Abstract
Our previous report has demonstrated that 5-formylhonokiol (FH), a derivative of honokiol (HK), exerts more potent anti-proliferative activities than honokiol in several tumor cell lines. In present study, we first explored the antiangiogenic activities of 5-formylhonokiol on proliferation, migration and tube formation of human umbilical vein endothelial cells (HUVECs) for the first time in vitro. Then we investigated the in vivo antiangiogenic effect of 5-formylhonokiol on zebrafish angiogenesis model. In order to clarify the underlying molecular mechanism of 5-formylhonokiol, we investigated the signaling pathway involved in controlling the angiogenesis process by western blotting assay. Wound-healing results showed that 5-formylhonokiol significantly and dose-dependently inhibited migration of cultured human umbilical vein enthothelial cells. The invasiveness of HUVEC cells was also effectively suppressed at a low concentration of 5-formylhonokiol in the transwell assay. Further F-actin imaging revealed that inhibitory effect of 5-formylhonokiol on invasion may partly contribute to the disruption of assembling stress fiber. Tube formation assay, which is associated with endothelial cells migration, further confirmed the anti-angiogenesis effect of 5-formylhonokiol. In in vivo zebrafish angiogenesis model, we found that 5-formylhonokiol dose-dependently inhibited angiogenesis. Furthermore, western blotting showed that 5-formylhonokiol significantly down-regulated extracellular signal-regulated kinase (ERK) expression and inhibited the phosphorylation of ERK but not affecting the total protein kinase B (Akt) expression and related phosphorylation, suggesting that 5-formylhonokiol might exert anti-angiogenesis capacity via down-regulation of the ERK signal pathway. Taken together, these data suggested that 5-formylhonokiol might be a viable drug candidate in antiangiogenesis and anticancer therapies.
Similar content being viewed by others
Introduction
Angiogenesis plays an important role in tumor growth and metastasis (Folkman, 1974; Carmeliet, 2000; Dong et al., 2009). New blood vessels are considered to be essential for the delivery of nutrients and oxygen to the tumor microenvironment, especially when the tumor volunm is 1-2 mm in diameter (Xiao and Singh, 2008; Dong et al., 2009). Moreover, new blood vessels seem critical by providing route for metastasis, a complex phenomenon in which tumour cells invade surrounding tissues to form distant secondary tumors, and thus it is considered as the major cause of cancer mortality (Bergers and Benjamin, 2003; Cooney et al., 2006; Yi and Benjamin, 2008). These discoveries have led to the design of therapeutic strategies toward the tumor vasculature, aiming either to prevent the formation of new vessels (antiangiogenic) or to damage existing vessels (vascular targeting) (Taraboletti and Giavazzi, 2004). The antiangiogenic strategy has led to the development of compounds which is designed to control tumor growth by blocking its ability to develop a blood supply.
Endothelial cells play a major role in each step of tumorous angiogenesis, including endothelial cell proliferation, adhesion, migration, invasion, and tube formation (Jain, 2003; Coultas et al., 2005; Yi et al., 2008). Many proangiogenic growth factors regulate angiogenesis through PI3K/Akt and MKK/ERK signaling pathways (Kim et al., 2004; Lu et al., 2005; Perona, 2006). MKK/ERK signaling pathway has been shown to play a crucial role in tumorigenesis and tumor metastasis (Ward et al., 2001; Huang et al., 2008), and sustained activation of ERK has been established as a requirement for angiogenesis (Berra et al., 2000; Dong et al., 2001; Depeille et al., 2007). AKT is also an important factor in mediating vasodilation, vascular remodeling, and angiogenesis.
HK, an active component purified from Magnolia, has been reported to possess anti-angiogenesis potency (Bai et al., 2003; Ikeda et al., 2003). Our recent studies have indicated that HK induces apoptosis in tumor cells, inhibits angiogenesis and lymphatic metastasis (Wen et al., 2009). The multiple biological properties of HK encouraged further structure modification to increase the potencies of anti-tumor activity. In our previous study on structure-activity relationship, we found that FH, a novel derivative of HK, displayed more potent anti-proliferative potentials than HK (Luo et al., 2009). The aim of this paper was to clarify its inhibitory capacity of angiogenensis and the underlying mechanism.
Results
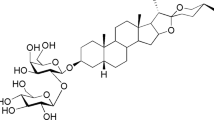
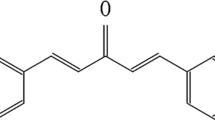
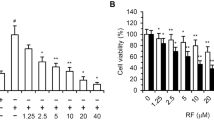
FH exerts higher inhibitory potency than HK on a proliferation MTT assay
In our previous study, a series of HK derivatives were first synthesized in our group for the screening of anti-proliferative assay by MTT (Luo et al., 2009). FH exerted more potent anti-proliferative activities than HK. As shown in Table 1, FH had 2-folds higher inhibitory potencies than HK both on LL-2 and A2780 tumor cell lines and a 1.5-folds on HepG-2. The IC50 values of HK and FH on HUVEC cells were 52.6 µM and 46.2 µM respectively. No significant cytotoxic effects were identified with respective 10, 20 and 40 µM (cell viability>60%) of the two compounds for 24 h, suggesting that all the experiments were done at non-toxic concentrations. Figure 1C indicated that FH inhibited HUVEC proliferation also in a time-dependent manner. A 40 µM FH resulted in an inhibition of 53.8% in 24 h treatment and 71% in 72 h treatment.
(A) Structure of HK. (B) Structure of FH. (C)HUVEC cells were treated with 40 µM for 24, 48 and 72 h, respectively. (D) HUVEC cells were scratched with a pipette tip and then treated with FH (10 µM, 20 µM, 40 µM), HK (10 µM, 20 µM, 40 µM) or medium alone (control) for 24 h. Migrating cells were photographed under a phase contrast micoscopy (100×). (E) Quantitation of HUVEC migration following 24 h of exposure to the indicated concentrations of FH and HK. Data represent the mean + standard error (SE) from three independent experiments. Bar, 50 µm; *P <0.05.
FH inhibits migration of HUVEC Cells via disrupting F-actin cytoskeleton organization
The migration of endothelial cells is a process of chemotaxis, which is an indispensable step in angiogenesis (Tong et al., 2006). We used wound-healing migration assay to assess the ability of FH to affect the migration of HUVECs and found that FH inhibited HUVEC migration in a concentration-dependent manner (Figure 1D). As shown in Figure 1E, FH exerted a more significant inhibition than HK when both agents were at the same concentrations, suggesting that FH effectively prevented the migration of HUVECs.
Tumor cell invasion to the extracellular matrix is an important event in the process of tumor metastasis. We proceeded to determine the effects of FH on the invasion of HUVECs using a modified Boyden chamber assay. Results were shown in Figure 2. In control group, a large number of cells migrated to the bottom layer of the membrane in the Boyden chamber, and FH significantly reduced the number of invading cells both at 10 µM and 20 µM concentrations compared to HK (Figure 2B).
Effect of FH on HUVEC invasion assay using Transwell. (A) Red cells stained with H&E were invaded cells attached on the outside surface of the top chamber following 24 h treatment with the indicated concentrations of FH or HK. (B) Data were obtained from five randomly chosen fields and were normalized to the control group for each time interval; bars, SE; Bar, 100 µm; *P <0.05.
Dynamic regulation of the filamentous actin (F-actin) cytoskeleton plays an important role in cell migration (Vicker, 2000; Chiou and Don, 2007; Tak et al., 2007). In order to further confirm the antimigrating activity of FH, fluorescence staining was used to visualize the changes in F-actin fiber organization of HUVEC cells. Compared to the controls (Figure 3), actin cytoskeleton organization was greatly disturbanced when treated by FH at 20 µM for 24 h. These results additionally confirmed that FH can effectively inhibit the HUVECs migration.
Effect of FH on the HUVEC cytoskeleton. HUVECs were seeded onto sterile cover slips in 6-well plates at a concentration of 5×104 cells/ml. The cells were allowed to adhere overnight before treatment for 24 h with or without 20 µM of FH. Cells were fixed and stained for F-actin (green, FITC-conjugated phalloidin, Sigma) and nuclei (blue, hoechst33258, Sigma).
FH disrupts tube formation
We evaluated the effects of FH on the formation of capillary-like tube structures by plating HUVECs on matrigel. The compound treatment caused the disruption of the capillary-like tube network in a concentration-dependent manner (Figure 4). The number of endotubes was substantially reduced after treated by 20 µM of FH (Figure 4D) and the tubes were completely destroyed at the concentration of 40 µM of FH (Figure 4F). The comparison between FH and HK is showed in Figure 4H. Our observation suggested that FH can effectively reduce the ability of HUVEC cells to form stable capillary-like network structures in vitro.
Inhibitory effect of FH on HUVEC tube-like structure formation. (A-G) Formation of capillary-like tube structures by HUVEC following 6 h of treatment with medium alone (A) or with 10 µM, 20 µM, 40 µM of FH (B-F) and HK (C-G). (H) Average number of tubes per microscopic field from three separate experiments. And the tubes were completely destroyed either at the concentration of 40 µM of FH or HK. Data were normalized to the control group for each time interval; bars, SE; *P <0.05.
FH reduces neovascularization of the zebrafish
Recently, the zebrafish has been proved to be an in vivo model for investigating the process of new blood vessel formation (Chan et al., 2002; Cross et al., 2003; Taraboletti and Giavazzi, 2004). Using this model, we examined the antiangiogenic activity of FH in vivo. As seen from the Figure 5, the newly-grown segmental vessels from the dorsal aorta of the control groups are perfect (the control group). Segmental vessel sprouts were not discernibly affected at a concentration of 10 µM of FH. In contrast, when the concentration was increased to 40 µM, FH showed a strong inhibition by occuring a few blood sprouts. The results illustrated that FH significantly inhibited angiogenesis on a zebrafish embryo assay.
Effect of FH on Neovascularization of the zebrafish. Zebrafish embryos were treated with embryo water alone (control), FH (10 µM, 20 µM, 40 µM) or HK (40 µM) which were added into embryo water. After incubation at 28.5℃ for 24 h, embryos were were anesthetized using 0.05% 2-phenoxyethanol in embryo water and photographed.
FH inhibited phosphorylation of ERK in HUVEC cells in vitro
Since FH demonstrated to have inhibitory effects on angiogenesis, the effects of the compound on the activation of ERK and AKT were investigated by western blots to further clarify the molecular mechanisms. As shown in Figure 6, western blotting revealed that ERK expression was sharply down-regulated with FH treatment, but AKT expression seemed unchanged, illustrating that FH-mediated HUVEC cell migration, invasion, proliferation and tube formation inhibition are mainly contributed to the suppression of ERK signaling pathway activation. The column is the ratio of gray intensity analysis of t-ERK1/2 and p-ERK1/2 protein bonds.
Effects of FH on ERK and AKT signaling pathways. HUVEC cells were cultured with FH (0, 10, 20, 40 µM) for 24 h, and whole cell lysates were subjected to SDS-PAGE followed by western blots with Antip44/42 MAPK, anti-Phospho-p44/42 MAPK, anti-AKT, anti-Phospho-AKT antibodies. The blots were stripped and reprobed with anti-β-actin antibody to ensure equal protein loading. Gray intensity analysis to the t-ERK1/2 and p-ERK1/2 protein bonds are also showed.
Discussion
Angiogenesis is the formation of new blood vessels from the endothelium of the existing vasculature, and inhibition of angiogenesis is associated with a significant delay of tumor growth (Tong et al., 2006). Based on our present results, we conclude that FH effectively inhibits endothelial cell proliferation, migration, invasion and tube formation, as well as prevents angiogenesis in vitro. In this study, the zebrafish models which were used for studying inhibitors of angiogenesis commonly, had several advantages that will make it a very potential method in vascular development assays. for example, the embryos are transparent, the vascular development is very rapid and large numbers of embryos can be easily manipulated. The observation that FH inhibited the newly formed blood vessel numbers of the zebrafish gave us a direct view of its anti-angiogenesis capacity. We also further confirmed the inhibitory impact on cell migration using F-actin cytoskelon assay for the first time. Cell migration is a multi-step cellular process initiated by forming protrusive structures like filopodia, lamellipodia via a combination of actin polymerization and depolymerization, and formation of these structures is driven by the control of F-actin polymerization (Kedrin et al., 2007). Thus, the changes in F-actin polymerization contribute to the process of cell migration (Huang et al., 2002; Wang et al., 2005).
To determine the mechanisms of activity of FH, we examined its effect on expression and phosphorylation of key signal transduction pathways. ERK and AKT pathways are the two major ones among the endothelial cell signaling pathways that regulates endothelial cell growth, migration, proliferation, and survival and it is necessary for essential cellular procedures of endothelial cells and angiogenesis after activation (Murphy et al., 2006; Huang et al., 2008). On the basis of present results, we suggest that anti-angiogenensis activity of FH is in great part due to the inhibition of ERK expression.
In conclusion, we systematically demonstrated that FH could effectively inhibit endothelial cell migration, invasion, proliferation, and tube formation in a dose-dependent manner in vitro and in vivo. Besides, we identified that FH mainly inhibited angiogenesis by suppressing the activation of ERK signaling pathway.
Together, these data suggested that FH appeared more effective compared with HK on angiogenesis and might play an important role in metastasis.
Methods
Cell culture and reagents
Human umbilical vein endothelial cells (HUVECs) were isolated from human umbilical cord with collagenase. After dissociation, the cells were collected and cultured on gelatin-coated culture flasks in M199 medium with 20% FBS, 10 ng/ml bFGF, 2 ng/ml VEGF, 100 IU/ml penicillin and 100 µg/ml streptomycin. Subcultures were performed with trypsin-EDTA. Media were refreshed every two days. The identity of umbilical vein endothelial cells was confirmed by their cobblestone morphology and strong positive immunoreactivity to von Willebrand factor. All cells were incubated in an atmosphere containing 5% CO2 at 37℃.
Anti-p44/42 MAP Kinase (ERK) monoclonal rabbit antibody, anti-Phospho-p44/42 MAP Kinase (p-ERK) monoclonal rabbit antibody, anti-AKT monoclonal rabbit antibody and anti-Phospho-AKT monoclonal mouse antibody were purchased from Cell Signaling Laboratories (Beverly, MA). Anti-β-actin monoclonal mouse antibody, goat anti-rabbit IgG/HRP and goat anti-mouse IgG/HRP were purchased from Santa Cruz Biotechnology (Santa Cruz, CA).
Matrigel was ordered from BD Biosciences. Transwell inserts for 24-well plates were obtained from Costar (Cambridge, MA).
FH and HK were synthesized by our own laboratory, and the purities were 99.8% determined by high-performance liquid chromatography.
Cellular proliferation assay
MTT assay was performed to evaluate the drug cytotoxicity. Cells were treated with various concentrations of the compound in 96-well culture plates for 24 h or longer times in final volumes of 200 µl (5×103 cells/well). Then 20 µl of MTT (5 mg/ml in normal sodium) was added to each well, and cells were incubated for an additional 3 h. Then the medium was carefully removed and precipitates were dissolved in 150 µl of DMSO, shaken mechanically for 10 min and then absorbance readings at a wavelength of 570 nm were taken on a spectrophotometer (Molecular Devices, Sunnyvale, CA). IC50 values were calculated using percentage of growth versus untreated control.
Wound-healing assays
HUVEC cells were seeded in 6-well plates precoated with 0.1% gelatin and grown overnight to confluence. The monolayer cells were wounded by scratching with 200 µl pipette tips and washed twice with serum-free DMEM to remove the nonadherent cells and then replaced by serum-free DMEM with the indicated concentrations of compounds for 24 h. Images were taken at 0 h and at 24 h independently after incubation at 37℃, 5% CO2. The migrated HUVEC cells were manually counted. The values were observed from three randomly selected fields. Similar patterns of the inhibition effects were observed in three independent experiments.
Cell invasion assays
Experiments assessing cell invasion ability were performed using a transwell chamber containing a polycarbonate filter with a pore size of 8 µm as described (Huang et al., 2002). At the top chambers, HUVEC Cells were counted and resuspended in serum-free DMEM containing 0.1% BSA at a final concentration of 5×104 cells/100 µl. The bottom chambers (600 µl) were filled with DMEM with 10% fetal bovine serum. The top and bottom chambers contained the same series of concentrations of the compound and were allowed to migrate for 24 h at 37℃, 5% CO2.
After incubation, the noninvasive cells that remained on the upper surface of the filter were removed by a cotton swab. Cells that traversed through the Matrigel and the polycarbonate filter were attached to the lower surface of the filter, and were fixed with 4% paraformaldehyde for 20 min and washed three times with 1×PBS. The cells were stained by H&E and then destained with 1×PBS. The number of invasive cells was additionally quantified by counting 3 random fields under the microscope.
F-actin fluorescence stain to assay cytoskeleton distribution
Cells were planted onto sterile cover slips in 6-well plates at a concentration of 5×104 cells/ml. Following incubation with test reagents for 24 h, the culture medium was aspirated and cells were immediately fixed with 4% paraformaldehyde at room temperature for 20 min. Then samples were washed three times in PBS and incubated with FITC-conjugated phalloidin (Molecular Probes, Inc.) (200 ng/ml) in dark condition for 2 h. Cells were visualized under fluorescence microscopy (Olympus) and photographed.
Tube formation assays
The effects of FH treatments on in vitro angiogenesis were determined by tube formation assay. Matrigel was dissolved at 4℃ for overnight. Each well of prechilled 96-well plates was coated with 50 µl Matrigel and incubated to solidify at 37℃ for 45 min. After removing the unsolid fluid, about 4×104 HUVEC cells were seeded and cultured in DMEM containing various concentrations of drugs for 24 h. Images were digitally captured (Olympus) at 6 h after plating.
Zebrafish embryos assays
Using TG (fli-1:EGFP) zebrafish embryos where EGFP is expressed in all endothelial cells of the vasculature, we examined the effect of the compound on embryonic angiogenesis. Zebrafish embryos were generated by natural pair-wise mating and raised at 28.5℃ in embryo water (0.2 g/L of Instant Ocean Salt in distilled water). At about 6 h post-fertilization (hpf), the embryos were sorted in the 6-well plate (6 embryos/well), removing dead and unhealthy embryos. Then the embryos were treated with the indicated concentrations of the compound which were added into embryo water. After incubation for 24 h, the embryos were anesthetized using 0.05% 2-phenoxyethanol in embryo water and photographed.
Western blot analysis
HUVEC cells were lysed with protein lysis buffer [150 mM NaCl, 1.0% Nonidet P-40, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris-HCl (pH 8.0), 10 mM sodium fluoride, 1 mM sodium orthovanadate and 1 mM phenylmethylsulfonyl fluoride (PMSF), 1 mM cocktail]. Protein concentration was determined by the Bradford protein assay. The samples were denatured in sample buffer, and equal amounts of protein were separated according to molecular weight on 10% SDS-PAGE gel and transferred onto a polyvinylidene difluoride (PVDF) membrane. Membranes were blocked for 1 hour in 5% dried milk in TBST(TBS + 0.1% Tween 20) at room temperature and probed overnight at 4℃ with ERK1/2, protein kinase B (AKT) and β-actin antibody diluted in "blocking buffer". Blots were washed thrice for about 15 min with TBST and incubated with corresponding secondary antibodies diluted in blocking buffer that were conjugated with horseradish peroxidase for 1 h at a temperature of 37℃. After three additional washes, blots were developed by a 1-min incubation with enhanced chemiluminescent substrate and exposure to Kodak X-OMAT autoradiographic film (Kodak, Hemel Hempstead, United Kingdom).
Abbreviations
- FH:
-
5-formylhonokiol
- HK:
-
honokiol
- PI3K/Akt:
-
phosphoinositide 3-kinase/protein kinase B
References
Bai X, Cerimele F, Ushio-Fukai M, Waqas M, Campbell PM, Govindarajan B, Der CJ, Battle T, Frank DA, Ye K, Murad E, Dubiel W, Soff G, Arbiser JL . Honokiol, a small molecular weight natural product, inhibits angiogenesis in vitro and tumor growth in vivo . J Biol Chem 2003 ; 278 : 35501 - 35507
Bergers G, Benjamin LE . Tumorigenesis and the angiogenic switch . Nat Rev Cancer 2003 ; 3 : 401 - 410
Berra E, Milanini J, Richard DE, Gall ML, Vinals F, Gothie E, Roux D, Pades G, Pouyssegur J . Signaling angiogenesis via p42/p44 MAP kinase and hypoxia . Biochem Pharmacol 2000 ; 60 : 1171 - 1178
Carmeliet P . Angiogenesis in cancer and other diseases . Nature 2000 ; 407 : 249 - 257
Chan J, Bayliss PE, Wood JM, Robert TM . Dissection of angiogenic signaling in zebrafish using a chemical genetic approach . Cancer Cell 2002 ; 1 : 257 - 267
Chiou WF, Don MJ . Cryptotanshinone inhibits macrophage migration by impeding F-actin polymerization and filopodia extension . Life Sci 2007 ; 81 : 109 - 114
Cooney MM, Heeckeren WV, Bhakta S, Ortiz J, Remick SC . Drug insight: vascular disrupting agents and angiogenesis-novel approaches for drug delivery . Nat Clin Pract Oncol 2006 ; 3 : 682 - 692
Coultas L, Chawengsaksophak K, Rossant J . Endothelial cells and VEGF in vascular development . Nature 2005 ; 438 : 937 - 945
Cross LM, Cook MA, Lin S, Chen JN, Rubinstein AL . Rapid analysis of angiogenesis drugs in a live fluorescent zebrafish assay . Arterioscler Thromb Vasc Biol 2003 ; 23 : 911 - 912
Depeille P, Young JJ, Boguslawski EA, Berghuis BD, Kort EJ, Resau JH, Frankel AE, Duesbery NS . Anthrax lethal toxin inhibits growth of and vascular endothelial growth factor release from endothelial cells expressing the human herpes virus 8 viral g protein coupled receptor . Clin Cancer Res 2007 ; 13 : 5926 - 5934
Dong DF, Li EX, Wang JB, Wu YY, Shi F, Guo JJ, Wu Y, Liu JP, Liu SX, Yang GX . Anti-angiogenesis and anti-tumor effects of AdNT4-anginex . Cancer Lett 2009 ; 285 : 218 - 224
Dong G, Chen Z, Li ZY, Yeh NT, Bancroft CC, Waes CV . Hepatocyte growth factor/scatter factor-induced activation of MEK and PI3K signal pathways contributes to expression of proangiogenic cytokines interleukin-8 and vascular endothelial growth factor in head and neck squamous cell carcinoma . Cancer Res 2001 ; 61 : 5911 - 5918
Folkman J . Tumor angiogenesis factor . Cancer Res 1974 ; 34 : 2109 - 2113
Huang D, Ding Y, Luo WM, Bender S, Qian CN, Kort E, Zhang ZF, VandenBeldt K, Duesbery NS, Resau JH, Teh BT . Inhibition of MAPK kinase signaling pathways suppressed renal cell carcinoma growth and angiogenesis in vivo . Cancer Res 2008 ; 68 : 81 - 88
Huang SM, Li J, Harari PM . Molecular Inhibition of angiogenesis and metastatic potential in human squamous cell carcinomas after epidermal growth factor receptor blockade . Mol Cancer Ther 2002 ; 1 : 507 - 514
Ikeda K, Sakai Y, Nagase H . Inhibitory effect of magnolol on tumour metastasis in mice . Phytother Res 2003 ; 17 : 933 - 937
Jain RK . Molecular regulation of vessel maturation . Nat Med 2003 ; 9 : 685 - 693
Kedrin D, Rheenen JV, Hernandez L, Condeelis J, Segall JE . Cell motility and cytoskeletal regulation in invasion and metastasis . J Mammary Gland Biol Neoplasia 2007 ; 12 : 143 - 152
Kim DW, Lu B, Hallahan DE . Receptor tyrosine kinase inhibitors as anti-angiogenic agents . Curr Opin Investig Drugs 2004 ; 5 : 597 - 604
Lu B, Shinohara ET, Edwards E, Geng L, Tan J, Hallahan DE . The use of tyrosine kinase inhibitors in modifying the response of tumor microvasculature to radiotherapy . Technol Cancer Res Treat 2005 ; 4 : 691 - 698
Luo YF, Xu YB, Chen LJ, Hu J, Peng C, Xie DC, Shi JY, Huang WC, Xu GB, Peng M, Han J, Li R, Yang SY, Wei YQ . Semi-synthesis and anti-proliferative activity evaluation of novel analogues of honokiol . Bioorg Med Chem Lett 2009 ; 19 : 4702 - 4705
Murphy DA, Makonnen S, Lassoued W, Feldman MD, Carter C, Lee WM . Inhibition of tumor endothelial ERK activation, angiogenesis, and tumor growth by sorafenib (BAY43-9006) . Am J Pathol 2006 ; 169 : 1875 - 1885
Perona R . Cell signalling: growth factors and tyrosine kinase receptors . Clin Transl Oncol 2006 ; 8 : 77 - 82
Tak H, Jang E, Kim SB, Park J, Suk J, Yoon YS, Ahn JK, Lee JH, Joe CO . 14-3-3epsilon inhibits MK5-mediated cell migration by disrupting F-actin polymerization . Cell Signal 2007 ; 19 : 2379 - 2387
Taraboletti G, Giavazzi R . Modelling approaches for angiogenesis . Eur J Cancer 2004 ; 40 : 881 - 889
Tong YG, Zhang XW, Geng MY, Yue JM, Xin XL, Tian F, Shen X, Tong LJ, Li MH, Zhang C, Li WH, Lin LP, Ding J . Pseudolarix acid b, a new tubulin-binding agent, inhibits angiogenesis by interacting with a novel binding site on tubulin . Mol Pharmacol 2006 ; 69 : 1226 - 1233
Vicker MG . Reaction-diffusion waves of actin filament polymerization/depolymerization in dictyostelium pseudopodium extension and cell locomotion . Biophys Chem 2000 ; 84 : 87 - 98
Wang W, Zhang WL, Han Y, Chen JZ, Wang YB, Zhang Z, Hui RT . NELIN, a new F-actin associated protein, stimulates HeLa cell migration and adhesion . Biochem Biophys Res Commun 2005 ; 330 : 1127 - 1131
Ward Y, Wang W, Woodhouse E, Linnoila I, Liotta L, Kelly K . Signal pathways which promote invasion and metastasis: critical and distinct contributions of extracellular signal-regulated kinase and Ral-specific guanine exchange factor pathways . Mol Cell Biol 2001 ; 21 : 5958 - 5969
Wen J, Fu AF, Chen LJ, Xie XJ, Yang GL, Chen XC, Wang YS, Li J, Chen P, Tang MH, Shao XM, Lu Y, Zhao X, Wei YQ . Liposomal honokiol inhibits VEGF-D-induced lymphangiogenesis and metastasis in xenograft tumor model . Int J Cancer 2009 ; 124 : 2709 - 2718
Xiao D, Singh SV . z-Guggulsterone, a constituent of ayurvedic medicinal plant commiphora mukul, inhibits angiogenesis in vitro and in vivo . Mol Cancer Ther 2008 ; 7 : 171 - 180
Yi TF, Cho SG, Yi ZF, Pang XF, Rodriguez M, Wang Y, Sethi G, Aggarwal BB, Liu MY . Thymoquinone inhibits tumor angiogenesis and tumor growth through suppressing AKT and extracellular signal-regulated kinase signaling pathways . Mol Cancer Ther 2008 ; 7 : 1789 - 1796
Acknowledgements
The authors greatly appreciate financial support from National Natural Science Foundation of China (30772776) and National Key Technologies R&D Program of 11th five-year plan (2009ZX09501-015).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Zhu, W., Fu, A., Hu, J. et al. 5-Formylhonokiol exerts anti-angiogenesis activity via inactivating the ERK signaling pathway. Exp Mol Med 43, 146–152 (2011). https://doi.org/10.3858/emm.2011.43.3.017
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2011.43.3.017
Keywords
This article is cited by
-
Phyto-polyphenols as potential inhibitors of breast cancer metastasis
Molecular Medicine (2018)
-
Radiation-induced senescence in securin-deficient cancer cells promotes cell invasion involving the IL-6/STAT3 and PDGF-BB/PDGFR pathways
Scientific Reports (2013)
-
Honokiol activates AMP-activated protein kinase in breast cancer cells via an LKB1-dependent pathway and inhibits breast carcinogenesis
Breast Cancer Research (2012)