Abstract
Purpose
To assess the clinical outcomes and patient satisfaction after simultaneous Implantable Collamer Lens (ICL) removal and phacoemulsification with intraocular lens (IOL) implantation in ICL-implanted eyes with developing cataracts.
Methods
We retrospectively reviewed the clinical charts of 10 eyes of eight patients who developed significant cataract after ICL implantation. Patient age was 47.2±5.9 (mean±SD) years (range, 37–57 years). We determined visual acuity (log MAR), manifest refraction, endothelial cell density, and subjective satisfaction with visual outcomes measured using a visual analogue scale, that ranged from 0 (very dissatisfied) to 10 (very satisfied), before and 3 months after cataract surgery.
Results
Log MAR best spectacle-corrected visual acuity was significantly improved from 0.19±0.30 preoperatively to −0.06±0.07 postoperatively (P=0.007, Wilcoxon signed-rank test). Eight (80%) and nine (90%) of the 10 eyes were within 0.5 D (diopter) and 1.0 D of the targeted correction, respectively. The endothelial cell density was 2584.9±266.2 cells/mm2 preoperatively, and 2340.1±269.7 cells/mm2 postoperatively. The overall satisfaction with visual outcomes was scored 1.8±1.1 (range: 0–3) preoperatively, and 7.9±1.4 (range: 6–10) postoperatively. No vision-threatening complications were seen throughout the follow-up period.
Conclusions
Simultaneous ICL removal and phacoemulsification with IOL implantation was safe and effective with predictable refractive results, and thus yielded a high level of patient satisfaction with ICL-induced cataract treatment.
Similar content being viewed by others
Introduction
Visian Implantable Collamer Lens (ICL, STAAR Surgical, Nidau, Switzerland), a posterior chamber phakic intraocular lens (IOL), has become widely accepted in the recent years as an effective method for the correction of moderate to high ametropia.1, 2, 3, 4, 5, 6, 7, 8, 9 This surgical procedure may have advantages over laser in situ keratomileusis (LASIK) because it is not only highly predictable but also reversible. It may also have advantages over refractive lens exchange because the crystalline lens, which plays a major role in accommodative function, especially in younger patients, remains untouched. On the other hand, there are ongoing concerns about one postoperative complication: the development of lens opacity after ICL implantation because of the close proximity of the ICL to the crystalline lens. In light of the prevalence of this surgical procedure, it is clinically important to assess the prognosis of patients with developing cataract after ICL implantation. However, there have been only a few studies on the prognosis of patients with developing cataract after ICL implantation.10, 11 Moreover, patient subjective satisfaction and endothelial cell loss after these procedures, both of which are major concerns in the prognosis of such patients, still remain unclear. The aim of this study is retrospectively to assess the clinical outcomes, including endothelial cell density and patient satisfaction after ICL removal and phacoemulsification with IOL implantation in eyes with ICL-induced cataract.
Materials and methods
We retrospectively reviewed the clinical charts of 37 eyes of 22 patients who had undergone ICL implantation at Musashino Red Cross Hospital (Tokyo, Japan) from 1997 to 1998 with a minimal follow-up for 6 months after surgery. ICL models V2, V3, and V4 were implanted in 24 (65%), four (11%), and nine (24%) eyes of these patients, respectively. Sixteen eyes (43%) of 12 patients developed anterior subcapsular cataract, and of them, 10 eyes (six of men and four of women) of the eight patients who developed cataract with a significant loss of two or more lines of best spectacle-corrected visual acuity (BSCVA), after ICL implantation for the correction of myopia, were included in this study. The remaining six of the 16 eyes did not require cataract surgery because cataract formation was asymptomatic and they were not included in this study. Informed consent was obtained from all patients. The study adhered to the tenets of the Declaration of Helsinki. Institutional Review Board approval was not required for this retrospective study.
Implantable collamer lens power calculations were performed by the manufacturer (STAAR Surgical) using a modified vertex formula. The size of the ICL was also chosen by the manufacturer on the basis of the horizontal corneal diameter and anterior chamber depth with scanning-slit topography (Orbscan IIz, Bausch & Lomb, Rochester, NY, USA). IOL power calculations were performed by the SRK-T formula using the axial length measured by A-scan ultrasonography (US-800, Nidek, Aichi, Japan) without any correction for the ICL in situ, and keratometric readings measured with an autorefractometer (RK-5, Canon, Tokyo, Japan).
Before ICL implantation, the patients underwent two peripheral iridectomies with a neodymium-YAG laser. On the day of surgery, the patients were administered dilating and cycloplegic agents. After topical anaesthesia, a model V2, V3, or V4 ICL was inserted through a 3-mm corneal incision with the use of an injector cartridge (STAAR Surgical) after the introduction of viscoelastic material (Opegan Santen, Osaka, Japan) into the anterior chamber. The ICL was placed in the posterior chamber, the remaining viscoelastic was completely washed out of the anterior chamber with balanced salt solution, and a miotic agent (acetylcholine chloride, Ovisort Daiichi-Sankyo, Tokyo, Japan) was instilled. After surgery, steroidal (0.1% betamethasone, Rinderon Shionogi, Osaka, Japan) and antibiotic (levofloxacin, Cravit Santen, Osaka, Japan) medications were topically administered four times daily for 2 weeks, with the dose being steadily reduced thereafter.
For ICL removal and phacoemulsification with monofocal IOL implantation, a 3.0-mm clear corneal incision at a site identical to the original incision, was created after topical anaesthesia. After the introduction of viscoelastic material (Opegan) into the anterior chamber, the proximal haptics of the ICL were dislocated, grasped with forceps, and extracted from the anterior chamber through the incision. Then, standard phacoemulsification was performed by capsulorrhexis, nuclear and cortex extraction, and IOL implantation (KS-3Ai, STAAR Surgical) using the same 3.0-mm incision. All surgeries were uneventfully performed by the same surgeon (KS) and no intraoperative complication was observed. After surgery, steroidal (0.1% betamethasone, Rinderon), antibiotic (levofloxacin, Cravit), diclofenac sodium (0.1% Diclod Wakamoto, Tokyo, Japan) medications were topically administered four times daily for 1 month, and then the dose was steadily reduced.
Before and 3 months after these combined surgeries, we performed the following examinations: uncorrected visual acuity (UCVA), BSCVA, manifest refraction, endothelial cell density measured with a non-contact specular microscope (SP-8800, Konan, Nishinomiya, Japan), and patient subjective satisfaction. The patient satisfaction was assessed according to the visual analog scale in a range from 0 (very dissatisfied) to 10 (very satisfied) by one of the authors who did not participate in the overall treatment or follow-up of the patients in the study.
All statistical analyses were performed using SPSS (SPSS Inc., Chicago, IL, USA). The results are expressed as mean±standard deviation (SD), and a value of P<0.05 was considered statistically significant.
Results
Patient demographics
Preoperative and postoperative patient demographics are listed in Table 1. The patient age at the time of cataract surgery was 47.2±5.9 years (range: from 37 to 57 years old). In six (60%) and four (40%) of the 10 eyes, the patients were men and women, respectively. The preoperative manifest refraction (spherical equivalent) before ICL implantation was −15.0±4.2 diopters (D) (range: from −10.4 to −24.0 D). The preoperative astigmatism was 1.1±1.2 D (range: from 0.0 to 3.5 D). The preoperative endothelial cell density was 2603.9±213.4 cells/mm2 (range: from 2239 to 2859 cells/mm2). The anterior chamber depth was 2.99±0.23 mm (range: from 2.76 to 3.35 mm). In nine (90%) and one (10%) of the 10 eyes, we implanted a model V2 and a V4 ICL, respectively. Intervals from ICL implantation to cataract surgery were 3.6±1.9 years (range: from 1.6 to 7.4 years). The follow-up duration was 7.8±2.9 years (range: from 2.5 to 10.0 years). There were no concomitant eye diseases, except for lattice dystrophy in two eyes (in case 2 and case 9) and for one eye with macular atrophy (in case 10).
Safety outcomes
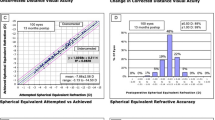
Log MAR BSCVA was significantly improved from 0.19±0.30 preoperatively to −0.06±0.07 postoperatively (P=0.008, Wilcoxon signed-rank test). The safety index (mean postoperative BSCVA/mean preoperative BSCVA) was 2.51±3.35, 3 months postoperatively. One eye (10%) showed no change in BSCVA, two eyes (20%) gained one line, seven eyes (70%) gained two or more lines, and no eyes lost any lines (Figure 1).
Effectiveness outcomes
Log MAR UCVA was changed from 0.56±0.28 preoperatively to 0.26±0.30 postoperatively (P=0.09, Wilcoxon signed-rank test). The targeted manifest refraction (spherical equivalent) was −2.34±1.22 D (range: from −0.74 to −4.27 D) depending on the refraction of the fellow eye and the patient's wish for near or far vision. Manifest refraction was −2.87±2.06 D preoperatively, and −2.07±1.56 D postoperatively. The efficacy index (mean postoperative UCVA/mean preoperative BSCVA) was 1.13±1.05, 3 months postoperatively. Seven (70%) of 10 eyes had UCVA of 0.5 or better 3 months after surgery.
Predictability
A scatter plot of the attempted versus the achieved refraction (manifest spherical equivalent) 3 months after surgery is shown in Figure 2. Eight (80%) and nine (90%) of the 10 eyes were within±0.5 D and 1.0 D, respectively, of the targeted correction.
Scatter plot of attempted vs achieved refraction (manifest spherical equivalent) in Implantable Collamer Lens (ICL) removal and intraocular lens (IOL) implantation. Eight (80%) and nine (90%) of the 10 eyes were within ±0.5 D and 1.0 D, respectively, of the targeted refraction 3 months after surgery.
Patient satisfaction
The overall satisfaction score with visual outcomes using the visual analogue score was significantly improved from 1.8±1.1 (range: 0–3) preoperatively to 7.9±1.4 (range: 6–10) 3 months postoperatively (P<0.001, Wilcoxon signed-rank test).
Adverse events
The endothelial cell density fell from 2584.9±266.2 cells/mm2 preoperatively to 2340.1±269.7 cells/mm2, 3 months postoperatively. The percentage of endothelial cell loss was 8.9±11.0%. No vision-threatening complications including intraocular pressure rise, posterior capsular opacity, cystoids macular oedema, and retinal detachment were seen at any time during the follow-up period.
Discussion
In this study, we have shown that simultaneous ICL extraction and phacoemulsification with a monofocal IOL were safe, effective, and predictable surgical methods in eyes with developing ICL-induced cataract. Bleckmann et al10 first reported that the BSCVA after ICL removal and cataract extraction with monofocal IOL implantation improved 1.44±1.33 lines more than that before ICL implantation. Morales et al11 also reported that the mean BSCVA before ICL implantation, after ICL implantation, and after cataract surgery were 0.31±0.32, 0.28±0.19, and 0.27±0.21, respectively. However, the endothelial cell loss after these surgical procedures, which is one of major concerns in the prognosis of these patients, was not investigated in these earlier articles. In this study, we observed a mean endothelial cell loss of 8.9±11.0%, which was considered to be clinically acceptable in such cases complicated by a developing significant ICL-induced cataract.
Concerns about the backgrounds of patients with developing ICL-induced cataract also exist. With regard to patient age, Gonvers et al12 reported that ICL-induced cataracts develop more frequently in older patients than in younger patients; the incidences in those of 40 years of age or less and of 41 or over were 14 and 37%, respectively. Lackner et al13 and Sarikkola et al14 proposed ages of 50 years or older and 45 years or older, respectively, as risk factors for cataract development after ICL implantation. Fujisawa et al15 stated that a decrease in accommodation with ageing may affect the continuous flow of the aqueous humour, resulting in a higher incidence of cataract development after ICL implantation. With regard to the ICL configuration, Sanders et al16 reported that the incidence of anterior subcapsular cataract with ICL V3 and V4 was 12.6 and 2.9%, respectively, probably because ICL V4 is designed to have a vaulting 0.13–0.21 mm higher than ICL V3, depending on dioptric power. Gonvers et al17 also stated that the central vaulting of ICL V3 was slightly less than that of ICL V4. Sarikkola et al14 reported the incidence of anterior subcapsular cataracts with ICL V4 in younger patients was 7.7%, whereas that with ICL V2, V3, or V4 in older patients was 47.7%. The US FDA trial showed that the incidence of anterior subcapsular cataract with ICL V4 was 2.7%.8 In this study, the patient age at the time of surgery was 47.2±5.9 years (mean±SD), and model ICL V2, V3, and V4 were implanted through nine (38%) of 24 eyes, none (0%) of four eyes, and one (12%) of nine eyes in the cases complicated by cataract. Although we cannot refute the possibility that the early clinical results are influenced by the surgeon's learning curve, only two eyes (20%) developed cataract immediately after surgery, suggesting that the learning curve alone may not contribute to the higher rate of ICL V2-induced cataract. We assume that the higher rate of ICL V2-induced cataract was attributable to the higher patient age, as well as to the learning curve. In another study, we also compared the patient backgrounds of the group in which cataracts developed with those of the group in which they did not. The eyes with cataract were found in patients of significantly higher age (49.5±6.0 years) than those without (42.2±9.1 years), but the amounts of myopia did not differ significantly between the eyes with cataract (−14.3±3.6 D) and those without (−13.9±2.7 D). The eyes with cataract (V2 69%, V3 13%, and V4 19%) were found to have ICLs with versions that were earlier than those in eyes without (V2 62%, V3 10%, and V4 29%). ICL V2 and V3 have now been withdrawn from the market, but our present findings are in good accordance with the earlier findings indicating that higher patient age and earlier versions of the ICL were risk factors for cataract development in ICL-implanted eyes. We assume that the rate of developing cataract with ICL V3 was higher than that with ICL V4 possibly because of a small sample size. The characteristics may also account for the higher incidence (43%) of developing cataracts in the overall population undergoing ICL implantation at that time than those in recent years.
With regard to the predictability of these combined procedures in eyes with ICL-induced cataract, Bleckmann et al10 stated that refractive error in no eyes ever exceeded the value of 1 D independent of the initial refraction or degree of hyperopia or myopia. Morales et al11 reported that the percentage of eyes within±1.0 D of the targeted correction was 71.4%. In this study, we have shown that the percentage of eyes within±0.5, and ±1.0 D of the targeted correction after 3 months after surgery were 80, and 90%, respectively, which is in accordance with their earlier findings that the combined procedures offer high predictability of the intended correction. Hoffer et al18 reported that the greatest difference in A-scan axial length measurements will occur with a silicone IOL in an eye with very high hyperopia, and that the least difference will occur with a ICL in an eye with very high myopia. Morales et al11 also stated that the difference between the axial length measurements before ICL implantation and those after was small. These findings may partly account for the higher predictability of these combined procedures.
Gimbel et al19 expressed the view that subjective patient information was as important as visual and refractive data because patient satisfaction would ultimately affect the future popularity of refractive surgery. Although patient satisfaction is known to be influenced by the status of the fellow eye, the UCVA of the fellow eye was excellent in six of these eight patients, because they had undergone bilateral ICL implantation. In this study, postoperative patient satisfaction, which was highly important for the future propagation of ICL implantation, was comparatively high, and no significant complications occurred during the observation period, supporting our view that these procedures are safe and effective for the treatment of ICL-induced cataract.
Nevertheless, the loss of accommodation in pseudophakic eyes was not negligible, especially for younger patients. It will be prominent in patients with a unilateral cataract, because there is little of depth of focus in the pseudophakic eye, but normal depth of focus in the fellow eye. Interestingly, the mean age of the patients who developed ICL-induced cataract was 47.2±5.9 (mean±SD) years, which is higher than that of the overall population who underwent ICL implantation. We have already shown that the accommodation of eyes with subcapsular cataracts was considerably lower than that of eyes without cataract even in ICL-implanted eyes.20 We have also examined the amplitude of accommodation in patients aged 46–50 years old after ICL implantation, and found that it was 2.95±1.88 D (mean±SD), which was not much different from that (apparent accommodation, 2.01±0.92 D) in monofocal IOL-implanted eyes (unpublished data). As the higher patient age may lead to the lower amplitude of accommodation even in phakic eyes, the loss of accommodation in pseudophakic eyes may not be as severe as we presumed, and this may contribute to the high levels of subjective satisfaction.
It is known that the risk of retinal detachment after refractive lens exchange or cataract extraction has been increased in high myopic eyes. We found lattice degeneration without holes in two eyes, but did not perform any photocoagulation in these eyes during the follow-up period. Although we found no retinal detachment in this study, more prolonged observation is necessary.
In conclusion, our results support the view that simultaneous ICL removal and phacoemulsification with IOL implantation was safe and effective, and that the accuracy was predictable for the treatment of developing cataracts in ICL-implanted eyes. These combined surgical procedures also provided high levels of patient satisfaction. The results indicate that we had a viable surgical option even when a significant cataract occurred after ICL implantation, which was important for the prognosis of these complicated cases. A further study in a large series of patients is required to confirm these findings.
References
Zaldivar R, Davidorf JM, Oscherow S . Posterior chamber phakic intraocular lens for myopia of –8 to –19 diopters. J Refract Surg 1998; 14: 294–305.
Sanders DR, Brown DC, Martin RG, Shepherd J, Deitz MR, DeLuca M . Implantable contact lens for moderate to high myopia: phase 1 FDA clinical study with 6-month follow-up. J Cataract Refract Surg 1998; 24: 607–611.
Jimenez-Alfaro I, Gomez-Telleria G, Bueno JL, Puy P . Contrast sensitivity after posterior chamber phakic intraocular lens implantation for high myopia. J Refract Surg 2001; 17: 641–645.
Uusitalo RJ, Aine E, Sen NH, Laatikainen L . Implantable contact lens for high myopia. J Cataract Refract Surg 2002; 28: 29–36.
Bloomenstein MR, Dulaney DD, Barnet RW, Perkins SA . Posterior chamber phakic intraocular lens for moderate myopia and hyperopia. Optometry 2002; 73: 435–446.
Sanders DR, Vukich JA, Gaston M . Implantable Contact Lens in Treatment of Myopia Study Group. US Food and Drug Administration clinical trial of the Implantable Contact Lens for moderate to high myopia. Ophthalmology 2003; 110: 255–266.
Lackner B, Pieh S, Schmidinger G, Hanselmayer G, Dejaco-Ruhswurm I, Funovics MA et al. Outcome after treatment of ametropia with implantable contact lenses. Ophthalmology 2003; 110: 2153–2161.
Sanders DR, Doney K, Poco M . ICL in Treatment of Myopia Study Group. United States Food and Drug Administration clinical trial of the Implantable Collamer Lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology 2004; 111: 1683–1692.
Pineda-Fernandez A, Jaramillo J, Vargas J, Jaramillo M, Jaramillo J, Galindez A . Phakic posterior chamber intraocular lens for high myopia. J Cataract Refract Surg 2004; 30: 2277–2283.
Bleckmann H, Keuch RJ . Results of cataract extraction after implantable contact lens removal. J Cataract Refract Surg 2005; 31: 2329–2333.
Morales AJ, Zadok D, Tardio E, Anzoulatous Jr G, Litwak S, Mora R et al. Outcome of simultaneous phakic implantable contact lens removal with cataract extraction and pseudophakic intraocular lens implantation. J Cataract Refract Surg 2006; 32: 595–598.
Gonvers M, Bornet C, Othenin-Girard P . Implantable contact lens for moderate to high myopia: relationship of vaulting to cataract formation. J Cataract Refract Surg 2003; 29: 918–924.
Lackner B, Pieh S, Schmidinger G, Simader C, Franz C, Dejaco-Ruhswurm I et al. Long-term results of implantation of phakic posterior chamber intraocular lenses. J Cataract Refract Surg 2004; 30: 2269–2276.
Sarikkola AU, Sen HN, Uusitalo RJ, Laatikainen L . Traumatic cataract and other adverse events with the implantable contact lens. J Cataract Refract Surg 2005; 31: 511–524.
Fujisawa K, Shimizu K, Uga S, Suzuki M, Nagano K, Murakami Y et al. Changes in the crystalline lens resulting from insertion of a phakic IOL (ICL) into the porcine eye. Graefes Arch Clin Exp Ophthalmol 2007; 245: 114–122.
Sanders DR, Vukich JA, ICL in Treatment of Myopia (ITM) Study Group. Incidence of lens opacities and clinically significant cataracts with the implantable contact lens: comparison of two lens designs. J Refract Surg 2002; 18: 673–682.
Gonvers M, Othenin-Girard P, Bornet C, Sickenberg M . Implantable contact lens for moderate to high myopia: short-term follow-up of 2 models. J Cataract Refract Surg 2001; 27: 380–388.
Hoffer KJ . Ultrasound axial length measurement in biphakic eyes. J Cataract Refract Surg 2003; 29: 961–965.
Gimbel HV, Van Westenbrugge JA, Johnson WH, Willerscheidt AB, Sun R, Ferensowicz M . Visual, refractive, and patient satisfaction results following bilateral photorefractive keratectomy for myopia. Refract Corneal Surg 1993; 9: S5–S10.
Kamiya K, Shimizu K, Aizawa D, Ishikawa H . Time course of accommodation after implantable collamer lens implantation. Am J Ophthalmol 2008; 146: 674–678.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest: None
Rights and permissions
About this article
Cite this article
Kamiya, K., Shimizu, K., Igarashi, A. et al. Clinical outcomes and patient satisfaction after Visian Implantable Collamer Lens removal and phacoemulsification with intraocular lens implantation in eyes with induced cataract. Eye 24, 304–309 (2010). https://doi.org/10.1038/eye.2009.87
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.87
Keywords
This article is cited by
-
Multicenter clinical outcomes of hole implantable collamer lens implantation in middle-aged patients
Scientific Reports (2022)
-
Femtosecond laser assisted cataract surgery in a cataract patient with a “0 vaulted” ICL: a case report
BMC Ophthalmology (2020)
-
Safety and visual outcomes following posterior chamber phakic intraocular lens bilensectomy
Eye and Vision (2020)
-
Etiology and outcomes of current posterior chamber phakic intraocular lens extraction
Scientific Reports (2020)
-
Successful toric intraocular lens implantation in a patient with induced cataract and astigmatism after posterior chamber toric phakic intraocular lens implantation: a case report
Journal of Medical Case Reports (2012)