Abstract
Aims
To compare intraocular pressure (IOP) readings between Tono-Pen tonometry and GAT, between noncontact tonometry (NCT) and GAT, and between dynamic contour tonometry (DCT) and Goldmann applanation tonometry (GAT). The correlation between IOP reading and possible confounder was identified.
Methods
This observational cross-sectional study enrolled sixty-two healthy subjects. All IOP and ocular pulse amplitude (OPA) measurements were taken by a single ophthalmologist; mean keratometric power (MK), central corneal thickness (CCT), and lens thickness (LT) were measured by a single experienced technician.
Results
Stepwise multiple regression analysis indicated that GAT (P=0.017) and DCT (P=0.002) readings correlated positively with MK; GAT, NCT, and Tono-Pen readings correlated positively with CCT (P<0.05); NCT (P=0.035), and DCT (P=0.016) readings correlated negatively with LT; GAT (P=0.006) and Tono-Pen (P=0.009) readings correlated positively with OPA.
Conclusions
The K, CCT, LT, and OPA are confounders in tonometry readings.
Similar content being viewed by others
Introduction
Intraocular pressure (IOP) is a basic measurement in ocular examinations; however, its diagnostic value depends on the consistency of measurements. Abnormally high IOP can eventually cause progressive optic neuropathy. Since its initial introduction in 1954, Goldmann applanation tonometry (GAT) has become a commonly used method of IOP measurement.1, 2, 3 The principle of this method is corneal applanation, and its accuracy is affected by corneal properties such as central corneal thickness (CCT).1, 2 Noncontact tonometry (NCT) also exploits applanation principles by measuring differences in IOP before and after the flattening of the corneal surface by a concentrated burst of air.4 Notably, NCT has higher patient tolerability because it does not require direct contact between the instrument and the corneal surface. The Tono-Pen is a portable, handheld instrument that enables rapid IOP measurements. Precise IOP measurements require cooperative patients. For patients unable to tolerate IOP measurements, Tono-Pen tonometry is an attractive alternative. Dynamic contour tonometry (DCT) employs a non-applanation tonometer featuring a pressure-sensitive tip with a concave contact surface for measuring transcorneal IOP,3 and its measurement presumes identical pressure within and outside the globe,5 even when used in children.6 The DCT approach can also measure ocular pulse amplitude (OPA) by differentiating between diastolic and systolic IOP.5, 6
The accuracy of all of the above approaches is subject to varying subject age, mean keratometric power (MK), CCT, axial length (AL), and OPA.6, 7, 8, 9, 10 Further, the precise differences among GAT, NCT, Tono-Pen, and DCT have not been thoroughly investigated. Most previous studies compared at least two different tonometers, usually GAT with DCT.2, 3, 8, 11 However, NCT and Tono-Pen are now widely used in clinical practise. Clarifying the comparative differences and limitations of these tonometers would be of great interest to practitioners. The purpose of this study is to investigate the differences in IOP readings among DCT, Tono-Pen tonometry, NCT, and GAT and analyse the correlations among IOP readings and possible confounders, including subject age, MK, CCT, anterior chamber depth (ACD), lens thickness (LT), vitreous length (VL), AL, and OPA, in a population of Taiwan.
Materials and methods
Sixty-two healthy subjects were enrolled in this observational and cross-sectional study. Agreement and correlation of GAT (Goldmann AT 900/870, Haag-Streit, Switzerland), computerised NCT (NT-2000, Nidek, Gamagori, Japan), Tono-Pen—XL applanation tonometer (Tono-Pen, Medtronic, Jacksonville FL, USA) and DCT (Pascal; SMT Swiss Microtechnology AG, Port, Switzerland) were analysed to determine the effects of subject age, MK, CCT, ACD, LT, VL, AL, and OPA. This study was approved by the Ethics Committee of the Institutional Review Board at this facility, and all participants gave informed consent to participate in the study. The study was performed in accordance with Declaration of Helsinki principles, which were clearly explained to all participants.
One eye in each of the sixty-two subjects was randomly selected for analysis. Exclusion criteria were any history of the following: severe dry eye syndrome, drug allergy, glaucoma, systemic disease, ocular inflammation or trauma, or ocular surgery. The healthy subject with refractive error was not excluded. Complete ocular examination included best spectacle corrected visual acuity (BSCVA) by AutoRefractoKeratometer (ARK-700, Nidek; Gamagori, Japan) and Snellen chart visual acuity examinations; anterior segment and anterior vitreous examination by slit-lamp biomicroscopy; posterior vitreous, disc and macula examination by slit-lamp biomicroscopy with 90-D lens; and cup-to-disc ratio less than 0.4 and no asymmetry exceeding a ratio of 0.2 between fellow eyes in each subject by funduscopy; peripheral retina by indirect ophthalmoscopy; visual field screen by frequency doubling technology instrument (Zeiss-Humphrey, Dublin, CA, USA); and peripapillary retinal nerve fibre layer (RNFL) thickness measurements by optical coherence tomography (Stratus OCT, software version 4.0, Carl Zeiss Meditec, Dublin, CA, USA). Exclusion criteria were the following: BSCVA less than 16/20, abnormal anterior segment, significant macular lesion, abnormal disc morphology, or visual field screen and abnormal RNFL thickness.
A single ophthalmologist (Hsu SY) performed all IOP readings using GAT, NCT, Tono-Pen, and DCT as well as all OPA measurements. Each subject underwent all measurements in a single day. An experienced technician took all MK, CCT, ACD, LT, VL, AL, and SE measurements on a different day. The MK was measured three times using AutoRefractoKeratometer; CCT was measured five times at the corneal centre using ultrasonic pachymeter (OcuScan RxP, Alcon; Fort Worth, TX, USA); ACD, LT, VL, and AL were measured 10 times each using A-scan (OcuScan RxP, Alcon) with contact technique; measurements were averaged and recorded.
In all subjects, IOP was determined by a random sequence of tonometric tests. Each tonometer was used to take three readings in each subject, and the average reading was recorded for each participant. In each participant, the cornea was anaesthetised before measurement with one drop of 0.5% proparacaine hydrochloride (Alcaine, Alcon Pharma; Puurs, Belgium). Before GAT measurement in each subject, the GAT probe was cleaned with 70% isopropyl alcohol and then dried. The examining physician cleaned the compressed air nozzle before NCT measurement in each subject. A new disposable tip diaphragm was used for DCT or Tono-Pen measurements in each subject. Before each GAT measurement, the fluorescein strip was stained on the inferior ocular fornix. If pulse pressure was detected, the intermediate pressure reading was recorded as the IOP. When performing NCT, the alignment was confirmed by positioning the alignment light close to the alignment circle, and the NT-2000 initiated the measurement after focusing. Readings using the Tono-Pen were taken by applying light pressure to the cornea with a 1.5 mm transducer tip. When using DCT, correct positioning was indicated by an audible signal with a pitch proportional to the IOP. The pressure signal was detected over 4 s, which corresponds to five to ten heartbeats. After lifting the tip away from the surface of the eye, the IOP and OPA were calculated automatically and shown on a display screen with the OPA and the quality score (Q). Scores of Q1 (optimum) to Q3 were acceptable, and scores of Q4 and Q5 were deemed unacceptable and excluded.
The IOP measurements were taken with the subjects relaxed in a seated position with both eyes open. Subjects were asked to breathe normally and to fixate on an object behind the examiner without blinking. All examinations were performed during the same time of day, between 1400 and 1700 hours. The mean of three consecutive tonometry measurements per device was used for statistical analysis.
The SPSS software (SPSS Institute Inc., Chicago, IL, USA) was used for statistical analysis. Paired t-test was used to compare the IOP readings between two tonometry methods. The analysis of variability was determined using a coefficient of variation (CV) defined as 100% × standard deviation (SD)/mean. Pearson correlation method and linear regression analysis were used to verify correlations among tonometry readings and possible confounders. Stepwise multiple regression analysis with a forward selection procedure was used to analyse possible confounders of tonometry readings. The tonometry readings were analysed as dependent variables, and possible confounders were analysed as independent variables. The coefficient (r) was used to estimate the degree of correlation. A P-value less than 0.05 or an F-value greater than 4.000 was considered statistically significant. For multiple comparisons, the α levels were adjusted by Bonferroni-modified test.
Results
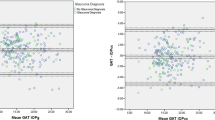
The mean age of enrolled subjects was 44.3±9.5 years (range, 20–72 years), and the average SE was 2.001±2.288 D (range 0.00–8.63 D). Table 1 displays the tonometry readings and possible confounders. The DCT measurements (20.976%) had a lower CV than the GAT measurements (28.06%) did. Further, Tono-Pen (18.5%) and NCT (19.76%) measurements had lower CVs than GAT and DCT measurements did. Paired t-test revealed significant differences between DCT and NCT (P=0.024), between DCT and GAT (P<0.001), between Tono-Pen and NCT (P=0.022) and between Tono-Pen and GAT (P<0.001); however, no significant differences were noted between DCT and Tono-Pen (P=0.659) or between NCT and GAT (P=0.110). Figure 1a indicates that the difference between Tono-Pen and GAT readings correlated negatively with the average of the two tonometry readings by Bland–Altman plots (P<0.001).
The difference of Tono-Pen and GAT IOP readings was negatively associated with the average of the two tonometry readings by Bland–Altman plots (a). CCT was positively associated with GAT (g, P=0.035), NCT (n, P=0.017) and Tono-Pen (t, P=0.005) but not DCT (d, P=0.889) IOP readings by Pearson's correlation method and linear regression analysis (b). CCT was the confounder to the differences of DCT and GAT tonometry readings (c). OPA was the confounder to the differences of DCT and GAT (d) and those of NCT and GAT tonometry readings (e).
Table 2 shows the results of correlation analysis among tonometry readings and possible confounders. The GAT readings correlated positively with K (P=0.032), CCT (P=0.035), and OPA (P=0.001); NCT readings correlated positively with CCT (P=0.017), VL (P=0.036), and AL (P=0.039) but negatively with subject age (P=0.040) and LT (P=0.026); Tono-Pen readings correlated positively with CCT (P=0.005) and OPA (P=0.001); DCT readings correlated positively with K (P=0.001) and ACD (P=0.035), but negatively with LT (P=0.009). However, three applanated tonometers, including GAT (P=0.035), NCT (P=0.017), and Tono-Pen (P=0.005), were positively associated with CCT, otherwise, DCT had no significant correlation with CCT (P=0.889) (Figure 1b).
Table 3 shows the analytical results among the correlated confounders (Table 2, by Pearson's correlation method) and tonometry readings using stepwise multiple regression analysis with a forward selection procedure and Bonferroni-modified test. The K, CCT, and OPA were significantly related to GAT reading (F=8.198, r=0.684, GAT reading=−56.177+1.071 × K+0.033 × CCT+1.751 × OPA). The CCT and LT were significantly related to NCT reading (F=10.652, r=0.651, NCT reading=−1.569+0.058 × CCT−3.312 × LT). The CCT and OPA were significantly related to Tono-Pen reading (F=9.562, r=0.630, Tono-Pen reading=−7.298+0.036 × CCT+1.211 × OPA). The K and LT were significantly related to DCT reading (F=10.808, r=0.653, DCT reading=−24.117+1.161 × K−2.671 × LT).
CCT was a confounder to the difference between DCT and GAT readings (P<0.001) (Figure 1c), and there was no significant correlation to the differences between Tono-Pen and GAT (P=0.561) and between NCT and GAT readings (P=0.928). OPA was a confounder to the differences between DCT and GAT (P<0.001) (Figure 1d) and between NCT and GAT (P<0.001) (Figure 1e).
Discussion
Applanation tonometry methods commonly used for IOP measurement include GAT, NCT, and Tono-Pen. Kanngiesser et al1 proposed that true IOP could be measured by an equilibrium of IOP, corneal rigidity, adhesion force of the tear film and appositional force and by DCT. In this study, DCT readings were highest and GAT readings were lowest. Tono-Pen readings were higher than NCT readings, and both Tono-Pen and NCT readings were higher than those of GAT, but lower than those of DCT. Further, IOP readings did not significantly differ between DCT and Tono-Pen or between NCT and GAT. Kaufmann et al2 reported less variation in DCT readings than in GAT readings. In this study, CVs for DCT, Tono-Pen, NCT, and GAT measurements were 20.976, 18.5, 19.76, and 28.06%, respectively. However, although DCT, Tono-Pen, and NCT readings revealed less variability than those of GAT, their measurements were not necessarily more consistent. Instead, the reduced variability may indicate that, in comparison with GAT, these three methods consistently obtain lower values in the high IOP range and higher values in the low IOP range. Although this study obtained CV data for each tonometry method across the entire study population, and although some tonometers might exaggerate or underestimate true variations, this study revealed a large SD in GAT measurements despite its low mean tonometry reading, which increased its CV. These findings are consistent with the data reported in Kaufmann et al2 Nevertheless, the lack of consistent IOP measurements obtained for a population does not indicate that the tonometer is inaccurate. However, the accuracy of the tonometer should be questioned if repeated measurements of a single subject within a short period of time are highly variable. Tono-Pen or NCT can quickly determine IOP levels and GAT and DCT require several seconds to determine the IOP. Previous reports suggest that using an audio cue during DCT is effective for helping the patient keep the eye open during measurements.2, 3 Although GAT is widely used for IOP measurement, DCT, Tono-Pen or NCT, are also useful for comparison purposes when considering multiple tonometry measurements in a single subject. Nevertheless, the current study indicated that the difference between Tono-Pen and GAT readings is inversely related to IOP value. The user should therefore avoid underestimating IOP readings when using Tono-Pen in a subject in which GAT obtains high IOP.
Tonometry readings using applanation tonometers are reportedly subject to various confounders.6, 7, 8, 9, 10 Previous reports also indicate that tonometry readings may deviate due to varying ocular biomechanical properties12, 13 This study therefore analysed the correlation between tonometry readings and available parameters of the ocular surface or inner structure. In this study, GAT and DCT readings correlated positively with K; GAT, NCT, and Tono-Pen readings, correlated positively with CCT; NCT and DCT readings correlated negatively with LT; GAT and Tono-Pen readings correlated positively with OPA according to Pearson analysis and stepwise multiple regression analysis.
Previous reports indicate that tonometry readings are dependent on biomechanical properties such as corneal curvature.12 The manufacturer of the DCT device has noted that non-applanation DCT readings are theoretically not significantly associated with K. Medeiros and Schneider et al9, 14 indicated that DCT and GAT are not significantly affected by K. However, Francis et al8 reported that K affects DCT readings, and Medeiros et al13 reported that K affects GAT readings. This study showed that GAT and DCT readings were all influenced by K and that steeper corneas correlate with higher readings. The DCT readings required contact with the eye for at least 3 s. Although the tip of the DCT resembles t to the surface of the central cornea, some applanation of the corneal surface is still needed to achieve sufficient contact area for the measuring tool to automatically calculate IOP. Otherwise, neither NCT nor Tono-Pen was significantly affected by K in this study. In subjects with highly variable corneal curvatures, NCT or Tono-Pen might be superior for IOP measurements.
Regarding CCT, IOP readings using applanation tonometers usually increase with thicker CCT.6, 9, 10, 12 Previous reports have proposed various CCT-based correction formulas for GAT;15, 16 however, some studies suggested that the nonlinear correlation between GAT readings and CCT precludes a simple correction formula.17, 18, 19 In some cases, the magnitude of change in IOP might be disproportional to ablation depth after refractive surgery.20 Our results indicate that GAT, NCT, and Tono-Pen correlate positively with CCT, but DCT readings do not. This finding is consistent with previous reports that DCT readings are not significantly associated with CCT.9, 21 Previous reports also indicate that CCT affects GAT significantly more than it affects DCT22 and that its effects on NCT are significantly greater than its effects on GAT,4 both of which are consistent with the current findings. The differences between DCT and GAT were larger in a thinner CCT and decreased as the CCT increased in the current study. The GAT measurement requires applanation of the corneal surface; hence, the thicker the cornea, the greater the bending force required. A similar effect is observable in NCT and Tono-Pen, which also produce varying corneal deformation depending on the force required for IOP measurements. Although applanation tonometry readings do not always reflect true IOP values and varying CCT produce substantial reading deviations,6, 9, 10, 12 CCT accounts for only a portion of tonometry reading errors. The GAT technique assumes that the internal fluid pressure exerted on a thin membrane sphere is the pressure required to flatten an area of the membrane.23 However, corneas actually have a finite thickness, which varies individually. In addition, the cornea, limbus and sclera differ in their biomechanical properties and rigidity.24 A more likely cause is ocular biomechanical properties12, 24 rather than only CCT. Therefore, varying cornea–limbus–scleral structural properties and varying ocular rigidity can cause substantial deviations in applanation tonometry readings. In subjects with unusually thin corneas or in those who have undergone post-refractive surgery, DCT may be superior for IOP measurements. In addition, the user should be careful to avoid underestimating IOP when using GAT rather than DCT in subjects with thin CCT.
Sihota et al6 reported that applanation tonometry readings decrease with longer AL in children. However, subsequent investigations of AL in children by Lee et al25 and of AL in adults by Morgan et al26 revealed no significant associations between IOP readings and AL. This study found that tonometry readings are unaffected by AL. Otherwise, LT was significantly associated with NCT or DCT readings. Although subjects with variable lens change no matter what the acquired or senile conditions are, a clinician could consider using GAT or Tono-Pen to measure IOP. Some studies have reported a positive association between IOP and OPA5, 7, 15, 27 In this study, OPA correlated positively with GAT and Tono-Pen readings, but was not significantly associated with NCT or DCT. Further, larger OPA was negatively correlated with the differences between DCT and GAT readings and between NCT and GAT readings. Isolated hypertension (systolic blood pressure substantially higher than diastolic blood pressure) is common in the elderly, but rare in young adults. Vascular smooth muscle elasticity also decreases with age. We postulate that NCT or DCT might be independent of OPA, even though OPA tends to vary in elderly subjects who have decreased vascular elasticity or who are susceptible to isolated hypertension. However, clinicians should be careful to avoid underestimating IOP readings in subjects with high OPA when using NCT or DCT and to avoid overestimating IOP readings in such subjects when using GAT.
An IOP reading is an important parameter for diagnosing glaucoma as well as for monitoring its treatment response, and the tonometry reading is subject to varying measuring tools and confounders. Because this study analysed only healthy subjects, the narrow range of confounders may limit the clinical use of IOP measurements because they are particularly important for diagnosing pathological conditions like glaucoma. Further studies are needed to investigate tonometry readings and confounders in a population of glaucoma patients. However, this study demonstrated that K was significantly associated with GAT and DCT readings. The CCT was a confounder when using applanation tonometry including GAT, NCT, or Tono-Pen, but was not significantly associated with DCT readings. The LT was significantly associated with NCT or DCT readings. The OPA was significantly associated with GAT or Tono-Pen readings. Clinicians should be careful to avoid underestimating IOP when using a tonometer. The differences between Tono-Pen and GAT readings were higher when IOP values were lower and decreased as the IOP increased. The differences between DCT and GAT were larger in a thinner CCT and decreased and the CCT increased. The differences between DCT and GAT readings and between NCT and GAT readings were higher when OPA values were lower and decreased as the OPA increased. These findings are clinically valuable when evaluating an individual eye using different tonometries, and clinicians must select the most accurate tonometer for IOP measurements in subjects with varying ocular properties or take multiple tonometry measurements to avoid underestimating IOP.
References
Kanngiesser HE, Kniestedt C, Robert YC . Dynamic contour tonometry: presentation of a new tonometer. J Glaucoma 2005; 14: 344–350.
Kaufmann C, Bachmann LM, Thiel MA . Comparison of dynamic contour tonometry with goldmann applanation tonometry. Invest Ophthalmol Vis Sci 2004; 45: 3118–3121.
Ku JY, Danesh-Meyer HV, Craig JP, Gamble GD, McGhee CN . Comparison of intraocular pressure measured by Pascal dynamic contour tonometry and Goldmann applanation tonometry. Eye 2006; 20: 191–198.
Tonnu PA, Ho T, Newson T, El Sheikh A, Sharma K, White E et al. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. Br J Ophthalmol 2005; 89: 851–854.
Kaufmann C, Bachmann LM, Robert YC, Thiel MA . Ocular pulse amplitude in healthy subjects as measured by dynamic contour tonometry. Arch Ophthalmol 2006; 124: 1104–1108.
Sihota R, Tuli D, Dada T, Gupta V, Sachdeva MM . Distribution and determinants of intraocular pressure in a normal pediatric population. J Pediatr Ophthalmol Strabismus 2006; 43: 14–18.
Kniestedt C, Lin S, Choe J, Nee M, Bostrom A, Stürmer J et al. Correlation between intraocular pressure, central corneal thickness, stage of glaucoma, and demographic patient data: prospective analysis of biophysical parameters in tertiary glaucoma practice populations. J Glaucoma 2006; 15: 91–97.
Francis BA, Hsieh A, Lai MY, Chopra V, Pena F, Azen S, et al., Los Angeles Latino Eye Study Group. Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology 2007; 114: 20–26.
Medeiros FA, Sample PA, Weinreb RN . Comparison of dynamic contour tonometry and goldmann applanation tonometry in African-American subjects. Ophthalmology 2007; 114: 658–665.
Kotecha A, Elsheikh A, Roberts CR, Zhu H, Garway-Heath DF . Corneal thickness and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Invest Ophthalmol Vis Sci 2006; 47: 5337–5347.
Doyle A, Lachkar Y . Comparison of dynamic contour tonometry with Goldman applanation tonometry over a wide range of central corneal thickness. J Glaucoma 2005; 14: 288–292.
Liu J, Roberts CJ . Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg 2005; 31: 146–155.
Medeiros FA, Weinreb RN . Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma 2006; 15: 364–370.
Schneider E, Grehn F . Intraocular pressure measurement-comparison of dynamic contour tonometry and goldmann applanation tonometry. J Glaucoma 2006; 15: 2–6.
Punjabi OS, Ho HK, Kniestedt C, Bostrom AG, Stamper RL, Lin SC . Intraocular pressure and ocular pulse amplitude comparisons in different types of glaucoma using dynamic contour tonometry. Curr Eye Res 2006; 31: 851–862.
Martinez-de-la-Casa JM, Garcia-Feijoo J, Vico E, Fernandez-Vidal A, Benitez del Castillo JM, Wasfi M et al. Effect of corneal thickness on dynamic contour, rebound, and Goldmann tonometry. Ophthalmology 2006; 113: 2156–2162.
Kniestedt C, Lin S, Choe J, Bostrom A, Nee M, Stamper RL . Clinical comparison of contour and applanation tonometry and their relationship to pachymetry. Arch Ophthalmol 2005; 123: 1532–1537.
Stodtmeister R . Applanation tonometry and correction according to corneal thickness. Acta Ophthalmol Scand 1998; 76: 319–324.
Elsheikh A, Wang D, Kotecha A, Brown M, Garway-Heath D . Evaluation of Goldmann applanation tonometry using a nonlinear finite element ocular model. Ann Biomed Eng 2006; 34: 1628–1640.
Hsu SY, Chang MS, Lee CJ . Intraocular Pressure Assessment in both eyes of the same patient after Laser in situ Keratomileusis. J Cataract Refract Surg 2009; 35 (1): 76–82.
Kniestedt C, Nee M, Stamper RL . Dynamic contour tonometry: a comparative study on human cadaver eyes. Arch Ophthalmol 2004; 122: 1287–1293.
Kotecha A, White ET, Shewry JM, Garway-Heath DF . The relative effects of corneal thickness and age on Goldmann applanation tonometry and dynamic contour tonometry. Br J Ophthalmol 2005; 89: 1572–1575.
Herndon LW . Measuring intraocular pressure-adjustments for corneal thickness and new technologies. Curr Opin Ophthalmol 2006; 17: 115–119.
Goldmann H, Schmidt T . Uber applanationstonometrie. Ophthalmologica 1957; 134: 221–242.
Lee AJ, Saw SM, Gazzard G, Cheng A, Tan DT . Intraocular pressure associations with refractive error and axial length in children. Br J Ophthalmol 2004; 88: 5–7.
Morgan AJ, Harper J, Hosking SL, Gilmartin B . The effect of corneal thickness and corneal curvature on pneumatonometer measurements. Curr Eye Res 2002; 25: 107–112.
Mori F, Konno S, Hikichi T, Yamaguchi Y, Ishiko S, Yoshida A . Factors affecting pulsatile ocular blood flow in normal subjects. Br J Ophthalmol 2001; 85: 529–530.
Acknowledgements
Paul Steve Lugue is appreciated for assistance with paper review and English editing. No financial support was received.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsu, SY., Sheu, MM., Hsu, AH. et al. Comparisons of intraocular pressure measurements: Goldmann applanation tonometry, noncontact tonometry, Tono-Pen tonometry, and dynamic contour tonometry. Eye 23, 1582–1588 (2009). https://doi.org/10.1038/eye.2009.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.77
Keywords
This article is cited by
-
Agreement of ocular response analyzer cornea compensated IOP with corvis ST biomechanical IOP following Femtosecond Laser-assisted LASIK
Eye (2023)
-
Comparative analysis of biomechanically corrected intraocular pressure with corneal visualization Scheimpflug technology versus conventional noncontact intraocular pressure
International Ophthalmology (2020)
-
Analysis of differences in intraocular pressure evaluation performed with contact and non-contact devices
BMC Ophthalmology (2018)
-
Agreement between diurnal variations of intraocular pressure by Tono-Pen and Goldmann applanation tonometer in patients on topical anti-glaucoma medication
International Ophthalmology (2016)
-
Indentation and needle insertion properties of the human eye
Eye (2014)