literature on the long-term clinical outcomes of phacomorphic glaucoma patients. The purpose of this study was to investigate the long-term visual acuity (VA) and intraocular pressure control post cataract extraction in phacomorphic glaucoma. The main outcome measures were pre- and post-operative VA, pre- and post-operative IOP, and time from symptoms to cataract extraction. Secondary outcome measures were post-operative gonioscopic findings, number of glaucoma eye drops/interventions required, vertical cup–disc ratio (VCDR), and pattern standard deviation (PSD), and mean deviation (MD) on the Humphrey automated perimetry.
Materials and methods
A retrospective review of medical records with the diagnosis of phacomorphic glaucoma was conducted from January 2000 to April 2009. All patients attended a single centre, The Caritas Medical Centre, Hong Kong Special Administrative Region, The People's Republic of China. The centre offers ophthalmic service for a population of 1.8 million (26% of the total Hong Kong population).6 The study received ethics approval from the institutional review board of the Hospital Authority of Hong Kong and followed the principles in the Declaration of Helsinki. Consent was obtained before laser therapy and cataract extraction.
Phacomorphic glaucoma was diagnosed based on the following: an IOP⩾21 mm Hg2 in the presence of an intumescent (swollen and white) cataract together with signs of phacomorphic glaucoma including a shallow central anterior chamber from slit-lamp examination, corneal oedema, mid-dilated pupil, and conjunctival injection. A gonioscopic examination was not required for the diagnosis as it was often not feasible in the presence of corneal oedema from the acute IOP elevation. Symptoms, although documented, were not required for the diagnosis, as a number of phacomorphic patients had dementia and the volunteering of symptoms was not always possible. Cases were excluded if there was any documented suspicion of acute primary angle closure from the medical records.
A total of 100 consecutive cases (100 eyes) of phacomorphic glaucoma were identified during the specified 9-year period. All cases presented with acute signs or symptoms. Twenty of these cases were on the waiting list for elective cataract extraction, 80 were new cases to our centre. For the first part of the study, all 100 cases were used for the descriptive statistics describing the presenting age, presenting IOP, and sex predominance, in order to provide a more accurate representation of the demographics of phacomorphic glaucoma over a 9-year period.
The second part of the study looked at the clinical outcomes post cataract extraction, including best correct visual acuity (BCVA), IOP control, gonioscopy, VCDR, and visual field. For the second part of the study that required a degree of patient cooperation, 18 cases with dementia were excluded due to the inability to assess pre- or post-operative VA.
All the 100 cases of phacomorphic glaucoma were managed uniformly. Cases were initially treated with systemic acetazolamide, if there were no systemic contraindications, together with topical steroids and combinations of glaucoma eye drops including timolol 0.5%, brimonidine, or carbonic anhydrase inhibitors. Pilocarpine was not part of the routine treatment protocol for phacomorphic glaucoma at our centre as contractions of the ciliary muscle caused by pilocarpine result in axial lens thickening, which theoretically aggravates the pupillary block.
Nineteen patients were found to have concomitantly received laser treatments (11 argon laser peripheral iridoplasty, ALPI; 7 laser iridotomy, LI; and 1 combined ALPI plus LI) before cataract extraction. The decision for laser therapy was primarily surgeon dependent.
When the IOP and inflammatory status of the involved eye settled, all patients underwent a one-stage cataract extraction under regional or general anaesthesia (4 phacoemulsifications and 96 extracapsular extractions, ECCEs). In 10 cases, an intraocular lens was not inserted due to an absence of light perception on presentation. Eighty-eight (88%) of the cataract extractions were performed by residents and 12% by associate consultants or consultants. There was only 1 case with intraoperative complication, vitreous loss from loosened zonules requiring anterior vitrectomy. The case was an ECCE performed by a resident surgeon.
The patients were followed up post-operatively on day 1, 1 week, 1 month, 3 months, and then based on individual clinical requirements. Post-operative steroid and glaucoma drops were tailed off between 1 to 3 months post-operatively and glaucoma treatments were re-implemented if the IOP was ⩾21 mm Hg on two or more follow-up readings.
Definitions and statistics
All visual acuity measurements were measured by the Snellen chart and converted to Logarithm of Minimal Angle of Resolution (LogMAR) units for statistical analysis, and the following LogMAR denotations were used for non-numeric visual acuities: finger count (FC)=1.7 LogMAR, hand movement (HM)=2.0 LogMAR, light perception (LP)=2.3 LogMAR, and no light perception (NLP)=3.0 LogMAR.
Differences between pre- and post-operative VA were calculated for each individual by subtracting the post-operative BCVA on the last follow-up from the VA at presentation (both in LogMAR units). Intraocular pressures were measured by Goldmann applanation tonometry.
All analyses were performed using statistical software (GraphPadPrism for Windows, ver. 5.0; GraphPad Software, Inc., La Jolla, CA, USA). Continuous data were presented as mean±standard deviation (s.d.). Statistical analysis with linear regression, Mann–Whitney U test, and Spearman's correlation coefficient were appropriate. Statistical significance was defined as P<0.05 for all tests.
All visual field assessments were done using the Humphrey Field Analyzer (Carl Zeiss Ophthalmic Systems, Inc., Dublin, CA, USA) using Swedish Interactive Threshold Algorithm Fast (SITA Fast), 24-2 strategy. SITA Fast was selected rather than the Full Threshold strategy to shorten the test time to facilitate more focus and cooperation from the elderly phacomorphic patients.
Results
Part 1
For the 100 cases of phacomorphic glaucoma, the presenting age was 73.8±10.6 years (range, 40–104 years). All patients were ethnic Chinese with a male to female ratio of 1 : 1.5. The presenting IOP was 49.4±11.7 mm Hg (range, 24–74 mm Hg). Twenty-six cases presented with more than one symptom. The summary of symptoms is shown in Table 1.
Part 2
For the 82 cases of phacomorphic glaucoma that were included in the second part of the study, the presenting VA was 2.2±0.3 LogMAR (range, 1.17–3 LogMAR; Snellen range, 4/60 to NLP; Snellen mode, LP). The median time from symptom onset to cataract extraction was 9 days.
The mean follow-up time was 3.1±2.6 years (range, 1 month to 9 years). Eight out of one hundred cases had a follow-up less than 6 months and then defaulted follow-up; the rest had follow-ups of least 6 months. The best-corrected visual acuity (BCVA) measured at 1.7 years±1.7 years post cataract extraction was 1.1±0.9 LogMAR. The mean VA improvement was 1.1±0.9 LogMAR units post cataract extraction. There was no correlation between the VA improvement and the time interval of when VA was measured post-operatively (P=0.1, linear regression). Sixty-seven out of eighty-two (81.7%) of the cases had improved visual acuity post-operatively.
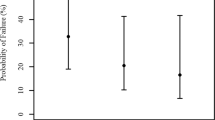
A linear regression analysis showed with statistical significance that a shorter duration of time from symptoms to cataract extraction resulted in greater visual improvement (r2=0.1, P=0.001). But a linear regression analysis of the presenting IOP and VA improvement did not show any statistical significance (P=0.5). There was no relationship between earlier cataract extraction and post-operative IOP control (P=0.2, linear regression) or angle status (P=0.3, Spearman's correlation coefficient). A lower IOP on presentation did not result in a prompter cataract extraction time (P=0.7, linear regression).
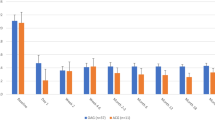
When looking at the mean IOP control at 1 week, 1 month, 3 months, 6 months, 1 year, 3 years, and 5 years post cataract extraction, a minimum of 86.7% of all phacomorphic patients who attended follow-up had IOP⩽21 mm Hg during the various follow-up intervals. The breakdown is shown in Table 2.
Of all phacomorphic cases, 80.5% (66/82) had IOP ⩽21 mm Hg without any additional glaucoma treatment during the mean follow-up of 3.1±2.6 years. Of the 19.5% that required additional glaucoma medication, the mean number of glaucoma eye drops required was 1.6±0.7. Three cases (3.7%) required additional glaucoma interventions for IOP control (1 LI and 2 trabeculectomies). The mean time for IOP spikes during follow-up prompting for further glaucoma intervention was 1.8±2.3 years (range, 1 week to 7 years).
The mean VCDR of the phacomorphic eye recorded at a mean of 3.1±2.6 years post-operatively was 0.6±0.3, which was statistically larger compared with VCDR (0.4±0.1) of the contralateral uninvolved eye (P=0.03).
The gonioscopic findings recorded at a mean of 3.1±2.6 years post-operatively revealed 99±90 degrees of PAS and the averaged gonioscopic grading of the four quadrants using the Shaffer gonioscopic grading system was 3.0±1.0. There was no significant correlation between the degrees of PAS to the following variables: the time from onset of symptoms to cataract extraction (P=0.9); presenting IOP (P=0.4); or post-operative IOP (P=0.3) (correlations using Spearman's correlation coefficient).
The Humphrey automated perimetry MD was 5.2±2.7 and the PSD was −15.9±10. There was no correlation between the time from symptoms to cataract extraction to the MD or PSD (P=0.9 and 0.6, respectively, Spearman's correlation coefficient).
Discussion
Although phacomorphic glaucoma is most common in developing Asian countries, it is, interestingly, not an uncommon disease in the developed metropolis of Hong Kong despite there being a relatively accessible and affordable, government-subsidized, healthcare system. Phacomorphic glaucoma combines two of the most common causes of visual impairment in the elderly7 and the reversibility of this acute condition makes it a worthwhile topic of study.
Our study subjects represent an aged population with multiple medical co-morbidities including hypertension, diabetes, chronic obstructive airway disease, ischaemic heart, congestive heart failure, and dementia, which partly explains the delays in seeking medical attention for their mature cataracts and the delays in presentation when phacomorphic glaucoma does occur.
To the best of our knowledge, this is the first case series documenting the long-term (>2 year mean) visual acuity and intraocular pressure control outcomes of phacomorphic glaucoma patients.
In phacomorphic glaucoma, the intumescent cataract narrows the iridoconeal angle either via a pupillary block or via the forward displacement of the lens–iris diaphragm. Although acute primary angle closure may present with similar symptoms and signs, based on the presence of a mature and swollen cataract, we felt that the major angle-closing factor in this series was due to the lens and cases were excluded if there was any doubt. Hence, cataract extraction is the only definitive treatment and the timing of cataract extraction is important. Although the healthy eye is believed to be able to withstand raised IOP for a reasonable period of time,8 prolonged increase in IOP causes irreversible damage to the optic nerve, impairing vision. We have demonstrated in this study that it is not the level of presenting IOP that directly correlates with the degree of visual loss (P=0.5), but rather the duration of this prolonged elevated pressure that determines the degree of visual loss (P=0.001) likely through irreversible ischaemic optic nerve damage and axonal flow disruption similar to primary acute angle closure.
Those with a lower presenting IOP and theoretically less corneal oedema or ‘less severe phacomorphic glaucoma’ did not have prompter cataract extraction compared with those with higher IOP (P=0.7). Other confounding factors affecting the timing of operation, including patient's medical fitness for operation, operating theatre availability, and the autonomy of patients and their family in deciding for surgery, were also important determinants in the timing of cataract extractions.
In our series, 81.7% of the phacomorphic glaucoma cases had VA improvement post cataract extraction and the mean VA improvement measured at 1.7±1.7 years was 1.1±0.9 LogMAR units from the presenting VA. For IOP control, 80.5% of cases had IOP ⩽21 mm Hg without any additional glaucoma treatment during the mean follow-up of 3.1±2.6 years. In the majority of the cases, cataract extraction alone was sufficient to lower the IOP to ⩽21 mm Hg as the primary pathology is in the mechanical anterior displacement of the intumescent cataract rather than in the trabecular meshwork. Only three cases required additional glaucoma intervention, two trabeculectomies, and one laser iridotomy for IOP control post cataract extraction.
Extracapsular cataract extraction was the predominant method of cataract extraction. Although phacoemulsification theoretically offers a smaller wound and lesser risk of expulsive hemorrhage, the intumescent cataract and the liquefied lens contents would make the continuous curvilinear capsulorhexis technically challenging and the presence of any residual corneal oedema and zonule loosening in the setting of a previous IOP elevation would make phacoemulsification less safe compared with ECCE and impose a greater risk of further endothelial damage by ultrasound energy. In addition, the phacoemulsification technology 9 years ago was not as advanced as it is today. There was only one case with intra-operative complication in our series, an ECCE with vitreous loss from loosened zonules requiring anterior vitrectomy.
We postulated that a higher IOP at presentation and longer duration of phacomorphic attack would lead to more PAS formation and subsequently poorer postoperative IOP control due to more angle closure. However, from the results of this study, there was no statistically significant correlation between the degrees of PAS formation and the above variables (all P values ⩾0.3). It is perhaps the degree of anterior displacement of the intumescent cataract and extent of iridocorneal contact at the angles that determine the degree of PAS formation, while IOP level is merely a reflection of the degree level of aqueous blockage. Thus, anterior chamber depth during the acute attack may be a more useful predictor of PAS formation. In addition, gonioscopic examination is subjective and variable between observers, the use of more objective assessments of angle status with ultrasound biomicroscopy (UBM) or anterior segment optical coherence tomography (OCT) would be more ideal in future prospective studies.
Various literatures have established ALPI as an effective and safe primary treatment for phacomorphic glaucoma before cataract extraction.9, 10 Laser therapy is replacing the conventional trend of medical therapy alone in the initial management of phacomorphic glaucoma as the success of IOP control in medical therapy is only about 63.5%.9 This trend was also noted at our centre, as those receiving laser therapy mainly presented after 2004, which was in and around the time of publications supporting the use of laser. However, in our series, laser therapy was only used as a concomitant therapy in addition to medical therapy and the decision for and the type of laser therapy received was not randomized; it was primarily surgeon dependent, based on the degree of corneal clarity and patient cooperation on presentation. As both ALPI and LI have been established as effective initial measures for IOP reduction in acute primary angle closure,11, 12, 13, 14 both techniques were justified in their use in phacomorphic glaucoma, which carries a secondary angle closure component. Comparisons between the clinical outcomes of medical vs medical plus laser therapy groups were beyond the scope of this retrospective study.
Although a shorter attack seems to offer better visual improvement, the correlation between attack duration and Humphrey perimetry defects was not significant. This is accounted for by the variability of Humphrey perimetry, which varies depending on the eye–hand coordination, intelligence, and education level of patients. Newer technologies that are now available, such as retinal nerve fibre layer analysis, would be a more objective assessment of glaucomatous optic neuropathy.
Conclusion
Cataract extraction is an effective definitive treatment for phacomorphic glaucoma with more than 80% of patients having visual improvements and IOP normalization without additional glaucoma intervention during a 3-year follow-up period. A shorter time interval from symptoms to cataract extraction seemed to offer better VA improvements. Post-operatively, the majority have open angles with a degree of PAS formation. The resultant glaucomatous optic neuropathy is evident from the increased VCDRs and defects on the Humphrey automated perimetry. Patients should be followed up for at least 2 years post-operatively to monitor for the 20% of cases that may require further glaucoma intervention for IOP control.

References
Angra SK, Pradhan R, Gary SP . Cataract induced glaucoma—an insight into management. Indian J Ophthalmology 1991; 39: 97–101.
Leibmann JM, Ritch R . Glaucoma associated with lens intumescence and dislocation. In: Ritch R, Shields MB, Krupin T (eds). The Glaucomas, Vol 2, 2nd ed. St Louis: Mosby, 1996; 1033.
David R, Tessler Z, Yassur Y . Long term outcome of primary acute angle closure glaucoma. Br J Ophthalmol 1993; 17: 33–36.
Kanellopoulos AJ, Perry HD, Donnenfeld ED . Comparison of topical timolol gel to oral acetazolamide in the prophylaxis of viscoelastic-induced ocular hypertension after penetrating keratoplasty. Cornea 1997; 16 (1): 12–15.
Hart WM, Becker B . The onset and evolution of glaucomatous visual field defect. Ophthalmology 1982; 89: 991–998.
Hong Kong Monthly Digest of Statistics. 2009, p. FC4.
Tham CC, Lai JS, Poon AS, Chan JC, Lam SW, Chua JK et al. Immediate argon laser peripheral iridoplasty (ALPI) as initial treatment for phacomorphic angle-closure (phacomorphic glaucoma) before cataract extraction: a preliminary study. Eye 2005; 19: 778–783.
Prajna NV, Ramakrishnan R, Krishnadas R, Manoharan N . Lens induced glaucomas—visual results and risk factors for final visual acuity. Indian J Ophthalmol 1996; 44: 149–155.
Yip PP, Leung WY, Hon CY, Ho CK . Argon laser peripheral iridoplasty in the management of phacomorphic glaucoma. Ophthalm Surg Laser Imaging 2005; 36 (4): 286–291.
Jain IS, Gupta A, Dogra MR, Gangwar DN, Dhir SP . Phacomorphic glaucoma-management and visual prognosis. Indian J Ophthalmol 1983; 31: 648–653.
Lai JS, Tham CC, Lam DS . Limited argon laser peripheral iridoplasty as immediate treatment for an acute attack of primary angle closure glaucoma; a preliminary study. Eye 1999; 13 (Part 1): 26–30.
Lam DS, Lai JS, Tham CC . Immediate argon laser peripheral iridoplasty as treatment for acute attack of primary angle-closure glaucoma: a preliminary study. Ophthalmology 1998; 105: 2231–2236.
Lam DS, Lai JS, Tham CC, Chua JK, Poon AS . Argon laser peripheral iridoplasty versus conventional systemic medical therapy in treatment of acute primary angle-closure glaucoma: a prospective, randomized, controlled trial. Ophthalmology 2002; 109: 1591–1596.
Tham CC, Lai JS, Lam DS . Immediate argon laser peripheral iridoplasty for acute attack of PACG (addendum to previous report). Ophthalmology 1999; 106: 1042–1043.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented in part as an oral presentation at the Annual Scientific Meeting Hong Kong Ophthalmology Symposium 2009 in Hong Kong SAR, December 5, 2009.
Rights and permissions
About this article
Cite this article
Lee, J., Lai, J., Yick, D. et al. Retrospective case series on the long-term visual and intraocular pressure outcomes of phacomorphic glaucoma. Eye 24, 1675–1680 (2010). https://doi.org/10.1038/eye.2010.108
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.108
Keywords
This article is cited by
-
Risk of central nervous system demyelinating attack or optic neuritis recurrence after pediatric optic neuritis in Korea
Neurological Sciences (2024)
-
Short-term outcomes of Mitomycin-C augmented phaco-trabeculectomy using subconjunctival injections versus soaked sponges: a randomized controlled trial
Eye (2023)
-
Predisposing factors, microbiological features and outcomes of patients with clinical presumed concomitant microbial and herpes simplex keratitis
Eye (2022)
-
Outcomes of suprachoroidal haemorrhage drainage with and without vitrectomy: a 10-year study
Eye (2021)
-
Utility of wound cultures in the management of open globe injuries: a 5-year retrospective review
Journal of Ophthalmic Inflammation and Infection (2020)