Abstract
Purpose
To investigate, by transmission electron microscopy (TEM), the effect on the posterior capsule of a young rabbit eye of 5-fluorouracil (5-FU) or thapsigargin in a sealed-capsule irrigation device.
Setting
St Erik's Eye Hospital, Stockholm, Sweden.
Methods
Clear lens extraction was performed unilaterally in eight 4-week-old rabbits. A sealed-capsule irrigation device was irrigated for 2 min with 20 ml of one of the following: balanced salt solution (BSS; n=2), thapsigargin 300 μ M (n=2), 5-FU 50 mg/ml (n=2), or 5-FU 25 mg/ml (n=2). The substances were washed out for 10 s with BSS. The eyes were left aphakic. Six weeks postoperatively, the animals were killed, and the posterior capsule was extracted and fixed for TEM. As a control, we also evaluated the capsules from the two fellow eyes in the BSS group that did not undergo surgery.
Results
The ultrastructure of the posterior capsule in eyes irrigated with 5-FU or thapsigargin did not differ from that in the eyes irrigated with BSS or in the eyes that did not have surgery. The membranes had the same ultrastructure with thin collagen fibres on the anterior and posterior face of the posterior capsule and an amorphic matrix.
Conclusion
Thapsigargin or 5-FU used in a sealed-capsule irrigation device does not seem to harm the posterior capsule, which appeared similar to when the capsule is irrigated with BSS.
Similar content being viewed by others
Introduction
Preventing posterior capsule opacification (PCO) plays an important role in improving visual acuity after cataract surgery in adults and children.1, 2 Recently, the use of antiproliferative drugs has been studied as a successful modality to target lens epithelial cells (LECs).3, 4, 5, 6 The sealed-capsule irrigation device (SCI) Perfect Capsule7, 8 (Milvella Ltd, Epping, Australia) was reported to be highly efficacious in sealing the capsular bag from the adjacent ocular structures in rabbit eyes.3 In humans, Rabsilber et al,9 reported that the device was safe when used after phacoemulsification. The capsular bag then was flushed with distilled deionized water (DDW), and afterwards a hydrophilic intraocular lens (IOL) was implanted. Irrigation with DDW, however, did not prevent the development of PCO either in humans9 or rabbits.3
We observed a beneficial effect in preventing PCO when the sealed system was irrigated with 5-fluorouracil (5-FU) 50 mg/ml in an animal model.3 We also reported the safety of 5-FU 50 mg/ml when used with the Perfect Capsule with no harmful effects to the surrounding tissues, such as the corneal endothelium, trabecular meshwork, and retina in young rabbits.10 We also evaluated a lower concentration of 5-FU (25 mg/ml), but this concentration did not have the same beneficial effect.4 Irrigation with thapsigargin also did not have a good effect in rabbit eyes;4 however, thapsigargin used in vitro in human capsules did have a beneficial effect.5
It is important to ascertain that the capsular bag is not damaged by either the use of an antiproliferative drug or by the absence of LECs. In this study of rabbit eyes, we used transmission electron microscopy (TEM) to study the posterior capsule morphology after exposure to different irrigation substances in the SCI system.
Materials and methods
Animals
Eight New Zealand 4-week-old white rabbits (average weight, 315 g) underwent unilateral clear lens extraction. The experiment was approved by the Northern Stockholm Animal Experiments Ethics Committee and adhered to the Association for Research in Vision and Ophthalmology statement on the use of animals in ophthalmic and vision research.
Surgery
Surgery was performed by one experienced anterior segment surgeon after general anaesthesia was induced as described previously.3 Briefly, a 2.8-mm clear corneal incision and small capsulorrhexis were created. Clear lens extraction using irrigation/aspiration was performed and the Perfect Capsule was inserted and sealed to the anterior capsule. The capsule was flushed with one of four substances for 2 min and balanced saline solution (BSS) for 10 s to wash out the residual substance, and the incision was closed with a 10-0 nylon suture. Cefuroxime (1 mg) was injected intracamerally at the end of surgery.
Study design
Two eyes each were irrigated with either BSS, thapsigargin 300 μ M (Sigma), 5-FU 50 mg/ml, or 5-FU 25 mg/ml. About 20 ml of each substance was washed through the system during the 2-min irrigation period.
All animals were sacrificed 6 weeks after surgery. The operated eye was enucleated and the capsular bag was dissected and immediately placed in fixative. To compare the capsules of the operated eyes with normal non-operated phakic eyes, we also extracted the capsular bags including the crystalline lens of the two fellow eyes in the rabbits irrigated with BSS.
TEM
The capsular bag was dissected and small pieces were fixed in 2% glutaraldehyde and 0.5%. paraformaldehyde in 0.1 M sodium cacodylate buffer containing 0.1 M sucrose and 3 mM CaCl2 (pH 7.4) at room temperature for 30 min followed by 24 h at 4°C. Specimens were rinsed in 0.15 M sodium cacodylate buffer containing 3 mM CaCl2 (pH 7.4), postfixed in 2% osmium tetroxide in 0.07 M sodium cacodylate buffer containing 1.5 mM CaCl2 (pH 7.4) at 4°C for 2 h, dehydrated in ethanol followed by acetone and embedded in LX-112 (Ladd, Burlington, VT, USA). Semi-thin sections were cut and stained with toludine blue and used for light microscopic analysis. Ultrathin sections (approximately 40–50 nm) were cut and contrasted with uranyl acetate followed by lead citrate and examined in a Tecnai 10 transmission electron microscope at 80 kV. Digital images were taken by using a Mega View III digital camera (Soft Imaging System, GmbH, Münster, Germany).11
Results
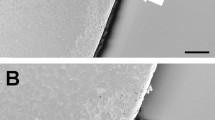
TEM showed an ultrastructure of thin collagen fibres on the anterior and posterior part of the posterior capsule. The collagen fibres are thin parallel lines that comprise approximately one-third of the thickness of the membrane. The rest of the membrane is embedded in an amorphic matrix. The ultrastructure was similar in all eyes, and no damage was observed in the eyes irrigated with BSS, 5-FU, or thapsigargin (Figure 1).
The specimens from the non-operated eyes were more difficult to analyse, probably because they included the crystalline lens, which makes sectioning difficult. However, morphologic analysis of the capsules showed the same ultrastructure compared with the operated eyes (Figure 2).
Discussion
This study showed no morphologic changes in the posterior capsule after irrigation with either thapsigargin or 5-FU. It is important to determine whether the capsule is damaged by different drugs or an absence of cells, since the capsule might rupture and the IOL could dislocate. The optimal substance and irrigation time associated with the Perfect Capsule have been debated and studied extensively. The substance that initially was intended to be used, DDW, was ineffective in humans or rabbits.3, 9 Mitomycin C or 5-FU has been reported to inhibit the proliferation of LECs and prevent PCO.3, 6 However, the use of these agents may be toxic to the ocular tissues. In our previous study of the safety of 5-FU 50 mg/ml, the adjacent ocular tissues were undamaged even when 5-FU was injected into the bag without the Perfect Capsule and left for 2 min before aspiration and irrigation.10 The previously cited study of mitomycin C with the Perfect Capsule reported that the drug was safe and did not damage the anterior lens capsule and central corneal endothelium, but its effect on the posterior capsule needs to be tested. In addition, if leakage occurs, it is uncertain whether mitomycin C is safe, because in that study, Perfect Capsule was used in all eyes.6 Mitomycin C and colchicine use in other studies had been reported to inhibit the growth of LEC.12, 13 Mitomycin C also was reported to damage cultured corneal keratocytes and cause bullous keratopathy in patients with glaucoma.14, 15 The safety of mitomycin C is questionable.
SCI increases the potential use of antimetabolites to target the LECs after cataract surgery. TEM has been used earlier to evaluate the lens and capsule.16, 17 A limitation of this study is that only two eyes were exposed to each substance and analysed with TEM, and of course we cannot be certain that there was no damage caused by the substance. No statistics is possible to perform with such a small sample size. Further studies are needed.
In conclusion, our results are promising regarding the use of 5-FU and thapsigargin with the Perfect Capsule. Morphologic evaluation showed that there was no damage to the posterior capsule when investigated with TEM.
References
Spalton DJ . Posterior capsular opacification after cataract surgery. Eye 1999; 13 (Pt 3b): 489–492.
Zetterstrom C, Lundvall A, Kugelberg M . Cataracts in children. J Cataract Refract Surg 2005; 31: 824–840.
Abdelwahab MT, Kugelberg M, Kugelberg U, Zetterstrom C . After-cataract evaluation after using balanced salt solution, distilled deionized water, and 5-fluorouracil with a sealed-capsule irrigation device in the eyes of 4-week-old rabbits. J Cataract Refract Surg 2006; 32: 1955–1960.
Abdelwahab MT, Kugelberg M, Zetterstrom C . Irrigation with thapsigargin and various concentrations of 5-fluorouracil in a sealed-capsule irrigation device in young rabbit eyes to prevent after cataract. Eye 2008; 28: e-pub ahead of print.
Duncan G, Wang L, Neilson GJ, Wormstone IM . Lens cell survival after exposure to stress in the closed capsular bag. Invest Ophthalmol Vis Sci 2007; 48: 2701–2707.
Kim SY, Kim JH, Choi JS, Joo CK . Comparison of posterior capsule opacification in rabbits receiving either mitomycin-C or distilled water for sealed-capsule irrigation during cataract surgery. Clin Experiment Ophthalmol 2007; 35: 755–758.
Maloof A, Neilson G, Milverton EJ, Pandey SK . Selective and specific targeting of lens epithelial cells during cataract surgery using sealed-capsule irrigation. J Cataract Refract Surg 2003; 29: 1566–1568.
Maloof AJ, Pandey SK, Neilson G, Milverton EJ . Selective death of lens epithelial cells using demineralized water and Triton X-100 with PerfectCapsule sealed capsule irrigation: a histological study in rabbit eyes. Arch Ophthalmol 2005; 123: 1378–1384.
Rabsilber TM, Limberger IJ, Reuland AJ, Holzer MP, Auffarth GU . Long-term results of sealed capsule irrigation using distilled water to prevent posterior capsule opacification: a prospective clinical randomised trial. Br J Ophthalmol 2007; 91: 912–915.
Abdelwahab MT, Kugelberg M, Seregard S, Zetterstrom C . Safety of irrigation with 5-fluorouracil in a sealed-capsule irrigation device in the rabbit eye. J Cataract Refract Surg 2007; 33: 1619–1623.
Park CB, Asin-Cayuela J, Camara Y, Shi Y, Pellegrini M, Gaspari M et al. MTERF3 is a negative regulator of mammalian mtDNA transcription. Cell 2007; 130: 273–285.
Haus CM, Galand AL . Mitomycin against posterior capsular opacification: an experimental study in rabbits. Br J Ophthalmol 1996; 80: 1087–1091.
Ismail MM, Alio JL, Ruiz Moreno JM . Prevention of secondary cataract by antimitotic drugs: experimental study. Ophthalmic Res 1996; 28: 64–69.
Mietz H, Roters S, Krieglstein GK . Bullous keratopathy as a complication of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol 2005; 243: 1284–1287.
Wu KY, Hong SJ, Huang HT, Lin CP, Chen CW . Toxic effects of mitomycin-C on cultured corneal keratocytes and endothelial cells. J Ocul Pharmacol Ther 1999; 15: 401–411.
Al-ghoul KJ, Novak LA, Kuszak JR . The structure of posterior subcapsular cataracts in the Royal College of Surgeons (RCS) rats. Exp Eye Res 1998; 67: 163–177.
Pandey SK, Cochener B, Apple DJ, Colin J, Werner L, Bougaran R et al. Intracapsular ring sustained 5-fluorouracil delivery system for the prevention of posterior capsule opacification in rabbits: a histological study. J Cataract Refract Surg 2002; 28: 139–148.
Acknowledgements
The Financial support for this study was provided through a regional agreement on medical training and clinical research (ALF) between the Stockholm county council and the Karolinska Institutet. The study also was supported in part by Stiftelsen Synfrämjandets Forskningsfond, the Jerring Foundation, Stiftelsen Kronprinsessan Margaretas Arbetsnämnd för Synskadade and Sigvard and Marianne Bernadottes Forskningsstiftelse för Barnögonvård, Sweden.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors have a proprietary or financial interest in any material, method, or product mentioned
Rights and permissions
About this article
Cite this article
Abdelwahab, M., Lindell, I., Hultenby, K. et al. Transmission electron microscopy of the rabbit posterior capsule irrigated with thapsigargin and 5-fluorouracil in a sealed-capsule irrigation device. Eye 23, 975–978 (2009). https://doi.org/10.1038/eye.2008.216
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.216