Abstract
Genetic testing is becoming more commonplace in general and specialist health care and should always be accompanied by genetic counselling, according to Swedish law. Genetic counsellors are members of the multi-disciplinary team providing genetic counselling. This study examined the role and added value of genetic counsellors in Sweden, using a cross-sectional on-line survey. The findings showed that the genetic counsellors added value in the clinical setting by acting as the ‘spider-in-the-web’ regarding case management, having a more holistic, ethical and psychological perspective, being able to offer continuous support and build a relationship with the patient, and being more accessible than medical geneticists. The main difference between a genetic counsellor and medical geneticist was that the doctor had the main medical responsibility. Thus genetic counsellors in Sweden contribute substantially to the care of patients in the clinical genetic setting.
Similar content being viewed by others
Introduction
One in 17 Europeans, or approximately 30 million people, will be affected by a rare disease (usually with a genetic cause) during their life and potentially require clinical genetic services.1 The number of genetic tests available for clinical use has risen from 300 to about 3000 in just 20 years.2 Consequently, the higher demand for and complexity of genetic testing3 inevitably results in increased pressure on clinical genetics services. The knowledge of disease-causing genetic mutations is also spreading to more health-care settings,4 leading to an increased demand for genetic testing and naturally the need for genetic counselling accompanying the testing, as required by law in Sweden.5, 6 However, genetic testing is not the only context for genetic counselling, as it is relevant in many other situations, including where a new genetic diagnosis is made, when a genetic risk assessment is made, when patients are making decisions about clinical screening or prophylactic treatment and when reproductive options are discussed.
There have been calls for specialist genetic professionals to work alongside other practitioners in primary, secondary and tertiary care.4 The specialist genetic team in many countries includes non-medical genetic counsellors.7 Before the introduction of genetic counsellors into clinical genetics in Sweden, genetic counselling was the responsibility of the medical geneticists; however, gradually genetic counsellors were included in the clinical team on an ad hoc basis. As there was no coordinated national policy, this means that there is no unified approach to the use of genetic counsellors within clinical teams. A common understanding of the genetic counsellor’s role can help to clarify how genetic counsellors should work within the health-care team, their added value to patient care and to the clinical team, as well as the necessary components in educational programmes for genetic counselling.
Genetic counsellors and genetic nurses are usually employed in specialist genetic clinics or other specialist services, such as oncology, cardiology and foetal medicine.8, 9 A genetic disease and testing may have an impact on the psychological, social and practical aspects of a patient’s life and the genetic counsellor has a responsibility to try to ensure the patient is appropriately equipped to manage it.10 The genetic counsellor should be specifically trained to help people understand and adapt to the medical, psychosocial and familial implications of genetics.11 Personal and professional competence is necessary to be able to provide safe and effective genetic counselling.12 The development of this competence depends upon specific education, a clear role13 and regulation of the profession; for example, the registration system for genetic counsellors that now exists in Europe.14 However, in many European countries, including Sweden, genetic counsellors are still an emerging professional group. The experiential and educational backgrounds of genetic counsellors vary considerably among individuals, ranging from nurses, biomedical analysts, molecular biologists or psychologists. In line with European recommendations for genetic testing,5, 6, 15 The Swedish law on genetic integrity6 requires that genetic testing is accompanied by genetic counselling and informed consent from the patient and that professionals providing genetic counselling must have specific training. In Sweden, there is at present neither university-level education in genetic counselling nor a requirement for professional licensing or registration. The professional standards of genetic counsellors may be eroded as institutions can employ anyone to perform this role, regardless of prior education or experience in the field. Since the law was passed in 2006, no substantial measures have been taken to improve the situation, and it appears that genetic counselling is not always provided according to European recommendations;5 for example, genetic testing is not always preceded by appropriate genetic counselling. The development of the profession in Sweden has grown out of clinical demand and employing people from other professional categories to work as genetic counsellors. All these individuals have higher education, and some have taken specific courses in genetic counselling, through university courses that no longer exist. At the time of writing, the only related course is a short continuiing professional development course on genetic counselling for midwives, focussed on non-invasive prenatal diagnosis in the clinical setting.
The role of the genetic counsellor was investigated in a systematic review of research published between 2003 and 2013.8 It showed that genetic counsellors, when utilised in the clinical genetics setting, undertook a significant workload related to direct patient care, and that this seemed acceptable to patients. However, none of the studies included in that research had been conducted in Sweden, or indeed in any other European country. The objective of our present study was therefore to describe the current practice of genetic counsellors and to explore the role and added value of the genetic counsellors in the clinical setting in Sweden.
Materials and Methods
Study design
A mixed method approach was chosen because it allowed collection of both quantitative and qualitative data.16 A cross-sectional survey included set-response and open-ended questions, which allowed participants to respond in their own words.
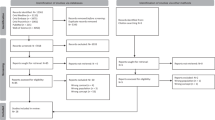
Recruitment procedure
The aim was to recruit professionals working as genetic counsellors in Sweden. The Swedish National Association for Genetic Counsellors (SFGV) is the official organisation for any person with a professional interest in genetic counselling. We invited the entire cohort using SFGV’s e-mail list serve, which at the time included 58 individuals. A short introductory letter, including the link to the survey, was e-mailed to recipients (Supplementary File S1). We allowed potential participants 2 weeks to respond, and they were invited to ask questions about the study during that time. Two reminders were sent out during this time. It was iterated that participation was anonymous and voluntary.
Data collection
As no previous survey on genetic counsellor tasks and perceptions could be found, the questionnaire was developed by studying the literature and discussing with experts. The survey included a short introduction, fixed-choice questions and several open-ended questions that allowed for more detailed responses to selected topics. The questions covered demographics, genetic counsellors’ work tasks, division of responsibilities and the unique contribution of genetic counsellors in the clinical setting. The survey took approximately 15–20 min to complete. Three academic colleagues (not included in the sample) were asked to pilot the survey to identify any changes that were required. Data collection was supported by the data collection tool in Google Drive (www.google.com).
Data analysis
Descriptive statistical analysis was performed on the data derived from responses to the fixed-choice questions. Values for missing answers varied from 0% to 31% and were not included in statistical analysis of that specific response. Thematic qualitative analysis17 was used to analyse this data set. Braun and Clarke17 describe a method that we used to answer specific questions, in a deductive way. The approach involved becoming familiar with the data, coding each statement and identifying those codes that were relevant to our research question. The codes were then grouped to find patterns of meaning, before being organised under key themes. These themes were reviewed by all the authors, defined and given a descriptive name.18
Ethical approval
This study did not involve sensitive personal information, biological samples or manipulation of subjects physically or psychologically. It was therefore exempt from ethical approval, according to the guidelines of the Central Ethical Review Board in Sweden.
Results
Demographic characteristics
The survey was completed by 19 genetic counsellors (33% response rate) with a mean age of 53 years (range 36–65 years). All were women. Two had <1 year’s experience as genetic counsellors, nine had 2–5 years’ experience, six had 6–10 years’ experience and two had >10 years’ experience in the occupation. Sixteen reported their professional title as genetic counsellor, while only 13 were officially employed as genetic counsellors. Five persons worked in a Clinical Genetics Department and nine in non-genetic specialist departments, such as oncology, cardiology, geriatrics or paediatrics. The highest general educational qualification of each respondent was reported: five had a PhD; nine a Master’s degree; three a Nursing degree; and one was trained as a laboratory technician. Regarding training specific to genetic counselling, 12 had a graduate diploma and only 1 had a Master’s degree; 4 had undertaken supplementary courses and 2 had received workplace education.
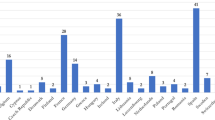
Genetic counsellors’ work tasks
The work tasks of genetic counsellors were identified as taking place before, during and/or after a patient’s clinic visit. Additional work tasks, not involved in the clinic visits, were also reported.
Preclinic tasks
The genetic counsellors all had similar tasks prior to a patient's clinic visit. As shown in Table 1, almost all made contact with the patients, collected relevant information from patients about family history and informed them about their investigation process. When risk assessment was performed, tools such as the Claus table were used. In some cases, a psychological assessment was done prior to the clinic visit, as this quote illustrates:
‘[I] try to get an idea of if the patient needs support, their view on prenatal screening and potential termination of pregnancy, before screening with genetic tests…’ (Respondent No. 9).
During the clinical consultation
The majority of respondents reported being present during the patients’ clinic visits and provided genetic counselling without other professionals present. Three quarters co-counselled with a medical doctor and one fifth co-counselled with another genetic counsellor. Nearly half of the respondents wrote specifically that, during patient consultations together with a medical doctor, they would not themselves give the genetic counselling. Instead this was provided by the doctor, as commented on by this respondent:
‘Often I have my own counselling visits but sometimes I sit in (without giving counselling) during the doctor’s visit’ (Respondent No. 4).
Postclinical consultation
The majority of genetic counsellors reported having follow-up contact with patients after their clinic visit, either in person, by telephone or in writing (Table 2).
Additional tasks
Nearly two-thirds of respondents (n=11, 61%) conducted research; the same number took part in professional development. More than half reported teaching co-workers (n=12, 67%), other health-care professionals (n=13, 72%) and the general public (n=9, 50%).
Division of responsibility: Who does what?
Opinions about responsibilities during the clinic visits were also sought. The questions were designed to identify which professional should have the main responsibility for a certain task, according to the respondent. The results can be seen in Table 3.
Genetic counsellors’ main responsibilities
The majority of respondents agreed that a genetic counsellor should be solely responsible to act as the family’s clinical contact person, draw a pedigree, provide follow-up contact after the clinic visit, provide psychosocial support and inform the patients about basic genetics and presymptomatic testing. There were a number of tasks that could be performed by either a genetic counsellor or medical geneticist. However, the majority of respondents agreed that the medical geneticists alone should be responsible for a range of medical tasks, including making a diagnosis.
Tasks not considered relevant for genetic counsellors
The survey included questions on work tasks actually undertaken by genetic counsellors, compared with what they thought they should do. It became clear which tasks were not considered part of the genetic counsellor's role. Administrative tasks such as sample handling, billing, arranging appointments and general administration were frequently done, even though most respondents did not regard them as appropriate tasks for genetic counsellors. Instead, most genetic counsellors wanted more patient-related work time. This was illustrated by several respondents:
‘I would desire less administrative work and more patient contact’ (Respondent No. 12).
‘More of my own patient visits would increase my competence so I would feel more secure when giving information, even when it is bad news’ (Respondent No. 6).
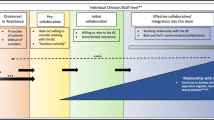
The value added by genetic counsellors in the clinical setting
The last part of the survey contained open-ended questions to investigate genetic counsellors’ unique competence and added value in a clinical setting. These questions focussed on how the genetic counsellor complete the clinical genetics team, which includes medical geneticists who also provide genetic counselling, and clinical scientists performing and analysing the genetic tests.
The value added by a genetic counsellor
One of the overall aims of the study was to identify whether there was a unique contribution made by genetic counsellors, which differs from other professionals providing genetic counselling in a clinical setting. Thematic analysis of responses to the second and third open-ended questions (see Supplementary File S1) made it clear what was considered added value by genetic counsellors in the clinical setting. The results are presented as four themes:
(1) Case management
This was the most apparent added value of a genetic counsellor, that is, necessary to be able to get an overview and insight into each case, and create an understanding for each patient’s unique situation. Several respondents used the term ‘Spider in the web’ to describe the practical contribution of genetic counsellors to each patient’s investigation, as illustrated by these quotes:
‘…(genetic counsellors) have a wide set of contacts in the whole country with medical record archives and authorities’ (Respondent No. 4).
‘The genetic counsellor does all the preparatory work with interviews, family research and pedigrees, collects and collates medical records and samples’ (Respondent No. 5).
(2) Holistic, ethical and psychological view
The second theme was the genetic counsellors’ capacity to attend to the whole individual or family, including the psychological aspects. Genetic counsellors’ holistic, ethical and psychological perspective on genetic counselling and on the patient was illustrated by several participants:
‘…to have the whole picture of the individual/family and to be responsive to the ethical and psychosocial bits…’ (Respondent No. 3).
‘…broader education in genetic counselling, meaning psychology and medical and even knowledge about the health care system as a whole.’ (Respondent No. 20).
‘To focus on the genetic information and the patient’s responses and questions, not on the medical aspects’ (Respondent No. 6).
(3) The genetic counsellor’s relationship with the patient and offering continuous support
The third theme was the genetic counsellor’s ability to build relationships with individuals and families, sometimes over many years, and to be able to offer continuous support to these people. This theme is illustrated by the following quotes:
‘…possibility for continuous family contact and consequently better support to the family’ (Respondent No. 19).
‘Often (the genetic counsellor) contacts the patient several times before the clinic visit…therefore there is already an established relationship when the patient comes for genetic counselling’ (Respondent No. 6).
(4) The genetic counsellor is more accessible compared with medical geneticist
This theme highlights the accessibility of genetic counsellors’ in comparison to medical geneticists. To be able to build relationships and offer continuous support, the genetic counsellor must be readily available and flexible. This was considered a benefit to the patient, as illustrated by the following quotes:
‘ …possibility to offer follow-up by phone or in person, whenever needed’ (Respondent No. 3).
‘Have more time and contact continuity’ (Respondent No. 8).
It became clear that the genetic counsellor’s role is specific but that some tasks may overlap with that of the medical geneticist. In this survey, the main contribution of the medical geneticist (M.D.) was considered their medical knowledge, accountability and the skill to deal with the more complex cases. Therefore, tasks requiring these skills were not considered to be appropriate for genetic counsellors, as shown by the following quote:
‘If there are medical questions or difficult assessments these should be done by an M.D.’ (Respondent No. 21).
Discussion
This study showed that the psychological aspects of genetic counselling, as well as building rapport with, and being available for the patients were central to the genetic counsellor’s role. Most respondents thought they had a responsibility to help patients express their own concerns, discuss common psychological reactions and feelings to genetic testing, including the potential effects on patients’ lives and relationships. This finding is consistent with the role of genetic counsellors found in the systematic review by Skirton et al,8 where an empathic, client-centred approach to the families was stressed.8 This approach requires flexibility and accessibility to patients and sufficient clinical time, which is not always the case for health professionals in specialist clinics.19 One rationale to use genetic counsellors to provide clinical care is because they may have more clinical time available, compared with, that is, medical geneticists,8 concurring with the findings reported in this study. Whether or not this is true, genetic counsellors in our study stressed that they were more accessible to patients than other colleagues.
Certain aspects of genetic counsellor work (eg, accessibility, continuity of care and a holistic approach) provide added value to the patient in the clinical setting and were clearly illustrated by this study. However, the study points to potential underuse of genetic counsellors in some cases, as compared with colleagues in other countries who may provide genetic counselling in a wider range of situations.8 Some respondents were not even actively involved in providing genetic counselling at all, and others reported that they did not provide genetic counselling while present in consultations with doctors. This situation differs greatly from that in other countries such as France and United Kingdom, where co-counselling between medical staff and genetic counsellors is common.20 Another factor contributing to misuse of resources was that many genetic counsellors were overly burdened by administrative tasks, reducing patient contact time. The respondents agreed that genetic counsellors generally should not undertake medical diagnostic exams or other medical tasks (such as prescribing medication), which was considered the responsibility of the medical geneticist. This matches the findings in the review on genetic counsellors’ role.8
Our results indicate that genetic counsellors differentiate between information provided by medical geneticists or by genetic counsellors. However, there were some differences of opinion. Although some thought informing the patients about diagnostic testing, familial risk (without a known mutation) and about genetic variants of unclear significance was considered a equal responsibility between genetic counsellors and medical geneticists, others believed these tasks could be the responsibility of the genetic counsellor. This indicates that at least some genetic counsellors are willing to take on more challenging and complex tasks. The delineation between the nature of information to be given is not an issue that, to our knowledge, has arisen in previous studies. One explanation could be the substantial variation in educational pathways and scientific knowledge among Swedish genetic counsellors.
The Swedish law on genetic integrity6 included a declaration that genetic education and genetic counselling were of utmost importance in order to provide adequate healthcare; however, these were found to be insufficient at the time.6 Moreover, university-level courses specific to genetic counselling were offered until 2013 but have shut down for administrative reasons. As described by Sahar et al,21 the development of genetic counselling as a profession may be hindered due to the lack of supportive professional infrastructure and an educational programme.21 In contrast to the Swedish situation, the French government took a different approach in 2004, when the French parliament passed a law protecting the professional title, and establishing an educational programme for genetic counsellors. A transfer of tasks between health professionals was initiated, and genetic counsellors were successfully integrated into health-care teams.22
Although it may not be possible to set up a national system and requirement for registration in a country with the small population of Sweden (9.14 million inhabitants in 2014), in order to harmonise genetic counselling practice and professional development nationally, and on a European scale, the European Board of Medical Genetics (EBMG) offer registration for qualification as a genetic counsellor in Europe since 2013 (endorsed by the European Society of Human Genetics).14 This could potentially give credit and recognition to a profession in growing demand. In fact, in 2015 at least one genetic counsellor from Sweden is already registered under the EBMG.14
Strengths and limitations of the study
The survey had a 33% response rate (19/58 responded) among all members of the national society for genetic counsellors (SFGV), the only professional interest group for genetic counselling in Sweden. However, not all SFGV members actually work as genetic counsellors, so not all recipients of the survey were eligible to participate. Members with a special interest, or education in genetic counselling, but not working as genetic counsellors were asked to refrain from participating in the survey. This limited the response rate, as well as a potential perceived lack of anonymity, as the community is rather small. There is also the risk that not all practicing genetic counsellors and genetic nurses in Sweden had the opportunity to participate, as membership in SFGV is voluntary. However, to the best of our knowledge, the vast majority of practicing genetic counsellors were members of this organisation at that time and the number of responses corresponds to the expected number of practicing genetic counsellors. The questionnaire was self-developed and study-specific, thus not validated, which is an additional limitation in this study.
Practical relevance
This research helps define the role and points to some of the added values of using genetic counsellors in the clinical setting in Sweden and may reflect the situation in some other European countries. However, more needs to be done in order to achieve established professional standards, which promote quality services and genetic counsellors to be a natural part of multidisciplinary health-care teams. In Sweden, achieving the core competency standards and a registration system as set by the EBMG will be difficult as long as there is no official further education specific to genetic counselling. This study may provide a platform for this to be achieved.
Conclusions
The results indicate that there is room to further advance the genetic counsellors’ role in the Swedish health-care system and merge it towards that of other countries in Europe where the genetic counselling profession is better developed. However, further research is needed to explore the conclusions of this study from the medical doctor’s and patient’s perspective. Ultimately, all efforts should be directed at ensuring safe and equitable genetic counselling services for all patients at risk of genetic conditions.
References
About rare diseases. Rare Disease UK 2014. Available at www.raredisease.org.uk (accessed 12 September 2014).
GeneTests. GeneTestsReviews. Available at www.ncbi.nlm.gov/sites/GeneTests (accessed 30 July 2014).
Hannig VL, Cohen MP, Pfotenhauer JP, Williams MD, Morgan TM, Phillips JA : Expansion of genetic services utilizing a general genetic counseling clinic. J Genet Couns 2014; 23: 64–71.
Battista RN, Blancquaert I, Laberge AM, Van Schendel N, Leduc N : Genetics in health care: An overview of current and emerging models. Public Health Genomics 2011; 15: 34–45.
EuroGentest. Harmonizing genetic testing across Europe. Available at http://www.eurogentest.org/index.php?id=154 (accessed 12 September 2014).
The Swedish government offices Law on Genetic Intergrity (Svensk Författningssamling) 2006, pp 1–10.
Cordier C, Lambert D, Voelckel MA, Hosterey-Ugander U, Skirton H : A profile of genetic counsellor and genetic nurse profession in Europe. J Community Genet 2012; 3: 19–24.
Skirton H, Cordier C, Ingvoldstad C, Taris N, Benjamin C : The role of the genetic counsellor: a systematic review of research evidence. Eur J Hum Genet 2015; 23: 452–458.
Henriksson K, Olsson H, Kristoffersson U : The need for oncogenetic counselling. Ten years’ experience of a regional oncogenetic clinic. Acta Oncol 2004; 43: 637–649.
Decruyenaere M, Evers-Kiebooms G, Cloostermans T et al: Psychological distress in the 5-year period after predictive testing for Huntington’s disease. Eur J Hum Genet 2003; 11: 30–38.
National Society of Genetic Counselors. About genetic counselors. Available at http://www.nsgc.org/p/cm/ld/fid=175 (accessed 30 June 2014).
Guimarães L, Sequeiros J, Skirton H, Paneque M : What counts as effective genetic counselling for presymptomatic testing in late-onset disorders? A study of the consultand’s perspective. J Genet Couns 2013; 22: 437–447.
Skirton H, Cordier C, Lambert D, Hosterey Ugander U, Voelckel MA, O’Connor A : A study of the practice of individual genetic counsellors and genetic nurses in Europe. J Community Genet 2013; 4: 69–75.
European Board of Medical Genetics. European process for registration as genetic counsellor or genetic nurse. Available at https://www.eshg.org/471.0.html (accessed 28 January 2015).
The Organisation for Economic Co-operation and Development. OECD Guidelines for Quality Assurance in Molecular Genetic Testing. Available at http://www.oecd.org/sti/biotech/oecdguidelinesforqualityassuranceingenetictesting.htm.
Johnson B, Christensen LB : Educational Research: Quantitative and Qualitative Approaches. University of Michigan, Ann Arbor, MI, USA: Allyn and Bacon, 2000.
Braun V, Clarke V : Using thematic analysis in psychology, 2006. Available at http://eprints.uwe.ac.uk/11735/1/thematic_analysis_revised_%2D_final.doc.
Polit DF, Beck CT : Nursing Research: Generating and Assessing Evidence for Nursing Practice, 9th edn. Philadelphia, PA, USA: LWW, 2011. Available at http://www.amazon.com/Nursing-Research-Generating-Assessing-Evidence/dp/1605477087/ref=sr_1_1?ie=UTF8&qid=1403544525&sr=8-1&keywords=pilot+and+beck+nursing+research.
O’Shea R, Murphy AM, Treacy E, Lynch SA, Thirlaway K, Lambert D : Communication of genetic information by other health professionals: the role of the genetic counselor in specialist clinics. J Genet Couns 2011; 20: 192–203.
Skirton H, Kerzin-Storrar L, Barnes C et al: Building the genetic counsellor profession in the United Kingdom: two decades of growth and development. J Genet Couns 2013; Vol 22: 902–906.
Sahar M, Young M-A, Sheffield L, Aitken M : Educating genetic counselors in Australia: developing an international perspective. J Genet Couns 2005; 4: 283–294.
Cordier C, Taris N, De Pauw H, Sobol N, Philip N, Voelckel MA : French professionals in genetic counselor careers. J Genet Couns 2013; 22: 844–848.
Acknowledgements
Financial support was rendered from the Department of Clinical Pathology and Clinical Genetics, and Department of Clinical and Experimental Medicine, Linköping University, Linköping, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on European Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Pestoff, R., Ingvoldstad, C. & Skirton, H. Genetic counsellors in Sweden: their role and added value in the clinical setting. Eur J Hum Genet 24, 350–355 (2016). https://doi.org/10.1038/ejhg.2015.110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2015.110
This article is cited by
-
Thirty-years of genetic counselling education in Europe: a growing professional area
European Journal of Human Genetics (2024)
-
The role of the Genetic Counsellor in the multidisciplinary team: the perception of geneticists in Europe
European Journal of Human Genetics (2022)
-
Developing a national certification pathway for genetic counselors in Sweden—a short report
Journal of Community Genetics (2020)
-
Factors influencing use of telegenetic counseling: perceptions of health care professionals in Sweden
Journal of Community Genetics (2019)
-
The Global State of the Genetic Counseling Profession
European Journal of Human Genetics (2019)