Abstract
Cinnamyl alcohol (CAL) is known as an antipyretic, and a recent study showed its vasodilatory activity without explaining the mechanism. Here we demonstrate the vasodilatory effect and the mechanism of action of CAL in rat thoracic aorta. The change of tension in aortic strips treated with CAL was measured in an organ bath system. In addition, vascular strips or human umbilical vein endothelial cells (HUVECs) were used for biochemical experiments such as Western blot and nitrite and cyclic guanosine monophosphate (cGMP) measurements. CAL attenuated the vasoconstriction of phenylephrine (PE, 1 µM)-precontracted aortic strips in an endothelium-dependent manner. CAL-induced vasorelaxation was inhibited by pretreatment with NG-nitro-L-arginine methyl ester (L-NAME; 10-4 M), methylene blue (MB; 10-5 M) and 1 H-[1,2,4]-oxadiazolole-[4,3-a] quinoxalin-10one, (ODQ; 10-6 or 10-7 M) in the endothelium-intact aortic strips. Atrial natriuretic peptide (ANP; 10-8 or 10-9 M) did not affect the vasodilatory effect of CAL. The phosphorylation of endothelial nitric oxide synthase (eNOS) and generation of nitric oxide (NO) were stimulated by CAL treatment in HUVECs and inhibited by treatment with L-NAME. In addition, cGMP and PKG1 activation in aortic strips treated with CAL were also significantly inhibited by L-NAME. Furthermore, CAL relaxed Rho-kinase activator calpeptin-precontracted aortic strips, and the vasodilatory effect of CAL was inhibited by the ATP-sensitive K+ channel inhibitor glibenclamide (Gli; 10-5 M) and the voltage-dependent K+ channel inhibitor 4-aminopyridine (4-AP; 2 × 10-4 M). These results suggest that CAL induces vasorelaxation by activating K+ channels via the NO-cGMP-PKG pathway and the inhibition of Rho-kinase.
Similar content being viewed by others
Introduction
CAL (Figure 1) is a well-known component of Cinnamomi cortex and C. ramulus (Gong et al., 2004; He et al., 2005). The plant phenolic CAL is used as a fragrance ingredient and has antipyretic and antiproliferative effects (Letizia et al., 2005; Guo et al., 2006; Ng and Wu, 2011). A recent report also demonstrated its vasodilatory activity (Ibarra-Alvarado et al., 2009). However, vasodilation as a mechanism for its antihypertensive effect has not been investigated.
High blood pressure is closely related to hypertension, arrhythmia, heart failure, and atherosclerosis. For this reason, regulation of vascular tone is very important in the treatment of hypertension-induced vascular diseases. Vascular dilation by relaxation of smooth muscle cells in the blood vessels is an effective means of lowering high blood pressure (Rich, 2009; Félétou et al., 2010).
In particular, endothelium-derived nitric oxide (NO) has an important role in the regulation of vascular smooth muscle tension (Vanhoutte and Scott-Burden, 1994). NO is produced by endothelial nitric oxide synthase (eNOS) and diffuses to smooth muscle (Palmer et al., 1987; Vanhoutte and Scott-Burden, 1994) where it then interacts with soluble guanylyl cyclase (sGC). Activation of sGC by NO stimulates the generation of guanosine 3',5'-cyclic monophosphate (cGMP) from guanosine triphosphate (GTP) (Ignarro et al., 1987, 1999). cGMP consequently activates cGMP-dependent protein kinase (PKG) (Qi et al., 2007; Prieto, 2008), which stimulates vascular relaxation through activation of K+ channels or inhibition of Ca2+ sensitization by activating myosin light-chain (MLC) phosphatase (Surks, 2007; Chai and Lin, 2008; Kitazawa et al., 2009; Chai et al., 2011).
Four types of K+ channels in arterial smooth muscle have been identified, voltage-dependent K+ channels, Ca2+-activated K+ channels, inward rectifier K+ channels, and ATP-sensitive K+ channels, which regulate a variety of vasoactive signals by changing the membrane potential (Kubo et al., 1994; Nelson and Quayle, 1995). In addition, activation of MLC phosphatase through NO-cGMP-PKG signaling is involved in the inhibition of Ca2+ sensitization by Rho-kinase signaling (Lee et al., 2004; Surks, 2007; Kitazawa et al., 2009).
In the present study, we demonstrate the vasodilatory effects of CAL and its mechanism in rat thoracic aorta.
Results
Cytotoxicity of CAL in HASMCs and HUVECs
To examine the cytotoxicity of CAL in HASMCs and HUVECs, we performed the XTT assay. HASMC and HUVEC cells were treated with CAL (0.4, 0.6, 1 or 2 mM) for 24 h and the cell viability was evaluated. As shown in Figure 2, CAL did not produce any significant cytotoxicity in the cells and this concentration range was appropriate for subsequent experiments.
Effects of CAL on the cell viability of HASMCs and HUVECs. Cells were treated with CAL (0.4, 0.6, 1, and 2 mM) for 24 h. Cell survival rate was determined by the XTT assay. Changes in survival are represented as percentages of normal control. Bars represent the mean ± S.D. from at least three independent experiments.
Endothelium-dependent vasodilation with CAL
To demonstrate the endothelium dependency of the vasodilatory efficacy of CAL, we measured the changes of the tension in endothelium-intact and -denuded aortas following cumulative treatment with CAL. Each group was treated with 0.2 mM, 0.4 mM, 0.6 mM, 1 mM or 1.5 mM CAL. The vasodilatory effect of CAL increased in a concentration-dependent manner. However, in endothelium-denuded aortas, the overall effect of CAL was decreased significantly to 3.1 ± 5.4% from 18.6 ± 7.8% at 0.2 mM, to 7.3 ± 6.2% from 31.8 ± 6.8% at 0.4 mM, to 9.2 ± 8.5% from 45.8 ± 6.8% at 0.6 mM, to 15.2 ± 6.4% from 63.2 ± 4.1% at 1 mM and to 17.3 ± 8.8% from 82.4 ± 4.2 at 1.5 mM (Figure 3A). Pre-incubation of endothelium-intact strips with the NOS inhibitor L-NAME significantly reduced the CAL-induced relaxation, with a maximal relaxant effect of 17.8 ± 9.2% at 1.5 mM CAL compared with control (85.8 ± 6.2%; Figure 3B).
Endothelium and NO dependency of vasodilatory effects of CAL on the PE-induced contraction of rat thoracic aorta. (A) Vasodilatory effect of CAL in the presence (○) and absence (■) of endothelium in rat aorta. (B) NO-dependent vasodilatory effect of CAL in response to pretreatment with NG-nitro-L-arginine methyl ester (L-NAME; 10-4 M; ■). (C) sGC-dependent vasodilatory effect of CAL in response to pretreatment with methylene blue (MB; 10-5 M; ■) and 1 H-[1,2,4]-oxadiazolole-[4,3-a] quinoxalin-10-one (ODQ; 10-6 M; □). (D) pGC-dependent vasodilatory effect of CAL in response to pretreatment with atrial natriuretic peptide (ANP; 10-8 and 10-9 M). Relaxation values are indicated as the percentage of decrease in maximal tension in response to PE. Each marker represents the mean ± S.D. from at least three independent experiments. *P < 0.01, **P < 0.001 compared with Control.
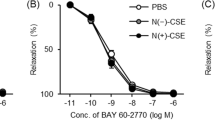
To more accurately investigate the relationship between CAL treatment and GC activation, we measured the changes in tension in aorta pretreated with sGC inhibitors MB, ODQ or the particulate guanylyl cyclase (pGC) activator ANP following cumulative treatment with CAL. In aorta pretreated with 10-5 M MB or 10-6 M ODQ, the overall effect of CAL was significantly decreased to 0% and 0% from 3.2 ± 5.4% at 0.2 mM, to 5.6 ± 4.0% and 2.2 ± 3.2% from 13.8 ± 5.8% at 0.4 mM, to 6.4 ± 4.2% and 6.2 ± 5.6% from 28.1 ± 10.2% at 0.6 mM, to 11.2 ± 3.6% and 11.2 ± 7.6% from 45.2 ± 9.8% at 1 mM, and to 12.7 ± 5.8% and 19.2 ± 3.2% from 66.4 ± 6.1 at 1.5 mM (Figure 3C); 10-8 and 10-9 M ANP did not affect the vasodilatory effect of CAL (Figure 3D).
Effects of CAL on eNOS expression and NO generation
To study the effects of CAL on NO generation in the aorta, the phosphorylated eNOS and nitrite levels were measured. In endothelial cells, the increase of NO by eNOS activation is considered the most important factor for remedy of vascular dysfunction such as atherosclerosis and hypertension (Chatterjee et al., 2008). Therefore, we measured the levels of phosphorylated eNOS (p-eNOS) at Ser1177 in CAL-treated aortas. Ach or CAL treatment increased the p-eNOS in the presence of PE, and the increased p-eNOS was reduced by addition of L-NAME with CAL, while total eNOS expression was not altered in any group (Figure 4A).
Effect of CAL on NO synthesis in HUVECs. (A) Western blots for Ser1177-phosphorylated eNOS (p-eNOS) or total eNOS in whole cell extracts. Typical blots are shown above the expression bar chart. (B) The concentration of NO was assessed by measurement of nitrite. Data are shown as mean ± S.D. of three independent experiments. *P < 0.05 compared with normal.
Measurement of NO concentration is difficult because of the short half-life of gaseous NO. The assay kit indirectly and accurately detects the level of NO by measuring nitrite, which is a precursor of NO in living tissue (Zweier et al., 2010). Nitrite concentration in CAL-treated aortas increased to 10.2 ± 0.5 µM at 0.4 mM CAL and 10.7 ± 0.5 µM at 0.6 mM CAL compared with normal (8.2 ± 0.5 µM) (Figure 4B). The positive control Ach increased nitrite concentration to 11.2 ± 0.3 µM.
Effect of CAL on cGMP production
To determine whether CAL treatment induces cGMP production in aortic strips, the accumulation of cGMP was measured. Incubation of aorta strips with CAL significantly increased the accumulation of cGMP in a dose-dependent manner compared with the PE group. Ach and L-NAME were used as positive and negative controls. CAL-induced cGMP was inhibited by L-NAME addition. As shown in Figure 5, each group produced cGMP: PE, 1.1 ± 0.82 pmol/g; Ach, 4.76 ± 0.69 pmol/g; 0.4 mM CAL, 3.27 ± 0.79 pmol/g; 0.6 mM CAL, 4.36 ± 1.18 pmol/g; L-NAME, 0.72 ± 0.68 pmol/g; L-NAME + 0.6 mM CAL, 0.43 ± 0.20 pmol/g.
Effect of CAL on PKG1 levels
cGMP is involved in the relaxation of vascular smooth muscle via PKG (Surks, 2007). Therefore, we measured the PKG1 levels to determine whether the production of cGMP by CAL is related to PKG1 expression. Similar to Ach, 0.6 mM CAL increased the PKG1 level, but the increase in PKG1 levels was inhibited by L-NAME pretreatment (Figure 6A).
Effect of CAL on the activation of PKG in rat aorta. (A) Western blots for PKG1 in whole aortic ring extracts. Total protein was normalized to actin. Typical blots are shown above the expression bar chart. (B) Effect of CAL on calpeptin-induced vasoconstriction. (C) Effects of CAL on K+ channel inhibitor (Gli, 4-AP, TEA) treatments in PE-precontracted rat aorta. Data represents the mean ± S.D. from at least three independent experiments. Ach and Y-27632 are used as positive control and L-NAME is used as negative control. *P < 0.05, **P < 0.001 compared with PE or calpeptin; #P < 0.001 compared with 0.6 mM CAL. Gli, glibenclamide (10-5 M); 4-AP, 4-aminopyridine (2 × 10-4 M); TEA, tetraethylammonium (10-3 M).
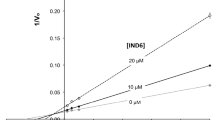
PKG induces vasodilation by inhibiting Ca2+ sensitization and/or activation of K+ channels (Surks, 2007; Prieto, 2008; Chai et al., 2011). To determine the downstream pathway of PKG-dependent vasodilation by CAL, we measured the tension in the presence of Rho-kinase activator or K+ channel inhibitors. Vascular tension induced by the Rho-kinase activator calpeptin (0.5 g) was significantly reduced by 0.6 mM CAL (0.24 ± 0.16 g) or Rho-kinase inhibitor Y-27632 (0.08 ± 0.36 g) (Figure 6B). On the other hand, pretreatment with Gli (10-5 M) and 4-AP (2 × 10-4 M) reduced the vasodilatory effect of 0.6 mM CAL to 22 ± 5.44% and 23 ± 4.86% from 53 ± 2.24%; however, TEA (10-3 M) had no effect (Figure 6C).
Discussion
The twig of Cinnamomum cassia is known as Cinnamomi ramulus (CR) and has traditionally been used to improve blood circulation in vascular disease. CR contains cinnamaldehyde, cinnamic acid and cinnamyl alcohol (CAL) as the main ingredients (He et al., 2005). Recently, we elucidated that CR relaxes vascular contraction through the inhibition of voltage-dependent Ca2+ channels and the downregulation of the Rho-kinase pathway (Kim and Shin, 2010; Kang and Shin, 2011). However, the possible vasodilatory efficacy of the ingredients remains to be examined.
The present study investigated the endothelium-dependent vasorelaxation of CAL in an organ bath system. The detailed mechanisms were further explored by measurement of NO level and by verification of the NO-related signal pathway.
Vascular tension plays an important role in blood pressure control. High blood pressure has been suggested to involve the abnormal reduction of endothelium-dependent vasodilators such as NO and prostacyclin in the vascular tissue. Therefore, the release of endothelium-derived relaxing factor NO is important for controlling blood pressure.
The antipyretic effect and low toxicity of CAL is well known (Guo et al., 2006), and the present study revealed no cytotoxic effects in the XTT cell viability assay of HASMCs and HUVECs at concentrations of 0.4-2 mM CAL. The vasodilatory effect of CAL is dependent on endothelium because NOS inhibitor L-NAME and sGC inhibitors MB or ODQ reduced the endothelium-dependent vasorelaxation by CAL. NO is a biological mediator of vascular relaxation and is produced by NOS. Among the NOS, the regulation of eNOS activity is important for vascular relaxation, which results in a decrease of high blood pressure (Ignarro et al., 1987, 1999; Prieto, 2008). CAL induces NO generation by phosphorylation of eNOS (p-eNOS) at Ser1177 in HUVECs. The p-eNOS level with 0.6 mM CAL treatment was similar to that with Ach and was inhibited with L-NAME (10-4 M). These results were consistent with the nitrite production, a precursor of NO, following CAL treatment, explaining NO production by eNOS activation.
NO interacts with sGC and then converts GTP to the second messenger cGMP, resulting in blood vessel dilation (Lucas et al., 2000; Priviero and Webb, 2010). Therefore, sGC activation is important for regulation of blood pressure through cGMP. In the present study, sGC inhibitors MB or ODQ significantly decreased the vasodilatory efficacy of CAL, but the particulate guanylyl cyclase (pGC) activator ANP did not affect vasodilation by CAL. These results suggest that CAL elevates cGMP levels via activation of sGC. In addition, 0.6 mM CAL significantly increased cGMP production to a level similar to that induced by Ach. The increase of cGMP level was inhibited by L-NAME, suggesting the involvement of cGMP in the vasorelaxation mechanism of CAL.
Induction of cGMP by sGC increases the PKG level, and cGMP binds to PKG through a conformational change (Chu et al., 1997; Word and Cornwell, 1998; Browner et al., 2004). Activation of PKG by cGMP stimulates vasodilation by decreasing intracellular cytosolic Ca2+ concentration through the activation of K+ channels and decreasing Ca2+ sensitization by activation of MLC phosphatase via inhibition of the RhoA/Rho-kinase pathway (Surks et al., 1999; Schlossmann et al., 2000; Lincoln et al., 2001; Lee et al., 2004; Chai et al., 2011).
As mentioned above, PKG exerts its vasodilatory activity through a variety of pathways in the regulation of vascular tone. Similar to Ach, CAL upregulates the expression of PKG1. However, this increase was reduced by L-NAME treatment. Furthermore, the vasodilatory effect of CAL was decreased by treatment with the ATP-sensitive K+ channel inhibitor Gli and the voltage-dependent K+ channel inhibitor 4-AP, but the Ca2+-activated K+ channel inhibitor TEA had no effect. In addition, CAL significantly relaxed the vasoconstriction induced by the Rho-kinase activator calpeptin, suggesting a reduction of Ca2+ sensitization via Rho-kinase.
Taken together, these results suggest that the endothelium-dependent vasodilation by CAL is closely related to the activation of K+ channels and to the inhibition of Rho-kinase, which reduce intracellular cytosolic Ca2+ levels and inhibit Ca2+ sensitization via the NO-cGMP-PKG pathway in rat thoracic aorta.
Methods
Materials
Male Sprague-Dawley rats, weighing 320 to 350 g, were purchased from SAMTAKO (Osan-si, Korea) for preparation of thoracic aortic strips.
First, antibodies against phosphorylated eNOS (p-eNOS), eNOS, PKG1, β-actin, and anti-rabbit or -goat secondary antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Cinnamyl alcohol (CAL), phenylephrine (PE), acetylcholine, 1 H-[1,2,4]-oxadiazolole-[4,3-a] quinoxalin-10one (ODQ) and atrial natriuretic peptide (ANP) were purchased from Sigma-Aldrich (St. Louis, MO). NG-nitro-L-arginine methyl ester (L-NAME), methylene blue (MB), glibenclamide (Gli) and calpeptin were purchased from Calbiochem (San Diego, CA). Each drug was prepared in dimethyl sulfoxide. All drugs were diluted in Krebs solution (NaCl, 115 mM; KCl, 4.7 mM; CaCl2, 2.5 mM; MgCl2, 1.2 mM; NaHCO3, 25 mM; KH2PO4, 1.2 mM; and dextrose, 10 mM) in an organ bath.
XTT Cell Proliferation, cGMP direct immunoassay, and NO detection kits were purchased from Roche Applied Science (Mannheim, Germany), Abcam (Cambridge, UK), and iNtRON Biotechnology (Seongnam-si, Korea), respectively.
Cell culture
HASMCs were maintained in smooth muscle cell medium SmGM-2 (Lonza, Walkersville, MD) with supplements provided by the supplier. HUVECs were cultured in EGM-2 Bulletkit (Lonza, Walkersville, MD) under standard culture conditions (37℃, 95% humidified air and 5% CO2). Cells in the 9th-12th passage were used in all experiments. The medium was changed every two days, and HASMCs and HUVECs were grown to 80-90% confluence and made quiescent by starvation for at least 24 h prior to the experiments.
Proliferation assay
Cell proliferation was assessed using a colorimetric assay system (XTT Cell Proliferation Kit). HASMCs and HUVECs (2 × 104 cells/well) were plated in each well of 96-well plates and incubated at 37℃ in a humidified atmosphere of 5% CO2, 95% air for 24 h. The attached cells were treated with 0.4, 0.6, 1, or 2 mM CAL for 24 h. Fifty microliters of XTT solution was added to each well. After incubation for 4 h, the colorimetric absorbance was measured at 450 nm (reference wavelength at 670 nm) using a microplate reader (Molecular Devices, Sunnyvale, CA). Cell proliferation was expressed as a percentage of normal controls.
Organ bath study
The investigations were performed according to protocols approved by the Institutional Animal Care and Use Committee of Dongguk University. Sprague-Dawley rats were provided with food and water ad libitum and allowed to adapt to the experimental conditions (temperature, 21 ± 2℃; humidity, 50-60%) for 1 week.
Tension was measured by a modification of a previously described procedure (Jeon et al., 2006). Briefly, animals were anesthetized by inhalation of evaporated ether in the desiccators. The thoracic aorta was immediately excised and immersed in ice-cold Krebs solution. The aorta was cleaned of all adherent connective tissue with wet filter paper and cut into six ring segments (3 mm in length). Two stainless-steel triangles were inserted through each vessel strip. One triangle was anchored to a stationary support, and the other was connected to a FT03 isometric force transducer (Grass, Quincy, MA). Each vessel strip was equilibrated in a water-jacketed organ bath (10 ml) for at least 50 min; the Krebs solution in the bath was maintained at 37℃ and aerated with a mixture of 95% O2 and 5% CO2. Each strip was stretched passively by imposing an optimal resting tension of approximately 2.0 g, which was maintained throughout the experiment. Isometric tension was recorded using a PowerLab/8SP computerized data acquisition system (ADInstruments, Castle Hill, NSW, Australia).
To study the endothelium dependency, the integrity of aortic strips with and without endothelium was checked by addition of 1 µM Ach to strip contracted by 1 µM PE treatment. After washing, aortic strips with and without endothelium were re-contracted by PE treatment. When the contraction reached a plateau, CAL was added to the bath cumulatively. To study the endothelium-dependent relaxation through the NO-cGMP pathway, aortic strips with endothelium were pretreated with L-NAME (10-4 M), ODQ (10-6 M), ANP (10-8 or 10-9 M) or MB (10-5 M) for 30 min and then contracted by treatment with PE. When the contraction reached a plateau, CAL was added to the bath by the same schedule described above.
To study the PKG-dependent relaxation mechanism of CAL, the tension change was measured in the presence of the Rho-kinase activator calpeptin (100 µg/ml), the ATP-sensitive K+ channel inhibitor glibenclamide (Gli, 10-5 M), the voltage-dependent K+ channel inhibitor 4-aminopyridine (4-AP, 2 × 10-4 M) or the Ca2+-activated K+ channel inhibitor tetraethylammonium (TEA, 10-3 M). When the contraction reached a plateau by calpeptin treatment, CAL was added to the bath cumulatively. To K+ channel inhibition, PE-contracted rat aortic strips were pretreated with Gli, 4-AP or TEA.
Preparation of protein extracts and western blot analysis
HUVECs were treated with 1 µM Ach, 0.4, 1 mM CAL, and 1 mM CAL+L-NAME for 4 h. Total protein extracts were harvested using cell lysis buffer containing a protease inhibitor cocktail (Roche Diagnostics, Indianapolis, IN). Aortic strips were contracted with PE (1 µM) followed by the addition of 1 µM Ach, 1 mM CAL, L-NAME, or 1 mM CAL + L-NAME for 30 min. The aortic strips were quick-frozen by immersion in liquid nitrogen. The frozen strip samples were homogenized in buffer containing 320 mM sucrose, 50 mM Tris, 1 mM EDTA, 1% Triton X-100, 1 mM dithiothreitol, and the following protease inhibitors: leupeptin (10 µg/ml), trypsin (10 µg/ml), aprotinin (2 µg/ml), or phenylmethylsulfonyl fluoride (100 µg/ml).
The amount of protein was measured using Bradford protein assay reagent (Bio-Rad Laboratories, Hercules, CA). Equal amounts of proteins were electrophoresed and the resolved proteins were transferred to PVDF membranes. The bands containing p-eNOS, eNOS, PKG1, or β-actin were detected by enhanced chemiluminescence visualized on film (Amersham Biosciences, Buckinghamshire, UK).
NO and cGMP analysis
The NO levels in HUVECs were measured with a NO detection kit (iNtRON Biotechnology, Seongnam-si, Korea) at 540 nm according to the manufacturer's instructions.
The cGMP levels in aortic strips were measured with cGMP direct immunoassay kit (Abcam, Cambridge, UK). Each frozen tissue was weighed and five volumes of 0.1 M HCl were added. The sample was homogenized on ice using a homogenizer, the tissue extract was centrifuged at 12,000 × g for 5 min, and the supernatant was collected. The supernatant was assayed directly at 450 nm according to the manufacturer's instructions.
Statistical analysis
All data points are represented as mean ± S.D. of experiments conducted at least in triplicate. Differences between treatment groups were examined using a paired Student's t-test. P < 0.05 was considered significant.
Abbreviations
- CAL:
-
cinnamyl alcohol
References
Browner NC, Dey NB, Bloch KD, Lincoln TM . Regulation of cGMP-dependent protein kinase expression by soluble guanylyl cyclase in vascular smooth muscle cells . J Biol Chem 2004 ; 279 : 46631 - 46636
Chai Y, Lin YF . Dual regulation of the ATP-sensitive potassium channel by activation of cGMP-dependent protein kinase . Pflugers Arch 2008 ; 456 : 897 - 915
Chai Y, Zhang DM, Lin YF . Activation of cGMP-dependent protein kinase stimulates cardiac ATP-sensitive potassium channels via a ROS/calmodulin/CaMKII signaling cascade . PLoS One 2011 ; 6 : e18191
Chatterjee A, Black SM, Catravas JD . Endothelial nitric oxide (NO) and its pathophysiologic regulation . Vascul Pharmacol 2008 ; 49 : 134 - 140
Chu DM, Corbin JD, Grimes KA, Francis SH . Activation by cyclic GMP binding causes an apparent conformational change in cGMP-dependent protein kinase . J Biol Chem 1997 ; 272 : 31922 - 31928
Félétou M, Köhler R, Vanhoutte PM . Endothelium-derived vasoactive factors and hypertension: possible roles in pathogenesis and as treatment targets . Curr Hypertens Rep 2010 ; 12 : 267 - 275
Gong F, Liang YZ, Fung YS . Analysis of volatile components from Cortex cinnamomi with hyphenated chromatography and chemometric resolution . J Pharm Biomed Anal 2004 ; 34 : 1029 - 1047
Guo JY, Huo HR, Zhao BS, Liu HB, Li LF, Guo SY, Jiang TL . Effect of 3-Phenyl-2-Propene-1-ol on PGE2 release from rat cerebral microvascular endothelial cells stimulated by IL-1beta . Am J Chin Med 2006 ; 34 : 685 - 693
He ZD, Qiao CF, Han QB, Cheng CL, Xu HX, Jiang RW, But PP, Shaw PC . Authentication and quantitative analysis on the chemical profile of cassia bark (cortex cinnamomi) by high-pressure liquid chromatography . J Agric Food Chem 2005 ; 53 : 2424 - 2428
Ibarra-Alvarado C, Rojas A, Luna F, Rojas JI, Rivero-Cruz B, Rivero-Cruz JF . Vasorelaxant constituents of the leaves of Prumus serotina "capulin" . Rev Latinoam Quim 2009 ; 37 : 164 - 173
Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G . Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide . Proc Natl Acad Sci USA 1987 ; 84 : 9265 - 9269
Ignarro LJ, Cirino G, Casini A, Napoli C . Nitric oxide as a signaling molecule in the vascular system: an overview . J Cardiovasc Pharmacol 1999 ; 34 : 879 - 886
Jeon SB, Jin F, Kim JI, Kim SH, Suk K, Chae SC, Jun JE, Park WH, Kim IK . A role for Rho kinase in vascular contraction evoked by sodium fluoride . Biochem Biophys Res Commun 2006 ; 343 : 27 - 33
Kang YH, Shin HM . Vasorelaxant effect of Cinnamomi ramulus ethanol extract via rho-kinase signaling pathway . Am J Chin Med 2011 ; 39 : 867 - 878
Kim JB, Shin HM . Vasodilation of ethanol extract of Cinnamomi Ramulus via voltage dependent Ca2+ channel blockage . Korean J Orient Physiol Pathol 2010 ; 24 : 592 - 597
Kitazawa T, Semba S, Huh YH, Kitazawa K, Eto M . Nitric oxide-induced biphasic mechanism of vascular relaxation via dephosphorylation of CPI-17 and MYPT1 . J Physiol 2009 ; 587 : 3587 - 3603
Kubo M, Nakaya Y, Matsuoka S, Saito K, Kuroda Y . Atrial natriuretic factor and isosorbide dinitrate modulate the gating of ATP-sensitive K+ channels in cultured vascular smooth muscle cells . Circ Res 1994 ; 74 : 471 - 476
Lee DL, Webb RC, Jin L . Hypertension and RhoA/Rho-kinase signaling in the vasculature: highlights from the recent literature . Hypertension 2004 ; 44 : 796 - 799
Letizia CS, Cocchiara J, Lalko J, Lapczynski A, Api AM . Fragrance material review on cinnamyl alcohol . Food Chem Toxicol 2005 ; 43 : 837 - 866
Lincoln TM, Dey N, Sellak H . Invited review: cGMP-dependent protein kinase signaling mechanisms in smooth muscle: from the regulation of tone to gene expression . J Appl Physiol 2001 ; 91 : 1421 - 1430
Lucas KA, Pitari GM, Kazerounian S, Ruiz-Stewart I, Park J, Schulz S, Chepenik KP, Waldman SA . Guanylyl cyclases and signaling by cyclic GMP . Pharmacol Rev 2000 ; 52 : 375 - 414
Nelson MT, Quayle JM . Physiological roles and properties of potassium channels in arterial smooth muscle . Am J Physiol 1995 ; 268 : C799 - C822
Ng LT, Wu SJ . Antiproliferative Activity of Cinnamomum cassia Constituents and Effects of Pifithrin-Alpha on Their Apoptotic Signaling Pathways in Hep G2 Cells . Evid Based Complement Alternat Med 2011 ; 2011 : 492148
Palmer RM, Ferrige AG, Moncada S . Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor . Nature 1987 ; 327 : 524 - 526
Prieto D . Physiological regulation of penile arteries and veins . Int J Impot Res 2008 ; 20 : 17 - 29
Priviero FB, Webb RC . Heme-dependent and independent soluble guanylate cyclase activators and vasodilation . J Cardiovasc Pharmacol 2010 ; 56 : 229 - 233
Qi H, Zheng X, Qin X, Dou D, Xu H, Raj JU, Gao Y . Protein kinase G regulates the basal tension and plays a major role in nitrovasodilator-induced relaxation of porcine coronary veins . Br J Pharmacol 2007 ; 152 : 1060 - 1069
Rich S . The effects of vasodilators in pulmonary hypertension: pulmonary vascular or peripheral vascular ? Circ Heart Fail 2009 ; 2 : 145 - 150
Schlossmann J, Ammendola A, Ashman K, Zong X, Huber A, Neubauer G, Wang GX, Allescher HD, Korth M, Wilm M, Hofmann F, Ruth P . Regulation of intracellular calcium by a signalling complex of IRAG, IP3 receptor and cGMP kinase Ibeta . Nature 2000 ; 404 : 197 - 201
Surks HK . cGMP-dependent protein kinase I and smooth muscle relaxation: a tale of two isoforms . Circ Res 2007 ; 101 : 1078 - 1080
Surks HK, Mochizuki N, Kasai Y, Georgescu SP, Tang KM, Ito M, Lincoln TM, Mendelsohn ME . Regulation of myosin phosphatase by a specific interaction with cGMP-dependent protein kinase Ialpha . Science 1999 ; 286 : 1583 - 1587
Vanhoutte PM, Scott-Burden T . The endothelium in health and disease . Tex Heart Inst J 1994 ; 21 : 62 - 67
Word RA, Cornwell TL . Regulation of cGMP-induced relaxation and cGMP-dependent protein kinase in rat myometrium during pregnancy . Am J Physiol 1998 ; 274 : C748 - C756
Zweier JL, Li H, Samouilov A, Liu X . Mechanisms of nitrite reduction to nitric oxide in the heart and vessel wall . Nitric Oxide 2010 ; 22 : 83 - 90
Acknowledgements
This work was supported by the Dongguk University Research Fund of 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
We have nothing to declare conflicts of interest.
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kang, Y., Yang, I., Morgan, K. et al. Cinnamyl alcohol attenuates vasoconstriction by activation of K+ channels via NO-cGMP-protein kinase G pathway and inhibition of Rho-kinase. Exp Mol Med 44, 749–755 (2012). https://doi.org/10.3858/emm.2012.44.12.083
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2012.44.12.083
Keywords
This article is cited by
-
Pharmacological Studies on Cinnamic Alcohol and Its Derivatives
Revista Brasileira de Farmacognosia (2021)