Abstract
Letter-writing is an integral practice for genetic health professionals. In Victoria, Australia, patients with a chromosomal variant of uncertain clinical significance (VUS) referred to a clinical geneticist (CG) for evaluation receive consultation summary letters. While communication of uncertainty has been explored in research to some extent, little has focused on how uncertainty is communicated within consultation letters. We aimed to develop a multi-layered understanding of the ways in which CGs communicate diagnostic uncertainty in consultation summary letters. We used theme-oriented discourse analysis of 49 consultation summary letters and thematic analysis of a focus group involving eight CGs. Results showed that CGs have become more confident in their description of VUS as ‘contributing factors’ to patients’ clinical features, but remain hesitant to assign definitive causality. CGs displayed strong epistemic stance when discussing future technological improvements to provide hope and minimise potentially disappointing outcomes for patients and families. CGs reported feeling overwhelmed by their workload associated with increasing numbers of patients with VUS, and this has led to a reduction in the number of review appointments offered over time. This study provides a rich description of the content and process of summary letters discussing VUS. Our findings have implications for letter-writing and workforce management. Furthermore, these findings may be of relevance to VUS identified by genomic sequencing in clinical practice.
Similar content being viewed by others
Introduction
Chromosomal microarray (CMA) is currently recommended as a first-tier diagnostic test for children with global developmental delay, intellectual disability and autism spectrum disorder.1 The higher resolution of CMA in detecting copy number variations (CNVs) has resulted in a 15-20% diagnostic yield compared to 3% with conventional karyotyping in this patient cohort.1 Additionally, CMA has resulted in a greater detection of chromosomal variants of uncertain clinical significance (VUS).2, 3 Although VUS are enriched in patient cohorts, they are also identified in apparently healthy control populations, and therefore their clinical significance is uncertain.
The Victorian Clinical Genetics Services (VCGS) in Melbourne, Australia began using CMAs diagnostically in 2009 and has reported approximately 37 000 CMA results, including approximately 1500 VUS at the time of this study. Two recurrent microdeletions consistently reported at the time by the VCGS laboratory as VUS involve chromosome regions 15q11.2 (containing the NIPA1 and NIPA2 genes) and 16p13.11 (containing the NDE1 gene). These microdeletions can be inherited or arise de novo. They are incompletely penetrant, and phenotypic expressivity is often highly variable even within families.4, 5
Patients in whom a VUS is detected by CMA are seen by a clinical geneticist (CG) for clinical evaluation and genetic counselling. As part of standard practice, patients (or their parents/caregivers) receive a summary letter following their consultation covering a range of information discussed in the consultation including test results, prognosis and plans for ongoing management. CGs often write a plain language summary letter directly to the patient/parents in addition to a more medically oriented letter to the referring doctor.
Receiving summary letters following medical consultations can: increase patient autonomy, and engagement in care; and improve patient compliance and satisfaction.6, 7 Parents of children with a genetic condition place great value in the summary letters received from their genetics specialist.8 However, some report that the language used between medical professionals is difficult to follow and that it is sometimes unclear what information was most relevant to them.7
There is currently limited research regarding how CGs approach genetic counselling of patients receiving CMA VUS results. The few studies conducted suggest that doctors may not be comfortable discussing VUS with their patients.9, 10, 11 Turbitt and colleagues9 reported that many Australian health professionals, both non-genetic and genetic specialists, became less confident about disclosing genetic test results as the clinical implications became less certain. This is consistent with findings from American health professionals where doctors reported feeling uncomfortable speaking to their patients about uncertain results.11
There has been no previous research investigating uncertainty within consultation summary letters written by CGs to patients. Additionally, there has been no research exploring how CGs experience writing letters in which a VUS has been identified. As we enter the era of large-scale genomic testing in clinical practice, understanding the different ways in which we communicate uncertainty is becoming increasingly important. This study aimed to develop a multi-layered understanding of the ways in which CGs communicate and experience diagnostic uncertainty in consultation summary letters. Specifically, we sought to investigate the content of letters discussing VUS; evaluate how CGs convey uncertainty in their letters; and understand why CGs choose the language used in their letters.
Methods
This study was an observational and exploratory study using qualitative approaches, based upon the theoretical framework of symbolic interactionism. This theory assumes that people act, or react, to an event according to the meaning they have for that event; that the meaning is based on their past experiences; and that meaning is negotiated through interactions with others.12 It included two parts; an analysis of consultation summary letters, and a focus group with CGs exploring their experiences of letter-writing. Ethical approval for this study was obtained through The Royal Children’s Hospital Human Research Ethics Committee (HREC number 34092A).
Letter analysis
We used purposive, criterion-based sampling13 to identify a selection of letters containing a discussion of uncertainty. As chromosome 15q11.2 and 16p13.11 microdeletions were consistently reported as VUS by VCGS Cytogenetics over the period 2009-2013, and occurred frequently enough to provide an adequate sample, we selected these as the focus of this study. All individuals with a 15q11.2 or 16p13.11 microdeletion reported from 2009 to 2013 inclusive were identified by database search. Only those letters pertaining to the proband, written by a VCGS CG, and addressing no other CNVs were included. Letters were de-identified with a code applied indicating the doctor who had written the letter, the letter number for that doctor, and the year in which the letter was written, for example, CG01_1_09. Identifying information within letters was removed, indicated by square brackets. Letters were imported into the QSR International software program NVivo1014 for management and storage of coding.
We used theme-oriented discourse analysis to analyse the letters.15 This involves a multi-step process of content, thematic and discourse analysis to achieve a ‘thick’ understanding of the text. Initially, each letter was inductively coded to allow characterisation of the structural form (content analysis) and the identification of themes (thematic analysis) common to the letters.16 The thematic focus of this study, communicating uncertainty, was explored further through discourse analysis.
Discourse analysis can be described as ‘anything beyond the sentence’17 including the ‘largely unconscious ways in which we process text and talk’.15 We analysed doctors’ use of stance18 to investigate their degree of commitment to their statements (epistemic stance) and attitudes (affective stance) towards VUS. Stance marking relates to how people position themselves in relation to what they are communicating.18 Epistemic stance indicates the degree of commitment a person displays towards what they are saying or writing and can be characterised as weak or strong.19 Examples of epistemic stance include discursive hedges such as ‘maybe’ or ‘might’ that act to lessen the speaker’s conviction towards a statement. We also coded the letters for discourse markers displaying positive or negative emotions regarding VUS – affective stance. Affective stance indicates a person’s attitude about what they are saying or writing and can be characterised as positive or negative.19
Focus group
CGs for the focus group were sampled using a purposive, criterion-based method13 to ensure that participants had experience writing consultation summary letters. Doctors were invited to participate if they were:
-
CGs or CG fellows practicing in Victoria at the time of recruitment and
-
working at VCGS between 2009 and 2013.
The focus group was digitally audio-recorded with informed consent and transcribed as described by Edwards.20 The transcript was imported into NVivo10 to facilitate the coding process. The focus group data were analysed using content and thematic analysis.21 Data were independently co-coded by two authors (RPC, JP) and themes were discussed and refined.
Results
Letter analysis
A total of 49 letters referring to patients identified with the 15q11.2 (n=35) or 16p13.11 (n=14) microdeletion were included for analysis. Twenty CGs wrote between one and 12 letters (x =4). Letters were written between 2009 (n=1) and 2013 (n=13), with the most written during 2011 (n=15). As most (96%) involved a paediatric patient, letters were addressed to the proband’s family member, although eight (16%) letters were addressed to the referring doctor, with parents/family sent a copy.
=4). Letters were written between 2009 (n=1) and 2013 (n=13), with the most written during 2011 (n=15). As most (96%) involved a paediatric patient, letters were addressed to the proband’s family member, although eight (16%) letters were addressed to the referring doctor, with parents/family sent a copy.
Content analysis
Table 1 presents the findings from the letter content analysis, representing the structural components of the letters that were identified, their frequency, and their average proportion within the letters. The three main components are discussed below.
Explanation of result
On average, 32.1% of each letter’s content was devoted to explaining the CMA result. While reporting the result, two thirds of letters also included an explanation of the CMA test itself. Twenty-six (53%) described CMA as a very detailed test, six (12%) explained that it was ‘looking for small missing or extra pieces of DNA’ (CG6_1_12) and 12 (25%) highlighted the ‘newness of microarray testing’ (CG12_4_13). Many letters (39%) described these microdeletions as ‘contributing factors’ to the child’s condition. Results were also described as: a ‘risk factor’ (29%), or ‘predisposing’ (12%) or ‘susceptibility’ factor (10%). Only three (6%) described the microdeletion as the major cause of the patient’s symptoms.
Discussion of uncertainty
Forty-seven letters (96%) included a discussion about uncertainty (Table 1), the focus of this study. The most common type of uncertainty discussed was whether the microdeletion could be considered the major cause of the patient’s symptoms (causal uncertainty; Table 2). In two letters the microdeletion was labelled as ‘normal variation’. Many letters included a reference to other areas of uncertainty, most commonly difficulties in predicting outcomes for future pregnancies (31%).
Managing the future
Twenty-one (43%) letters referred to genetics as an evolving field, with ongoing improvements in technology. This was often in the context of encouraging people to return for ‘an update’ in genetic knowledge regarding the 15q11.2 and 16p13.11 microdeletions. The two most frequent statements relating to future genetics contact were either: offering or arranging a review appointment with a specified time-frame (eg ‘We will arrange another appointment for you in our clinic in 2–3 years’ time’ CG8_2_11), or suggesting that the patient/family take responsibility for contacting the genetics service (eg ‘I would suggest that you contact us in two to three years to see if we might have further information about this deletion’ CG10_3_13). CGs described the patient as ‘discharged from genetics’ in only seven (14%) of the letters analysed in this study. There was a noticeable shift in practice from 2009 to 2013 with a decline in the number of review appointments arranged or offered over this period (data not shown).
Thematic analysis
We conducted a detailed thematic analysis to understand the ways in which CGs expressed different types of uncertainty. Table 3 provides an overview of themes related to uncertainty which were identified from analysis of letters. Extracts will be presented as evidence to illustrate the two main emergent themes.
The importance of knowing
CGs made comments regarding the importance for parents and patients to be aware of the VUS identified, particularly in regards to cascade testing, and future reproductive options for the parents and the child.
[Patient] will certainly need to be aware of this information before she has children of her own. She and her partner could be seen in a genetic clinic for counselling… CG11_1_10
Many encouraged patients to return to genetics before making reproductive decisions.
We would recommend that [patient] come back to see us when he is wanting to start a family so that we can discuss any new developments and knowledge about this particular deletion with him. CG9_3_12
Hope for the future
CGs expressed their hope that the future would bring more answers for patients and families through improvements in testing and in interpreting results.
It is likely that when [sibling] and [patient] are adults and considering having children we will have a more complete understanding about the significance of carrying a chromosomal abnormality like the 15q11.2 microdeletion. CGF2_2_CG7_2_11
Regarding improvements in understanding the impact of these microdeletions, many of the letters made comments about ‘the newness of microarray testing’, implying this would result in improvements in the interpretation of results over time.
We discussed that SNP microarray is a new test, and more information about this particular microdeletion is likely to become available in the future. CG8_2_11
They also conveyed hope to families regarding the development and management of children with the microdeletion.
We do not expect this deletion to cause any new health problems for [patient] in the future… CGF4_3_CG10_2_13
CGs provided hope to parents of children exhibiting learning difficulties through making positive statements in their letters and by writing letters to schools to help facilitate education support.
…we would certainly be very supportive of any additional assistance that [patient] could be given at this stage to help her with her early learning and I hope that now we have pin-pointed this abnormality, further assistance may be offered. CG1_4_12
Discourse analysis
CGs displayed both weak and strong epistemic stance and positive and negative affective stance when explaining VUS; however, there were clear patterns in the use of each. CGs developed stronger epistemic stance towards VUS results over time.
Epistemic stance
For the letters written between 2009 and 2010, CGs often displayed weak epistemic stance when describing the meaning of the result (discourse markers of ‘uncertainty’ underlined below).
I suspect that it probably could explain some of the early problems that she has had in the past. CG3_1_10
It is likely that this deletion is contributing to [patient’s] learning problems and behaviour difficulties but it may not be the only cause. CGF6_2_CG10_7_13
They described the VUS as being a contributing factor, risk factor or a susceptibility locus.
Our current understanding of the 15q11.2 microdeletion is that it is likely to be a contributing factor to the type of problems [patient] has presented with. CGF2_2_CG7_2_11
Even when CGs were seemingly assigning cause to the microdeletion, they still used some mitating language.
…this deletion has probably impaired his overall learning and functioning and is probably the major cause of this. CG4_1_09
CGs also displayed a consistently weak epistemic stance in regards to predicting the phenotype of children who inherit the microdeletion.
…a child who inherits this deletion might be at increased risk of neurocognitive and neurobehavioural problems. CG10_1_12
For the letters written in the period 2011-2013 that had changed to a predominantly stronger epistemic stance, with fewer markers of uncertainty.
This means that having this microdeletion is a risk factor for having problems with learning and behaviour. CGF3_2_11
Therefore, it is considered to be a risk factor for these issues. CG8_4_13
Although there was weaker epistemic commitment during interpretation of results, CGs included stronger commitment to statements at the conclusion of the letter.
It will be important for [patient] to return to the Genetic Service when she is a young adult… CGF2_2_CG7_2_11
We found that CGs used a stronger epistemic stance when describing future improvements in genetic knowledge and technology.
In the coming years our understanding of the 15q11.2 microdeletion syndrome will expand significantly. CGF2_1_CG7_1_11
Finally, the majority of CGs demonstrated a strong epistemic stance towards dissemination of information to children with the microdeletion.
[Patient] will certainly need to be aware of this information before she has children of her own. CG11_1_10
This will be important information for her when she grows up and therefore I would encourage [you] to let her know to seek genetic advice before she has children of her own. CG10_6_13
Affective stance
CGs demonstrated a negative affective stance towards diagnostic uncertainty and implications of results.
At this stage, then, it continues to be the case that we, unfortunately, do not have a specific diagnosis for [patient]. CG1_2_10
They also displayed a negative affective stance towards prenatal testing, using language to indicate their belief that these options would be undesirable.
Given the difficulty in predicting the phenotypic outcome in any given individual who inherits the 15q11 deletion, prenatal diagnosis and Preimplantation Genetic Diagnosis by IVF are typically quite difficult to counsel for and usually not requested by most affected families. CG10_5_13
Testing is available in pregnancy to detect this; however, if a baby is found to have the microdeletion, we would not be able to predict what effect if any it will have on the child, which would make any decisions about the pregnancy extremely difficult. CG8_6_11
However, doctors appeared to have more varied attitudes towards cascade testing, with some using positive and others negative affective stance in relation to this topic.
Positive: “It is possible that other members of his family have the same microdeletion, and we would be happy to offer him an appointment to discuss this further”. CG8_6_11
Negative: “We would not recommend that other members of [mother’s] family are tested for the change on chromosome 15”. CGF2_1_CG7_1_11
Overall, doctors displayed a positive affective stance when comparing the future of genetic knowledge and technology with that which is currently available.
It is possible that in the future when our genetic testing is even better than it is today, we will be able to point to other variants which have played a role for [patient] as well. CG1_1_12
Focus group
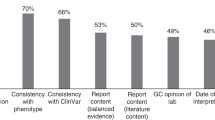
Six CGs and two CG fellows participated in the focus group. Discussion was based around findings and interpretations from the letter analysis, outlined in Table 4. The description of the microdeletion was discussed in detail in the focus group and is presented below. CGs attributed this evolution in language to seeing more families with the microdeletions as well as becoming more confident in the growing body of literature describing the phenotypic impact of the microdeletions. However, they all believed that there was still uncertainty around whether the microdeletion could be described as ‘the cause’.
CGs discussed that much has been published in recent times regarding the 15q11.2 and 16p13.11 microdeletions and they believe they are no longer considered CNVs of uncertain clinical significance at a population level. CGs reported changing their language to reflect that, moving from describing them as uncertain to using descriptors such as ‘contributing factor’ or ‘risk factor’ when communicating with patients, and often ‘susceptibility locus’ when communicating with each other.
I don’t think we use the term uncertain clinical significance in-house because it’s too non-specific…so I think the ‘risk factor’, ‘susceptibility loci’ are more… precise language when you’re talking amongst friends. CG56
However, despite recent advances in knowledge about the microdeletions, CGs felt uncertainty remained regarding how much weight could be attributed to the microdeletion as ‘the sole cause’ of ID, DD or neurobehavioural symptoms in their patients.
…because you do have findings that are really uncertain and in a way I don’t think of these in that way anymore…I think we did when they…first came along…whereas now with these we’re more confident…I guess the main question is when you’re seeing a child with this spectrum of disorders is whether this is ‘the cause’ or something else. CG6
The thematic analysis of the focus group discussion yielded a rich array of themes (Table 5) and two major themes will be detailed.
Feeling overwhelmed by the volume of VUS
Coping involves changing clinical practice
CGs believed that the greater volume of VUS they encountered influenced multiple aspects of their practice, including making fewer offers for review appointments and cascade testing.
We’ve had to move from karyotype abnormalities which are less common and more pathogenic, as a stereotype, through to susceptibility things. We can’t possibly manage the volume of-… and so we’ve had to shift our practice according to that sort of reduced pathogenicity. CG5
They described feeling like they were ‘drowning’ (CG5) in VUS results and spoke about offering fewer review appointments as a way of coping.
…our practice has shifted…to put the ball back in their [parents’] court a bit more…mostly in recognition of the swamping of our clinic with microarray changes… CG6
Turning uncertainty into an opportunity for hope
CGs recognised that VUS often challenged their ability to provide solutions for patients and families.
…families come hoping…for us to deliver…all the way back from a cure to organising…specific behavioural interventions, having some sway with how much funding they get. We don’t provide that, we don’t even provide certainty CG6
However, doctors also described uncertainty as something that could be used positively as an opportunity to provide patients with hope.
I always feel with these results, that I don’t actually have good information to give them about their child’s future, so I think this is in a way trying to move that into ‘we’re not able to help you now, but we may be able to help you better in the future’. CG4
Another CG described using the uncertainty associated with predicting phenotype as a way of reducing patients’ or parents’ anxiety regarding future pregnancy outcomes.
…it’s also managing their anxiety… and so you’re emphasising that it may not be as severe next time… CG3
Concerned by a perceived lack of control
CGs expressed concern about the lack of control they had over how patients, families and non-genetics health professionals responded to VUS.
Trying to pre-empt the thoughts, feelings and actions of others
CGs worried that some paediatricians were not accurately interpreting CMA reports of uncertain significance, and therefore those patients were missing the opportunity to be referred to a genetics service.
I’ve had a couple of conversations with the general paediatricians recently and they’re saying, ‘oh, you know, no, I’m not referring these, it’s just an uncertain result, it’s nothing’. Some of them are just ignoring them. CG2
CGs also described trying to pre-empt what patients might think or feel about a range of issues including receiving the summary letter, being a carrier of the microdeletion, future pregnancy, the possibility of prenatal testing and access to funding. One doctor described modifying their letters ‘depending on the parents’ distress [during the consultation] and my anticipated impact of the letter…’ (CG4).
They reported using language that aimed to dissuade patients from prenatal diagnosis in an attempt to pre-empt the patients’ possible interpretation of the offer of testing:
…we are countering the fact that the patient can see the offering of a test as an endorsement or a recommendation or us saying they should do that so we’re kind of trying to say ‘well yes, you can test for this but this is not necessarily a good idea (CG5).
Feeling a sense of responsibility towards the family and actions of others
When writing their letters, they felt a sense of responsibility towards ensuring positive outcomes for their patients and families. For example, trying to dissuade from prenatal testing in order to reduce the risks associated with an invasive procedure.
…you don’t want them not wanting to go through another pregnancy because they’re worried about this occurring again, and so you’re emphasising that it may not be as severe next time because there are these other factors that may not be inherited necessarily next time, so they’re not sent away with this burden… CG3
When not offering a review appointment, CGs would still encourage patients/families to contact them at any point because they wanted to end the letter with a statement ‘that provides them [family] with a way forward, it’s not discharging’ (CG6). CG1 also spoke about providing parents with some options for the future because ‘parents come wanting to know what to do, at least you can…include a recommendation to see the general paediatric team regularly…so they’ve got a place to go next’.
Discussion
CGs devoted most of the letters to explaining the test result and discussing the associated uncertainty, the main category of which was whether the microdeletion could be considered ‘the cause’ of the patient’s phenotype. They also included statements regarding the predictive uncertainty related to the VUS. Over time, statements related to the VUS had more epistemic certainty as more evidence emerged and CGs became more confident of their interpretation. Findings from the focus group identified that doctors’ letter-writing was influenced by a range of factors, related to both practical concerns, such as availability of resources, and emotional concerns such as trying to minimise anxiety for their patients/families.
Discussion of causal uncertainty
Almost all letters included some reference to causal uncertainty related to the microdeletion and the patient’s phenotype. Doctors were hesitant to assign causality, with only 6% of those letters referring to the VUS as the main explanation for the patient’s symptoms. Interestingly, previous studies have found that parents of children diagnosed with a VUS are likely to assign cause to the finding,22 even following a consultation with a VCGS genetics specialist23, 24 where they would likely have received a summary letter. Studies have also found that many parents experience a sense of relief once they know ‘the reason’ for their child’s problems, even when the result is a VUS, and that they felt it helped them to accept their child’s symptoms.23, 24
The ‘newness of microarray testing’
Describing CMA testing as ‘new’ occurred in letters written from 2010 to 2013 and by seven individual doctors. This language is consistent with a previous study which found doctors use statements such as ‘this testing is still new’ in order to provide context for the patient/family regarding the source of uncertainty.25 Furthermore, Pereira24 and Wilkins23 have suggested that parents of children diagnosed with a VUS valued the CG providing context around the ‘newness’ of CMA testing. The notion of providing context for uncertain findings by using words such as ‘new’ and terms such as ‘evolving understanding’ was confirmed by the doctors in the focus group. Notably, they also felt that this was a way of mitigating any potential discrepancies between current and future management of patients with 15q11.2 and 16p13.11 microdeletions. This could relate to the concept of doctors trying to reduce medico-legal risk.26 Contextualising their lack of certainty may be an attempt to reduce their responsibility.
Review appointments
Analysis of the letter content revealed a trend over time towards offering fewer follow-up appointments to patients with chromosome 15q11.2/16p13.11 microdeletions. When exploring possible interpretations for this trend during the letter analysis, two explanations were considered most likely: resource constraints and an increasing understanding of the inherent phenotypic variability of 15q11.2/16p13.11 microdeletions. It was also reasoned that the increased knowledge of chromosome 15q11./16p13.11 microdeletion phenotypes and penetrance27 would equate to a decrease in the need for further clinical evaluation within review appointments. When asked to comment on this trend, doctors in the focus group confirmed the above interpretations, specifically stating that chromosome 15q11.2/16p13.11 microdeletions are no longer considered of uncertain clinical significance at a population level. Doctors described feeling that they were ‘drowning’ in VUS and commented that they were trying to reserve appointments for patients where it would offer the most clinical utility. However, as many studies have consistently found, adequate follow-up is associated with improved psychosocial outcomes for patients and their families who value follow-up appointments for a range of reasons beyond clinical utility.23, 24, 28
Providing hope
Doctors demonstrated a strong epistemic stance towards future improvements in technology and knowledge suggesting strong commitment to these statements. This strong epistemic stance may suggest that doctors are confident the improvements will eventuate. Doctors are perhaps optimistic about this because evidence to date suggests that improvements in genetic technology, and therefore diagnostic potential, will continue to develop.29 In fact, this is the case with whole exome and genome sequencing currently being implemented into clinical practice.30 Doctors may also display a strong epistemic stance to provide hope to patients/families that the future holds a more certain outcome. This could be seen as a positive practice, and perhaps something that doctors have learnt through their clinical experience, as studies show that patients who perceive uncertainty as an opportunity for hope may demonstrate better adaptation to challenging circumstances.31, 32, 33 Doctors in the focus group supported the above interpretations regarding hope. Some doctors also reported being explicitly aware of using concrete statements about the future as a way of reframing current uncertainty as hope for the future.
Conclusions
From the multi-layered analysis of both the letters and focus group discussion, it appears that CGs in this study are confident with the description of chromosome 15q11.2/16p13.11 microdeletions as ‘contributing factors’ towards their patients’ phenotype; however, they remain hesitant when predicting phenotypic outcomes, particularly in relation to prenatal testing. Importantly, this study found that many components of their letter-writing were influenced by doctors’ desire to provide hope and ‘a plan for the future’ in the face of uncertainty. This study also found that there is a growing role for genetic counsellors in managing the needs of patients/families where a VUS has been diagnosed, particularly in conducting review appointments.
Implications for practice
Doctors in our study reported feeling overwhelmed by the volume of VUS results and no longer able to offer review appointments to every family; however, studies have consistently found that patients perceive greater follow-up as beneficial when receiving a genetic diagnosis such as a VUS.23, 34, 35 In cases where clinical evaluation is less important, genetic counsellors could take the role of providing follow-up. Contact with a genetic counsellor following their consultation would offer opportunities to address misunderstandings and facilitate positive adaptation in the patient and their family, which is central to the genetic counselling process.36, 37 Genetic counsellors are experienced at working with patients and their families to manage uncertainty and many have already begun adapting to managing the uncertainty associated with VUS, including the prenatal setting.38 At VCGS genetic counsellors are now taking a leading role in management of patients with a CMA VUS. This shift in workforce will assist in managing the greater number of VUS diagnosed by CMA testing and whole exome/genome sequencing technology.
Limitations
This was an exploratory study to document and understand CGs’ letter-writing practices when faced with VUS. Results may not be generalisable to all CG practices and settings. The use of a focus group could be a source of bias as participants may be reluctant to speak out in front of colleagues.39 Less experienced doctors may have felt constrained and not able to contribute as freely as more experienced doctors.
Future directions
Letter-writing is an integral component of practice for genetic health professionals and this study has evaluated the use of consultation summary letters to communicate uncertainty regarding VUS from CMA testing. It would be useful to evaluate the effectiveness of the letters in communicating uncertainty by surveying opinions of stakeholder groups such as referring doctors, patients and their families. These findings can be used to potentially improve the written communication of CGs and genetic counsellors. This is an important area for continued research, as the implementation of new sequencing technologies will continue to give rise to results of uncertain clinical significance.
References
Miller DT, Adam MP, Aradhya S et al: Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 2010; 86: 749–764.
George A, Marquis-Nicholson R, Zhang LT et al: Chromosome microarray analysis in a clinical environment: new perspective and new challenge. Br j biomed sci 2011; 68: 100–108.
Bruno DL, Beddow R, Caramins M et al: Interpreting clinical microarray genomic data in 2012: what have we learnt and what challenges remain? Curr Top Genet 2013; 5: 67–79.
Doornbos M, Sikkema-Raddatz B, Ruijvenkamp CAL et al: Nine patients with a microdeletion 15q11.2 between breakpoints 1 and 2 of the Prader–Willi critical region, possibly associated with behavioural disturbances. Eur J Hum Genet 2009; 52: 108–115.
Chaste P, Sanders SJ, Mohan KN et al: Modest impact on risk for autism spectrum disorder of rare copy number variants at 15q11.2, specifically breakpoints 1 to 2. Autism Res 2014; 7: 355–362.
O'Reilly M, Cahill M, Perry I : Writing to patients: a randomised control trial. Clin Med (Lond) 2006; 6: 178–182.
Roberts NJ, Partridge MR : How useful are post consultation letters to patients? BMC med 2006; 4: 2.
Hallowell N, Murton F : The value of written summaries of genetic consultations. Patient Educ Couns 1998; 35: 27–34.
Turbitt E, Halliday JL, Metcalfe SA : Key informants’ perspectives of implementing chromosomal microarrays into clinical practice in australia. Twin Res Hum Genet 2013; 16: 833–839.
Reiff M, Mueller R, Mulchandani S, Spinner NB, Pyeritz RE, Bernhardt BA : A qualitative study of healthcare providers' perspectives on the implications of genome-wide testing in pediatric clinical practice. J Genet Couns 2014; 23: 474–488.
Reiff M, Ross K, Mulchandani S et al: Physicians' perspectives on the uncertainties and implications of chromosomal microarray testing of children and families. Clin Genet 2013; 83: 23–30.
Blumer H : Symbolic Interactionism: Perspective and Method. New Jersey: Prentice-Hall Inc, 1969.
Babbie E : The Practice of Social Research, 9th edn. Belmont, CA: Wadsworth Thomson, 2001.
QSR International: NVivo qualitative data analysis Software [computer program], Version 10. Melbourne: QSR International Pty Ltd, 2012.
Roberts C, Sarangi S : Theme-oriented discourse analysis of medical encounters. Med Educ 2005; 39: 632–640.
Saldana J : The Coding Manual for Qualitative Researchers, 2nd edn. Thousand Oaks, CA: SAGE Publications Inc., 2013.
Cameron D : Working With Spoken Discourse. London: SAGE Publishing Ltd., 2001.
Goodwin MH, Cekaite A, Goodwin C . Emotion as stance. in: Sorjonen M, Perakyla A (eds): Emotion in Interaction. Oxford, UK: Oxford University Press, 2012; 16–41.
Ochs E, Capps L : Narrating the self. Annu rev anthropol 1996; 19–43.
Edwards JG The transcription of discourse. in: Schiffrin D, Tannen D, Hamilton HE (eds): The Handbook of Discourse Analysis. Malden, MA, USA: Blackwell Publishers Ltd., 2001; 321–348.
Holloway I, Wheeler S : Qualitative Research in Nursing and Healthcare. John Wiley & Sons, 2013.
Reiff M, Bernhardt BA, Mulchandani S et al: ‘What does it mean?’: uncertainties in understanding results of chromosomal microarray testing. Genet Med 2012; 14: 250–258.
Wilkins E : "It wasn't a Disaster or Anything": Parents' Experiences of Their Child's Uncertain Chromosomal Microarray Result. Melbourne, Australia: The University of Melbourne, 2013.
Pereira K : Exploring the Experiences of Families with a Child with an Autism Spectrum Disorder and an Abnormal Microarray. Melbourne, Australia: The University of Melbourne, 2013.
Crowe M : Discourse analysis: towards an understanding of its place in nursing. J Adv Nurs 2005; 51: 55–63.
Abbott R, Cohen M : Medico-legal issues in cardiology. Cardiol Rev 2013; 21: 222–228.
Rosenfeld JA, Coe BP, Eichler EE, Cuckle H, Shaffer LG : Estimates of penetrance for recurrent pathogenic copy-number variations. Genet Med 2013; 15: 478–481.
McAllister M, Payne K, MacLeod R, Nicholls S, Donnai D, Davies L : What process attributes of clinical genetics services could maximise patient benefits. Eur J Hum Genet 2008; 16: 1467–1476.
Phadke S : Cytogenetic microarray in prenatal and postnatal diagnosis. Mol Cytogenet 2014; 7 (Suppl 1 Proceedings of the International Conference on Human): I32.
Biesecker LG, Green RC : Diagnostic clinical genome and exome sequencing. N Engl J Med 2014; 371: 1170.
Babrow AS, Kasch CR, Ford LA : The many meanings of uncertainty in illness: toward a systematic accounting. Health Commun 1998; 10: 1–23.
Bliton MJ : Parental hope confronting scientific uncertainty: a test of ethics in maternal-fetal surgery for spina bifida. Clin Obstet Gynecol 2005; 48: 595–607.
Truitt M, Biesecker B, Capone G, Bailey T, Erby L : The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Educ Couns 2012; 87: 233–238.
Biesecker BB, Erby L : Adaptation to living with a genetic condition or risk: a mini-review. Clin. Genet 2008; 74: 401–407.
Lipinski SE, Lipinski MJ, Biesecker LG, Biesecker BB : Uncertainty and perceived personal control among parents of children with rare chromosome conditions: the role of genetic counseling. Am J Med Genet A 2006; 142: 232.
Veach P, LeRoy B, Bartels D : Genetic Counseling Practice: Advanced Concepts and Skills. Hoboken, NJ: John Wiley & Sons, Inc, 2010.
Resta R, Biesecker BB, Bennett RL et al: A new definition of Genetic Counseling: National Society of Genetic Counselors' Task Force report. J Genet Couns 2006; 15: 77–83.
Bernhardt BA, Soucier D, Hanson K, Savage MS, Jackson L, Wapner RJ : Women's experiences receiving abnormal prenatal chromosomal microarray testing results. Genet Med 2013; 15: 139–145.
Liamputtong P : Focus Group Methodology: Principle and Practice. Thousand Oaks, CA: SAGE Publications Inc., 2011.
Acknowledgements
This study was supported by the Murdoch Childrens Research Institute and the Victorian Government's Operational Infrastructure Support Program. It was completed in partial fulfilment of the requirements for the Master of Genetic Counselling, University of Melbourne, Victoria, Australia. The authors acknowledge the course coordinators Margaret Sahhar and Jan Hodgson for supporting the original development of this research for RPC’s minor thesis. We also acknowledge the clinical geneticists who participated in the focus group and allowed us to analyse their letter writing practices.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Paul, J., Pope-Couston, R., Wake, S. et al. Communicating microarray results of uncertain clinical significance in consultation summary letters and implications for practice. Eur J Hum Genet 25, 22–30 (2017). https://doi.org/10.1038/ejhg.2016.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2016.135
This article is cited by
-
Who ever heard of 16p11.2 deletion syndrome? Parents’ perspectives on a susceptibility copy number variation syndrome
European Journal of Human Genetics (2020)
-
Phenotypic association of 15q11.2 CNVs of the region of breakpoints 1–2 (BP1–BP2) in a large cohort of samples referred for genetic diagnosis
Journal of Human Genetics (2019)